Laser-Assisted Depigmentation—An Introspection of the Science, Techniques, and Perceptions
Abstract
1. Introduction
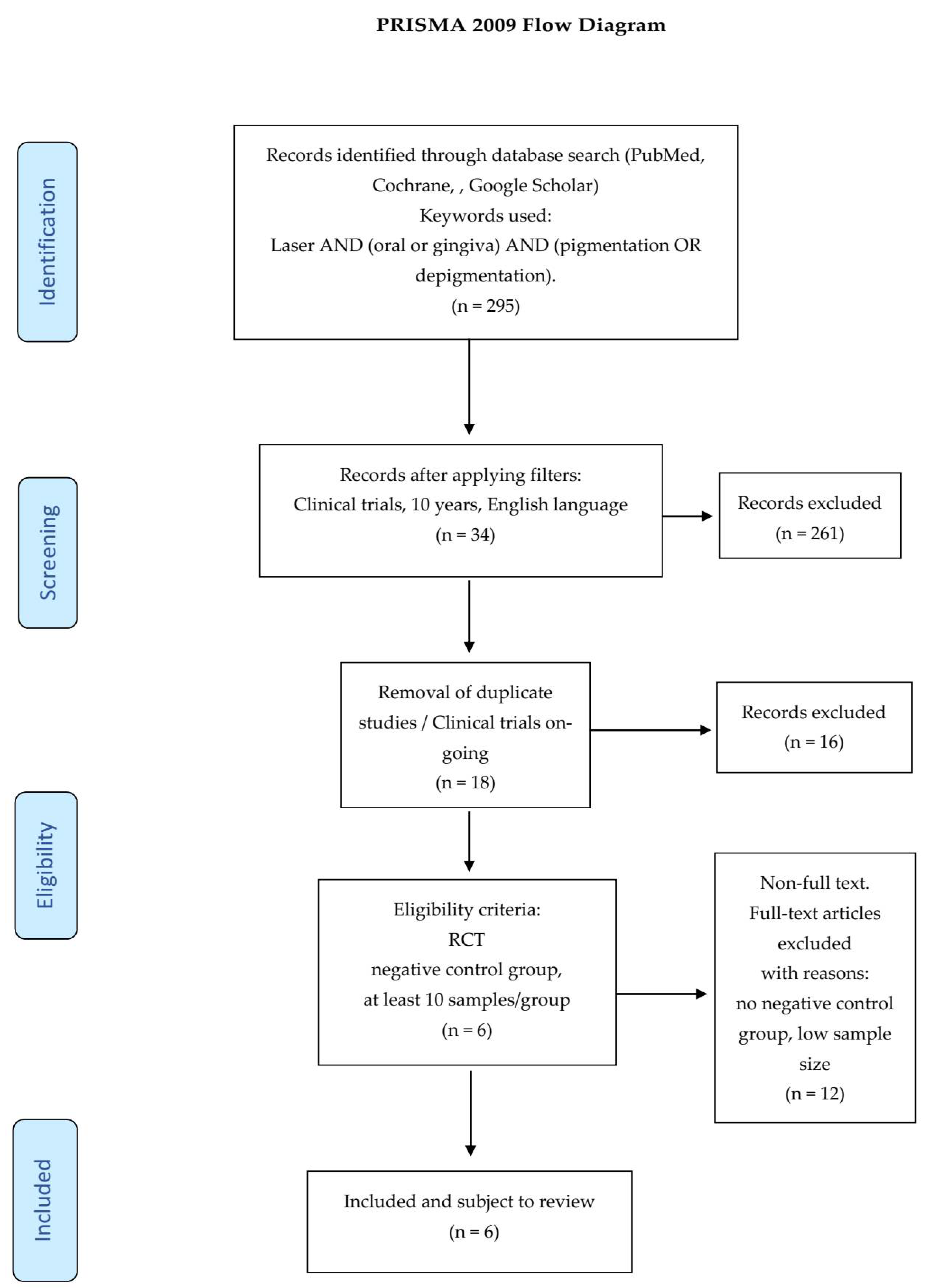
2. Materials and Methods
2.1. Search Strategy
- laser used as light source,
- at least 10 samples/patients per group,
- only randomized clinical trials and studies,
- a minimum of a 3 month follow-up.
- duplicates or studies with the same ethical approval number,
- no negative control group,
- low sample/patient sizes (less than 10 per group),
- no randomized controlled clinical trials or pilot studies,
- <3 month follow-up.
2.2. Data Extraction
- citation (first author and publication year),
- type of study/number of samples,
- test/control groups,
- follow-up,
- outcome.
2.3. Quality Assessment
- randomization,
- sample size calculation and required sample numbers included,
- baseline situation similar to that of the test group,
- blinding,
- parameters of laser use described appropriately and associated calculations correct,
- power meter used,
- numerical results available (statistics),
- no missing outcome data,
- all samples/patients completed the follow-up evaluation,
- correct interpretation of data acquired.
- High risk: 0–4,
- Moderate risk: 5–7,
- Low risk: 8–10.
3. Results
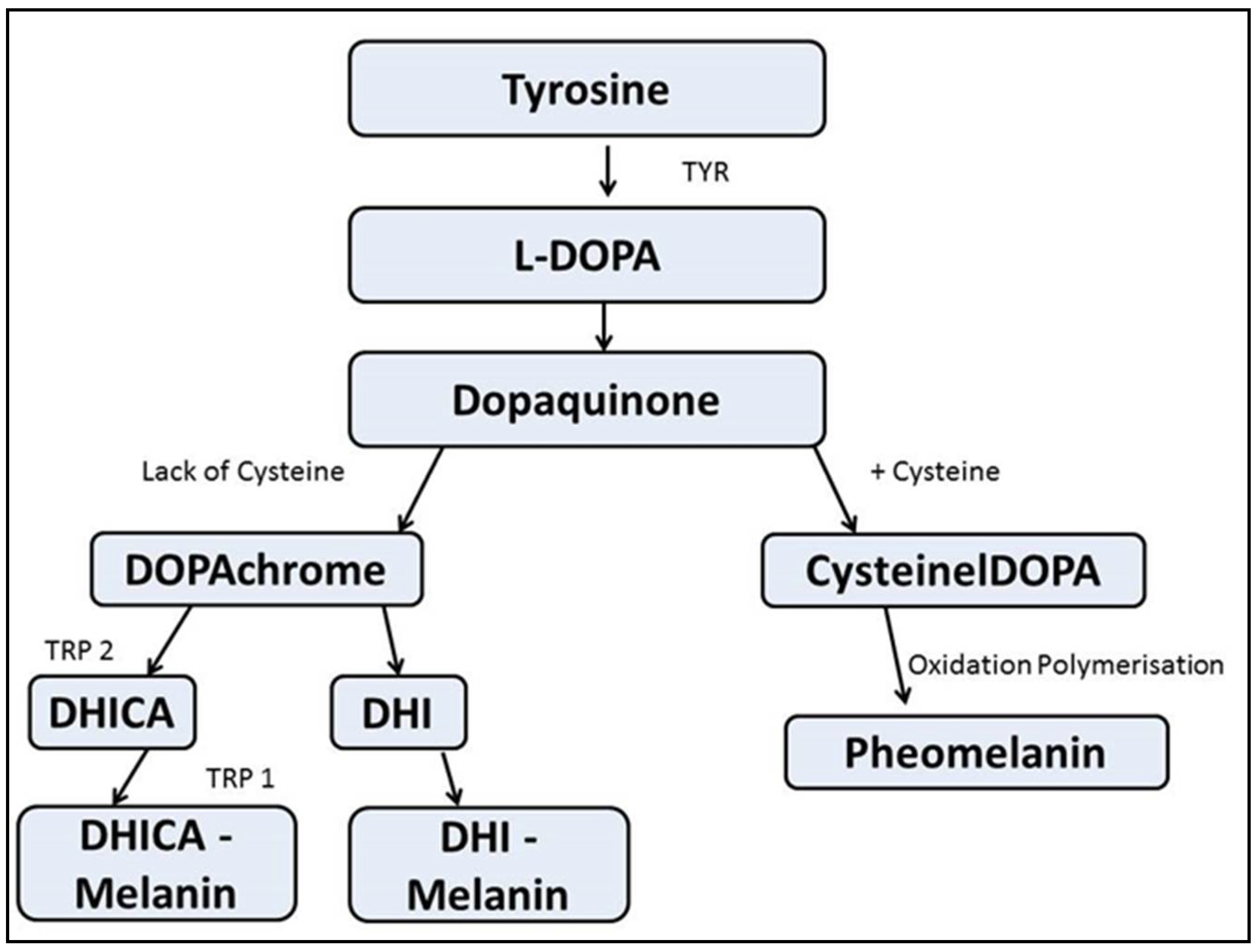
4. Discussion
4.1. Classification of Gingival Depigmentation Techniques
4.1.1. Topical Application (Chemical Cauterization)
4.1.2. Surgical Techniques
4.1.3. Electrosurgery
4.1.4. Lasers
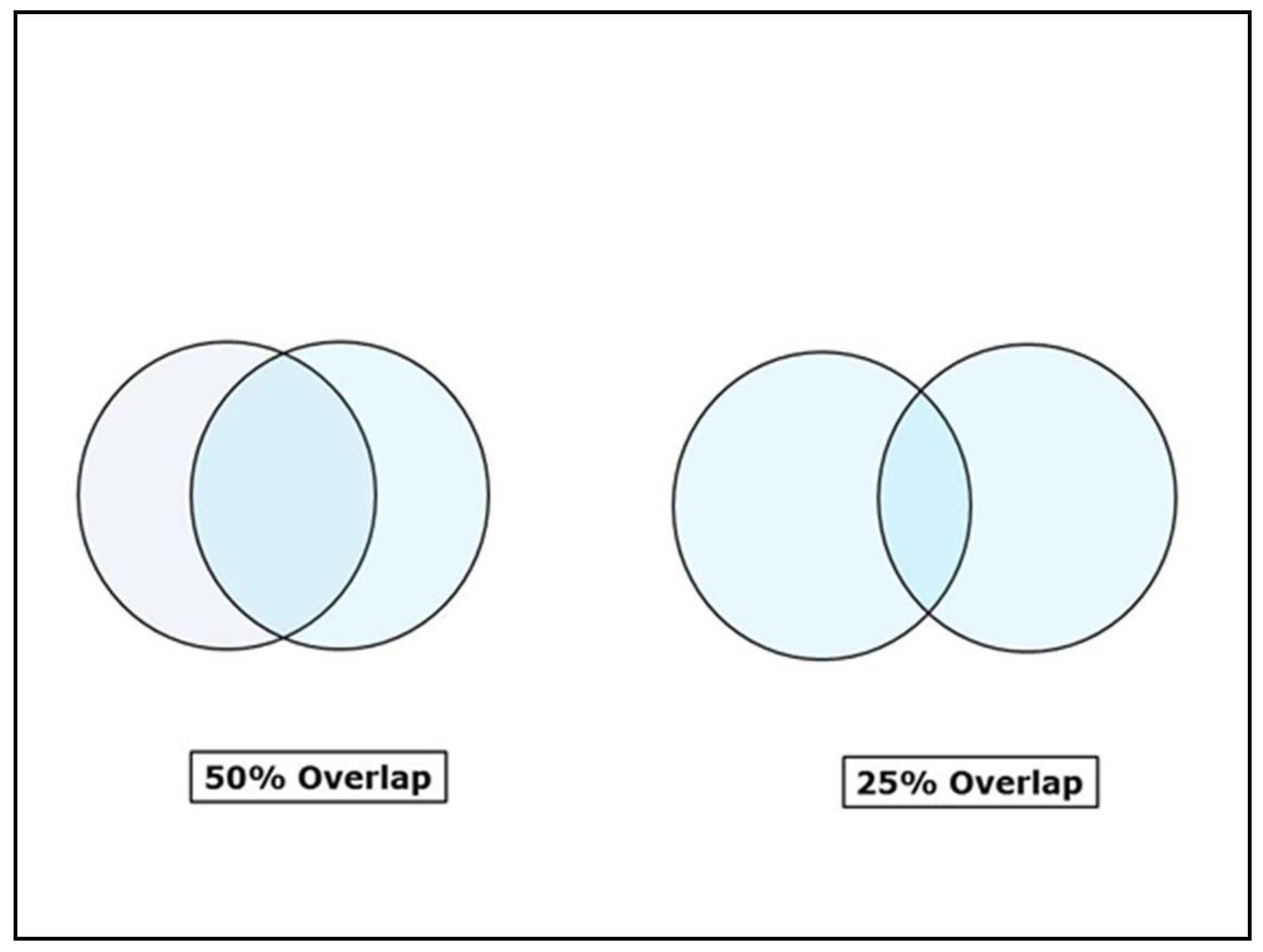
Contact Mode
Non-Contact Mode
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jones, J.; McFall, W.T., Jr. A photometric study of the color of healthy gingiva. J. Periodontol. 1977, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Dummett, C.O.; Gupta, O.M. Estimating the epidemiology of oral pigmentation. J. Dent. Res. 1964, 56, 419–420. [Google Scholar]
- Anderson, R.R.; Parrish, J.A. The optics of human skin. J. Investig. Dermatol. 1981, 77, 13–19. [Google Scholar] [CrossRef]
- Bleehen, S.S.; Anstey, A.V. Disorders of skin color. In Rook’s Text Book of Dermatology, 8th ed.; Burns, T., Breathnach, S., Eds.; Wiley-Blackwell: Hoboken, NJ, USA, 2013; pp. 1754–1767. [Google Scholar]
- Hirschfeld, I.; Hirschfeld, L. Oral pigmentation and method of removing it. Oral Surg. Oral. Med. Oral. Pathol. 1951, 4, 1012–1016. [Google Scholar] [CrossRef]
- Stasio, D.D.; Lauritano, D. Measurement of Oral Epithelial Thickness by Optical Coherence Tomography. Diagnostics 2019, 9, 90. [Google Scholar] [CrossRef]
- Nanci, A. Oral mucosa. In Ten Cate’s Oral histology, Development, Structure and Function, 9th ed.; Elsevier: Alpharetta, GA, USA, 2017; pp. 319–357. [Google Scholar]
- Briganti, S.; Camera, E. Chemical and instrumental approaches to treat hyperpigmentation. Pigment Cell Res. 2003, 16, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Hedin, C.A. Smokers melanosis. Arch Dermatol. 1977, 113, 1533–1538. [Google Scholar] [CrossRef]
- Peeran, S.; Ramalingam, K.; Peeran, S.; Altaher, O.; Alsaid, F.; Mugrabi, M. Gingival pigmentation index proposal of a new index with a brief review of current indices. Eur. J. Dent. 2014, 8, 287–290. [Google Scholar] [CrossRef]
- Jepson, S.; Caton, J.; Albandar, J.; Bissada, N.; Bouchard, P.; Cortellini, P.; Demirel, K.; Sanctis, M.; Ercoli, C.; Fan, J.; et al. Periodontal manifestations of systemic diseases and developmental and acquired conditions: Consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 45, S219–S222. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, T.P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement (Reprinted from Annals of Internal Medicine). PLoS Med. 2009, 6. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Basha, M.I.; Hegde, R.V. Comparison of Nd:YAG Laser and Surgical Stripping for Treatment of Gingival Hyperpigmentation: A Clinical Trial. Photomed. Laser Surg. 2015, 33, 424–436. [Google Scholar] [CrossRef] [PubMed]
- Chandra, G.B.; Vinay, K.M.B. Evaluation of surgical scalpel versus semiconductor diode laser techniques in the management of gingival melanin hyperpigmentation: A split-mouth randomized clinical comparative study. J. Indian Soc. Periodontol. 2020, 24, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Gholami, L.; Moghaddam, S.A. Comparison of gingival depigmentation with Er,Cr:YSGG laser and surgical stripping, a 12-month follow-up. Lasers Med. Sci. 2018, 33, 1647–1656. [Google Scholar] [CrossRef] [PubMed]
- Nammour, S.; El Mobadder, M. A Randomized Comparative Clinical Study to Evaluate the Longevity of Esthetic Results of Gingival Melanin Depigmentation Treatment Using Different Laser Wavelengths (Diode, CO2, and Er:YAG). Photomed. Las. Surg. 2020, 38, 167–173. [Google Scholar] [CrossRef]
- Ribeiro, F.V.; Cavaller, C.P. Esthetic treatment of gingival hyperpigmentation with Nd:YAG laser or scalpel technique: A 6-month RCT of patient and professional assessment. Lasers Med. Sci. 2014, 29, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Kaya, G.S.; Yapici, Y.G. A comparison of diode laser and Er:YAG lasers in the treatment of gingival melanin pigmentation. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2012, 113, 293–299. [Google Scholar] [CrossRef]
- Yamamoto, Y.; Yonei, N. Effect of chemical peeling on dental epithelial cells. J. Dermatol. Sci. 2004, 35, 158–161. [Google Scholar] [CrossRef]
- Tal, H.; Landsberg, J.; Kozlovsky, A. Cryosurgical depigmentation of the gingiva-a case report. J. Clin. Periodontol. 1987, 14, 614–617. [Google Scholar] [CrossRef]
- Yeh, C.J. Cryosurgical treatment of melanin pigmented gingiva. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 1988, 86, 660–663. [Google Scholar] [CrossRef]
- Patsakas, A.; Demetriou, N. Melanin pigmentation and inflammation in human gingiva. J. Periodontol. 1981, 52, 701–704. [Google Scholar] [CrossRef]
- Kumar, S.; Bhat, G.S. Effectiveness of cryogen tetrafluoroethane on elimination of gingival epithelium and its clinical application in gingival depigmentation-histological findings and case series. J. Clin. Diagn. Res. 2013, 7, 3070–3072. [Google Scholar]
- Brenner, M.; Hearing, V.J. Modifying skin pigmentation-Approaches through intrinsic biochemistry and exogenous agents. Drug Discov. Today Dis. Mech. 2008, 5, 189–199. [Google Scholar] [CrossRef] [PubMed]
- Shimada, Y.; Tai, H. Effects of Ascorbic Acid on Gingival Melanin Pigmentation In Vitro and In Vivo. J. Periodontol. 2009, 80, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Ginwalla, T.M.S.; Gomes, B.C. Surgical removal of gingival pigmentation (a preliminary study). J. Indian Dent. Assoc. 1966, 38, 147–150. [Google Scholar] [PubMed]
- Mokeem, S.A. Management of gingival hyperpigmentation by surgical abrasion–report of three cases. Saudi Dent. J. 2006, 18, 162–166. [Google Scholar]
- Almas, K.; Sadig, W. Surgical treatment of melanin–Pigmented gingiva; an esthetic approach. Indian J. Dent. Res. 2002, 13, 70–73. [Google Scholar]
- Dummett, C.O. Physiologic pigmentation of the oral and cutaneous tissues in the Negro. J. Dent. Res. 1946, 25, 421–432. [Google Scholar] [CrossRef]
- Perlmutter, S.; Tal, H. Repigmentation of the gingiva following surgical injury. J. Periodontol. 1986, 57, 48–50. [Google Scholar] [CrossRef]
- Bjorn, H. Free transplantation of gingiva propria. Sver. Tandlaekarefoerbunds Tidn. 1963, 55, 676–684. [Google Scholar]
- Takei, H.H.; Scheyer, E.T. Periodontal Plastic Surgery. In Carranza; Clinical Periodontology, 10th ed.; Newman, M.G., Takei, H.H., Eds.; Saunders Elsevier: Philadelphia, PA, USA, 2007; pp. 109–125. [Google Scholar]
- Tamizi, M.; Taheri, M.T. Treatment of severe physiologic gingival pigmentation with free gingival autograft. Quintessence Int. 1996, 27, 555–558. [Google Scholar] [PubMed]
- Dummett, C.O.; Bolden, T.E. Post-Surgical clinical repigmentation of the gingiva. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 1963, 16, 353–361. [Google Scholar] [CrossRef]
- Jayaprasad, K.; Vijaykumar, C. Case report: De-epthelization (a way to obtain esthetic smile). J. Indian Soc. Periodontol. 1999, 2, 98–100. [Google Scholar]
- Dey, S.M.; Nagarathna, D.V. Split Mouth Gingival Depigmentation with Scalpel and Diode Laser: A Comparative Study. IOSR J. Dent. Med. Sci. 2017, 16, 54–57. [Google Scholar] [CrossRef]
- Williams, V.D. Electrosurgery and wound healing: Review of the literature. J. Am. Dent. Assoc. 1984, 108, 220–222. [Google Scholar] [CrossRef]
- Sachdeva, S.; Dogra, A. Radiofrequency, ablation in dermatology. Ind. J. Dermatol. 2007, 52, 134–137. [Google Scholar] [CrossRef]
- Mutalik, S. Standard guidelines for electrosurgery with radiofrequency current. Ind. J. Dermatol. 2009, 75, S83–S100. [Google Scholar]
- Gufran, K.A. Comparative evaluation of two different techniques for esthetic management of gingival melanin hyperpigmentation: A clinical study. J. Dent. Res. Rev. 2016, 3, 13–16. [Google Scholar] [CrossRef]
- Prasad, D.; Sunil, S.; Mishra, R. Treatment of gingival pigmentation: A case series. Ind. J. Dent. Res. 2005, 16, 171–176. [Google Scholar]
- Sherman, J.A. Radiosurgery for Gingival Melanin Depigmentation. Dent. Today 2009, 28, 118–121. [Google Scholar]
- Riesz, J.J.; Gilmore, J.B. The transition dipole strength of melanin. Phys. Rev. 2007, 76, 021915. [Google Scholar]
- D’Alba, L.; Shawkey, M.D. Melanosomes: Biogenesis, Properties, And Evolution of An Ancient Organelle. Physiol. Rev. 2019, 99, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Duchon, J.; Borovansky, J. Chemical composition of ten kinds of various melanosomes. Pigment Cell Res. 1973, 1, 165. [Google Scholar]
- Trelles, M.A.; Verkruysse, W. Treatment of melanotic spots in the gingiva by argon laser. J. Oral. Maxillofac. Surg. 1993, 51, 759–761. [Google Scholar] [CrossRef]
- Atsawasuwan, P.; Greethong, K. Treatment of Gingival Hyperpigmentation for Esthetic Purposes by Nd:YAG Laser: Report of 4 Cases. J. Periodontol. 2000, 71, 315–321. [Google Scholar] [CrossRef]
- Chandna, S.; Kedige, S.D. Evaluation of pain on use of electrosurgery and diode lasers in the management of gingival hyperpigmentation: A comparative study. J. Indian Soc. Periodontol. 2015, 19, 49–55. [Google Scholar] [CrossRef]
- Raaman, A.R.; Pratebha, B. Comparison of efficacy of depigmentation of gingiva in terms of ImageJ intensity values and surface area of repigmentation using scalpel and diode laser. Int. J. Oral. Health Sci. 2016, 6, 59–64. [Google Scholar]
- Balagué, C. Hemostasis and technology. Energy. Development of new technologies. Cir. Esp. 2009, 85, 15–22. [Google Scholar] [CrossRef]
- Luk, K.; Anagnostaki, E. Impact of laser dentistry in management of color in aesthetic zone. In Lasers in Dentistry—Current Concepts; Coluzzi, D.J., Steven, P.A.P., Eds.; Springer: Berlin, Germany, 2017; pp. 337–356. [Google Scholar]
- Manal, M.; Azzeh, T. Treatment of Gingival Hyperpigmentation by Erbium-Doped:Yttrium, Aluminum, and Garnet Laser for Esthetic Purposes. J. Periodontol. 2007, 78, 177–184. [Google Scholar]
- Cobb, C.M. Lasers in Periodontics: A Review of the Literature. J. Periodontol. 2006, 77, 545–564. [Google Scholar] [CrossRef]
- Tal, H.; Oegiesser, D. Gingival depigmentation by Erbium:YAG laser: Clinical observations and patient responses. J. Periodontol. 2003, 74, 1660–1667. [Google Scholar] [CrossRef] [PubMed]
- Rosa, D.S.A.; Aranha, A.C.C. Esthetic Treatment of Gingival Melanin Hyperpigmentation with Er:YAG Laser: Short-Term Clinical Observations and Patient Follow-Up. J. Periodontol. 2007, 78, 2018–2025. [Google Scholar] [CrossRef]
- Hegde, R.; Padhye, A. Comparison of surgical stripping; erbium-doped:yttrium, aluminum, and garnet laser; and carbon dioxide laser techniques for gingival depigmentation: A clinical and histologic study. J. Periodontol. 2013, 84, 738–748. [Google Scholar] [CrossRef] [PubMed]
- Ozbayrak, S.; Dumlu, A. Treatment of melanin–Pigmented gingiva and oral mucosa by CO2 laser. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2000, 90, 14–15. [Google Scholar] [CrossRef] [PubMed]
- Hedin, C.A.; Axell, T. Oral melanin pigmentation in 467 Thai and Malaysian people with special emphasis on smokers melanosis. J. Oral. Pathol. Med. 1991, 20, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Yerger, V.; Malone, R. Melanin and nicotine: A review of the literature. Nicotine Tob. Res. 2006, 8, 487–498. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cicek, Y.; Ertas, U. The normal and pathological pigmentation of oral mucous membrane: A review. J. Contemp. Dent. Pract. 2003, 15, 76–86. [Google Scholar]
- Natali, C.; Curtis, J.L.; Suarez, L.; Millman, E.J. Oral mucosa pigment changes in heavy drinkers and smokers. J. Nat. Med. Assoc. 1991, 83, 434–438. [Google Scholar]
- Haresaku, S.; Hanioka, T.A. Association of lip pigmentation with smoking and gingival melanin pigmentation. J. Oral. Dis. 2007, 13, 71–76. [Google Scholar] [CrossRef]
- Nakamura, Y.; Funato, A. A study on the removal of the melanin pigmentation of dog gingiva by CO2 laser irradiation. J. Clin. Laser Med. Surg. 1992, 10, 41–46. [Google Scholar] [CrossRef]
- Nakamura, Y.; Hossain, M. A clinical study on the removal of gingival melanin pigmentation with the CO2 laser. Lasers Surg. Med. 1999, 25, 140–147. [Google Scholar] [CrossRef]
- Johnson, M.A.; Gadacz, T.R.; Pfeifer, E.A. Comparison of CO2 Laser, Electrosurgery and Scalpel incisions on acute–Phase reactants in rat skin. Am. Surg. 1997, 63, 13–16. [Google Scholar] [PubMed]
- Esen, E.; Haytac, M.C. Gingival melanin pigmentation and its treatment with the CO2 laser. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2004, 98, 522–527. [Google Scholar] [CrossRef] [PubMed]
- Coleton, S. Lasers in surgical periodontics and oral medicine. Dent. Clin. N. Am. 2004, 48, 937–962. [Google Scholar] [CrossRef] [PubMed]
- Land, H.Z. Melanotic tumors in the skin. In Atlas of Tumor Pathology, Armed Forces Institute of Pathology; Wash: 6825 16th St NW #54; American Registry of Pathology Publication & Education: Washington, DC, USA, 1962; p. 29. [Google Scholar]
- Kumarswamy, A. Beauty is indeed skin deep. Ann. Plast. Surg. 1980, 4, 462–468. [Google Scholar]
- Meleti, M.; Vescovi, P. Pigmented lesions of the oral mucosa and perioral tissues: A flow-chart for the diagnosis and some recommendations for the management. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2008, 105, 606–616. [Google Scholar] [CrossRef]
- Bayindir, F.; Bayindir, Y.Z. Coverage error of gingival shade guide systems in measuring color of attached anterior gingiva. J. Prosthet. Dent. 2009, 101, 46–53. [Google Scholar] [CrossRef]









| Dummett-Gupta Oral Pigmentation Index (DOPI) | |
|---|---|
| Score | Scale of Pigmentation |
| 0 | 1. Pink–no pigmentation |
| 1 | 2. Light Brown–mild pigmentation |
| 2 | 3. Mixed Pink and Brown or Medium Brown |
| 3 | 4. Deep Brown–Blackish Brown |
| Hedin’s Classification | |
|---|---|
| Score | Scale of Pigmentation |
| Degree 1 | Isolated—only 1 or 2 pigmented interdental papillae |
| Degree 2 | Numerous pigmented interdental papillae |
| Degree 3 | Short continuous ribbons |
| Degree 4 | Long continuous ribbon |
| Pigmented Lesions Index | Proposed Gingival Melanin Pigmentation |
|---|---|
| Score 0 | Coral pink-colored gingiva, no gingival pigmentation, and/or pigmented lesions |
| Score 1 | Mild, solitary/diffuse, gingival melanin pigmentation involving anterior gingiva, with or without the involvement of posterior gingiva |
| Score 2 | Moderate to severe, solitary or diffuse, gingival melanin pigmentation involving anterior gingiva with or without the involvement of posterior gingiva |
| Score 3 | Gingival melanin pigmentation only in posterior gingiva |
| Score 4 | Tobacco-associated pigmentation: smoker’s melanosis, chewing tobacco |
| Score 5 | Gingival pigmentation due to exogenous pigments: amalgam tattoos arsenic, bismuth, hewing betel nut, cultural gingival tattooing, drinks, food colors, lead-Burtonian line, mercury, silver, topical medications, idiopathic, etc. |
| Score 6 | Gingival pigmentation due to other endogenous pigments: bilirubin, blood breakdown products, ecchymosis, hemochromatosis, hemosiderin, petechiae, etc. |
| Score 7 | Drug-associated gingival pigmentation: antimalarial drugs, minocycline, oral contraceptives, etc. |
| Score 8 | Gingival pigmentation associated with other causes: Addison’s disease, Albright’s syndrome, basilar melanosis with incontinence, hereditary hemorrhagic telangiectasia, HIV patients, lichen planus, neurofibromatosis, Peutz–Jeghers syndrome, pyogenic granuloma/granulomatous epulis, etc. |
| Score 9 | Pigmented benign lesions: hemangioma, melanocytic nevus, pigmented macule |
| Score 10 | Pigmented malignant lesions: angiosarcoma, Kaposi’s sarcoma, malignant melanoma |
| Citation [ref] | Type of Study/Number of Samples/Pocket Depth | Test/Control Groups | Laser Used | Scoring Used | Follow-up | Outcome |
|---|---|---|---|---|---|---|
| Basha et al. 2015 [14] | Clinical trial 20 patients 40 sites. Both sexes, 18–38 years Randomized, SB, comparative, split-mouth, clinical trial | Gr (i) Surgical stripping Gr (ii) laser | Nd:YAG 1064 nm Av Power 3.0 W 30 mj/pp 100 Hz Contact mode | Dummett Oral Pigmentation Index (DOPI) for intensity of pigmentation, Hedin Melanin Index for extent of pigmented area. VAS pain | 6 months | Nd:YAG laser can be used as an alternative technique for gingival depigmentation No statistical significance for all results. Time with laser significantly less (p = 0.05) |
| Chandra et al. 2020 [15] | Split-mouth RCT. DB. 20 patients | Gr (i) Surgical stripping Gr (ii) laser | Diode 810 nm 1.5–2.0 W CW. Contact mode | Plaque and gingival index, bleeding, pain perception, wound healing, recurrence, and intensity of repigmentation (DOPI) were evaluated | No recurrence at 9 months were followed even up to 3 years. | Surgical scalpel technique remained as the “gold standard” procedure for treatment. Bleeding significantly less for laser (p = 0.05). No significant difference otherwise. |
| Gholami 2018 [16] | RCT DB 22 patients 66 sites | Gr (i) Laser 4.5 W Gr (ii) 2.5 W Gr (iii) Blade | Er,Cr:YSGG 2780 nm G. (i) 4.5 W, 50 Hz, 60 μs pulse, air, water G. (ii) 2.5 W, 50 Hz, 700 μs pulse, air, water | Bleeding, pain perception, wound healing, recurrence, and intensity of repigmentation (DOPI) were evaluated | 1 month 12 months | Patient satisfaction/bleeding significantly better with laser (p = 0.05). Healing not statistically significant. |
| Nammour 2020 [17] | RC Study DB 72 patients | 6 groups – 3 smokers/3 non-smokers | Diode 980 nm 1.5 W 50 Hz, fiber diameter 0.3 mm F = 21.22 J/cm2. Contact mode Er:YAG 2940 nm 5.0 W/20 Hz, 250 mJ, F = 39.31 J/cm2. Non-contact mode CO2 10,600 nm. 1.5 W SP 40 Hz, beam dia 0.3 mm, F = 17 J/cm2. Non-contact mode | Hedin Melanin Index (HMI) was used | 2 weeks to 60 months All measured values within significance (p = 0.05). | Diode laser provides the longest-term stability in treatment. Smoking negatively affects the longevity of GD. Er laser gives the shortest time before the reappearance of gingival pigmentation. |
| Ribeiro 2014 [18] | Split-mouth RCT. DB. 11 patients | Gr. (i) Laser Gr. (ii) scalpel Random blinded determined operating side | Nd:YAG 6 W, 60 mJ/pulse, 100 Hz Contact mode | VAS Digitized photograph pixel count. | 7, 15 days, 3, 6 months Significant differences in more pain, better patient acceptance (p = 0.05). | Nd:YAG laser has advantages in terms of less discomfort/ pain during the post-therapy period and a reduction of treatment chair time. |
| Simsek Kaya 2012 [19] | Randomized prospective study 20 patients 13 F, 7 M | Gr. (i) Diode 810 nm Gr. (ii) Er:YAG | Diode 810 nm 1.0 W CW Contact mode Er:YAG 2940 nm Av. Power 1.0 W Non-contact mode | Melzack’s McGill Pain Questionnaire Digitized photograph pixel count | Average pain scores: diode 1.5; Er:YAG 1.0 FU 7 days, 10–14 months. | Diode and Er:YAG lasers administered at 1 W both result in satisfactory depigmentation of GMP (p = 0.05) Diode surgically Quicker than Er:YAG (p = 0.05). |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muruppel, A.M.; Pai, B.S.J.; Bhat, S.; Parker, S.; Lynch, E. Laser-Assisted Depigmentation—An Introspection of the Science, Techniques, and Perceptions. Dent. J. 2020, 8, 88. https://doi.org/10.3390/dj8030088
Muruppel AM, Pai BSJ, Bhat S, Parker S, Lynch E. Laser-Assisted Depigmentation—An Introspection of the Science, Techniques, and Perceptions. Dentistry Journal. 2020; 8(3):88. https://doi.org/10.3390/dj8030088
Chicago/Turabian StyleMuruppel, Alex Mathews, B.S. Jagadish Pai, Subraya Bhat, Steven Parker, and Edward Lynch. 2020. "Laser-Assisted Depigmentation—An Introspection of the Science, Techniques, and Perceptions" Dentistry Journal 8, no. 3: 88. https://doi.org/10.3390/dj8030088
APA StyleMuruppel, A. M., Pai, B. S. J., Bhat, S., Parker, S., & Lynch, E. (2020). Laser-Assisted Depigmentation—An Introspection of the Science, Techniques, and Perceptions. Dentistry Journal, 8(3), 88. https://doi.org/10.3390/dj8030088





