Abstract
Background/Objectives: To compare the marginal integrity of sectional non-invasive laminate veneers versus sectional minimally invasive laminate veneers. Methods: A total of eighty (80) intact maxillary and mandibular frontal teeth (central incisors) were randomly divided into four groups (n = 20). Two groups received non-invasive veneers made of feldspathic porcelain (Feldspathic Non-Invasive—FNI) and lithium disilicate (Lithium Disilicate Non-Invasive—LNI) accordingly. Groups FP and LP received minimally invasive veneers manufactured by feldspathic porcelain and lithium disilicate, respectively. Following cementation, three grooves with mesio-distal orientation on the labial surface of teeth of each sample, at the incisal, middle, and cervical third, were made. Before and after artificial aging, the mesio-distal distance between the end of the groove on the tooth and the edge of each veneer was measured in micrometers (μm) employing an SEM immediately after cementation (T0), after simulated artificial aging equivalent to four months of everyday brushing (T1), and after twelve months of everyday brushing (2 times per day) (T2) to identify the wear of veneers. In the same manner, the horizontal dimension of the cement layer extending from its edge till the margin of the veneer was measured for all the groups at T0, T1, and T2, respectively. The statistical analysis was performed employing non-parametric Kruskal–Wallis ANOVA and Dunn’s test. Results: No significant differences from T0 to T1 and from T1 to T2, as well as from T0 to T2, were identified for all the groups tested. No significant differences were allocated among all groups for the dimensional changes in the cement. Conclusions: All the groups responded similarly to aging factors, regardless of the non-invasive or minimally invasive approach, or the material used to fabricate the veneers.
1. Introduction
Porcelain veneers were introduced to the profession by John Calamia of New York University, USA, in the early 1980s [1]. Since then, a lot of effort has been made to improve the optical characteristics of the ceramic materials, the bond strength with tooth structure, and the esthetic outcome of veneer restorations [1,2,3,4,5]. However, clinical success and endurance of porcelain veneers are challenging due to the variety of factors involved. Marginal and internal fit [6,7,8,9,10], combined with adequate ceramic thickness [11,12,13], tooth preparation design [14,15,16,17,18], and most importantly, cementation [19,20,21,22], are factors that affect the success of the treatment. Gentle handling during the clinical try-in procedures [23], precise seating of the veneer, and control of the cement excess [24] are crucial to avoid marginal fractures, excessive marginal gaps, microleakage, and secondary caries due to malposition [19,20,21,22,25].
At the same time, the clinician depends on the technician’s expertise to fabricate a prosthesis that fulfills not only the esthetic expectations of the patient but also the mechanical demands during function. Thus, the manufacturing technique [7,26,27,28,29,30,31,32,33], the type of ceramic material [26,34,35] are of paramount importance for the clinical efficacy of these restorations.
In the last few years, minimally invasive dentistry has been introduced as a promising solution for closing diastemas in the frontal area [8,36,37,38,39]. The concept of preserving tooth structure by non-invasive veneers has many advantages. During the treatment, there is no need for anesthesia, the periodontal tissue is not disturbed by impression cords, and provisional restorations are not necessary [40,41,42]. The patient experiences minimal discomfort during the clinical steps and a pain-free transition from the unaesthetic tooth diastema to a beautiful smile. Up to now, there are studies that evaluate sectional non-invasive veneers under aging factors both in vitro and in vivo, but there are no data to compare sectional invasive and non-invasive veneers [40,41,43,44,45,46].
A relevant clinical question is whether non-invasive or minimally invasive veneers can be a reliable solution for closing diastemas in the frontal area. The aim of this comparative study is to test the marginal integrity of sectional non-invasive and minimal invasive laminate veneers ex vivo under simulated aging factors. The null hypothesis is that marginal integrity is not affected either by the clinical approach (non-invasive or minimally invasive) or by the materials used for the fabrication of the veneers.
2. Materials and Methods
All materials (Table 1) used in this comparative study were acquired by one manufacturer and were handled according to the manufacturer’s instructions. A total of eighty (80) intact maxillary and mandibular frontal teeth were included in this study. The selected teeth were extracted due to aggressive periodontitis, orthodontic treatment, or surgical reasons. The research protocol has been approved by the ethics committee of the Dental School of the National and Kapodistrian University of Athens. (Ethics approval number: 295-09/03/2016).

Table 1.
Brand names and lot numbers of materials included in this study.
The teeth were stored in physiological saline solution [22]. Subsequently they were cleaned with hand scaling to remove calculus and periodontal fibers and were examined with magnification loupes at 2.3× nominal magnification to assess tooth structure. The teeth were randomly divided into four (4) groups (n = 20/group) with the following characteristics:
Group FNI received non-invasive laminate veneers, made of feldspathic porcelain
Group LNI received non-invasive laminate veneers, made of lithium disilicate.
Group FP received minimally invasive laminate veneers, made of feldspathic porcelain.
Group LP received minimally invasive laminate veneers, made of lithium disilicate.
Teeth preparation: All the teeth samples from Group FP and Group LP underwent partial veneer preparation. The veneer preparation was completed with a water-cooled high-speed handpiece (Kavo, Gentlesilence LUX 6500B, Biberah, Germany). A diamond bur system specific to ceramic veneers (Komet, REF 4151, Lemgo, Germany) was used to create the necessary space for the veneer. The outline form of each partial veneer extended from the midline of the labial surface to the mesial or the distal surface of the tooth, and 2 mm above the CEJ up to the incisal edge of the tooth. The preparation was initiated by depth cutter burs (Komet, REF4151, CVS-1) to define the appropriate depth of 0.6 mm, followed by a chamfer bur (Komet, REF4151, CVS-4) to refine the preparation. The incisal edge was not prepared. Group FNI and Group LNI received sectional non-invasive veneers, and thus, no preparation was performed.
Fabrication of the porcelain veneers: A duplicate model was fabricated for each specimen. A single dental technician fabricated all the necessary veneers using either feldspathic porcelain (IPS e.max Ceram, Ivoclar Vivadent AG, Schaan, Liechtenstein) or IPS e.max Press ingots (Ivoclar Vivadent AG). Group FNI and group FP received feldspathic porcelain veneers. The refractory dyes technique (Nori-Vest; Kuraray Noritake Dental Inc., Hattersheim am Main, Germany) was used to manufacture feldspathic veneers. This technique permitted the use of layers with multiple levels of opacity, claiming enhanced esthetics [34,47,48,49,50]. Pressed lithium disilicate (IPS e.max Press ingots manually generated with staining) was used to fabricate the restorations for group LNI and LP. Following the recommendations of the manufacturer, pressed lithium disilicate is recommended for laminate veneers with a minimum preparation of 0.6 mm.
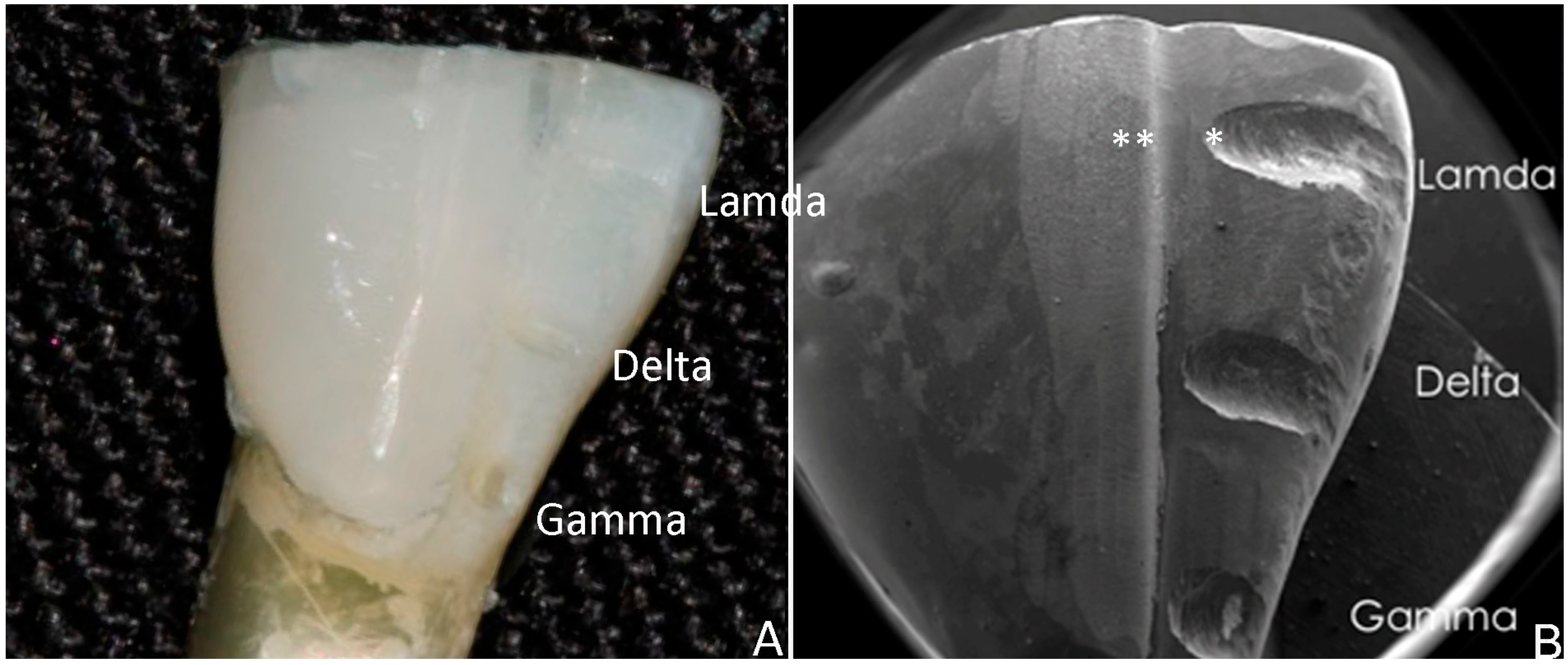
Cementation: Prior to cementation, all the teeth samples were cleaned with a micromotor brush using a fluoride-free cleaning paste (Proxyt, RDA 36, Ivoclar Vivadent AG). The paste was removed with water spray and oil-free air. A self-etching glass-ceramic primer (Monobond, Ivoclar Vivadent AG) was applied on the intaglio surface of the veneer with a micro brush for twenty seconds and allowed to react for forty seconds. Then, the primer was removed with water spray and oil-free air for ten seconds. A phosphoric acid gel (Total Etch, Ivoclar Vivadent AG) was applied on the designated labial area of the tooth and reacted for thirty seconds. The gel was removed with water spray and oil-free air. In the same area, a light-cured adhesive (Adhese Universal Vivapen, Ivoclar Vivadent AG) was applied for twenty seconds. Excess adhesive was removed with gentle air spray. The adhesive was then light-cured for ten seconds. A light-curing luting composite (Variolink Esthetic LC, Ivoclar Vivadent AG) of translucent color was applied on the intaglio surface of the veneer, and the restoration was seated on the designated area of the tooth by means of an adhesive tip applicator (Optra Stick, Ivoclar Vivadent AG). While seated, the excess cement was light-cured for ten seconds following the margin line and was removed with a scaler without damaging the veneer. To prevent oxygen inhibition, a glycerine gel (Liquid Strip, Ivoclar Vivadent AG) was applied on the margin and light-cured for ten seconds. The gel was rinsed with water spray. Finally, the margin of the veneer was polished with a diamond polishing system (OptraFine, Ivoclar Vivadent AG). Following cementation, a thin diamond bur was used to make three (3) horizontal grooves on the labial surface of each sample, at the incisal, middle, and cervical third. These grooves were used as reference points for future observations under the SEM. (Figure 1).
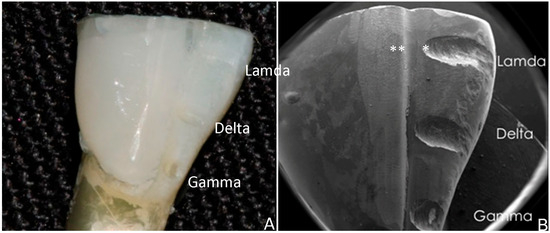
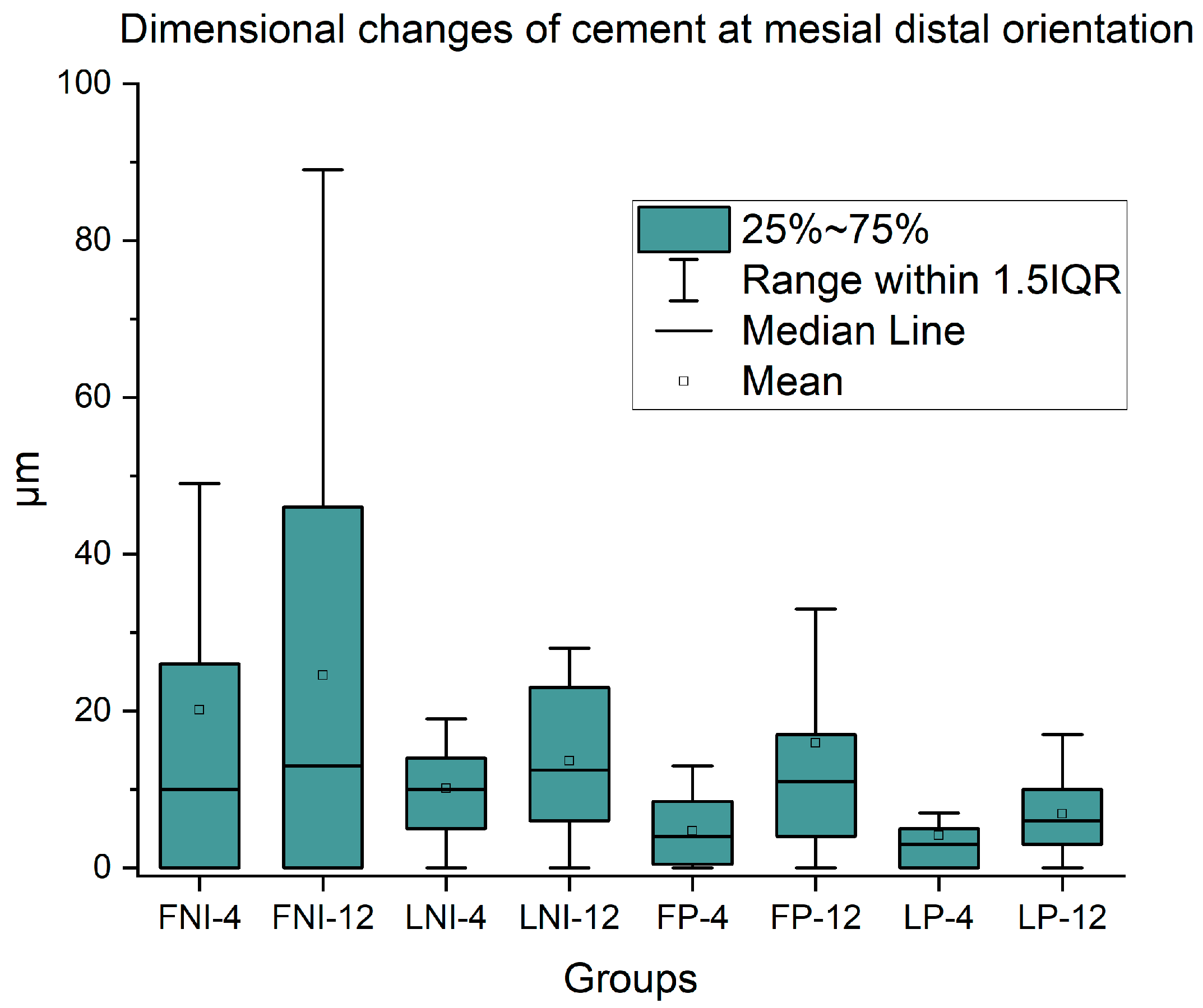
Figure 1.
(A) Stereomicroscope image of prepared teeth (nominal magnification 3×) and (B) Secondary Electron Image from the surface of prepared teeth (nominal magnification 6×). The initial point (edge of the notch) and the final point (edge of the veneer) are indicated by one and two asterisks, respectively.
Artificial Aging Regime: All the specimens were exposed to aging procedures, including thermocycling and brushing, in order to age the veneers in a similar way to the clinical situation. The specimens underwent thermocycling (ISO 11405) at 5000 cycles between two water baths with distilled water of 5 °C and 55 °C with a dwell time of 60 s in a custom-made thermocycling machine. A robotic arm was used to immerse the specimens in two baths for the preset dwell time. After thermocycling the specimens were rinsed with distilled water and allowed to dry in ambient conditions. The aging through brushing was simulated following Fones’ Rotary technique using an electric powered toothbrush (Philips Sonicare DiamondClean 9000, Philips, Amsterdam, The Netherlands) and a toothpaste (Colgate Total, Colgate-Palmolive, Swidnica, Poland) [48,49,50,51,52,53,54]. A custom-made device was used to stabilize the tooth position on a horizontal plane, and the brushing procedure was implemented by a single operator by mixing toothpaste with tap water. The operator was brushing in a continuous cycling motion mimicking the brushing technique. For each specimen a period of thirty (30) seconds of brushing per day was estimated. All the specimens underwent brushing aging equivalent to a duration of four months initially and twelve months in total. All specimens were subjected to 10,000 strokes simulating approximately one year of oral aging [55].
Measurements: All the specimens were subjected to Scanning Electron Microscope (Quanta Inspect D8334, FEI, Hillsboro, OR, USA) observation, at three stages:
1. Immediately after cementation (T0).
2. Following simulated artificial aging equivalent to four months (T1).
3. Following simulated artificial aging equivalent to twelve months (T2).
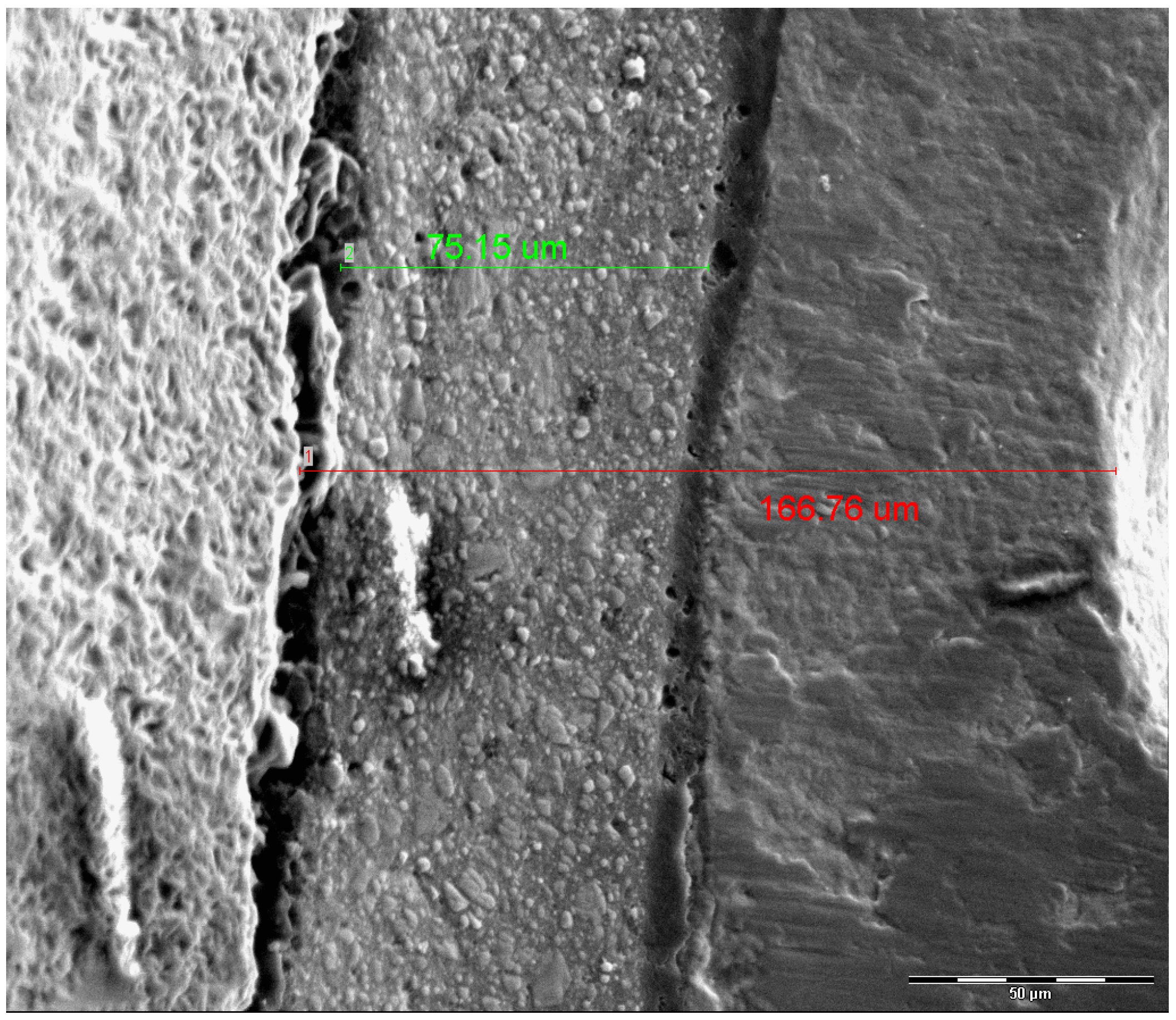
At T0, the horizontal grooves (incisal, middle, cervical) of the labial surface were examined in relationship with the margin and the cement layer. One of the grooves was randomly selected employing a free online randomization software (https://www.randomizer.org, accessed on 16 March 2023). Henceforth, for each specimen, that area of the labial surface was examined, and the groove included in the selected area will define the area of interest until the end of the observation period [56]. The specimens were placed on aluminum stubs, sputter-coated with gold (Emitech SC7620 Sputter Coater; Emitech, Paris, France) and imaged by Secondary Electron Detector employing high vacuum conditions, operating at 15 kV, 98 μA beam current, and observed at 500× nominal magnification. Secondary Electron Images (SEI) were taken from the selected area. The horizontal distance between the end of the groove and the edge of each veneer (in the mesio-distal orientation) was measured in micrometers (μm) employing the dedicated image analysis software (XT Docu ver3.2; Soft Imaging System GmbH, FEI) as shown in Figure 2. The measurements took place at T0, T1, and T2, respectively. The teeth were placed in the SEM stage with the same orientation, and the stored image at T0 was used to identify the reference point at the edge of the groove (Figure 2). In the same manner, the mesio-distal distance of the cement layer extending from its edge till the margin of the veneer was measured for all the groups at T0, T1, and T2, respectively.
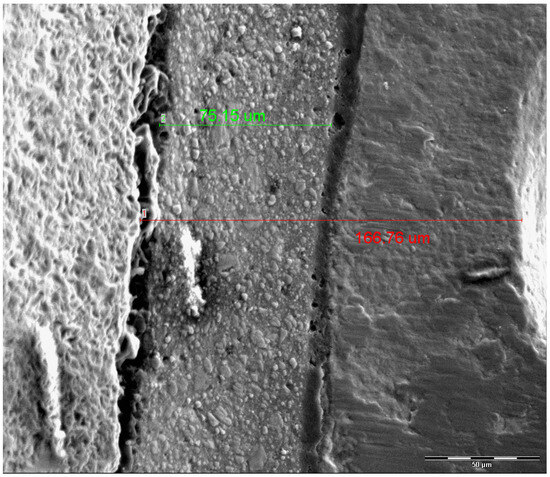
Figure 2.
Measurement of mesio-distal distance between the groove and the edge of the veneer (red line) and the extent of the cement layer (green line). Nominal magnification 500×, scale bar: 50 μm.
Statistical Analysis
All the results were initially tested for the presence of outliers employing the Grubbs test. Then the groups were first tested for normality using the Kolmogorov–Smirnov criterion. Quantitative variables were presented with mean, median, and 25% and 75% quartiles as normality check failed. Statistically significant differences were identified by non-parametric Kruskal–Wallis ANOVA and Dunn’s multiple comparison test. In all the cases the statistical level of significance was set at α = 0.05. The statistical analysis was carried out by OriginPro 2021 v. 9.8 (OriginLab Corporation, Northampton, MA, USA).
3. Results
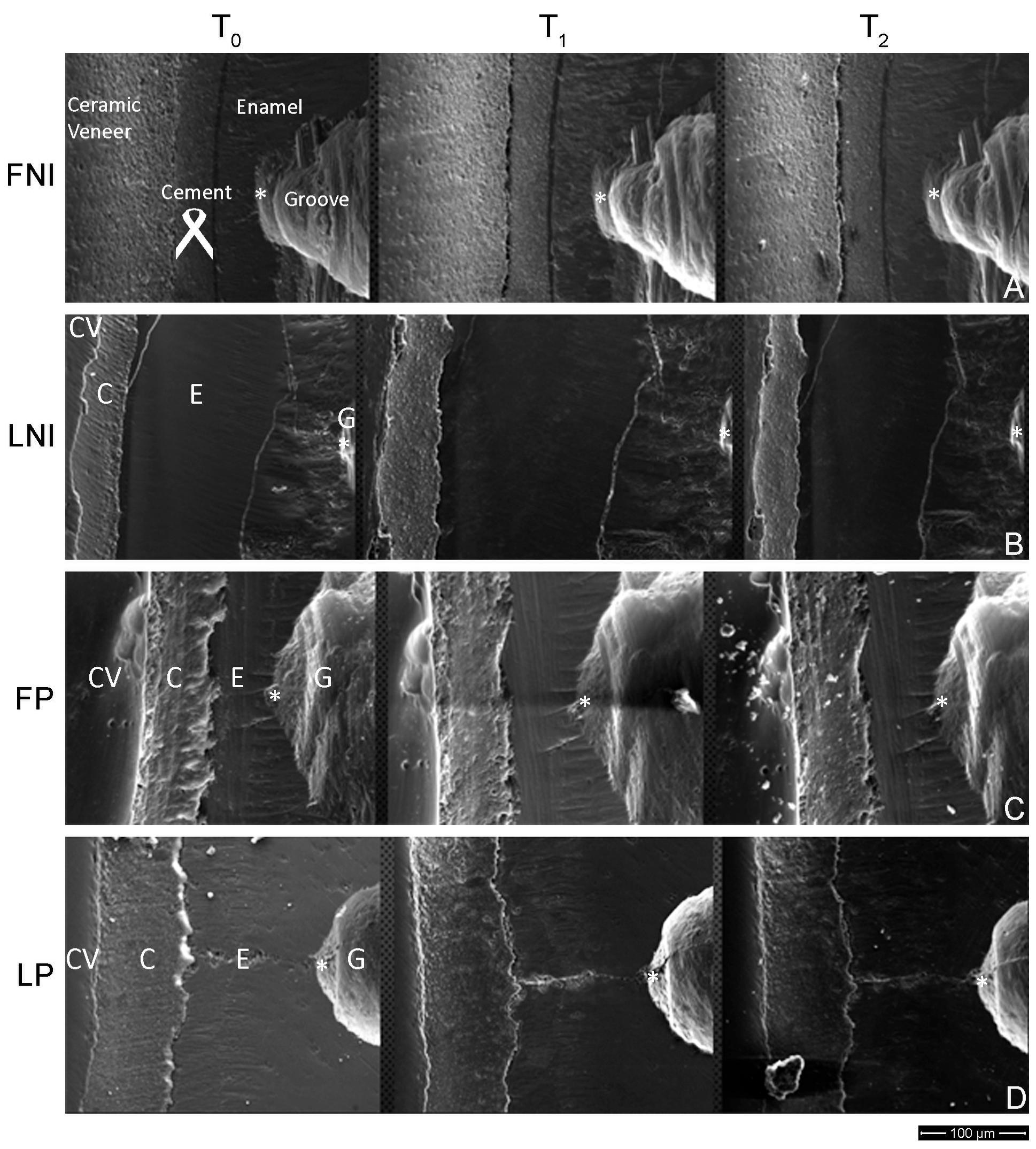
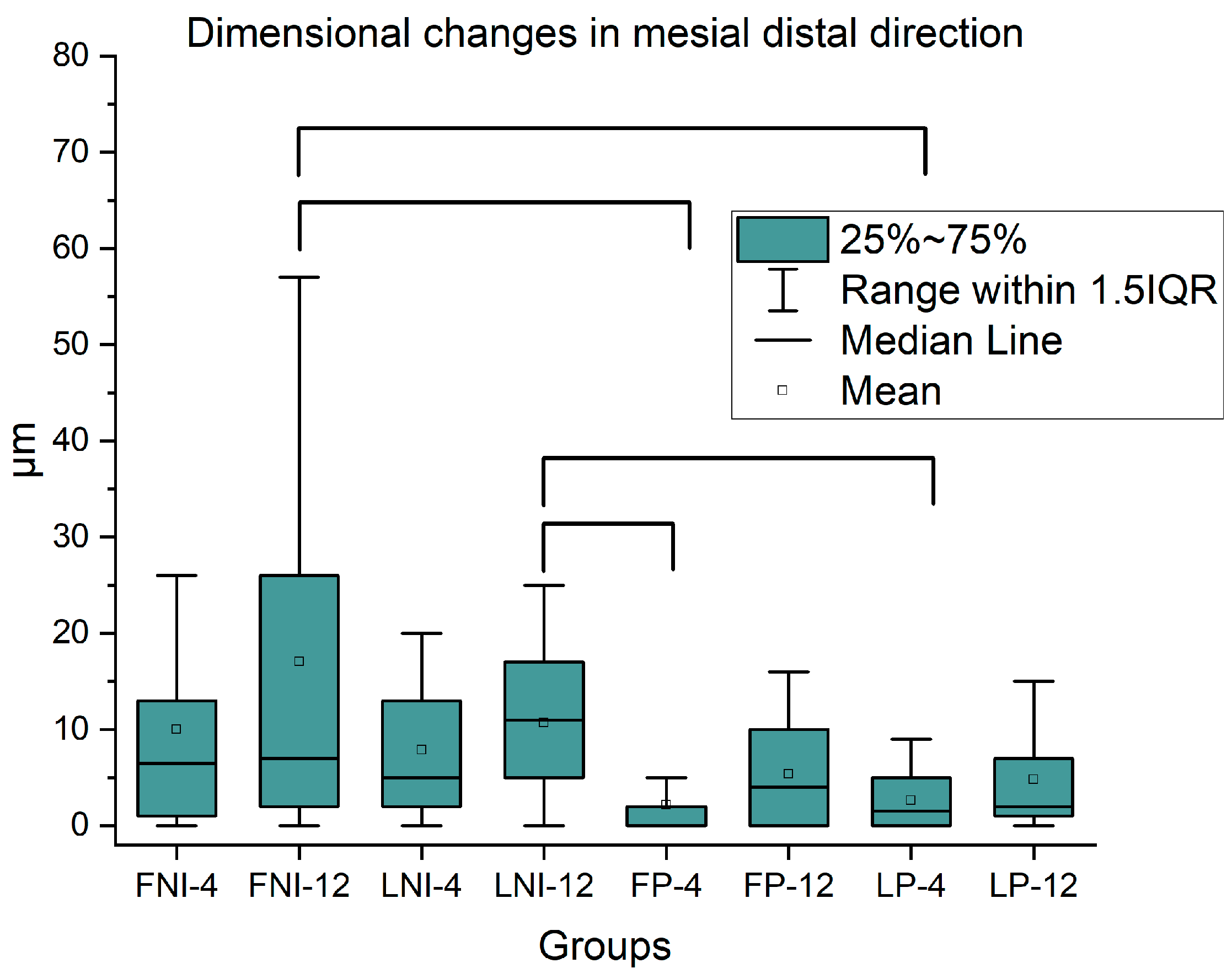
Figure 3 presents successive images from the same region of interest for all the groups tested at T0, T1, and T2. Different regions are identified on the left image of each row, indicating the ceramic veneer, the cement, the enamel, and the groove areas, while Figure 4 shows the dimensional changes in the mesial–distal direction with mean, median, 25% and 75% percentiles. Brackets connect mean values with statistically significant differences (p < 0.05).
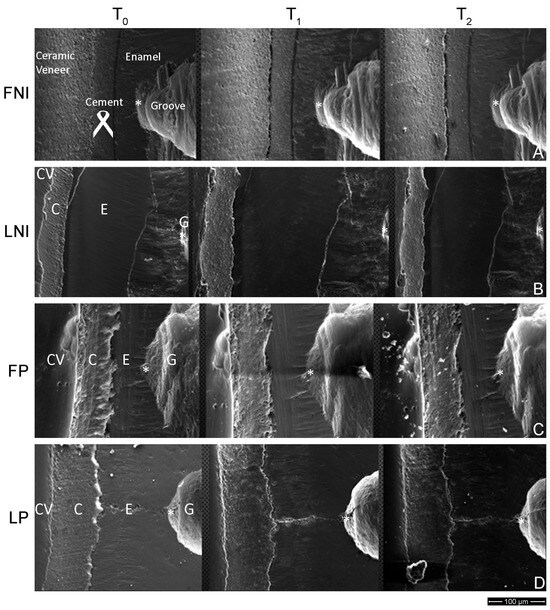
Figure 3.
Successive SE images from the same region for all the groups tested at T0, T1, and T2. (A) FNI, (B) LNI, (C) FP, and (D) LP. All the reference points are indicated by an asterisk. Ceramic venners (CV), cement (C), enamel (E), and groove (G) are indicated on the left images. Nominal magnification 500×, scale bar: 100 μm.
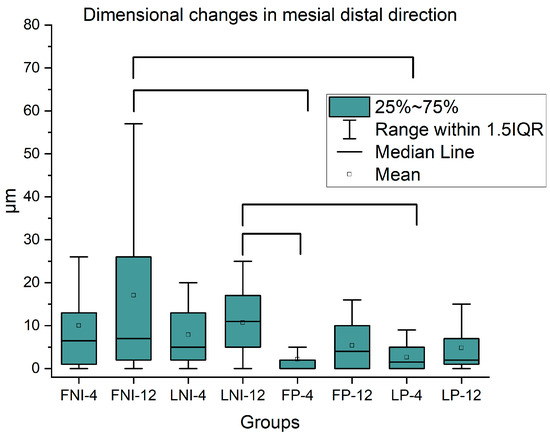
Figure 4.
Box plots including mean, median, and 25% and 75% percentiles of dimensional changes in the mesial–distal direction for all the groups tested (n = 20). Brackets connect mean values with statistically significant differences (p < 0.05).
During the follow-up period, mesio-distal distance from the notch to the margin of the veneer was increased for all under-study groups, indicating wear of the veneer. However, no significant differences were identified from T0 to T1, from T1 to T2, as well as from T0 to T2 for all the groups tested. In Figure 5 the dimensional changes in the cement in the mesial–distal orientation with mean, median, 25%, and 75% percentiles are presented. In all the measurements, there were non-significant differences among all the groups under study (p > 0.05).
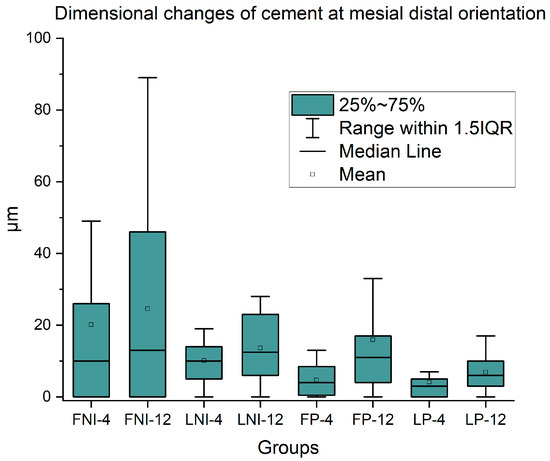
Figure 5.
The dimensional changes in cement in the mesial–distal orientation with mean, median, and 25% and 75% percentiles are presented (n = 20). No statistically significant differences were found for all the groups tested (p > 0.05).
4. Discussion
The results of the study confirm both parts of the null hypothesis. Regarding the first part, all the groups had similar performance to aging factors with no significant differences between the non-invasive and minimally invasive approaches. For the second part, both materials used to fabricate the veneers responded evenly to the aging factors with no significant differences between them, and thus both null hypotheses should be accepted.
Water thermocycling was used to simulate the wet oral environment and the effect of temperature fluctuations at the interfaces of different materials (enamel, cement, porcelain) with differences in coefficients of thermal expansion. In clinical circumstances, when sectional non-invasive veneers are used to close diastemas on the frontal area, it is common for clinicians to correct interferences and thus avoid any force load applied on the veneer [45,46,47]. At the same time, patients are instructed to avoid extensive biting force over veneered teeth but not to neglect brushing them. Brushing of teeth is the most common way of oral care, and this is why it was selected as an aging factor in the study. Patients are educated by dentists to brush their teeth at least two times per day as a standard of care, and the toothbrush is the most recommended product to do so [48,49]. A power toothbrush was chosen over a manual one because it is commonly used by the public [49,54]. Nowadays, power toothbrushes are strongly commercially promoted, and thus more patients tend to embed them in their daily oral care routine. Natural teeth rather than models were chosen in the study to utilize their natural, physical, and mechanical properties, bonding capacity, and geometrical characteristics, eliminating differences from real clinical situations [11,40]. Instead of multiple clinicians participating, only one operator was handling the try-in procedures and the cementation of the veneers in an effort to minimize the effect of human factor on the outcome of this study [23]. SEM was used to document the marginal integrity of the samples under an artificial aging regime. This approach has the advantage of obtaining detailed information on the areas of interest, keeping intact the tooth surface, and analyzing the samples in a successive manner, a common methodology for this type of experimental characterization [6,56]. Three different areas were chosen in order to homogenize the possible differences in wear among cervical, middle, and incisal regions.
The specific aging periods of simulated 4 and 12 months were selected to match with first (common 4 to 6 months) and annual recall. During the evaluation period, none of the groups tested presented fracture, debonding, crack lines, or any sign of macroscopically detected surface deterioration (wear, loss of gloss, etc.) due to artificial aging. This is in accordance with previous studies where no significant wear was detected on ceramic and composite materials under the abrasive action of toothbrushing [49,50,51,52,53]. It is interesting to point out that their focus area was at the center surface of the material and not on its margins, as the latter are thinner and sharper and thus more vulnerable to wear phenomena. On the macroscopical level, the marginal deterioration of both groups was not adequate enough to create a difference that a clinician could detect at recall examination using a probe. Contrarily, on microscopic evaluation under an SEM, all the groups showed a marginal deterioration of a few microns but without statistically significant differences either between restorative materials or restorative approach, verifying both null hypotheses. In Figure 4 a few groups showed statistically significant differences after one-way ANOVA, but these comparisons would not be included in a typical 2-way ANOVA as they comprise different materials and time periods (i.e., FNI-12 with NP-4), and thus, no comparison is feasible. This complication arises from the absence of non-parametric two-way ANOVA (non-parametric tests are necessary for populations without normal distributions), and thus one-way ANOVA was the only option for statistical comparison. On a parallel observation, the cement used for the cementation of the veneers behaved in a similar manner during the whole observation period, with no significant differences between the groups. The absence of statistically significant differences is expected as the same material was used for all the groups tested, and thus, the same response to artificial aging was anticipated. Noteworthy to mention that despite the gradual loss of its layer, it delivered an acceptable clinical outcome.
Despite the efforts to simulate oral conditions as much as possible, this study is not free from the inherent limitation of experimental studies where oral parameters (chewing loading, pH fluctuations, irradiation, food consumption, and others) can not be totally simulated. In addition, it should be noted that the absence of significant differences does not imply equivalence, as more data is required to verify this hypothesis from a statistical standpoint of view. The results of this study showed that sectional non–invasive veneers can be a promising option for closing tooth diastemas, providing alternative solutions to esthetic demands. However, more data based on clinical studies, including clinical success, survival, chipping, color stability, etc.) should be collected to enlighten our picture for the clinical efficacy of sectional non-invasive veneers as a promising, safe, and efficient candidate for everyday practice.
5. Conclusions
Under the limitations of this study, the following conclusions can be drawn:
The effect of aging factors included in this study (water thermocycling and brushing) is not dependent on either invasive protocol (Sectional non-invasive and minimally invasive) or materials used for the fabrication of veneers.
Sectional non-invasive and minimally invasive veneers responded similarly to aging factors such as brushing and thermocycling for a simulated aging duration of twelve months.
Both materials used to fabricate the veneers, namely feldspathic porcelain and lithium disilicate, performed equally through the testing period regardless of the minimally invasive or non-invasive approach.
The cement used for the cementation was prepared in a similar manner for all the groups throughout the whole testing period.
Author Contributions
P.P.: investigation, formal analysis, visualization, and writing—original draft preparation. P.K.: conceptualization, methodology, investigation, writing—review and editing, and supervision. G.P.: conceptualization, methodology, investigation, and writing—review and editing. S.Z.: formal analysis, validation, visualization, and writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by the ethics committee of the Dental School of the National and Kapodistrian University of Athens. (Ethics approval number: 295-09/03/2016).
Data Availability Statement
Dataset available on request from the authors.
Acknowledgments
The materials used in the study were provided disinterestedly by Ivoclar Vivadent AG, Schaan, Liechtenstein.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Calamia, J.R. Etched porcelain veneers: The current state of the art. Quintessence Int. 1985, 16, 5–12. [Google Scholar] [PubMed]
- Vanlioglu, B.A.; Kulak-Ozkan, Y. Minimally invasive veneers: Current state of the art. Clin. Cosmet. Investig. Dent. 2014, 6, 101–107. [Google Scholar] [CrossRef]
- Beier, U.S.; Kapferer, I.; Burtscher, D.; Dumfahrt, H. Clinical performance of porcelain laminate veneers for up to 20 years. Int. J. Prosthodont. 2012, 25, 79–85. [Google Scholar]
- Silva, L.H.D.; Lima, E.; Miranda, R.B.P.; Favero, S.S.; Lohbauer, U.; Cesar, P.F. Dental ceramics: A review of new materials and processing methods. Braz. Oral Res. 2017, 31, e58. [Google Scholar] [CrossRef]
- Morimoto, S.; Albanesi, R.B.; Sesma, N.; Agra, C.M.; Braga, M.M. Main Clinical Outcomes of Feldspathic Porcelain and Glass-Ceramic Laminate Veneers: A Systematic Review and Meta-Analysis of Survival and Complication Rates. Int. J. Prosthodont. 2016, 29, 38–49. [Google Scholar] [CrossRef]
- Ranganathan, H.; Ganapathy, D.M.; Jain, A.R. Cervical and Incisal Marginal Discrepancy in Ceramic Laminate Veneering Materials: A SEM Analysis. Contemp. Clin. Dent. 2017, 8, 272–278. [Google Scholar] [CrossRef]
- Kang, S.Y.; Lee, H.N.; Kim, J.H.; Kim, W.C. Evaluation of marginal discrepancy of pressable ceramic veneer fabricated using CAD/CAM system: Additive and subtractive manufacturing. J. Adv. Prosthodont. 2018, 10, 347–353. [Google Scholar] [CrossRef]
- Mozayek, R.S.; Allaf, M.; Dayoub, S. Porcelain sectional veneers, an ultra-conservative technique for diastema closure (three-dimensional finite element stress analysis). Dent. Med. Probl. 2019, 56, 179–183. [Google Scholar] [CrossRef]
- Al-Dwairi, Z.N.; Al-Sardi, M.; Goodacre, B.J.; Goodacre, C.J.; Al Hamad, K.Q.; Özcan, M.; Husain, N.A.-H.; Baba, N.Z. Evaluation of Marginal and Internal Fit of Ceramic Laminate Veneers Fabricated with Five Intraoral Scanners and Indirect Digitization. Materials 2023, 16, 2181. [Google Scholar] [CrossRef]
- Baig, M.R.; Qasim, S.S.B.; Baskaradoss, J.K. Marginal and internal fit of porcelain laminate veneers: A systematic review and meta-analysis. J. Prosthet. Dent. 2024, 131, 13–24. [Google Scholar] [CrossRef]
- Blunck, U.; Fischer, S.; Hajto, J.; Frei, S.; Frankenberger, R. Ceramic laminate veneers: Effect of preparation design and ceramic thickness on fracture resistance and marginal quality in vitro. Clin. Oral Investig. 2020, 24, 2745–2754. [Google Scholar] [CrossRef]
- Ge, C.; Green, C.C.; Sederstrom, D.; McLaren, E.A.; White, S.N. Effect of porcelain and enamel thickness on porcelain veneer failure loads in vitro. J. Prosthet. Dent. 2014, 111, 380–387. [Google Scholar] [CrossRef]
- Ge, C.; Green, C.C.; Sederstrom, D.A.; McLaren, E.A.; Chalfant, J.A.; White, S.N. Effect of tooth substrate and porcelain thickness on porcelain veneer failure loads in vitro. J. Prosthet. Dent. 2018, 120, 85–91. [Google Scholar] [CrossRef]
- Lin, T.M.; Liu, P.R.; Ramp, L.C.; Essig, M.E.; Givan, D.A.; Pan, Y.H. Fracture resistance and marginal discrepancy of porcelain laminate veneers influenced by preparation design and restorative material in vitro. J. Dent. 2012, 40, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, K.K.; Chiayabutr, Y.; Phillips, K.M.; Kois, J.C. Influence of preparation design and existing condition of tooth structure on load to failure of ceramic laminate veneers. J. Prosthet. Dent. 2011, 105, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Stappert, C.F.; Ozden, U.; Gerds, T.; Strub, J.R. Longevity and failure load of ceramic veneers with different preparation designs after exposure to masticatory simulation. J. Prosthet. Dent. 2005, 94, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Tugcu, E.; Vanlioglu, B.; Ozkan, Y.K.; Aslan, Y.U. Marginal Adaptation and Fracture Resistance of Lithium Disilicate Laminate Veneers on Teeth with Different Preparation Depths. Int. J. Periodontics Restor. Dent. 2018, 38, s87–s95. [Google Scholar] [CrossRef]
- Tsouknidas, A.; Karaoglani, E.; Michailidis, N.; Kugiumtzis, D.; Pissiotis, A.; Michalakis, K. Influence of Preparation Depth and Design on Stress Distribution in Maxillary Central Incisors Restored with Ceramic Veneers: A 3D Finite Element Analysis. J. Prosthodont. 2020, 29, 151–160. [Google Scholar] [CrossRef]
- Quintas, A.F.; Oliveira, F.; Bottino, M.A. Vertical marginal discrepancy of ceramic copings with different ceramic materials, finish lines, and luting agents: An in vitro evaluation. J. Prosthet. Dent. 2004, 92, 250–257. [Google Scholar] [CrossRef]
- Ratnaweera, P.M.; Fukagawa, N.; Tsubota, Y.; Fukushima, S. Microtensile bond strength of porcelain laminate veneers bonded to fluorosed teeth. J. Prosthodont. 2009, 18, 205–210. [Google Scholar] [CrossRef]
- Runnacles, P.; Correr, G.M.; Baratto Filho, F.; Gonzaga, C.C.; Furuse, A.Y. Degree of conversion of a resin cement light-cured through ceramic veneers of different thicknesses and types. Braz. Dent. J. 2014, 25, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Haralur, S.B. Microleakage of porcelain laminate veneers cemented with different bonding techniques. J. Clin. Expr. Dent. 2018, 10, e166–e171. [Google Scholar]
- Sorrentino, R.; Ruggiero, G.; Borelli, B.; Barlattani, A.; Zarone, F. Dentin Exposure after Tooth Preparation for Laminate Veneers: A Microscopical Analysis to Evaluate the Influence of Operators’ Expertise. Materials 2022, 15, 1763. [Google Scholar] [CrossRef] [PubMed]
- Alhekeir, D.F.; Al-Sarhan, R.A.; Al Mashaan, A.F. Porcelain laminate veneers: Clinical survey for evaluation of failure. Saudi Dent. J. 2014, 26, 63–67. [Google Scholar] [CrossRef]
- de Bragança, G.F.; Mazao, J.D.; Versluis, A.; Soares, C.J. Effect of luting materials, presence of tooth preparation, and functional loading on stress distribution on ceramic laminate veneers: A finite element analysis. J. Prosthet. Dent. 2021, 125, 778–787. [Google Scholar] [CrossRef]
- Ioannidis, A.; Park, J.M.; Hüsler, J.; Bomze, D.; Mühlemann, S.; Özcan, M. An in vitro comparison of the marginal and internal adaptation of ultrathin occlusal veneers made of 3D-printed zirconia, milled zirconia, and heat-pressed lithium disilicate. J. Prosthet. Dent. 2022, 128, 709–715. [Google Scholar] [CrossRef]
- Aboushelib, M.N.; Elmahy, W.A.; Ghazy, M.H. Internal adaptation, marginal accuracy and microleakage of a pressable versus a machinable ceramic laminate veneers. J. Dent. 2012, 40, 670–677. [Google Scholar] [CrossRef]
- Gakis, P.; Kontogiorgos, E.; Zeller, S.; Nagy, W.W. Effect of firing and fabrication technique on the marginal fit of heat-pressed lithium disilicate veneers. J. Prosthet. Dent. 2022, 127, 154–160. [Google Scholar] [CrossRef]
- Yuce, M.; Ulusoy, M.; Turk, A.G. Comparison of Marginal and Internal Adaptation of Heat-Pressed and CAD/CAM Porcelain Laminate Veneers and a 2-Year Follow-Up. J. Prosthodont. 2019, 28, 504–510. [Google Scholar] [CrossRef]
- Pereira, D.D.; Marquezan, M.; Grossi, M.L.; Oshima, H.M.S. Analysis of Marginal Adaptation of Porcelain Laminate Veneers Produced by Computer-Aided Design/Computer-Assisted Manufacturing Technology: A Preliminary In Vitro Study. Int. J. Prosthod. 2018, 31, 346–348. [Google Scholar] [CrossRef]
- Guachetá, L.; Stevens, C.D.; Cardona, J.A.T.; Murgueitio, R. Comparison of marginal and internal fit of pressed lithium disilicate veneers fabricated via a manual waxing technique versus a 3D printed technique. J. Esthet. Restor. Dent. 2022, 34, 715–720. [Google Scholar] [CrossRef]
- Al-Dwairi, Z.N.; Alkhatatbeh, R.M.; Baba, N.Z.; Goodacre, C.J. A comparison of the marginal and internal fit of porcelain laminate veneers fabricated by pressing and CAD-CAM milling and cemented with 2 different resin cements. J. Prosthet. Dent. 2019, 121, 470–476. [Google Scholar] [CrossRef]
- Al-Akhali, M.; Kern, M.; Elsayed, A.; Samran, A.; Chaar, M.S. Influence of thermomechanical fatigue on the fracture strength of CAD-CAM-fabricated occlusal veneers. J. Prosthet. Dent. 2019, 121, 644–650. [Google Scholar] [CrossRef]
- El-Mowafy, O.; El-Aawar, N.; El-Mowafy, N. Porcelain veneers: An update. Dent. Med. Probl. 2018, 55, 207–211. [Google Scholar] [CrossRef]
- Abdulrahman, S.; Mahm, C.V.; Talabani, R.; Abdulateef, D. Evaluation of the clinical success of four different types of lithium disilicate ceramic restorations: A retrospective study. BMC Oral Health 2021, 21, 625. [Google Scholar] [CrossRef]
- Wolff, D.; Kraus, T.; Schach, C.; Pritsch, M.; Mente, J.; Staehle, H.J.; Ding, P. Recontouring teeth and closing diastemas with direct composite buildups: A clinical evaluation of survival and quality parameters. J. Dent. 2010, 38, 1001–1009. [Google Scholar] [CrossRef]
- Farias-Neto, A.; Gomes, E.M.; Sanchez-Ayala, A.; Sanchez-Ayala, A.; Vilanova, L.S. Esthetic Rehabilitation of the Smile with No-Prep Porcelain Laminates and Partial Veneers. Case Rep. Dent. 2015, 2015, 452765. [Google Scholar] [CrossRef] [PubMed]
- Novelli, C.; Scribante, A. Minimally Invasive Diastema Restoration with Prefabricated Sectional Veneers. Dent. J. 2020, 8, 60. [Google Scholar] [CrossRef] [PubMed]
- Chander, N.G.; Padmanabhan, T.V. Finite Element Stress Analysis of Diastema Closure with Ceramic Laminate Veneers. J. Prosthodont. 2009, 18, 577–581. [Google Scholar] [CrossRef] [PubMed]
- D’Arcangelo, C.; Vadini, M.; D’Amario, M.; Chiavaroli, Z.; De Angelis, F. Protocol for a new concept of no-prep ultrathin ceramic veneers. J. Esthet. Restor. Dent. 2018, 30, 173–179. [Google Scholar] [CrossRef]
- De Angelis, F.; D’Arcangelo, C.; Angelozzi, R.; Vadini, M. Retrospective clinical evaluation of a no-prep porcelain veneer protocol. J. Prosthet. Dent. 2023, 129, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.B.M.R. Conventional Versus Minimally Invasive Veneers: A Systematic Review. Cureus J. Med. Sci. 2023, 15, e44638. [Google Scholar]
- Ojeda, G.D.; Naves, L.; Oosterhaven, A.; Kleinsman, R.; Bäumer-König, A.; Körner, G.; Wendler, M.; Gresnigt, M. 8-year multicenter retrospective study on partial laminate veneers. J. Prosthodont. Res. 2023, 67, 206–213. [Google Scholar] [CrossRef]
- Chen, C.T.; Yang, B.; Yin, Y.X.; Wang, X.D.; Zhao, K. Maxillary midline diastema closure with sectional feldspathic porcelain veneers: A case series followed 1 to 4 years. J. Esthet. Restor. Dent. 2023, 35, 1022–1029. [Google Scholar] [CrossRef]
- Gresnigt, M.M.M.; Cune, M.S.; Jansen, K.; van der Made, S.A.M.; Özcan, M. Randomized clinical trial on indirect resin composite and ceramic laminate veneers: Up to 10-year findings. J. Dent. 2019, 86, 102–109. [Google Scholar] [CrossRef]
- Gresnigt, M.M.M.; Cune, M.S.; Schuitemaker, J.; van der Made, S.A.M.; Meisberger, E.W.; Magne, P.; Özcan, M. Performance of ceramic laminate veneers with immediate dentine sealing: An 11 year prospective clinical trial. Dent. Mater. 2019, 35, 1042–1052. [Google Scholar] [CrossRef]
- Jha, R.; Jain, V.; Das, T.K.; Shah, N.; Pruthi, G. Comparison of Marginal Fidelity and Surface Roughness of Porcelain Veneers Fabricated by Refractory Die and Pressing Techniques. J. Prosthodont. 2013, 22, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Wainwright, J.; Sheiham, A. An analysis of methods of toothbrushing recommended by dental associations, toothpaste and toothbrush companies and in dental texts. Br. Dent. J. 2014, 217, E5. [Google Scholar] [CrossRef]
- Thomassen, T.M.J.A.; Van der Weijden, F.G.A.; Slot, D.E. The efficacy of powered toothbrushes: A systematic review and network meta-analysis. Int. J. Dent. Hyg. 2022, 20, 3–17. [Google Scholar] [CrossRef]
- Rosentritt, M.; Sawaljanow, A.; Behr, M.; Kolbeck, C.; Preis, V. Effect of tooth brush abrasion and thermo-mechanical loading on direct and indirect veneer restorations. Clin. Oral Investig. 2015, 19, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.D.; Forjanic, M.; Ohmiti, K.; Rousson, V. Surface deterioration of dental materials after simulated toothbrushing in relation to brushing time and load. Dent. Mater. 2010, 26, 306–319. [Google Scholar] [CrossRef]
- Nam, N.E.; Shin, S.H.; Lim, J.H.; Shim, J.S.; Kim, J.E. Effects of Artificial Tooth Brushing and Hydrothermal Aging on the Mechanical Properties and Color Stability of Dental 3D Printed and CAD/CAM Materials. Materials 2021, 14, 6207. [Google Scholar] [CrossRef]
- Daghrery, A. Color Stability, Gloss Retention, and Surface Roughness of 3D-Printed versus Indirect Prefabricated Veneers. J. Funct. Biomater. 2023, 14, 492. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Xu, Y.; Zhang, J.; Chen, X.; Liang, W.; Liu, X.; Xian, J.; Xie, H. Comparison of the effectiveness between power toothbrushes and manual toothbrushes for oral health: A systematic review and meta-analysis. Acta Odontol. Scand. 2020, 78, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Yuan, J.C.; Barão, V.A.R.; Wee, A.G.; Alfaro, M.F.; Afshari, F.S.; Sukotjo, C. Effect of brushing and thermocycling on the shade and surface roughness of CAD-CAM ceramic restorations. J. Prosthet. Dent. 2018, 72, 1000–1006. [Google Scholar] [CrossRef] [PubMed]
- Soteriou, D.; Ntasi, A.; Papagiannoulis, L.; Eliades, T.; Zinelis, S. Decomposition of Ag-based soldering alloys used in space maintainers after intra-oral exposure. A retrieval analysis study. Acta Odontol. Scand. 2014, 72, 130–138. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).