Bond Strength of an Epoxy Resin Root Canal Sealer Prototype
Abstract
1. Introduction
2. Materials and Methods
2.1. Preliminary Tests
2.1.1. Investigation of Storage Time on Bond Strength
- Single root canal without isthmuses or branches;
- Straight root canal;
- Mature apex;
- No caries or at least the lowest possible degree of destruction;
- Radiographically suitable canal shape;
- Initial canal dimension and shape smaller than the dimension of final file.
2.1.2. Preparation of the Access Cavity and Root Canal Preparation
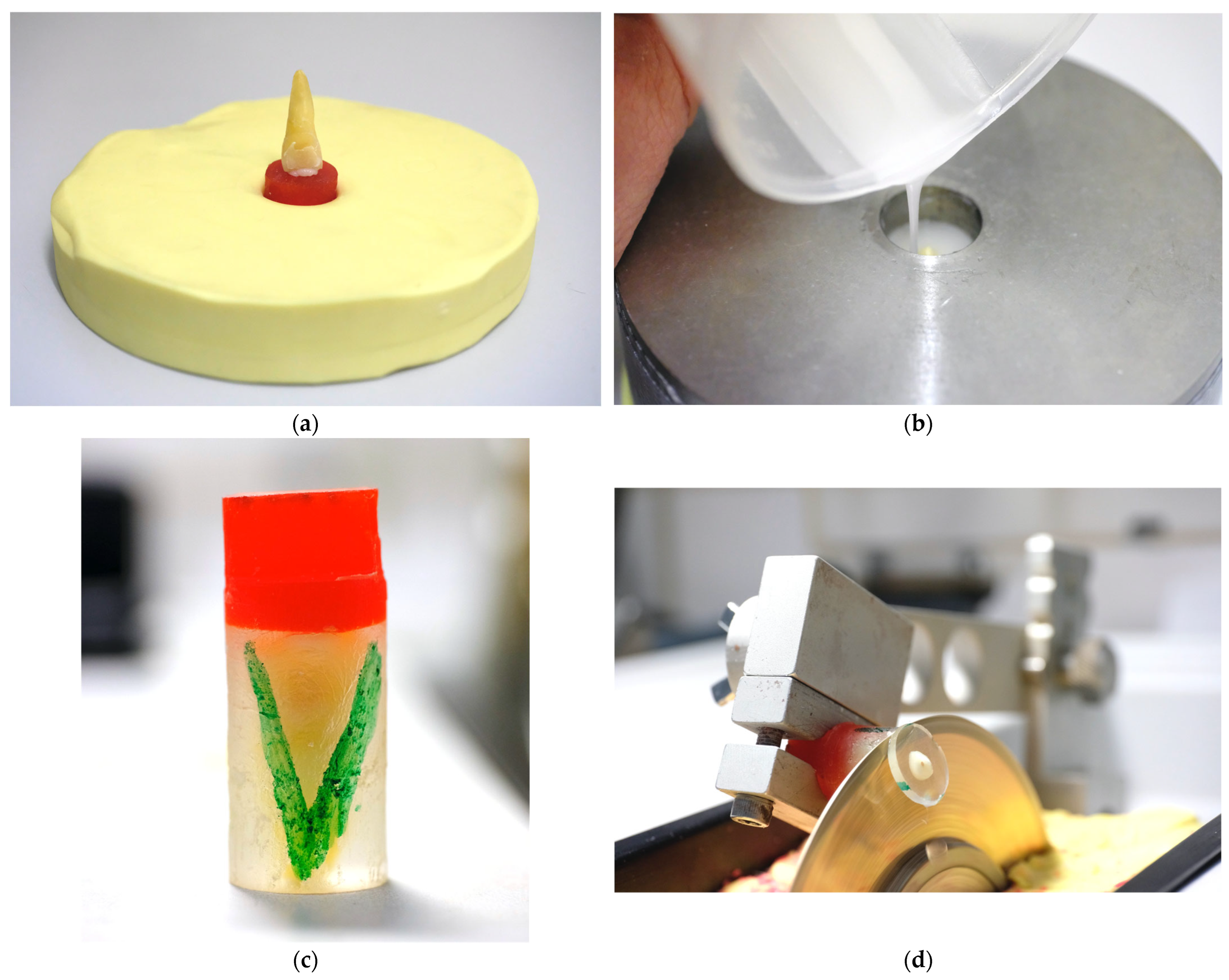
2.1.3. Embedding of the Specimens and Investigation of Generated Temperatures During the Embedding and Cutting Process
2.2. Main Investigation
2.2.1. Access Cavity, Instrumentation, Irrigation, Activation, and Drying of the Root Canals
2.2.2. Obturation and Sealing of the Access Cavity
2.2.3. Specimen Embedding
2.2.4. Cutting Process
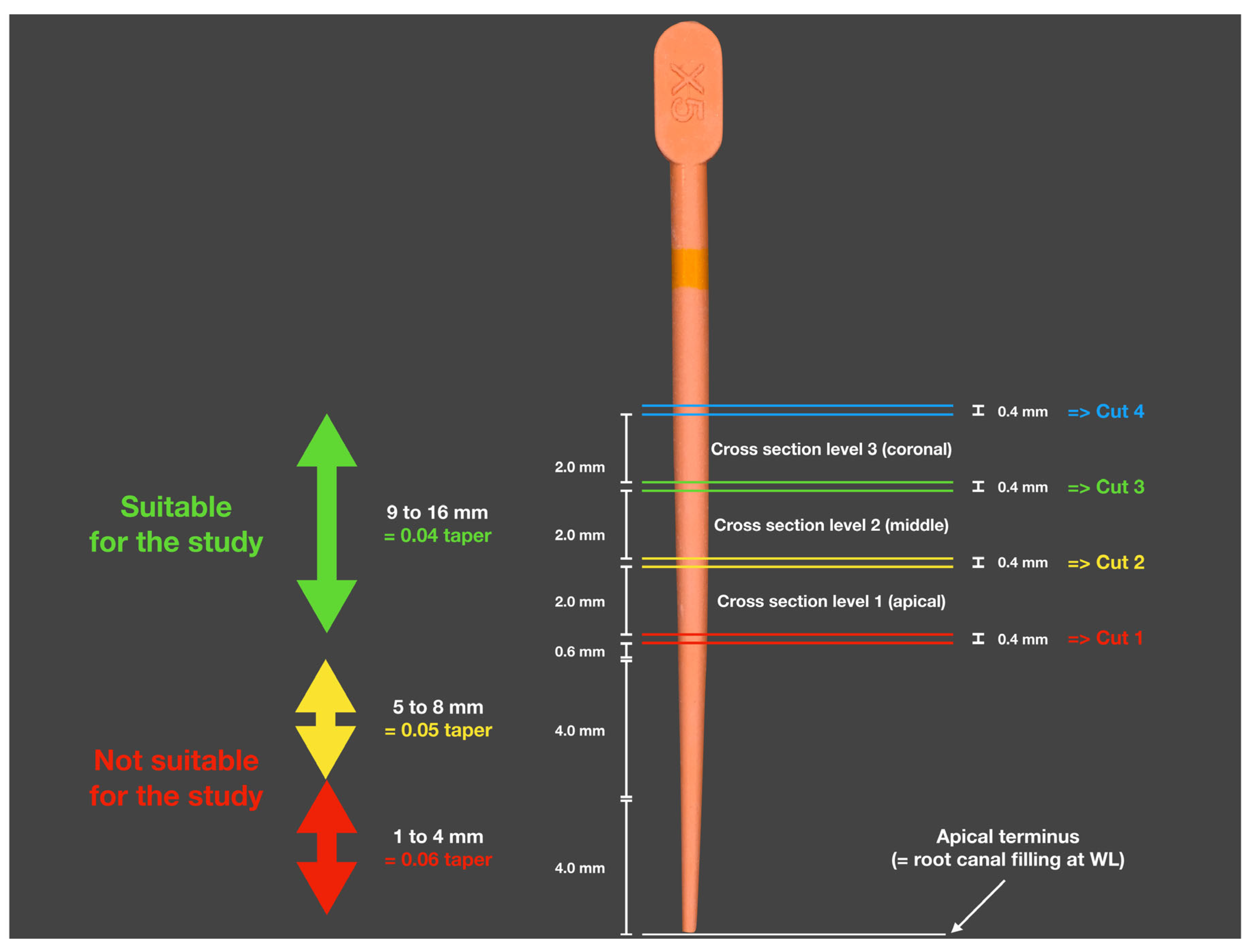
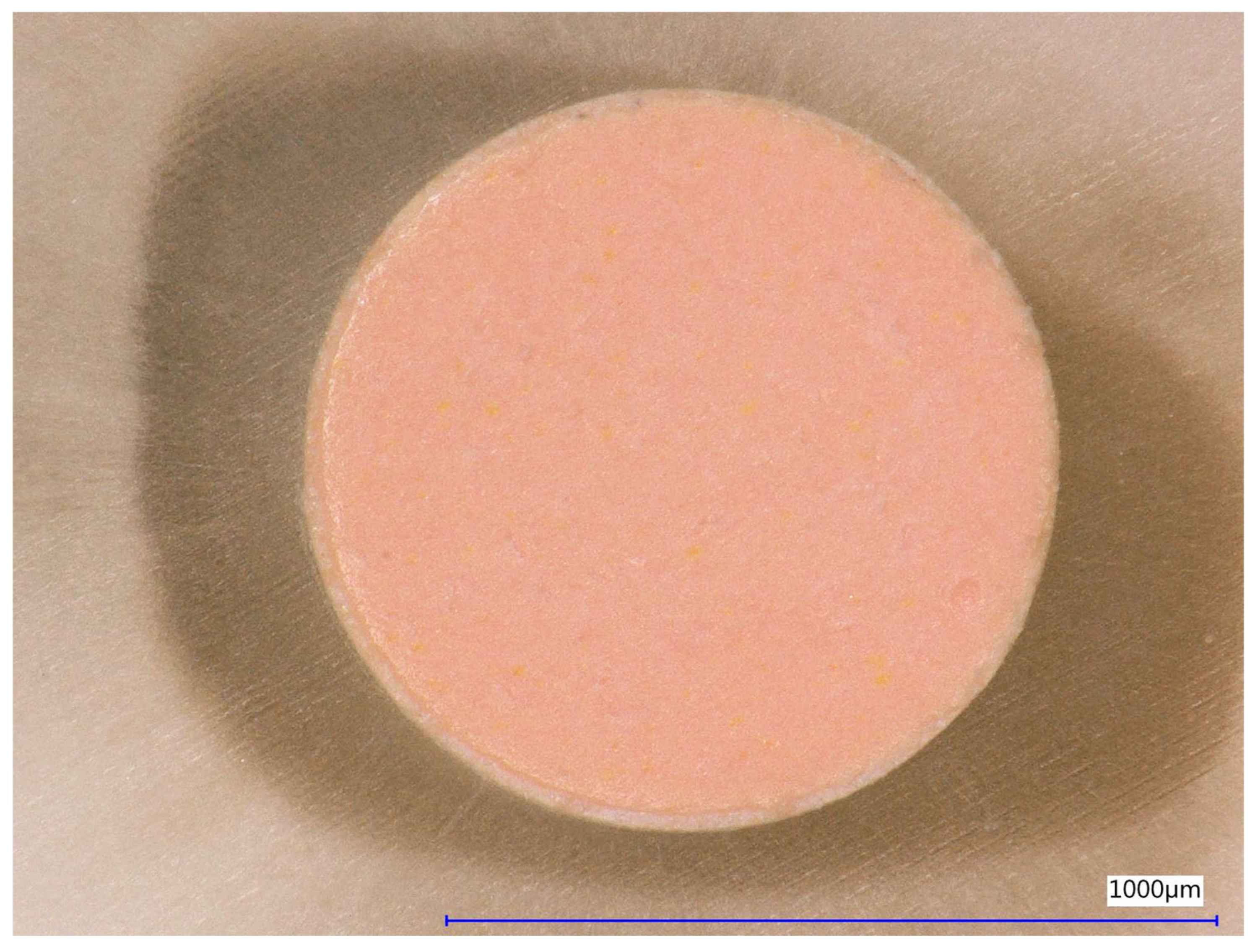
2.2.5. Analysis of the Diameters of Root Canal Fillings
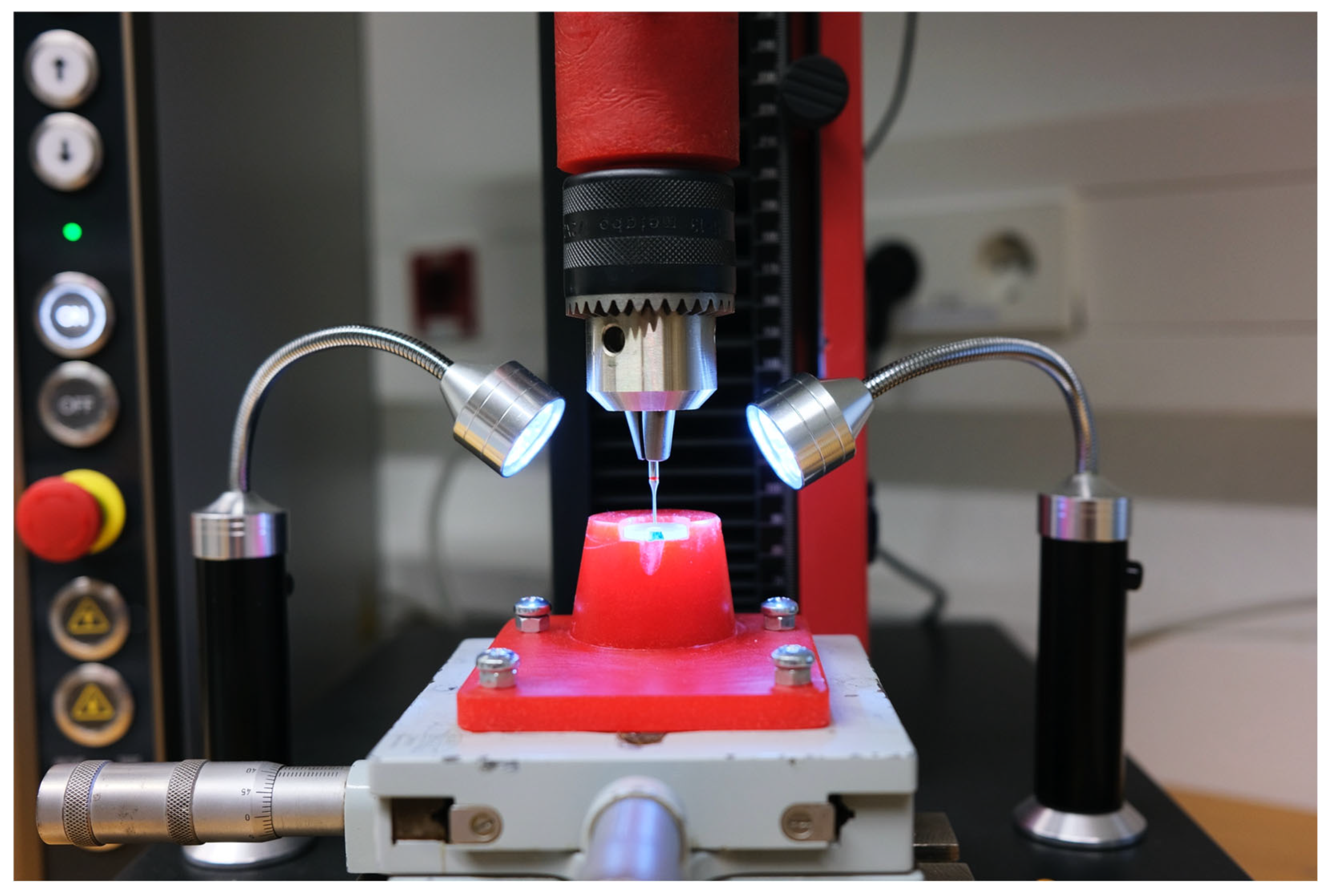
2.2.6. Preparation and Implementation of the Bond Strength Analysis
2.2.7. Manufacturing of Customized Holders for Push-Out Analysis
2.2.8. Performing Fractographic Analysis
2.2.9. Statistical Evaluation
3. Results
3.1. Preliminary Study Results
3.1.1. Effect of Storage Time on Pull-Out Bond Strength
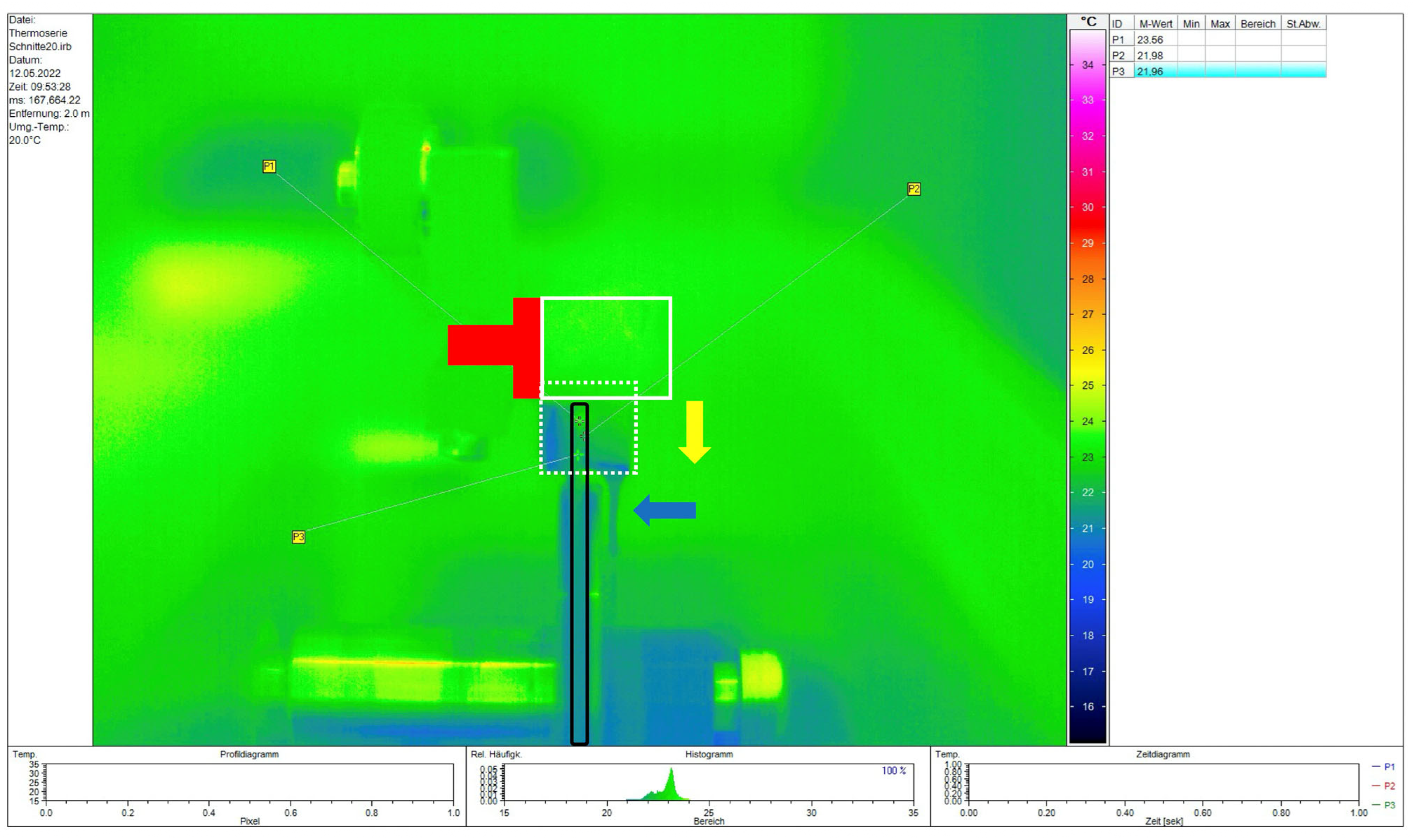
3.1.2. Temperatures Generated During Embedding and Sectioning of the Specimens
3.2. Main Study Results
3.3. Non-Parametric Analysis of the Bond Strength Values
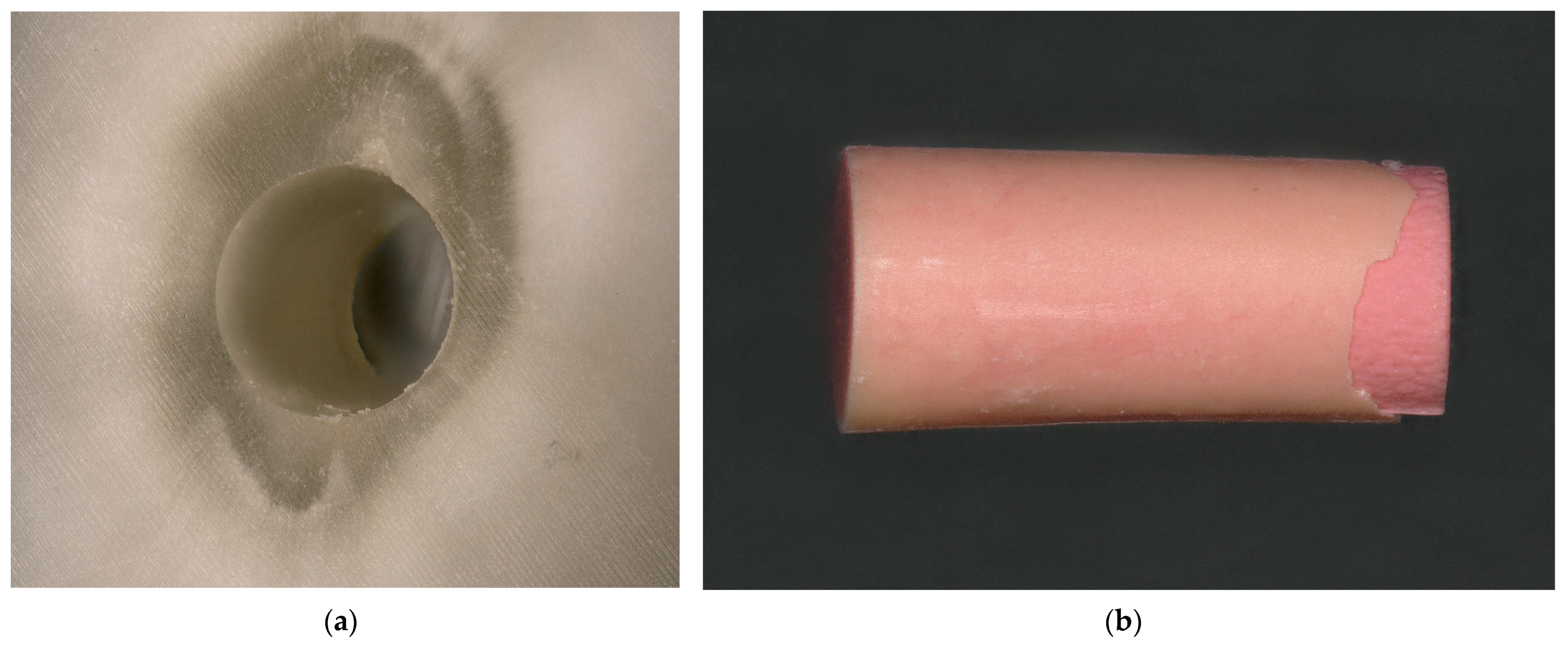
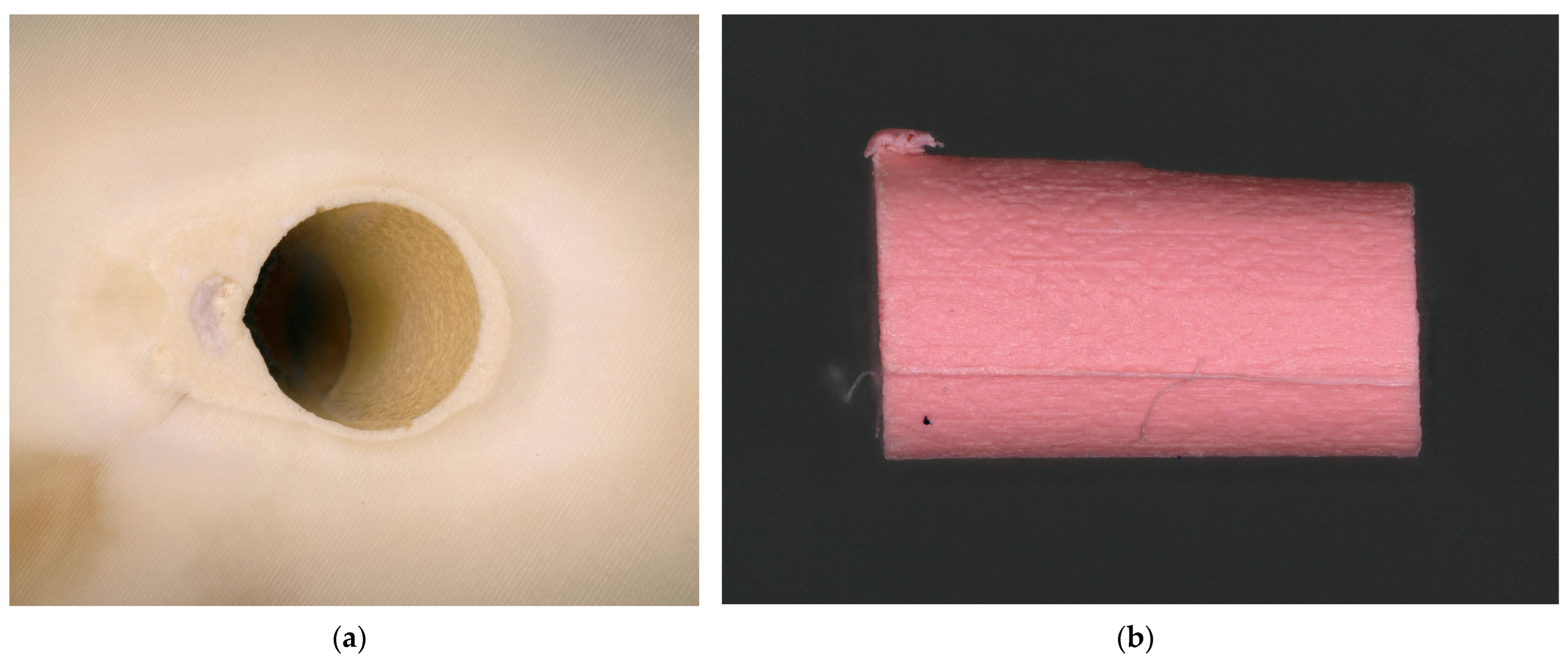
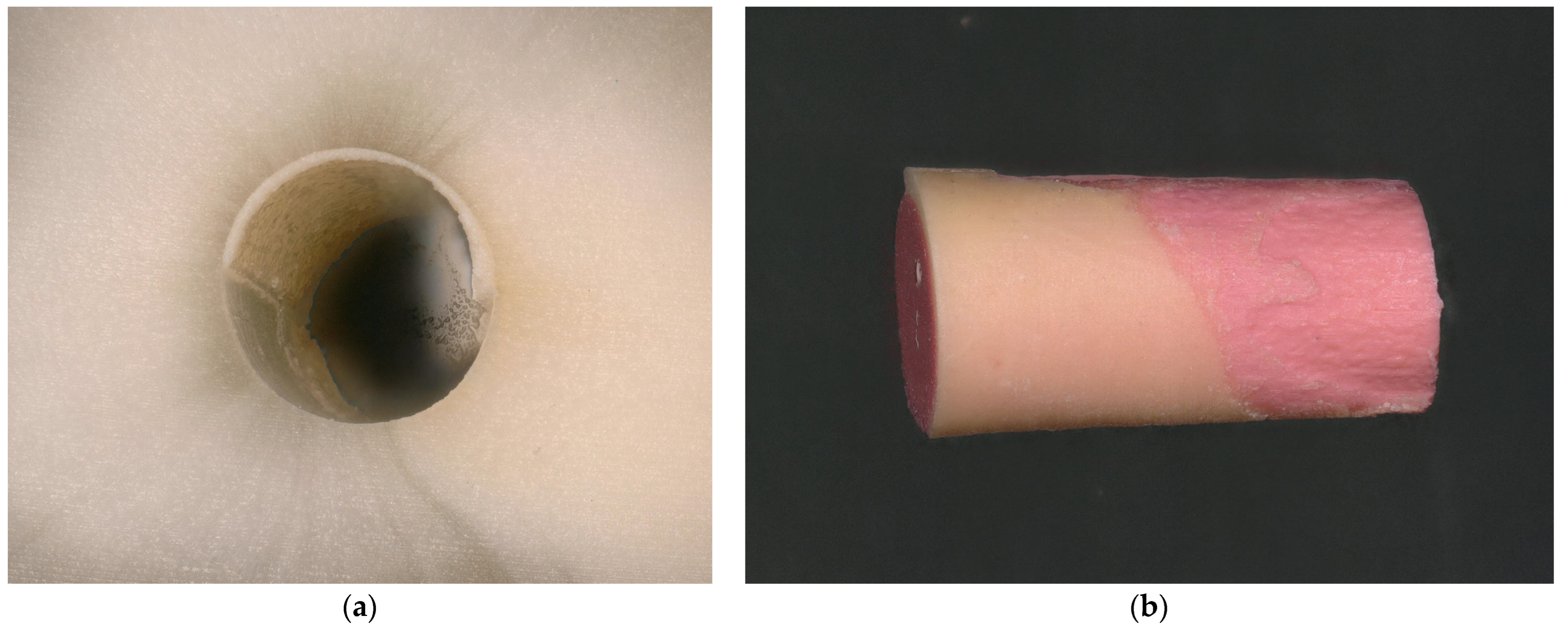
3.4. Fractographic Analysis
3.5. Evaluation of Fracture Modes
4. Discussion
4.1. Method
4.1.1. Storage Period and Storage Medium
4.1.2. Analysis of Temperatures During Embedding and Cutting
4.1.3. Irrigation Protocol and Drying of the Root Canals
4.1.4. Selection of the Cutting Planes
4.1.5. Bond Strength Analysis
4.1.6. Limitations of the Study
4.2. Discussion of Results
POBS Values and Comparison with Other Studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wu, M.K.; Fan, B.; Wesselink, P.R. Diminished leakage along root canals filled with gutta-percha without sealer over time: A la boratory study. Int. Endod. J. 2000, 33, 121–125. [Google Scholar] [CrossRef]
- Taha, N.A.; Maghaireh, G.A.; Bagheri, R.; Abu Holy, A. Fracture strength of root filled premolar teeth restored with silorane and methacrylate-based resin composite. J. Dent. 2015, 43, 735–741. [Google Scholar] [CrossRef]
- Heberer, M.T.; Roggendorf, H.C.; Faber, F.J.; Lawrenz, N.A.; Frankenberger, R.; Roggendorf, M.J. Longitudinal craze line propagation in human root dentin after instrumentation with NiTi rotary files of different instrument tapers after long-term chewing simulation. Clin. Oral Investig. 2022, 26, 2671–2679. [Google Scholar] [CrossRef]
- Karapinar Kazandag, M.; Sunay, H.; Tanalp, J.; Bayirli, G. Fracture resistance of roots using different canal filling systems. Int. Endod. J. 2009, 42, 705–710. [Google Scholar] [CrossRef]
- Ersoy, I.; Evcil, M.S. Evaluation of the effect of different root canal obturation techniques using two root canal sealers on the fracture resistance of endodontically treated roots. Microsc. Res. Tech. 2015, 78, 404–407. [Google Scholar] [CrossRef] [PubMed]
- Ravanshad, S.; Torabinejad, M. Coronal dye penetration of the apical filling materials after post space preparation. Oral. Surg. Oral Med. Oral Pathol. 1992, 74, 644–647. [Google Scholar] [CrossRef] [PubMed]
- Ricci, E.R.; Kessler, J.R. Apical seal of teeth obturated by the laterally condensed gutta-percha, the Thermafil plastic and Thermafil metal obturator techniques after post space preparation. J. Endod. 1994, 20, 123–126. [Google Scholar] [CrossRef] [PubMed]
- Torres, F.F.E.; Zordan-Bronzel, C.L.; Guerreiro-Tanomaru, J.M.; Chávez-Andrade, G.M.; Pinto, J.C.; Tanomaru-Filho, M. Effect of immersion in distilled water or phosphate-buffered saline on the solubility, volumetric change and presence of voids within new calcium silicate-based root canal sealers. Int. Endod. J. 2020, 53, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Razdan, A.; Benetti, A.R.; Bakhshandeh, A.; Darvann, T.A.; Bjørndal, L. Dimensional changes of endodontic sealers-An in vitro model simulating a clinical extrusion scenario during 18 months. Clin. Exp. Dent. Res. 2023, 9, 299–313. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Urban, K.; Neuhaus, J.; Donnermeyer, D.; Schäfer, E.; Dammaschke, T. Solubility and pH Value of 3 Different Root Canal Sealers: A Long-term Investigation. J. Endod. 2018, 44, 1736–1740. [Google Scholar] [CrossRef] [PubMed]
- Donnermeyer, D.; Schemkämper, P.; Bürklein, S.; Schäfer, E. Short and Long-Term Solubility, Alkalizing Effect, and Thermal Persistence of Premixed Calcium Silicate-Based Sealers: AH Plus Bioceramic Sealer vs. Total Fill BC Sealer. Materials 2022, 15, 7320. [Google Scholar] [CrossRef]
- Gernhardt, C.R.; Krüger, T.; Bekes, K.; Schaller, H.G. Apical sealing ability of 2 epoxy resin-based sealers used with root canal obturation techniques based on warm gutta-percha compared to cold lateral condensation. Quintessence Int. 2007, 38, 229–234. [Google Scholar]
- Hergt, A.; Wiegand, A.; Hülsmann, M.; Rödig, T. AH Plus root canal sealer—An updated literature review. Endod. Pract. Today 2015, 9, 245–265. [Google Scholar]
- Donnermeyer, D.; Dornseifer, P.; Schäfer, E.; Dammaschke, T. The push-out bond strength of calcium silicate-based endodontic sealers. Head Face Med. 2018, 20, 13. [Google Scholar] [CrossRef]
- Bowen, R.L. Use of epoxy resins in restorative materials. J. Dent. Res. 1956, 35, 360–369. [Google Scholar] [CrossRef]
- Watson, T.F.; Atmeh, A.R.; Sajini, S.; Cook, R.J.; Festy, F. Present and future of glass-ionomers and calcium-silicate cements as bioactive materials in dentistry: Biophotonics-based interfacial analyses in health and disease. Dent. Mater. 2014, 30, 50–61. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- López-García, S.; Pecci-Lloret, M.R.; Guerrero-Gironés, J.; Pecci-Lloret, M.P.; Lozano, A.; Llena, C.; Rodríguez-Lozano, F.J.; Forner, L. Comparative Cytocompatibility and Mineralization Potential of Bio-C Sealer and TotalFill BC Sealer. Materials 2019, 12, 3087. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Santos, J.M.; Coelho, C.M.; Sequeira, D.B.; Marques, J.A.; Pereira, J.F.; Sousa, V.; Palma, P.J.; Santos, A.C. Subcutaneous Implantation Assessment of New Calcium-Silicate Based Sealer for Warm Obturation. Biomedicines 2021, 9, 24. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.; Kim, E.; Lee, S.; Park, S.; Chen, D.; Shin, S.J.; Kim, E.; Kim, S. Comparison of Biocompatibility of Calcium Silicate-Based Sealers and Epoxy Resin-Based Sealer on Human Periodontal Ligament Stem Cells. Materials 2020, 13, 5242. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- López-García, S.; Myong-Hyun, B.; Lozano, A.; García-Bernal, D.; Forner, L.; Llena, C.; Guerrero-Gironés, J.; Murcia, L.; Rodríguez-Lozano, F.J. Cytocompatibility, bioactivity potential, and ion release of three premixed calcium silicate-based sealers. Clin. Oral Investig. 2020, 24, 1749–1759. [Google Scholar] [CrossRef] [PubMed]
- Donnermeyer, D.; Schmidt, S.; Rohrbach, A.; Berlandi, J.; Bürklein, S.; Schäfer, E. Debunking the Concept of Dentinal Tubule Penetration of Endodontic Sealers: Sealer Staining with Rhodamine B Fluorescent Dye Is an Inadequate Method. Materials 2021, 14, 3211. [Google Scholar] [CrossRef]
- Ebert, J.; Leyer, A.; Günther, O.; Lohbauer, U.; Petschelt, A.; Frankenberger, R.; Roggendorf, M.J. Bond strength of adhesive cements to root canal dentin tested with a novel pull-out approach. J. Endod. 2011, 37, 1558–1561. [Google Scholar] [CrossRef]
- Kokubo, T.; Takadama, H. How useful is SBF in predicting in vivo bone bioactivity? Biomaterials 2006, 27, 2907–2915. [Google Scholar] [CrossRef]
- Yap, W.Y.; Che Ab Aziz, Z.A.; Azami, N.H.; Al-Haddad, A.Y.; Khan, A.A. An in vitro Comparison of Bond Strength of Different Sealers/Obturation Systems to Root Dentin Using the Push-Out Test at 2 Weeks and 3 Months after Obturation. Med. Princ. Pract. 2017, 26, 464–469. [Google Scholar] [CrossRef]
- Shokouhinejad, N.; Gorjestani, H.; Nasseh, A.A.; Hoseini, A.; Mohammadi, M.; Shamshiri, A.R. Push-out bond strength of gutta-percha with a new bioceramic sealer in the presence or absence of smear layer. Aust. Endod. J. 2013, 39, 102–106. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, N.K.; Prado, M.C.; Senna, P.M.; Neves, A.A.; Souza, E.M.; Fidel, S.R.; Sassone, L.M.; Silva, E.J.N.L. Do smear-layer removal agents affect the push-out bond strength of calcium silicate-based endodontic sealers? Int. Endod. J. 2017, 50, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Jainaen, A.; Palamara, J.E.; Messer, H.H. Push-out bond strengths of the dentine-sealer interface with and without a main cone. Int. Endod. J. 2007, 40, 882–890. [Google Scholar] [CrossRef] [PubMed]
- Nagas, E.; Uyanik, M.O.; Eymirli, A.; Cehreli, Z.C.; Vallittu, P.K.; Lassila, L.V.; Durmaz, V. Dentin moisture conditions affect the adhesion of root canal sealers. J. Endod. 2012, 38, 240–244. [Google Scholar] [CrossRef] [PubMed]
- Pawar, A.M.; Pawar, S.; Kfir, A.; Pawar, M.; Kokate, S. Push-out bond strength of root fillings made with C-Point and BC sealer versus gutta-percha and AH Plus after the instrumentation of oval canals with the Self-Adjusting File versus WaveOne. Int. Endod. J. 2016, 49, 374–381. [Google Scholar] [CrossRef]
- Penukonda, R.; Teja, K.V.; Kacharaju, K.R.; Xuan, S.Y.; Mohan, D.A.P.; Sheun, L.Y.; Cernera, M.; Iaculli, F. Comparative evaluation of smear layer removal with Ultra-X device and XP-Endo Finisher file system: An ex-vivo study. G. Ital. Endod. 2023, 37, 1–7. [Google Scholar] [CrossRef]
- Cardoso, L.R.; Baldasso, F.E.R.; Delai, D.; Montagner, F.; Kopper, P.M.P. Effect of EDTA, sodium, and calcium hypochlorite on the inorganic component of root canal dentin: A SEM analysis. Microsc. Res. Tech. 2019, 82, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Augusto, C.M.; Cunha Neto, M.A.; Pinto, K.P.; Barbosa, A.F.A.; Silva, E.J.N.L.; Dos Santos, A.P.P.; Sassone, L.M. Influence of the use of chelating agents as final irrigant on the push-out bond strength of epoxy resin-based root canal sealers: A systematic review. Aust. Endod. J. 2022, 48, 347–363. [Google Scholar] [CrossRef]
- Rajamanickam, K.; Teja, K.V.; Ramesh, S.; Choudhari, S.; Cernera, M.; Armogida, N.G.; Mustafa, M.; Spagnuolo, G. Evaluation of Root Canal Cleanliness on Using a Novel Irrigation Device with an Ultrasonic Activation Technique: An Ex Vivo Study. Appl. Sci. 2023, 13, 796. [Google Scholar] [CrossRef]
- Caron, G.; Nham, K.; Bronnec, F.; Machtou, P. Effectiveness of different final irrigant activation protocols on smear layer removal in curved canals. J. Endod. 2010, 36, 1361–1366. [Google Scholar] [CrossRef]
- Urban, K.; Donnermeyer, D.; Schäfer, E.; Bürklein, S. Canal cleanliness using different irrigation activation systems: A SEM evaluation. Clin. Oral Investig. 2017, 21, 2681–2687. [Google Scholar] [CrossRef] [PubMed]
- Sarrafan, A.; Soleymani, A.; Bagheri Chenari, T.; Seyedmajidi, S. Comparison of push-out bond strength of endodontic sealers after root canal drying with different techniques. Clin. Exp. Dent. Res. 2023, 9, 314–321. [Google Scholar] [CrossRef]
- Roggendorf, M.J.; Ebert, J.; Petschelt, A.; Frankenberger, R. Influence of moisture on the apical seal of root canal fillings with five different types of sealer. J. Endod. 2007, 33, 31–33. [Google Scholar] [CrossRef]
- Patil, S.A.; Dodwad, P.K.; Patil, A.A. An in vitro comparison of bond strengths of Gutta-percha/AH Plus, Resilon/Epiphany self-etch and EndoREZ obturation system to intraradicular dentin using a push-out test design. J. Conserv. Dent. 2013, 16, 238–242. [Google Scholar] [CrossRef] [PubMed]
- Frankenberger, R.; Strobel, W.O.; Krämer, N.; Lohbauer, U.; Winterscheidt, J.; Winterscheidt, B.; Petschelt, A. Evaluation of the fatigue behavior of the resin-dentin bond with the use of different methods. J. Biomed. Mater. Res. B Appl. Biomater. 2003, 67B, 712–721. [Google Scholar] [CrossRef]
- Bitter, K.; Gläser, C.; Neumann, K.; Blunck, U.; Frankenberger, R. Analysis of resin-dentin interface morphology and bond strength evaluation of core materials for one stage post-endodontic restorations. PLoS ONE 2014, 28, e86294, Erratum in PLoS ONE 2015, 10, e0118109. [Google Scholar] [CrossRef][Green Version]
- Frankenberger, R.; Winter, J.; Dudek, M.C.; Naumann, M.; Amend, S.; Braun, A.; Krämer, N.; Roggendorf, M.J. Post-Fatigue Fracture and Marginal Behavior of Endodontically Treated Teeth: Partial Crown vs. Full Crown vs. Endocrown vs. Fiber-Reinforced Resin Composite. Materials 2021, 14, 7733. [Google Scholar] [CrossRef]
- Horiuchi, Z.H.; Silva-Sousa, Y.T.; Raucci Neto, W.; Rached-Junior, F.J.; Souza-Gabriel, A.E.; Silva, S.R.; Alfredo, E. Effect of thermoplastic filling techniques on the push-out strength of root sealing materials. Braz. Oral Res. 2016, 30, S1806-83242016000100207. [Google Scholar] [CrossRef]
- Üreyen Kaya, B.; Keçeci, A.D.; Orhan, H.; Belli, S. Micropush-out bond strengths of gutta-percha versus thermoplastic synthetic polymer-based systems—An ex vivo study. Int. Endod. J. 2008, 41, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Carneiro, S.M.; Sousa-Neto, M.D.; Rached, F.A., Jr.; Miranda, C.E.; Silva, S.R.; Silva-Sousa, Y.T. Push-out strength of root fillings with or without thermomechanical compaction. Int. Endod. J. 2012, 45, 821–828. [Google Scholar] [CrossRef] [PubMed]
- Nagas, E.; Cehreli, Z.; Uyanik, M.O.; Durmaz, V. Bond strength of a calcium silicate-based sealer tested in bulk or with different main core materials. Braz. Oral Res. 2014, 28, S1806-83242014000100256. [Google Scholar] [CrossRef] [PubMed]
- Pane, E.S.; Palamara, J.E.; Messer, H.H. Critical evaluation of the push-out test for root canal filling materials. J. Endod. 2013, 39, 669–673. [Google Scholar] [CrossRef]
- Nagas, E.; Uyanik, O.; Durmaz, V.; Cehreli, Z.C. Effect of plunger diameter on the push-out bond values of different root filling materials. Int. Endod. J. 2011, 44, 950–955. [Google Scholar] [CrossRef]
- El-Ma’aita, A.M.; Qualtrough, A.J.; Watts, D.C. The effect of smear layer on the push-out bond strength of root canal calcium silicate cements. Dent. Mater. 2013, 29, 797–803. [Google Scholar] [CrossRef]
- Rached-Júnior, F.J.; Souza, A.M.; Macedo, L.M.; Raucci-Neto, W.; Baratto-Filho, F.; Silva, B.M.; Silva-Sousa, Y.T. Effect of root canal filling techniques on the bond strength of epoxy resin-based sealers. Braz. Oral Res. 2016, 30, S1806-83242016000100217. [Google Scholar] [CrossRef]
- Oliveira, D.S.; Cardoso, M.L.; Queiroz, T.F.; Silva, E.J.; Souza, E.M.; De-Deus, G. Suboptimal push-out bond strengths of calcium silicate-based sealers. Int. Endod. J. 2016, 49, 796–801. [Google Scholar] [CrossRef]
- de Freitas, J.V.; Ebert, J.; Mazzi-Chaves, J.F.; Tomazinho, F.S.F.; Sousa-Neto, M.D.; Lohbauer, U.; Baratto-Filho, F. Temperature changes affect the rheological properties of a silicone-based and an epoxy resin-based root canal sealers. Aust. Endod. J. 2020, 46, 394–399. [Google Scholar] [CrossRef] [PubMed]
- Donnermeyer, D.; Urban, K.; Bürklein, S.; Schäfer, E. Physico-chemical investigation of endodontic sealers exposed to simulated intracanal heat application: Epoxy resins and zinc oxide–eugenols. Int. Endod. J. 2020, 53, 690–697. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, S.; Schäfer, E.; Bürklein, S.; Rohrbach, A.; Donnermeyer, D. Minimal Dentinal Tubule Penetration of Endodontic Sealers in Warm Vertical Compaction by Direct Detection via SEM Analysis. J. Clin. Med. 2021, 10, 4440. [Google Scholar] [CrossRef] [PubMed]



| Instrument | Taper/Size | LOT |
|---|---|---|
| 0.02/#16 | 1715532 |
| 0.04/#17 | 1717171 | |
| 0.06/#25 | 1720579 | |
| 0.07/#30 | 1717170 | |
| 0.06/#40 | 1466954 | |
| 0.06/#50 | 1721076 |
| Sealer | Paste A | Paste B |
|---|---|---|
| Group 1: AH Plus Jet (LOT: #2201001033) | Calcium tungstate, epoxy resins, zirconium oxide, polydimethylsiloxane, silicon dioxide, and iron oxide pigments. | Calcium tungstate, zirconium oxide, amine resins, silicon dioxide, and polydimethylsiloxane. |
| Group 2: K-0189 (LOT: #2201004013) 1 | Calcium tungstate, epoxy resins, silicon dioxide, polymeric additives, and iron oxide pigments. | Calcium tungstate, amine resins, silicon dioxide, polydimethylsiloxane, and polymeric additive. |
| Obturation Point | Obturation Technique | LOT | Manufacturer |
|---|---|---|---|
| A: ProTaper NEXT X5 gutta-percha point | Cold Obturation (CO) | 0000294451 | Dentsply Maillefer |
| B: ProTaper Universal F5 gutta-percha point | Cold Obturation (CO) | 384061O | Dentsply Maillefer |
| C: GuttaCore X5 obturator | Warm Obturation (WO) | 0000340472 | Dentsply Tulsa |
| Gates–Glidden Bur | Size | Diameter of Plunger [mm] |
|---|---|---|
| white | 50 | 0.35 |
| yellow | 70 | 0.45 |
| red | 90 | 0.55 |
| blue | 110 | 0.65 |
| green | 130 | 0.75 |
| black | 150 | 0.85 |
| Fracture Mode | Visual Appearance |
|---|---|
| adhesive to dentin | The root canal surface was largely or completely free of root canal sealer or gutta-percha, while the gutta-percha was largely covered with sealer. |
| adhesive to gutta-percha | The root canal filling was largely uncovered by sealer, but there was a visible layer of sealer on most of the root canal surface. |
| cohesive | A thin sealer film covered both the canal surface and the gutta-percha filling. |
| mixed | Two or more fracture patterns were identified, but no clearly predominant fracture pattern could be determined. |
| Group | Obturation | Mean | SD | Median | Min. | Max. | IQ | p-Value a |
|---|---|---|---|---|---|---|---|---|
| 1A | AH/PTX | 2.09 | 0.95 | 2.03 | 1.04 | 7.22 | 0.57 | <0.001 * |
| 1B | AH/PTU | 2.16 | 0.52 | 2.12 | 1.46 | 4.25 | 0.45 | <0.001 * |
| 1C | AH/GC | 3.49 | 1.50 | 3.20 | 1.10 | 7.79 | 2.14 | 0.058 |
| 2A | K/PTX | 2.19 | 0.89 | 1.91 | 1.35 | 5.06 | 0.96 | <0.001 * |
| 2B | K/PTU | 2.52 | 0.73 | 2.56 | 0.70 | 3.86 | 1.02 | 0.314 |
| 2C | K/GC | 3.65 | 1.44 | 3.36 | 1.36 | 7.18 | 2.21 | 0.478 |
| 1A | 1B | 1C | 2A | 2B | 2C | ||
|---|---|---|---|---|---|---|---|
| Sealer/Cone | AH/PTX | AH/PTU | AH/GC | K/PTX | K/PTU | K/GC | |
| 1A | AH/PTX | - | 0.155 | <0.001 * | 0.927 | <0.001 * | <0.001 * |
| 1B | AH/PTU | 0.155 | - | <0.001 * | 0.223 | 0.001 * | <0.001 * |
| 1C | AH/GC | <0.001 * | <0.001 * | - | <0.001 * | <0.001 * | 0.508 |
| 2A | K/PTX | 0.927 | 0.223 | <0.001 * | - | 0.011 * | <0.001 * |
| 2B | K/PTU | <0.001 * | 0.001 * | <0.001 * | 0.011 * | - | <0.001 * |
| 2C | K/GC | <0.001 * | <0.001 * | 0.508 | <0.001 * | <0.001 * | - |
| Group | Adhesive to Dentin | Adhesive to Gutta-Percha | Cohesive | Mixed |
|---|---|---|---|---|
| 1A | 0 | 34.88 | 2.33 | 62.79 |
| 1B | 0 | 72.73 | 2.27 | 25.0 |
| 1C | 0 | 0 | 38.0 | 62.0 |
| 2A | 0 | 91.67 | 0 | 8.33 |
| 2B | 1.82 | 70.91 | 3.64 | 23.63 |
| 2C | 0 | 12.20 | 78.04 | 9.76 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roggendorf, M.J.; Roggendorf, H.C.; Müller-Krott, M.; Faber, F.-J.; Frankenberger, R. Bond Strength of an Epoxy Resin Root Canal Sealer Prototype. Dent. J. 2025, 13, 415. https://doi.org/10.3390/dj13090415
Roggendorf MJ, Roggendorf HC, Müller-Krott M, Faber F-J, Frankenberger R. Bond Strength of an Epoxy Resin Root Canal Sealer Prototype. Dentistry Journal. 2025; 13(9):415. https://doi.org/10.3390/dj13090415
Chicago/Turabian StyleRoggendorf, Matthias J., Hubert C. Roggendorf, Markus Müller-Krott, Franz-Josef Faber, and Roland Frankenberger. 2025. "Bond Strength of an Epoxy Resin Root Canal Sealer Prototype" Dentistry Journal 13, no. 9: 415. https://doi.org/10.3390/dj13090415
APA StyleRoggendorf, M. J., Roggendorf, H. C., Müller-Krott, M., Faber, F.-J., & Frankenberger, R. (2025). Bond Strength of an Epoxy Resin Root Canal Sealer Prototype. Dentistry Journal, 13(9), 415. https://doi.org/10.3390/dj13090415







