Salt-Related Knowledge, Attitudes and Behavior in an Intervention to Reduce Added Salt When Cooking in a Sample of Adults in Portugal
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Salt-Related Knowledge, Attitudes and Behavior
2.3. 24-h Urinary Sodium Excretion
2.4. 24-h Dietary Recall
2.5. Other Measures
2.6. Statistical Methods
3. Results
3.1. Baseline Data
3.2. 24-h Urinary Excretion and 24-h Dietary Recall
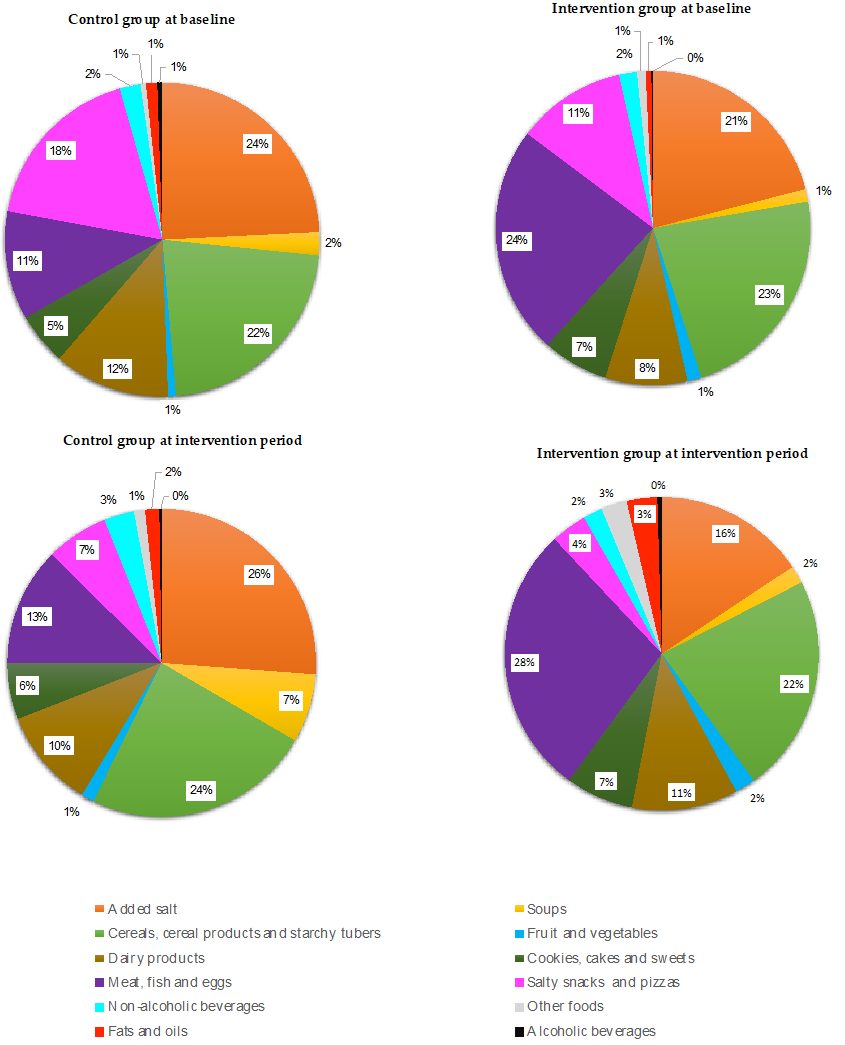
3.3. Sources of Salt Intake
3.4. Salt-Related Knowledge, Attitudes and Behavior
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Graudal, N.A.; Hubeck-Graudal, T.; Jurgens, G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst. Rev. 2011, 9, Cd004022. [Google Scholar] [CrossRef]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [Green Version]
- He, F.J.; MacGregor, G.A. Reducing population salt intake worldwide: From evidence to implementation. Prog. Cardiovasc. Dis. 2010, 52, 363–382. [Google Scholar] [CrossRef] [PubMed]
- Gauci, A.A.; Laaser, U. Intersalt: An International Study of Electrolyte Excretion and Blood Pressure. Results for 24 hour urinary sodium and potassium excretion. Intersalt Cooperative Research Group. BMJ 1988, 297, 319–328. [Google Scholar] [CrossRef] [Green Version]
- Zhou, B.F.; Stamler, J.; Dennis, B.; Moag-Stahlberg, A.; Okuda, N.; Robertson, C.; Zhao, L.; Chan, Q.; Elliott, P. Nutrient intakes of middle-aged men and women in China, Japan, United Kingdom, and United States in the late 1990s: The INTERMAP study. J. Hum. Hypertens. 2003, 17, 623–630. [Google Scholar] [CrossRef] [Green Version]
- Khaw, K.T.; Bingham, S.; Welch, A.; Luben, R.; O’Brien, E.; Wareham, N.; Day, N. Blood pressure and urinary sodium in men and women: The Norfolk Cohort of the European Prospective Investigation into Cancer (EPIC-Norfolk). Am. J. Clin. Nutr. 2004, 80, 1397–1403. [Google Scholar] [CrossRef]
- He, F.J.; Pombo-Rodrigues, S.; Macgregor, G.A. Salt reduction in England from 2003 to 2011: Its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open 2014, 4, e004549. [Google Scholar] [CrossRef] [Green Version]
- Karppanen, H.; Mervaala, E. Sodium intake and hypertension. Prog. Cardiovasc. Dis. 2006, 49, 59–75. [Google Scholar] [CrossRef]
- He, F.J.; Li, J.; Macgregor, G.A. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ 2013, 346, f1325. [Google Scholar] [CrossRef] [Green Version]
- Aburto, N.J.; Ziolkovska, A.; Hooper, L.; Elliott, P.; Cappuccio, F.P.; Meerpohl, J.J. Effect of lower sodium intake on health: Systematic review and meta-analyses. BMJ 2013, 346, f1326. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. WHO Guidelines Approved by the Guidelines Review Committee. In Guideline: Sodium Intake for Adults and Children; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- He, F.J.; Tan, M.; Ma, Y.; MacGregor, G.A. Salt Reduction to Prevent Hypertension and Cardiovascular Disease: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 75, 632–647. [Google Scholar] [CrossRef] [PubMed]
- Powles, J.; Fahimi, S.; Micha, R.; Khatibzadeh, S.; Shi, P.; Ezzati, M.; Engell, R.E.; Lim, S.S.; Danaei, G.; Mozaffarian, D. Global, regional and national sodium intakes in 1990 and 2010: A systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open 2013, 3, e003733. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turck, D.; Castenmiller, J.; de Henauw, S.; Hirsch-Ernst, K.I.; Kearney, J.; Knutsen, H.K.; Maciuk, A.; Mangelsdorf, I.; McArdle, H.J.; Pelaez, C.; et al. Dietary reference values for sodium. EFSA J. Eur. Food Saf. Auth. 2019, 17, e05778. [Google Scholar] [CrossRef] [Green Version]
- Bhat, S.; Marklund, M.; Henry, M.E.; Appel, L.J.; Croft, K.D.; Neal, B.; Wu, J.H.Y. A Systematic Review of the Sources of Dietary Salt Around the World. Adv. Nutr. 2020, 11, 677–686. [Google Scholar] [CrossRef] [PubMed]
- Lopes, C.; Torres, D.; Oliveira, A.; Severo, M.; Alarcão, V.; Guiomar, S.; Mota, J.; Teixeira, P.; Rodrigues, S.; Lobato, L.; et al. Inquérito Alimentar Nacional e de Atividade Física, IAN-AF 2015–2016—Relatório de Resultados. Available online: https://ian-af.up.pt/sites/default/files/IAN-AF%20Relatório%20Resultados_0.pdf (accessed on 19 January 2022).
- Trieu, K.; Neal, B.; Hawkes, C.; Dunford, E.; Campbell, N.; Rodriguez-Fernandez, R.; Legetic, B.; McLaren, L.; Barberio, A.; Webster, J. Salt Reduction Initiatives around the World—A Systematic Review of Progress towards the Global Target. PLoS ONE 2015, 10, e0130247. [Google Scholar] [CrossRef] [Green Version]
- Silva-Santos, T.; Moreira, P.; Rodrigues, M.; Padrão, P.; Pinho, O.; Norton, P.; Ndrio, A.; Gonçalves, C. Interventions That Successfully Reduced Adults Salt Intake—A Systematic Review. Nutrients 2021, 14, 6. [Google Scholar] [CrossRef]
- Yang, Y.; Wang, J.; Ma, J.; Shi, W.; Wu, J. Comparison of Salt-Related Knowledge and Behaviors Status of WeChat Users between 2019 and 2020. Nutrients 2021, 13, 2141. [Google Scholar] [CrossRef]
- Sparks, E.; Paterson, K.; Santos, J.A.; Trieu, K.; Hinge, N.; Tarivonda, L.; Snowdon, W.; Johnson, C.; Webster, J. Salt-Related Knowledge, Attitudes, and Behaviors on Efate Island, Vanuatu. Int. J. Environ. Res. Public Health 2019, 16, 1027. [Google Scholar] [CrossRef] [Green Version]
- Gonçalves, C.; Silva-Santos, T.; Abreu, S.; Padrão, P.; Graça, P.; Oliveira, L.; Esteves, S.; Norton, P.; Moreira, P.; Pinho, O. Innovative equipment to monitor and control salt usage when cooking at home: iMC SALT research protocol for a randomised controlled trial. BMJ Open 2020, 10, e035898. [Google Scholar] [CrossRef]
- Silva-Santos, T.; Moreira, P.; Pinho, O.; Padrão, P.; Abreu, S.; Esteves, S.; Oliveira, L.; Norton, P.; Rodrigues, M.; Ndrio, A.; et al. Impact of an Innovative Equipment to Monitor and Control Salt Usage during Cooking at Home on Salt Intake and Blood Pressure-Randomized Controlled Trial iMC SALT. Nutrients 2021, 14, 8. [Google Scholar] [CrossRef]
- Rodrigues, S.S.; Franchini, B.; Graça, P.; de Almeida, M.D. A new food guide for the Portuguese population: Development and technical considerations. J. Nutr. Educ. Behav. 2006, 38, 189–195. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. STEPS Instruments for NCD Risk Factors (Core and Expanded Version 1.4); World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Cardiovascular Disease and Alimentary Comparison (CARDIAC) Study Committee. CARDIAC Study Protocol and Manual of Operations; WHO Collaborating Center on Primary Prevention of Cardiovascular Diseases, and Cardiovascular Disease Unit: Shimane, Japan; Geneva, Switzerland, 1986. [Google Scholar]
- Campaniço, H. Validade Simultânea do Questionário Internacional de Actividade Física Através da Medição Objectiva da Actividade Física por Actigrafia Proporcional. Ph.D. Thesis, University of Lisbon, Lisbon, Portugal, 2016. [Google Scholar]
- Stewart, A.; Marfell-Jones, M.; Olds, T.; Ridder, H. International Standards for Anthropometric Assesment (2011); ISAK—International Society for the Advancement of Kinanthropometry: Wellington, New Zealand, 2016. [Google Scholar]
- Chaudhary, S.; Kumar, S.; Kaur, B.; Mehta, S.K. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ). RSC Adv. 2016, 6, 90526–90536. [Google Scholar] [CrossRef]
- Do, H.T.; Santos, J.A.; Trieu, K.; Petersen, K.; Le, M.B.; Lai, D.T.; Bauman, A.; Webster, J. Effectiveness of a Communication for Behavioral Impact (COMBI) Intervention to Reduce Salt Intake in a Vietnamese Province Based on Estimations From Spot Urine Samples. J. Clin. Hypertens. 2016, 18, 1135–1142. [Google Scholar] [CrossRef] [PubMed]
- Grimes, C.A.; Khokhar, D.; Bolton, K.A.; Trieu, K.; Potter, J.; Davidson, C.; Dunford, E.K.; Jan, S.; Woodward, M.; Bolam, B.; et al. Salt-Related Knowledge, Attitudes and Behaviors (KABs) among Victorian Adults Following 22-Months of a Consumer Awareness Campaign. Nutrients 2020, 12, 1216. [Google Scholar] [CrossRef] [PubMed]
- Wentzel-Viljoen, E.; Steyn, K.; Lombard, C.; De Villiers, A.; Charlton, K.; Frielinghaus, S.; Crickmore, C.; Mungal-Singh, V. Evaluation of a Mass-Media Campaign to Increase the Awareness of the Need to Reduce Discretionary Salt Use in the South African Population. Nutrients 2017, 9, 1238. [Google Scholar] [CrossRef] [Green Version]
- Magalhães, P.; Sanhangala, E.J.; Dombele, I.M.; Ulundo, H.S.; Capingana, D.P.; Silva, A.B. Knowledge, attitude and behaviour regarding dietary salt intake among medical students in Angola. Cardiovasc. J. Afr. 2015, 26, 57–62. [Google Scholar] [CrossRef] [Green Version]
- Cornélio, M.E.; Gallani, M.C.; Godin, G.; Rodrigues, R.C.; Nadruz, W., Jr.; Mendez, R.D. Behavioural determinants of salt consumption among hypertensive individuals. J. Hum. Nutr. Diet. Off. J. Br. Diet. Assoc. 2012, 25, 334–344. [Google Scholar] [CrossRef]
- McKenzie, B.; Santos, J.A.; Trieu, K.; Thout, S.R.; Johnson, C.; Arcand, J.; Webster, J.; McLean, R. The Science of Salt: A focused review on salt-related knowledge, attitudes and behaviors, and gender differences. J. Clin. Hypertens. 2018, 20, 850–866. [Google Scholar] [CrossRef] [Green Version]
- Mhurchu, C.N.; Gorton, D. Nutrition labels and claims in New Zealand and Australia: A review of use and understanding. Aust. N. Z. J. Public Health 2007, 31, 105–112. [Google Scholar] [CrossRef]
- Freedman, L.S.; Kipnis, V.; Schatzkin, A.; Tasevska, N.; Potischman, N. Can we use biomarkers in combination with self-reports to strengthen the analysis of nutritional epidemiologic studies? Epidemiol. Perspect. Innov. EP+I 2010, 7, 2. [Google Scholar] [CrossRef] [Green Version]
- Strauss-Kruger, M.; Wentzel-Viljoen, E.; Ware, L.J.; Van Zyl, T.; Charlton, K.; Ellis, S.; Schutte, A.E. Early evidence for the effectiveness of South Africa’s legislation on salt restriction in foods: The African-PREDICT study. J. Hum. Hypertens. 2022. [Google Scholar] [CrossRef] [PubMed]
- Land, M.A.; Webster, J.; Christoforou, A.; Johnson, C.; Trevena, H.; Hodgins, F.; Chalmers, J.; Woodward, M.; Barzi, F.; Smith, W.; et al. The association of knowledge, attitudes and behaviours related to salt with 24-hour urinary sodium excretion. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holbrook, J.T.; Patterson, K.Y.; Bodner, J.E.; Douglas, L.W.; Veillon, C.; Kelsay, J.L.; Mertz, W.; Smith, J.C., Jr. Sodium and potassium intake and balance in adults consuming self-selected diets. Am. J. Clin. Nutr. 1984, 40, 786–793. [Google Scholar] [CrossRef] [PubMed]
| Participants’ Characteristics | Total (n = 97) | Intervention Group (n = 48) | Control Group (n = 49) | p-Value 1 |
|---|---|---|---|---|
| Age (mean ± SD) | 48 ± 10 | 46 ± 10 | 50 ± 10 | 0.065 |
| Women n (%) | 51 (52.6) | 26 (54.2) | 25 (51.0) | 0.457 |
| Education n (%) | 0.393 | |||
| No higher education | 13 (13.4) | 5 (10.4) | 8 (16.3) | |
| Higher education | 84 (86.6) | 43 (89.6) | 41 (83.7) | |
| Marital Status n (%) | ||||
| Single | 17 (17.5) | 10 (20.8) | 7 (14.3) | 0.281 |
| Married | 66 (68.0) | 29 (60.4) | 37 (75.5) | |
| Divorced | 12 (12.4) | 7 (14.6) | 5 (10.2) | |
| Widow/er | 2 (2.1) | 2 (4.2) | 0 (0.0) | |
| Hypertensive n (%) | 39 (40.2) | 20 (41.7) | 19 (38.8) | 0.772 |
| Body mass index, kg/m2 (mean ± SD) | 25.9 ± 3.9 | 25.5 ± 3.9 | 26.2 ± 3.9 | 0.384 |
| Energy intake (kcal) (median [P25; P75]) | 2072 [1642; 2588] | 2041 [1664; 2597] | 2105 [1631; 2538] | 0.931 |
| Physical activity n (%) | ||||
| Low | 35 (36.1) | 16 (33.3) | 19 (38.8) | 0.846 |
| Moderate | 46 (47.4) | 24 (50.0) | 22 (44.9) | |
| High | 16 (16.5) | 8 (16.7) | 8 (16.3) |
| Descriptive Data | Baseline | Intervention | ||
|---|---|---|---|---|
| Urinary Excretion (mg/day) n = 80 | 24 h Food Recall (mg/day) n = 80 | Urinary Excretion (mg/day) n = 80 | 24 h Food Recall (mg/day) n = 80 | |
| Mean ± SD | 3186 ± 1231 | 3124 ± 1688 | 3131 ± 1221 | 3318 ± 1724 |
| Median | 3025 | 2670 | 3007 | 3185 |
| Minimum | 1219 | 569 | 667 | 600 |
| Maximum | 5957 | 8938 | 6946 | 10,753 |
| p-Value 1 | 0.204 | 0.514 | ||
| Knowledge, Attitudes and Behaviors Regarding Salt Intake | Intervention Group | Control Group | ||||
|---|---|---|---|---|---|---|
| Baseline | After Intervention | p-Value 1 | Baseline | After Intervention | p-Value 1 | |
| Behavior related to added salt | ||||||
| Add salt to food (often or always) (%) | 2.1 | 0.0 | 0.589 | 2.0 | 0.0 | 0.558 |
| Add salt while cooking (often or always) (%) | 93.7 | 81.2 | 0.037 | 91.8 | 85.7 | 0.078 |
| Consume processed foods high in salt (often or always) (%) | 37.5 | 31.3 | 0.221 | 38.7 | 24.5 | 0.119 |
| Knowledge and attitudes | ||||||
| Perceived salt consumption (too much or far too much) (%) | 14.6 | 27.1 | 0.142 | 16.3 | 12.2 | 0.432 |
| Importance of lowering salt in the diet (Not at all important) (%) | 10.4 | 4.2 | 0.617 | 6.1 | 4.1 | 0.405 |
| Agreed that too much salt could cause health problems (no) (%) | 2.1 | 10.4 | 0.250 | 2.0 | 6.1 | 0.625 |
| Behaviors to reduce salt | ||||||
| Avoid consuming processed foods (yes) (%) | 54.2 | 83.3 | 0.001 | 67.3 | 77.6 | 0.070 |
| Look at the salt labels on food (yes) (%) | 18.8 | 39.6 | 0.013 | 24.5 | 42.9 | 0.035 |
| Eat meals without adding salt at the table (yes) (%) | 87.5 | 91.7 | 0.687 | 95.9 | 89.8 | 0.687 |
| Buy low-salt alternatives (yes) (%) | 43.8 | 60.4 | 0.039 | 44.9 | 63.3 | 0.031 |
| Cook meals without adding salt (yes) (%) | 29.2 | 29.2 | 1.000 | 20.4 | 26.5 | 0.508 |
| Use spices other than salt when cooking (yes) (%) | 62.5 | 75.0 | 0.180 | 65.3 | 63.3 | 1.000 |
| Avoid eating out (yes) (%) | 35.4 | 54.2 | 0.064 | 49.0 | 65.3 | 0.039 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva-Santos, T.; Moreira, P.; Pinho, O.; Padrão, P.; Norton, P.; Gonçalves, C. Salt-Related Knowledge, Attitudes and Behavior in an Intervention to Reduce Added Salt When Cooking in a Sample of Adults in Portugal. Foods 2022, 11, 981. https://doi.org/10.3390/foods11070981
Silva-Santos T, Moreira P, Pinho O, Padrão P, Norton P, Gonçalves C. Salt-Related Knowledge, Attitudes and Behavior in an Intervention to Reduce Added Salt When Cooking in a Sample of Adults in Portugal. Foods. 2022; 11(7):981. https://doi.org/10.3390/foods11070981
Chicago/Turabian StyleSilva-Santos, Tânia, Pedro Moreira, Olívia Pinho, Patrícia Padrão, Pedro Norton, and Carla Gonçalves. 2022. "Salt-Related Knowledge, Attitudes and Behavior in an Intervention to Reduce Added Salt When Cooking in a Sample of Adults in Portugal" Foods 11, no. 7: 981. https://doi.org/10.3390/foods11070981
APA StyleSilva-Santos, T., Moreira, P., Pinho, O., Padrão, P., Norton, P., & Gonçalves, C. (2022). Salt-Related Knowledge, Attitudes and Behavior in an Intervention to Reduce Added Salt When Cooking in a Sample of Adults in Portugal. Foods, 11(7), 981. https://doi.org/10.3390/foods11070981








