Prevalence of Metabolic Syndrome According to Physical Activity, Dietary Habits, Mental Status, Social Status, Health Behavior, and Obesity Phenotypes in Korean Adolescents: 2016–2021
Abstract
:1. Introduction
2. Materials and Methods
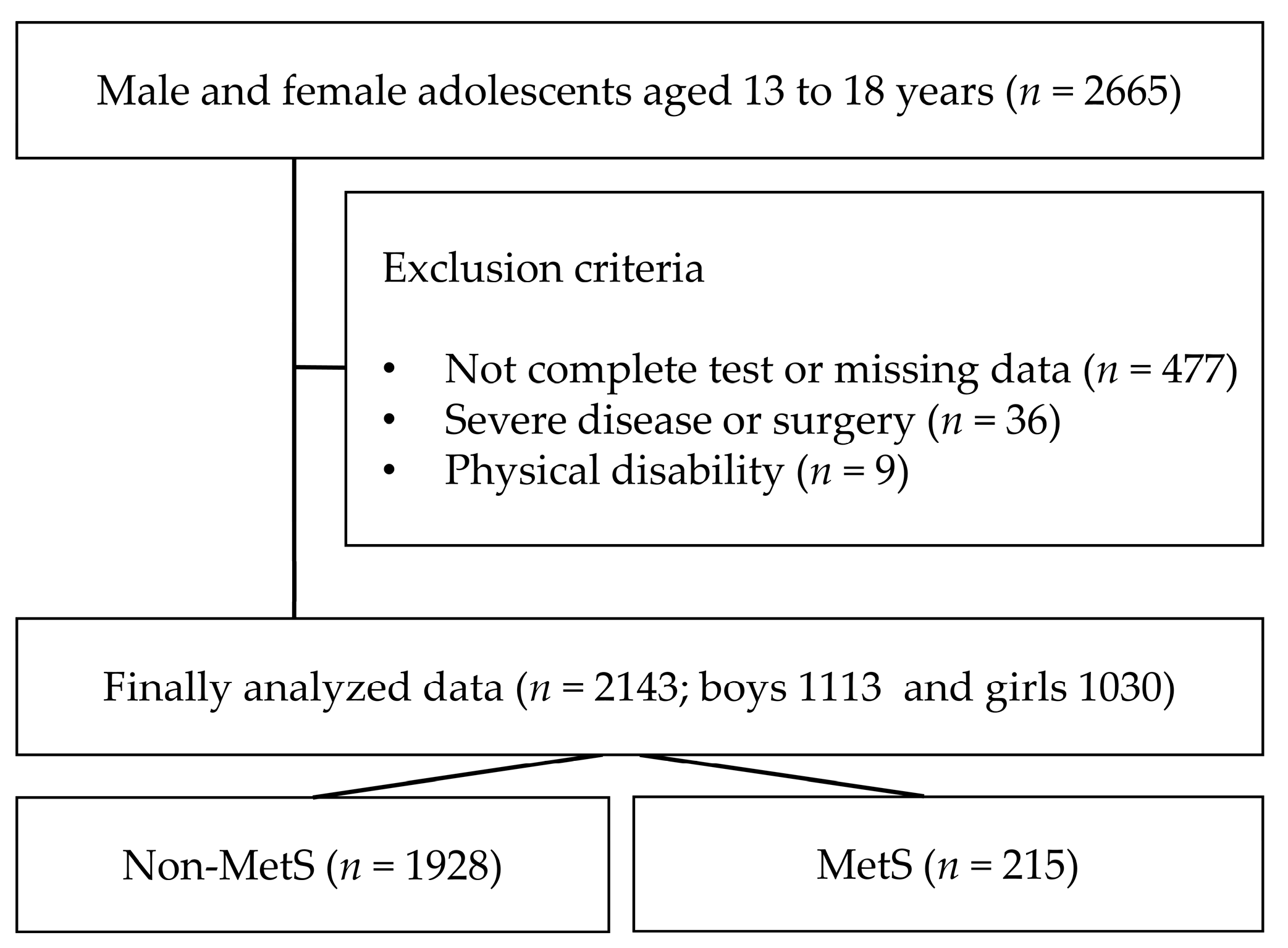
2.1. Research Process and Participants
2.2. Questionnaire: Leisure PA, Dietary Habits, Alcohol, Smoking, Household Income
2.3. Body Measurements, Blood Collection, and BP
2.4. Diagnosis MetS and Obesity
2.5. Data Analysis
3. Results
3.1. General Characteristics and Sociological Status of Participants with and without MetS
3.2. MetS OR According to Social and Mental Status Health
3.3. MetS OR According to PA and Dietary Habits
3.4. Relationship between PA and Dietary Habits in MHO and MUNW
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Reisinger, C.; Nkeh-Chungag, B.N.; Fredriksen, P.M.; Goswami, N. The prevalence of pediatric metabolic syndrome—A critical look on the discrepancies between definitions and its clinical importance. Int. J. Obes. 2021, 45, 12–24. [Google Scholar] [CrossRef]
- Haththotuwa, R.N.; Wijeyaratne, C.N.; Senarath, U. Worldwide Epidemic of Obesity; Elsevier: Amsterdam, The Netherlands, 2020; pp. 3–8. [Google Scholar]
- Sanyaolu, A.; Okorie, C.; Qi, X.; Locke, J.; Rehman, S. Childhood and adolescent obesity in the United States: A public health concern. Glob. Pediatr. Health 2019, 6, 2333794X19891305. [Google Scholar] [CrossRef]
- Guo, Y.; Yin, X.; Wu, H.; Chai, X.; Yang, X. Trends in overweight and obesity among children and adolescents in China from 1991 to 2015: A meta-analysis. Int. J. Environ. Res. Public Health 2019, 16, 4656. [Google Scholar] [CrossRef] [PubMed]
- Simmonds, M.; Llewellyn, A.; Owen, C.G.; Woolacott, N. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 95–107. [Google Scholar] [CrossRef]
- Nilsson, P.M.; Tuomilehto, J.; Rydén, L. The metabolic syndrome—What is it and how should it be managed? Eur. J. Prev. Cardiol. 2019, 26, 33–46. [Google Scholar] [CrossRef]
- Li, X.; Zhai, Y.; Zhao, J.; He, H.; Li, Y.; Liu, Y.; Feng, A.; Li, L.; Huang, T.; Xu, A. Impact of metabolic syndrome and it’s components on prognosis in patients with cardiovascular diseases: A meta-analysis. Front. Cardiovasc. Med. 2021, 8, 704145. [Google Scholar] [CrossRef]
- Xu, F.; Cohen, S.A.; Lofgren, I.E.; Greene, G.; Delmonico, M.J.; Greaney, M.L. The association between physical activity and metabolic syndrome in older adults with obesity. J. Frailty Aging 2019, 8, 27–32. [Google Scholar] [CrossRef]
- Hoyas, I.; Leon-Sanz, M. Nutritional challenges in metabolic syndrome. J. Clin. Med. 2019, 8, 1301. [Google Scholar] [CrossRef] [PubMed]
- Booker, R.; Chander, H.; Norris, K.C.; Thorpe, R.J., Jr.; Vickers, B.; Holmes, M.E. Comparison of Leisure Time Physical Activities by Metabolic Syndrome Status among Adolescents. Int. J. Environ. Res. Public Health 2022, 19, 1415. [Google Scholar] [CrossRef] [PubMed]
- Kirk, D. The ‘obesity crisis’ and school physical education. Sport Educ. Soc. 2006, 11, 121–133. [Google Scholar] [CrossRef]
- Tamashiro, K.L. Metabolic syndrome: Links to social stress and socioeconomic status. Ann. N. Y. Acad. Sci. 2011, 1231, 46–55. [Google Scholar] [CrossRef]
- Tomiyama, A.J. Stress and obesity. Annu. Rev. Psychol. 2019, 70, 703–718. [Google Scholar] [CrossRef]
- Chandola, T.; Brunner, E.; Marmot, M. Chronic stress at work and the metabolic syndrome: Prospective study. BMJ 2006, 332, 521–525. [Google Scholar] [CrossRef]
- Ehrlich, K.B.; Hoyt, L.T.; Sumner, J.A.; McDade, T.W.; Adam, E.K. Quality of relationships with parents and friends in adolescence predicts metabolic risk in young adulthood. Health Psychol. 2015, 34, 896. [Google Scholar] [CrossRef]
- Craig, C.; Marshall, A.; Sjostrom, M.; Bauman, A.; Lee, P.; Macfarlane, D.; Lam, T.; Stewart, S. International physical activity questionnaire-short form. J. Am. Coll. Health 2017, 65, 492–501. [Google Scholar]
- Oh, J.Y.; Yang, Y.J.; Kim, B.S.; Kang, J.H. Validity and reliability of Korean version of International Physical Activity Questionnaire (IPAQ) short form. J. Korean Acad. Fam. Med. 2007, 28, 532–541. [Google Scholar]
- Liguori, G. ; American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2020. [Google Scholar]
- Jung, H. Validation of Food Frequency Questionnaire for Korea National Health and Nutrition Examination Survey; Korea Center for Diease Control and Prevention: Osong, Republic of Korea, 2010.
- Hwang, J.-Y.; Kim, Y.-H.; Lee, H.-S.; Park, E.-J.; Kim, J.-S.; Shin, S.-A.; Kim, K.-N.; Bae, Y.-J.; Kim, K.-R.; Woo, T.-J.; et al. The development of resources for the application of 2020 Dietary Reference Intakes for Koreans. J. Nutr. Health 2022, 55, 21–35. [Google Scholar] [CrossRef]
- Yun, S.H.; Shim, J.-S.; Kweon, S.; Oh, K. Development of a food frequency questionnaire for the Korea National Health and Nutrition Examination Survey: Data from the fourth Korea National Health and Nutrition Examination Survey (KNHANES IV). Korean J. Nutr. 2013, 46, 186–196. [Google Scholar] [CrossRef]
- Hong, H.-S.; Park, S.-J.; Lee, D.-K.; Lee, H.-J. Comparison of the portion sizes of Korean adults across eating places: Korea National Health and Nutrition Examination Survey (2012–2016). J. Nutr. Health 2020, 53, 676–687. [Google Scholar] [CrossRef]
- Tee, E.S.; Nurliyana, A.R.; Karim, N.A.; Jan Mohamed, H.J.B.; Tan, S.Y.; Appukutty, M.; Hopkins, S.; Thielecke, F.; Ong, M.K.; Ning, C. Breakfast consumption among Malaysian primary and secondary school children and relationship with body weight status-Findings from the MyBreakfast Study. Asia Pac. J. Clin. Nutr. 2018, 27, 421–432. [Google Scholar]
- Adolphus, K.; Lawton, C.L.; Dye, L. The relationship between habitual breakfast consumption frequency and academic performance in British adolescents. Front. Public Health 2015, 3, 68. [Google Scholar] [CrossRef]
- Levis, B.; Benedetti, A.; Thombs, B.D. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: Individual participant data meta-analysis. BMJ 2019, 365, 1476–1486. [Google Scholar] [CrossRef]
- Humeniuk, R.; Ali, R.; Babor, T.F.; Farrell, M.; Formigoni, M.L.; Jittiwutikarn, J.; De Lacerda, R.B.; Ling, W.; Marsden, J.; Monteiro, M. Validation of the alcohol, smoking and substance involvement screening test (ASSIST). Addiction 2008, 103, 1039–1047. [Google Scholar] [CrossRef]
- Cook, S.; Weitzman, M.; Auinger, P.; Nguyen, M.; Dietz, W.H. Prevalence of a metabolic syndrome phenotype in adolescents: Findings from the third National Health and Nutrition Examination Survey, 1988-1994. Arch. Pediatr. Adolesc. Med. 2003, 157, 821–827. [Google Scholar] [CrossRef]
- Oh, K.; Jang, M.J.; Lee, N.Y.; Moon, J.S.; Lee, C.G.; Yoo, M.H.; Kim, Y.T. Prevalence and trends in obesity among Korean children and adolescents in 1997 and 2005. Clin. Exp. Pediatr. 2008, 51, 950–955. [Google Scholar] [CrossRef]
- Lee, C.-G.; Moon, J.-S.; Choi, J.-M.; Nam, C.-M.; Lee, S.-Y.; Oh, K.-W.; Kim, Y.-T. Normative blood pressure references for Korean children and adolescents. Korean J. Pediatr. 2008, 51, 33–41. [Google Scholar] [CrossRef]
- World Health Organization. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment; Health Communications Australia: Sydney, Australia, 2000. [Google Scholar]
- Whooten, R.; Kerem, L.; Stanley, T. Physical activity in adolescents and children and relationship to metabolic health. Curr. Opin. Endocrinol. Diabetes Obes. 2019, 26, 25–31. [Google Scholar] [CrossRef]
- Stabelini Neto, A.; Sasaki, J.E.; Mascarenhas, L.P.; Boguszewski, M.C.; Bozza, R.; Ulbrich, A.Z.; da Silva, S.G.; de Campos, W. Physical activity, cardiorespiratory fitness, and metabolic syndrome in adolescents: A cross-sectional study. BMC Public Health 2011, 11, 674. [Google Scholar] [CrossRef]
- Oliveira, R.G.d.; Guedes, D.P. Physical activity, sedentary behavior, cardiorespiratory fitness and metabolic syndrome in adolescents: Systematic review and meta-analysis of observational evidence. PLoS ONE 2016, 11, e0168503–e0168526. [Google Scholar] [CrossRef]
- Stensvold, D.; Tjønna, A.E.; Skaug, E.-A.; Aspenes, S.; Stølen, T.; Wisløff, U.; Slørdahl, S.A. Strength training versus aerobic interval training to modify risk factors of metabolic syndrome. J. Appl. Physiol. 2010, 108, 804–810. [Google Scholar] [CrossRef]
- Choi, M.; Han, J.; Kim, Y.; Chung, J. The relationship between metabolic syndrome and smoking and alcohol experiences in adolescents from low-income households. Children 2021, 8, 812. [Google Scholar] [CrossRef] [PubMed]
- Ko, D.H.; Kim, Y.H.; Han, J.K. Relationship between cardiovascular disease risk factors, health behavior and physical fitness according to visceral fat in older men. J. Men’s. Health 2022, 18, 128. [Google Scholar] [CrossRef]
- Bakker, E.A.; Lee, D.-C.; Sui, X.; Artero, E.G.; Ruiz, J.R.; Eijsvogels, T.M.; Lavie, C.J.; Blair, S.N. Association of resistance exercise, independent of and combined with aerobic exercise, with the incidence of metabolic syndrome. Mayo Clin. Proc. 2017, 92, 1214–1222. [Google Scholar] [CrossRef] [PubMed]
- Castro-Piñero, J.; Laurson, K.R.; Artero, E.G.; Ortega, F.B.; Labayen, I.; Ruperez, A.I.; Zaqout, M.; Manios, Y.; Vanhelst, J.; Marcos, A. Muscle strength field-based tests to identify European adolescents at risk of metabolic syndrome: The HELENA study. J. Sci. Med. Sport 2019, 22, 929–934. [Google Scholar] [CrossRef]
- Cadenas-Sanchez, C.; Ruiz, J.R.; Labayen, I.; Huybrechts, I.; Manios, Y.; Gonzalez-Gross, M.; Breidenassel, C.; Kafatos, A.; De Henauw, S.; Vanhelst, J. Prevalence of metabolically healthy but overweight/obese phenotype and its association with sedentary time, physical activity, and fitness. J. Adolesc. Health 2017, 61, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Wennberg, M.; Gustafsson, P.E.; Wennberg, P.; Hammarström, A. Poor breakfast habits in adolescence predict the metabolic syndrome in adulthood. Public Health Nutr. 2015, 18, 122–129. [Google Scholar] [CrossRef]
- Smith, K.J.; Gall, S.L.; McNaughton, S.A.; Blizzard, L.; Dwyer, T.; Venn, A.J. Skipping breakfast: Longitudinal associations with cardiometabolic risk factors in the Childhood Determinants of Adult Health Study. Am. J. Clin. Nutr. 2010, 92, 1316–1325. [Google Scholar] [CrossRef]
- Karatzi, K.; Moschonis, G.; Barouti, A.-A.; Lionis, C.; Chrousos, G.P.; Manios, Y. Dietary patterns and breakfast consumption in relation to insulin resistance in children. The Healthy Growth Study. Public Health Nutr. 2014, 17, 2790–2797. [Google Scholar] [CrossRef] [PubMed]
- Salas-González, M.D.; Lozano-Estevan, M.d.C.; Aparicio, A.; Bermejo, L.M.; Loria-Kohen, V.; Ortega, R.M.; López-Sobaler, A.M. Breakfast Quality and Insulin Resistance in Spanish Schoolchildren: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 1181. [Google Scholar] [CrossRef]
- Witbracht, M.; Keim, N.L.; Forester, S.; Widaman, A.; Laugero, K. Female breakfast skippers display a disrupted cortisol rhythm and elevated blood pressure. Physiol. Behav. 2015, 140, 215–221. [Google Scholar] [CrossRef]
- Donnelly, S. Breakfast—The most important meal of the day. QJM 2018, 111, 681. [Google Scholar] [CrossRef] [PubMed]
- de la Hunty, A.; Gibson, S.; Ashwell, M. Does regular breakfast cereal consumption help children and adolescents stay slimmer? A systematic review and meta-analysis. Obes. Facts 2013, 6, 70–85. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, S.P.; Ramadas, A.; Fatt, Q.K.; Shin, H.L.; Onn, W.Y.; Kadir, K.A. Relationship of sociodemographic and lifestyle factors and diet habits with metabolic syndrome (MetS) among three ethnic groups of the Malaysian population. PLoS ONE 2020, 15, e0224054. [Google Scholar] [CrossRef] [PubMed]
- Lepe, A.; de Kroon, M.L.; Reijneveld, S.A.; de Winter, A.F. Socioeconomic inequalities in paediatric metabolic syndrome: Mediation by parental health literacy. Eur. J. Public Health 2023, 33, 179–183. [Google Scholar] [CrossRef]
- Blanquet, M.; Legrand, A.; Pélissier, A.; Mourgues, C. Socio-economics status and metabolic syndrome: A meta-analysis. Diabetes Metab. Syndr. 2019, 13, 1805–1812. [Google Scholar] [CrossRef]
- Jones, A. Race, socioeconomic status, and health during childhood: A longitudinal examination of racial/ethnic differences in parental socioeconomic timing and child obesity risk. Int. J. Environ. Res. Public Health 2018, 15, 728. [Google Scholar] [CrossRef]
- Kuo, W.C.; Bratzke, L.C.; Oakley, L.D.; Kuo, F.; Wang, H.; Brown, R.L. The association between psychological stress and metabolic syndrome: A systematic review and meta-analysis. Obes. Rev. 2019, 20, 1651–1664. [Google Scholar] [CrossRef]
- Ko, J.-K.; Han, K.-M.; Shin, C.; Lee, S.-H.; Han, C.; Kim, Y.-K.; Yoon, H.-K.; Ko, Y.-H. Association of metabolic syndrome and its components with suicidal ideation and depression in adults: A nationally representative sample of the Korean population. J. Affect. Disord. 2019, 249, 319–326. [Google Scholar] [CrossRef]

| Variables | Non-MetS (n = 1928) | MetS (n = 215) | t or 2 | p |
|---|---|---|---|---|
| Sex, boys/girls | 985 (51.1%)/943 (48.9%) | 128 (59.5%)/87 (40.5%) | 5.527 | 0.019 |
| Age, years | 15.4 ± 1.7 | 15.5 ± 1.7 | −0.943 | 0.346 |
| Height, cm | 166.1 ± 8.1 | 168.1 ± 8.5 | −3.444 | <0.001 |
| Weight, kg | 58.5 ± 11.9 | 79.9 ± 14.4 | −24.492 | <0.001 |
| BMI, kg/m2 | 21.1 ± 3.3 | 28.1 ± 4.0 | −28.740 | <0.001 |
| WC, cm | 71.3 ± 9.1 | 89.2 ± 10.3 | −27.179 | <0.001 |
| SBP, mmHg | 108.1 ± 9.5 | 118.0 ± 11.1 | −14.277 | <0.001 |
| DBP, mmHg | 67.5 ± 8.2 | 72.9 ± 9.2 | −8.970 | <0.001 |
| TG, mg/dL | 79.9 ± 39.0 | 148.8 ± 79.0 | −21.447 | <0.001 |
| HDLC, mg/dL | 52.4 ± 9.6 | 41.3 ± 6.4 | 16.490 | <0.001 |
| Glucose, mg/dL | 90.7 ± 7.1 | 96.9 ± 20.4 | −9.346 | <0.001 |
| Obesity, n | MHO 281 (14.6%) | MUO 163 (75.8%) | 441.623 | <0.001 |
| Normal weight, n | MHNW 1647 (85.4%) | MUNW 52 (24.2%) | ||
| PA attendance, n | 1925 (72.0%) | 134 (62.3%) | 8.796 | 0.003 |
| Household income, KW | 560.8 ± 311.2 | 522.1 ± 304.1 | 9.881 | 0.078 |
| Alcohol exp, n | 585 (30.3%) | 68 (31.6%) | 0.151 | 0.698 |
| Smoking exp, n | 200 (10.4%) | 23 (10.7%) | 0.022 | 0.906 |
| Variables | non-MetS (n = 1928) | MetS (n = 215) | 2 | p | OR |
|---|---|---|---|---|---|
| Sex | |||||
| boys (n = 1113) | 985 (88.5%) | 128 (11.5%) | 5.572 | 0.021 | Reference |
| girls (n = 1030) | 943 (91.6%) | 87 (8.4%) | 0.728 (0.546–0.972) | ||
| Social section | |||||
| Household income | |||||
| High | 1002 (52%) | 106 (49.3%) | 0.693 | 0.707 | Reference |
| Medium | 450 (23.3%) | 55 (25.6%) | 1.073 (0.721–1.596) | ||
| Low | 476 (24.7%) | 54 (25.1%) | 0.929 (0.658–1.313) | ||
| School | |||||
| Middle school | 997 (51.7%) | 95 (44.2%) | 4.384 | 0.036 | Reference |
| High school | 931 (48.3%) | 120 (55.8%) | 1.338 (1.001–1.789) | ||
| Mental section | |||||
| Depression | |||||
| No | 1773 (92.0%) | 188 (87.4%) | 5.082 | 0.024 | Reference |
| Yes | 155 (8.0%) | 27 (12.6%) | 1.640 (1.059–2.539) | ||
| Stress awareness | |||||
| None | 1407 (73.0%) | 149 (69.3%) | 1.612 | 0.447 | Reference |
| A little | 454 (23.5%) | 59 (27.4%) | 0.993 (0.447–2.203) | ||
| Max or Many | 67 (3.5%) | 7 (3.3%) | 1.230 (0.893–1.693) | ||
| Suicide ideation | |||||
| No | 1857 (96.3%) | 209 (97.2%) | 0.444 | 0.505 | Reference |
| Yes | 71 (3.7%) | 6 (2.8%) | 1.291 (0.553–3.016) |
| Variables | Non-MetS (n = 1928) | MetS (n = 215) | 2 | p | OR |
|---|---|---|---|---|---|
| PA section | |||||
| Aerobic PA | |||||
| High, 6–7 d/wk | 718 (37.2%) | 72 (33.5%) | 6.584 | 0.037 | Reference |
| Medium, 3–4 d/wk | 664 (34.4%) | 60 (27.9%) | 1.097 (0.626–3.016) | ||
| Low, 0–2 d/wk | 546 (28.3%) | 83 (38.6%) | 1.528 (1.092–2.203) | ||
| Strength training | |||||
| High, 4–7 d/wk | 360 (18.7%) | 33 (15.3%) | 1.579 | 0.454 | Reference |
| Medium, 2–3 d/wk | 389 (20.2%) | 48 (22.3%) | 1.336 (0.838–2.130) | ||
| Low, 0–1 d/wk | 1179 (61.2%) | 134 (62.3%) | 1.234 (0.828–1.839) | ||
| Sedentary time | |||||
| Low | 833 (43.2%) | 69 (32.1%) | 15.264 | <0.001 | Reference |
| Medium | 479 (24.8%) | 50 (23.3%) | 1.250 (0.853–1.832) | ||
| High | 616 (32.0%) | 96 (44.7%) | 1.863 (1.342–2.587) | ||
| Dietary section | |||||
| Energy intake | |||||
| Low | 613 (31.8%) | 58 (27.0%) | 7.337 | 0.026 | 1.013 (0.696–1.475) |
| Medium (recommend) | 643 (33.4%) | 62 (28.8%) | Reference | ||
| High | 672 (34.9%) | 95 (44.2%) | 1.466 (1.046–2.055) | ||
| Eating out frequency | |||||
| Low, ≤4 times/wk | 800 (41.5%) | 96 (44.7%) | 0.803 | 0.669 | Reference |
| Medium, 5–6 times/wk | 905 (46.9%) | 95 (44.2%) | 0.866 (0.642–1.169) | ||
| High, 1–2 time/day | 223 (11.6%) | 24 (11.2%) | 0.914 (0.570–1.467) | ||
| Weekly breakfast frequency | |||||
| High, 5–7 days/wk | 990 (51.3%) | 84 (39.1%) | 11.828 | 0.003 | Reference |
| Medium, 3–4 days/wk | 316 (16.4%) | 42 (19.5%) | 1.562 (1.055–2.314) | ||
| Low, 0–2 days/wk | 622 (32.3%) | 89 (41.4%) | 1.706 (1.244–2.339) | ||
| Nutrition education | |||||
| No | 1392 (72.2%) | 158 (73.5%) | 0.689 | 0.748 | Reference |
| Yes | 536 (27.8%) | 57 (26.5%) | 1.081 (0.785–1.488) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dou, X.; Kim, Y.; Chu, H. Prevalence of Metabolic Syndrome According to Physical Activity, Dietary Habits, Mental Status, Social Status, Health Behavior, and Obesity Phenotypes in Korean Adolescents: 2016–2021. Foods 2023, 12, 3304. https://doi.org/10.3390/foods12173304
Dou X, Kim Y, Chu H. Prevalence of Metabolic Syndrome According to Physical Activity, Dietary Habits, Mental Status, Social Status, Health Behavior, and Obesity Phenotypes in Korean Adolescents: 2016–2021. Foods. 2023; 12(17):3304. https://doi.org/10.3390/foods12173304
Chicago/Turabian StyleDou, Xiangxiang, Yonghwan Kim, and Hyunsik Chu. 2023. "Prevalence of Metabolic Syndrome According to Physical Activity, Dietary Habits, Mental Status, Social Status, Health Behavior, and Obesity Phenotypes in Korean Adolescents: 2016–2021" Foods 12, no. 17: 3304. https://doi.org/10.3390/foods12173304
APA StyleDou, X., Kim, Y., & Chu, H. (2023). Prevalence of Metabolic Syndrome According to Physical Activity, Dietary Habits, Mental Status, Social Status, Health Behavior, and Obesity Phenotypes in Korean Adolescents: 2016–2021. Foods, 12(17), 3304. https://doi.org/10.3390/foods12173304






