Abstract
Although many randomized controlled trials (RCT) have evaluated the efficacy of powered or electric toothbrushes compared with manual or traditional toothbrushes to remove biofilm and plaque, only one systematic review has been published for pediatric patients. The primary objective of this study was to perform a systematic review and meta analysis for this population. Using the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) protocol, N = 321 studies were initially identified. Three independent, blinded abstract reviews were completed resulting in a total of n = 38/322 or 11.8% for the final analysis (n = 27 non-orthodontic, n = 11 orthodontic studies). Meta analysis of these outcome data have revealed a strong reduction in plaque index scores among pediatric patients using electric toothbrushes of approximately 17.2% for non-orthodontic patients and 13.9% for orthodontic patients. These results provide strong clinical evidence for recommending electric toothbrushing to pediatric patients, as well as those patients undergoing orthodontic therapy and treatment.
1. Introduction
Many randomized controlled trials (RCT) have evaluated the efficacy of powered or electric toothbrushes compared with manual or traditional toothbrushes to remove biofilm and plaque [1,2]. As many of these studies involved adults, there are also multiple lines of evidence to demonstrate the effect of powered or electric toothbrushes to improve or prevent gingivitis and early periodontitis [3,4,5]. The depth and breadth of research in this area has allowed multiple systematic reviews and meta analyses to be conducted on this topic, mainly focusing on adult patients and the improvements to oral health [6,7,8].
Due to the breadth and depth of research on the effectiveness of electric (powered) toothbrushes to reduce biofilm and plaque in adults, many research groups have also evaluated these effects among adolescents—although most of this research has focused on orthodontic patients [9,10,11]. These studies have also led to systematic reviews and meta analyses that provide for plaque control and biofilm reduction among this specific population, which includes both pediatric and adult patients [12,13,14]. However, the evidence comparing manual versus electric (powered) toothbrushes among pediatric patients without fixed orthodontic appliances is less robust [15,16,17].
However, despite evidence comparing these methods in pediatric patients, only one systematic review has been published for this specific population subgroup [18]. Although this review encompassed nine well-executed studies on the effectiveness of electric versus manual toothbrushing in pediatric patients, an expanded search has revealed additional studies published before and after this review was completed, which significantly increase the total number of available studies for inclusion [15,16,17]. In addition, an analysis of the cited references from each of these studies also led to additional resources for this systematic review. Finally, the evidence of strong correlation between the major plaque indices, including the Rustogi et al. Modified Navy Plaque Index (RMNPI) and the Turesky et al. Modification of the Quigley Hein Plaque Index(TQHPI), allowed for these many differing studies to be analyzed in this review [19].
Based upon this information, the primary objective of this study is to perform an expanded systematic review and meta analysis to answer the clinical research question “Do pediatric patients (Population) using powered or electric toothbrushes (Intervention) compared with manual or traditional toothbrushes (Comparison) exhibit reduced plaque indices (Outcome).”
2. Materials and Methods
2.1. Human Subjects Approval
This study was reviewed and approved as Exempt by the Institutional Review Board (IRB) and Office for the Protection of Research Subjects (OPRS) under protocol [1619329-1] titled Retrospective analysis of Oral Health Status of Dental Population on 24 July 2020.
2.2. PRISMA Protocol
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines and protocol [20,21]. The National Library of Medicine (NLM) and PubMed databases were searched using Medical Subject Headings (MeSH), which are appropriate for controlled vocabulary indexing of published evidence relating to pediatric toothbrushing. The Boolean search terms used to search for relevant articles included the following, using AND/OR operators: “Pediatric”, “Children”, “Electric toothbrush”, “Powered toothbrush”, “Manual toothbrush”, “Traditional toothbrush”, “Primary dentition”, and “Mixed dentition”. Cited references from each of the studies identified were also evaluated to determine any potential resources not identified through the initial database search results.
The inclusion criteria were those related to human subjects that were pediatric patients (<18 years of age) in a dental setting using manual versus electric toothbrushes. Exclusion criteria included non-human subjects (animal or in vitro studies), studies involving only adult patients (>18 years of age), non-dental clinical applications (ex vivo), or study settings involving a second party, such as disabled or physically impaired patients. Studies that did not include measurements of plaque index, including Rustogi et al. Modified Navy Plaque Index (RMNPI), Silness-Loe plaque index (SLPI), or the Turesky et al. Modification of the Quigley Hein Plaque Index (TQHPI), were also excluded. All relevant articles were imported into an online system (Rayyan.ai) for comparison and analysis by the study authors.
2.3. Two-Step Review
This process was initially performed by the lead author and then separately and independently performed and confirmed by the second and third authors. Any discrepancies and questions were marked for discussion and review, which did not influence the final articles selected. The final articles selected were agreed upon by all three reviewers prior to the full-text review of each study.
2.4. Data Analysis
Data regarding plaque index were extracted from each study and presented in both table and graphic formats. Baseline (starting) measurements were compared with manual (control) and electric or powered (experimental) toothbrushing for each study endpoint (outcome). To enable analysis of studies using different plaque indices, including the Rustogi et al. Modified Navy Plaque Index or RMNPI, Silness-Loe plaque index or SLPI, and the Turesky et al. modification of the Quigley Hein Plaque Index or TQHPI, percent changes between baseline and control or experimental groups were used to determine the relative effect (RE) of electric versus manual toothbrush use. Pediatric studies including patients undergoing orthodontic therapy that involved the use of fixed brackets were analyzed separately from the studies involving pediatric patients without any orthodontic appliances.
3. Results
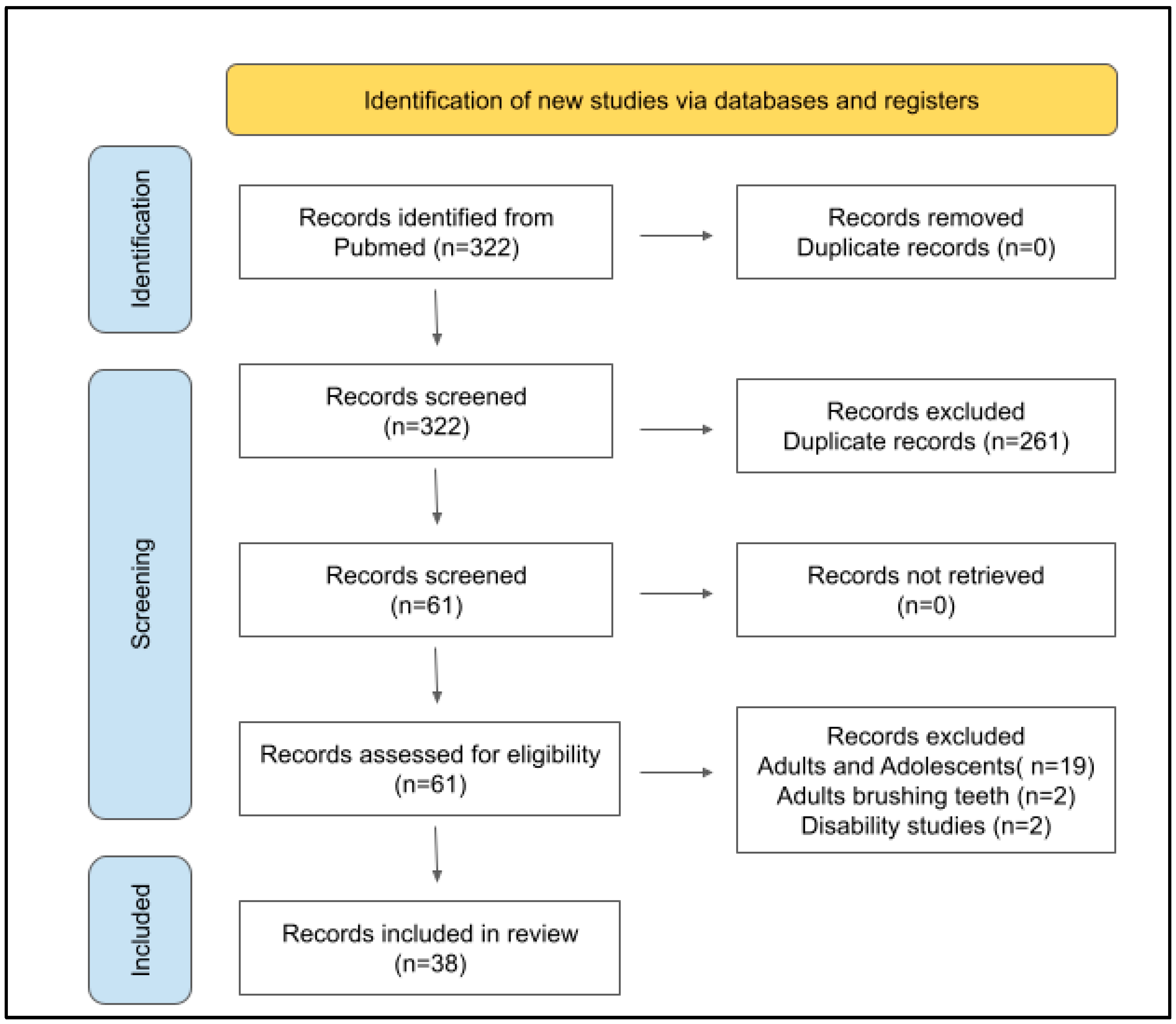
Using the PRISMA protocol and PubMed search strategy, a total of n = 309 citations were found using the operators “Pediatric”, “Electric toothbrush”, “Powered toothbrush”, “Manual toothbrush”, and “Traditional toothbrush” and no duplicate entries were identified (Figure 1). The results were then screened by each reviewer independently, which resulted in more than half of the citations being excluded by all three reviewers upon initial review (n = 194/322 or 60.2%). The remaining studies where one or two reviewers disagreed (n = 67/322 or 20.8%) were reviewed together by all three reviewers. The total number of studies excluded at the review stage was n = 261/322 or 81.1%, with n = 61/322 or 18.9% marked for further review and full-text analysis.
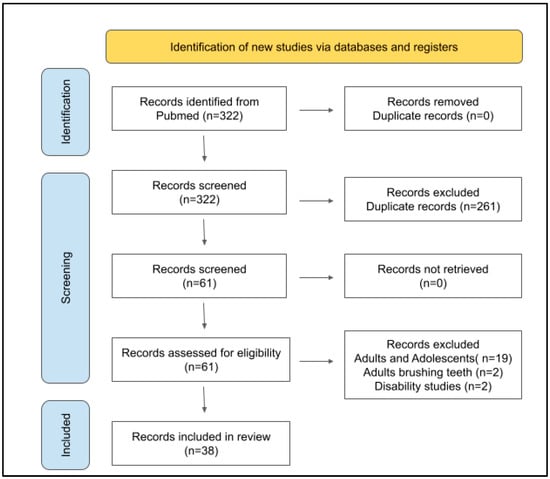
Figure 1.
PRISMA protocol flow diagram of the literature review. Using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol, the search in PubMed yielded a total of n = 322 research papers. Application of the inclusion and exclusion criteria reduced the number of articles to n = 60 for full-text retrieval. Final review of these studies and outcome measures resulted in n = 38/322 or 11.8% included in this systematic review.
Following the retrieval of full-text articles for all studies, n = 19 studies were excluded after review of the study parameters including many studies involving participants that included both adolescents and adults over 18 years of age. In addition, two studies were excluded from this review following data extraction, which revealed these studies included adults brushing the teeth for their children and two more studies involved children that were disabled and unable to brush their teeth without assistance. The remaining studies n = 38/322 or 11.8% were included in this review.
Full text reviews of all non-orthodontic pediatric studies (n = 27) were completed (Table 1). The analysis of data from all studies provided the year of the study publication, which ranged from 1967 to 2021. Sample sizes from each study were also evaluated, which ranged from n = 12 to n = 200 and averaged n = 60.2. The age ranges from each study varied from patients as young as two years old up to and including patients 17 years of age. Finally, all studies included in this systematic review had baseline and final outcome measures for control (manual) and experimental (electric/powered) groups using versions of the Rustogi et al. Modified Navy Plaque Index (RMNPI), the Silness-Loe plaque index (SLPI), or the Turesky et al. Modification of the Quigley Hein Plaque Index (TQHPI) to provide systematic objective criteria for comparison. These data demonstrated relative effects (electric versus manual toothbrush) on plaque index outcomes ranging from 0.5% to 35.4% that averaged 17.2%.

Table 1.
Characteristics of pediatric, non-orthodontic inclusion studies.
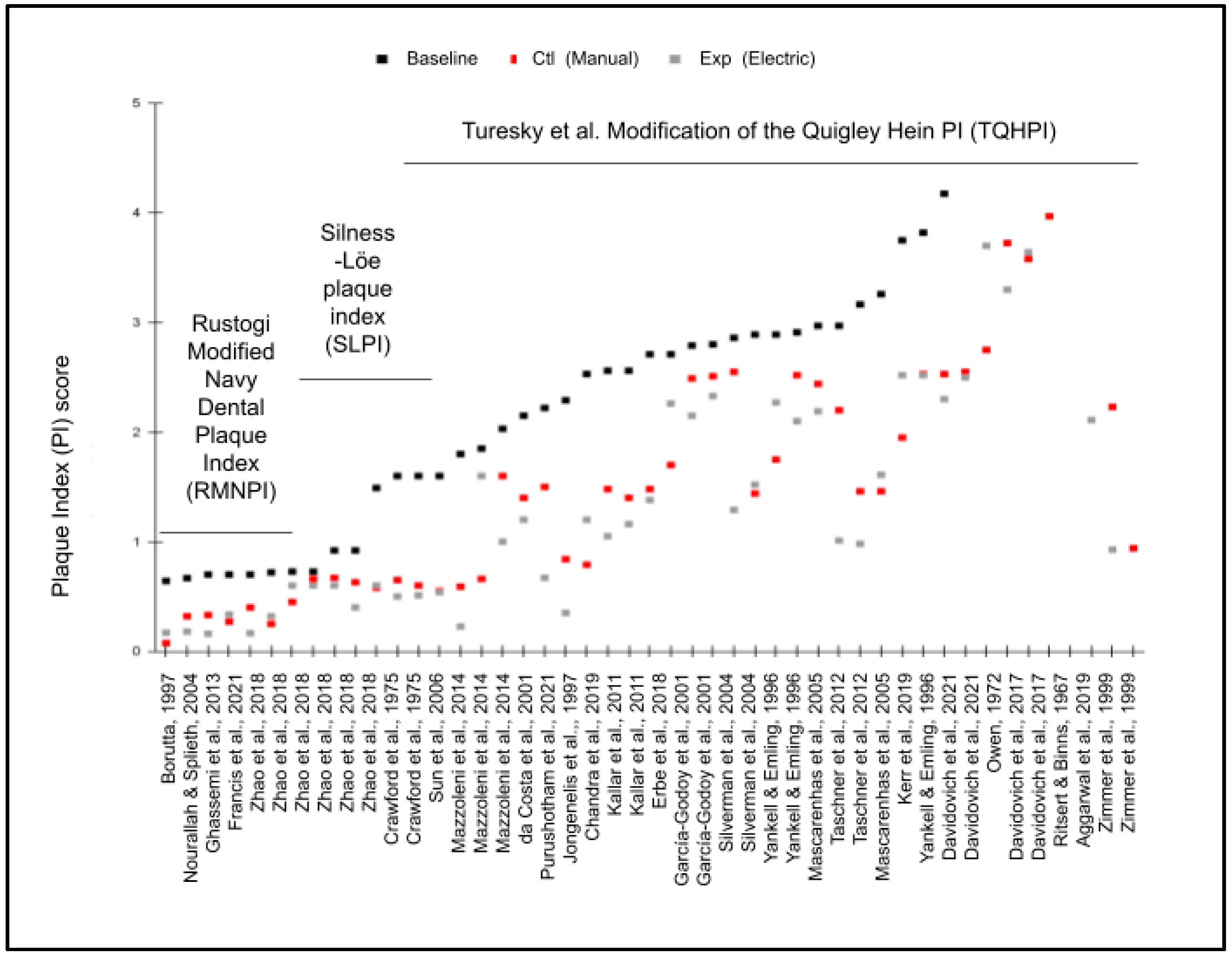
The plaque index data were extracted from each of the studies where baseline and endpoint plaque indices were provided (Figure 2). Four of the studies used the Rustogi et al. Modified Navy Plaque Index (RMNPI), four used the Silness-Loe plaque index (SLPI), with most of the remainder (n = 15) using the Turesky et al. Modification of the Quigley Hein Plaque Index (TQHPI). Although some of the studies included multiple outcome data points (different trial lengths) and scales differed among each of the individual studies, these results demonstrate that every study demonstrated more significant reductions in the plaque index using electric toothbrushes compared with manual toothbrushes.
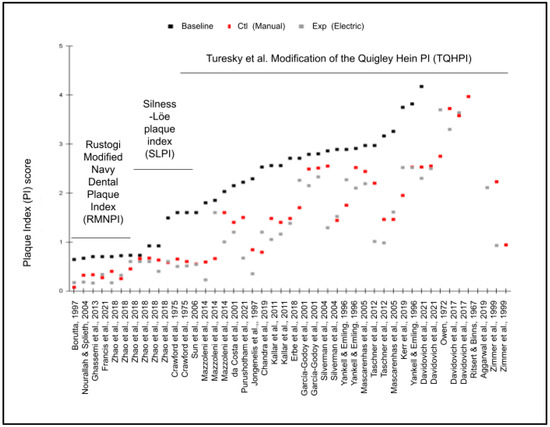
Figure 2.
Graphic display of baseline and endpoint plaque indices. Baseline and endpoints from studies with Rustogi et al. Modified Navy Plaque Index (RMNPI, n = 8), Silness-Loe plaque index (SLPI, n = 6), and the Turesky et al. Modification of the Quigley Hein Plaque Index (TQHPI, n = 30) each demonstrated more significant reductions in the plaque index with the experimental variable (Exp) electric toothbrushes compared with the control (Ctl) variable manual toothbrushes [22,23,24,25,26,27,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48].
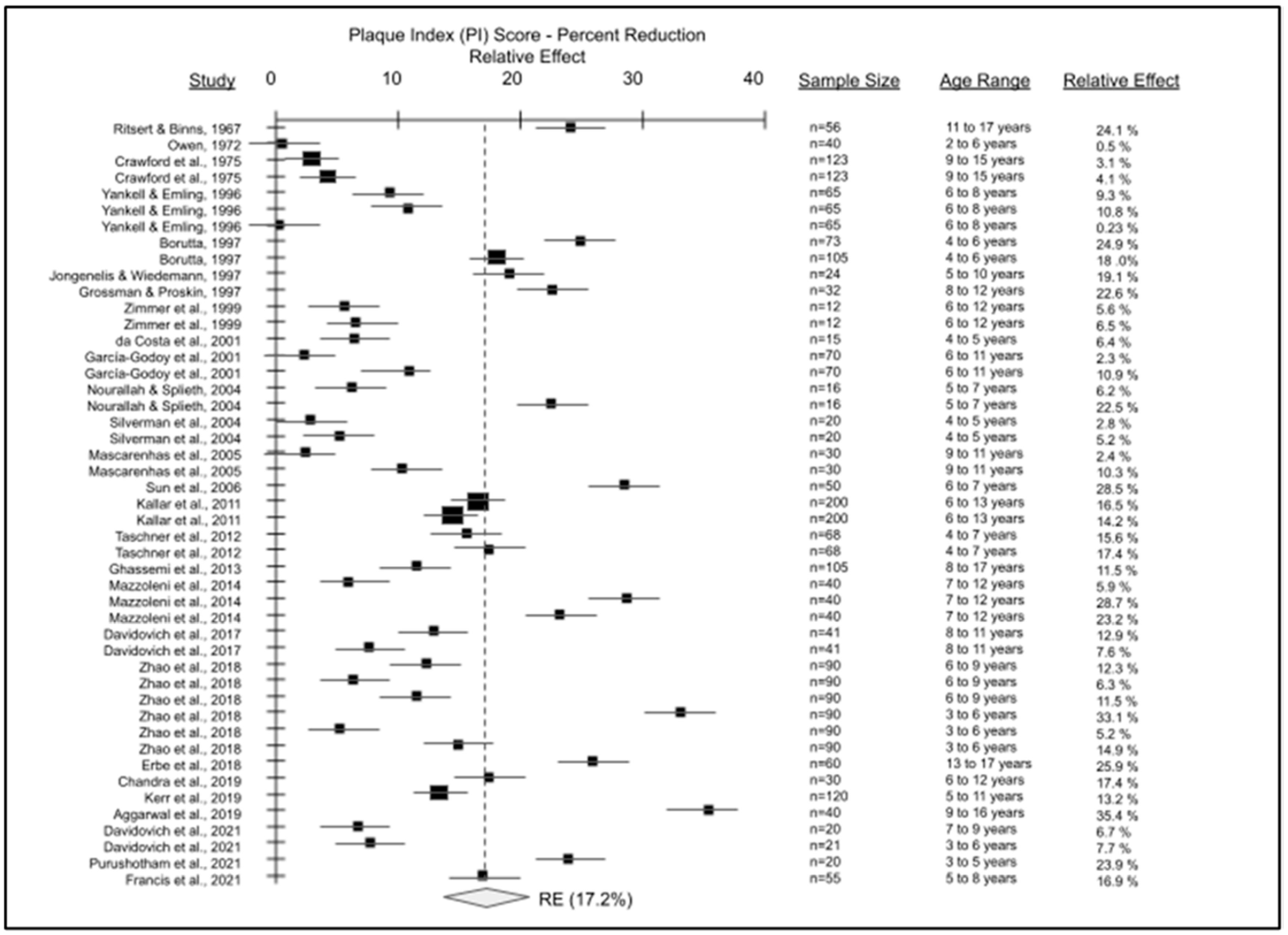
The data from the final articles included for pediatric, non-orthodontic studies were combined to create the forest plot of plaque index score reductions comparing electric versus manual toothbrushes (Figure 3). Detailed analysis of the forest plot for the meta analysis outcome variable has revealed a strong reduction in plaque index scores among pediatric patients using electric toothbrushes compared with manual toothbrushes. Comparison of the baseline measurements compared with the manual toothbrush endpoint measurements revealed no statistical significance (p = 0.065), but comparison of baseline measurements with electric toothbrush endpoint measurements revealed statistically significant results (p = 0.0073). Percent reduction in plaque index scores from these RCT demonstrated comparative reductions in plaque with electric versus manual toothbrushes ranging from 0.23% to 35.4%, yielding an average reduction or relative effect (RE) of 17.2%.
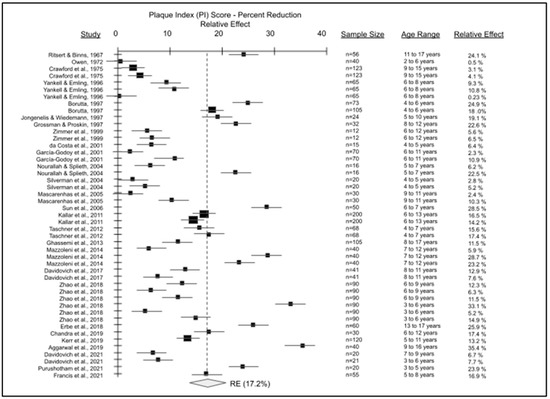
Figure 3.
Forest plot of pediatric, non-orthodontic studies of manual versus electric toothbrushing comparing plaque index (PI). A total of 27 studies were evaluated with sample sizes ranging from n = 12 to n = 200 were plotted to determine an average reduction in plaque index or relative effect (RE) with electric toothbrush use of approximately 17.2%, p = 0.0073 [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48].
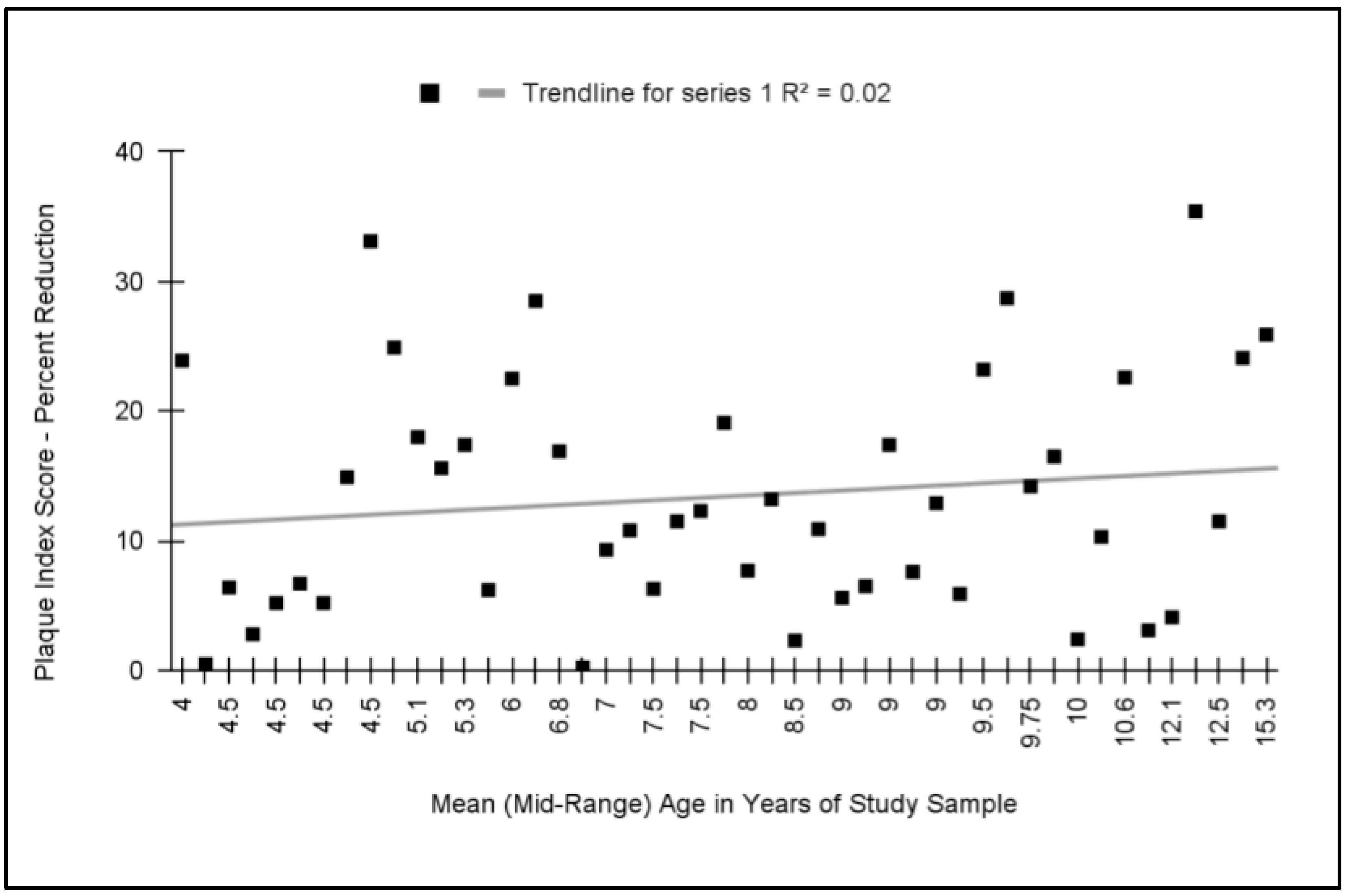
To determine if any relationship exists between the relative effect and the mean or mid-range age of the study sample participants, these data were graphed and analyzed (Figure 4). The analysis of these data demonstrated that no significant relationship exists between these variables with a coefficient of determination (R2 = 0.02). Outcomes from studies with the average or mid-range age of participants between the ages of two and six (n = 16) exhibited an average relative reduction in plaque index (comparing electric with manual toothbrushes) of 13.6%, which was not significantly different from those outcomes from studies with the average or mid-range age of participants between six and seventeen years old (n = 30) that exhibited a reduction of 13.3%, p = 0.899.
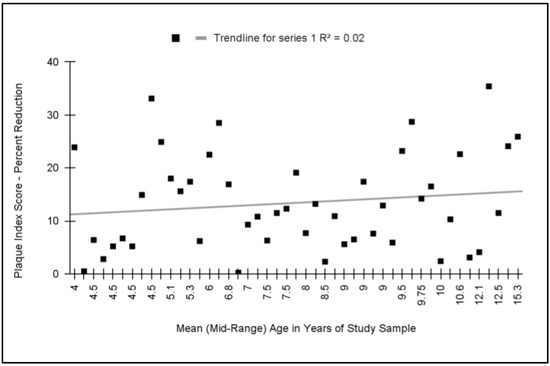
Figure 4.
Meta analysis of relative effect (percent reduction in plaque index) plotted against average or mid-range age of study participants. No significant association was found between these variables with a coefficient of determination, R2 = 0.02. Studies with the average age of participants under six and over six years of age exhibited similar reductions in plaque index with electric toothbrushes (13.5% and 13.3%, respectively), p = 0.899.
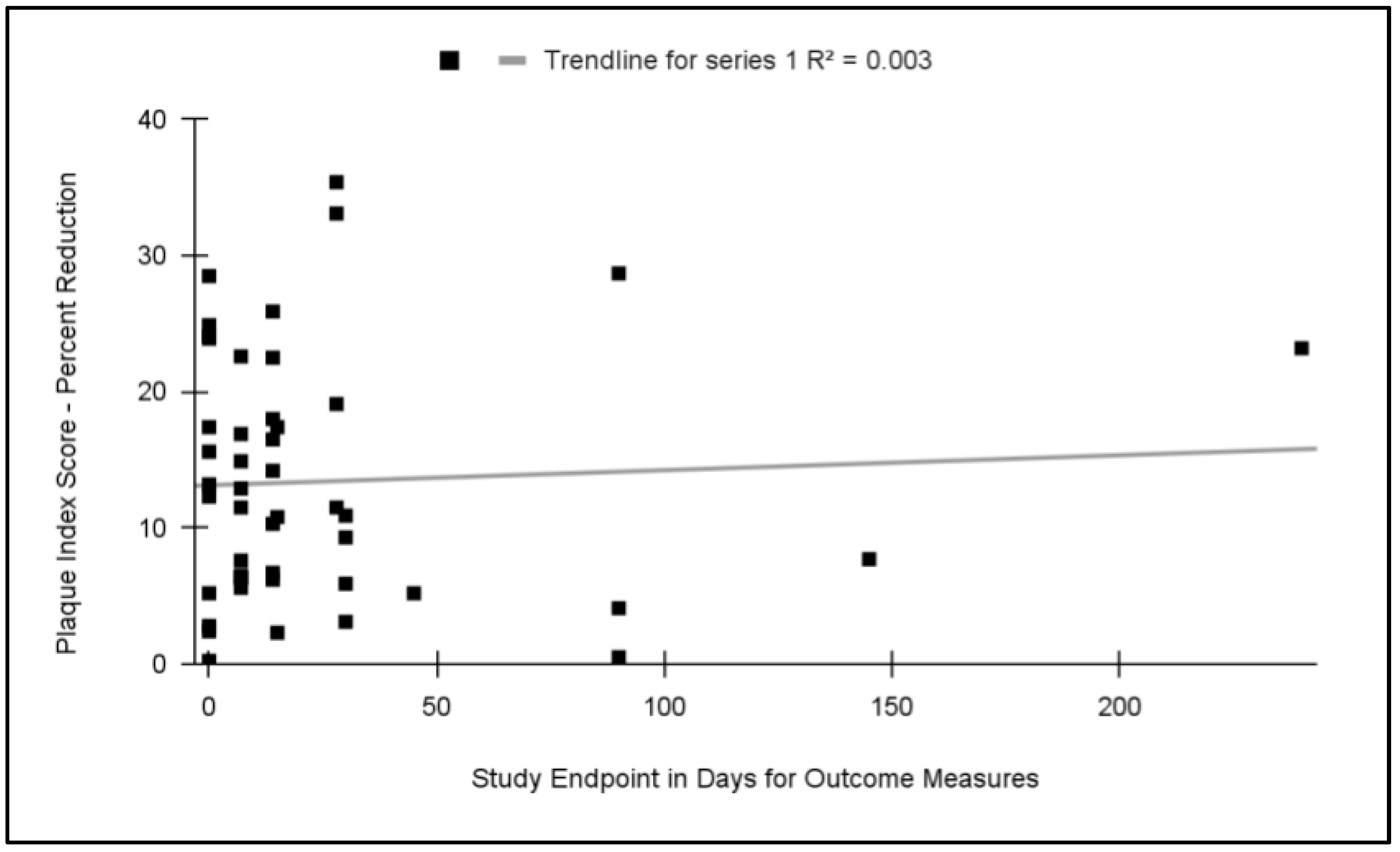
To evaluate the potential effects on the study outcomes related to the length of study (endpoint measures), these data were graphed and analyzed (Figure 5). This analysis revealed that no significant relationship exists between the length of the study and the relative effect (R2 = 0.003). More specifically, the average relative effect (plaque index reduction) among the 0 day trials (14.2%) was not significantly different from the average of trials lasting one to two weeks (13.8%), p = 0.711, or trials lasting 30 days or longer (14.1%), p = 0.92.
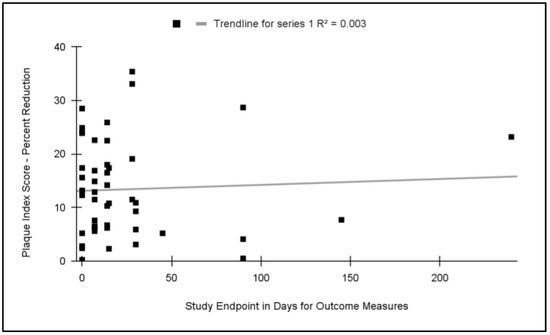
Figure 5.
Meta analysis of relative effect (percent reduction in plaque index) plotted against study length (endpoint measures). No significant association was found between these variables with a coefficient of determination, R2 = 0.003. Studies lasting 0 days exhibited similar average plaque reduction effects (14.2%) as those lasting 7 to 14 days (13.8%), p = 0.711, or 30 days and longer (14.1%), p = 0.92.
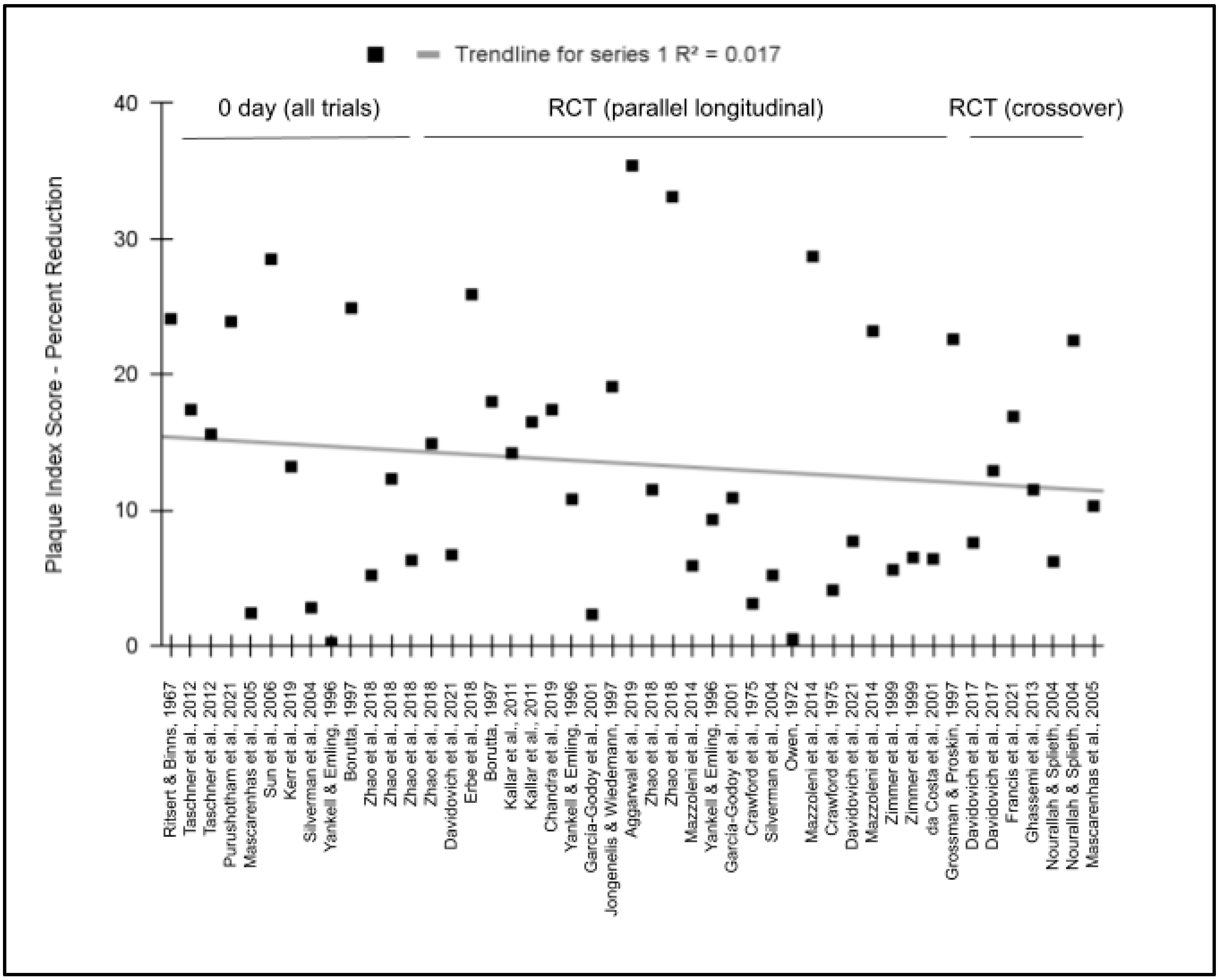
To evaluate the potential effects on the study outcomes related to the study design, these data were graphed and analyzed (Figure 6). This analysis revealed that no significant relationship exists between the type of the study (such as longitudinal parallel RCTs and crossover RCT) and the relative effect (R2 = −0.017). More specifically, the average relative effect (plaque index reduction) among all of the zero day trials (14.2%) was not significantly different from the average of longitudinal parallel RCTs lasting any length of time (13.2%), p = 0.767, or crossover RCTs regardless of length (12..9%), p = 0.735.
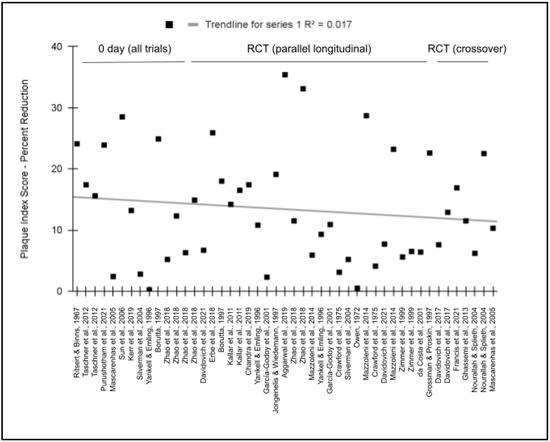
Figure 6.
Meta analysis of relative effect (percent reduction in plaque index) plotted against study design. No significant association was found between these variables with a coefficient of determination, R2 = −0.017. Studies lasting 0 days exhibited similar average plaque reduction effects (14.2%) as longitudinal RCTs (13.2%), p = 0.767, and crossover RCTs (12.9%), p = 0.735 [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48].
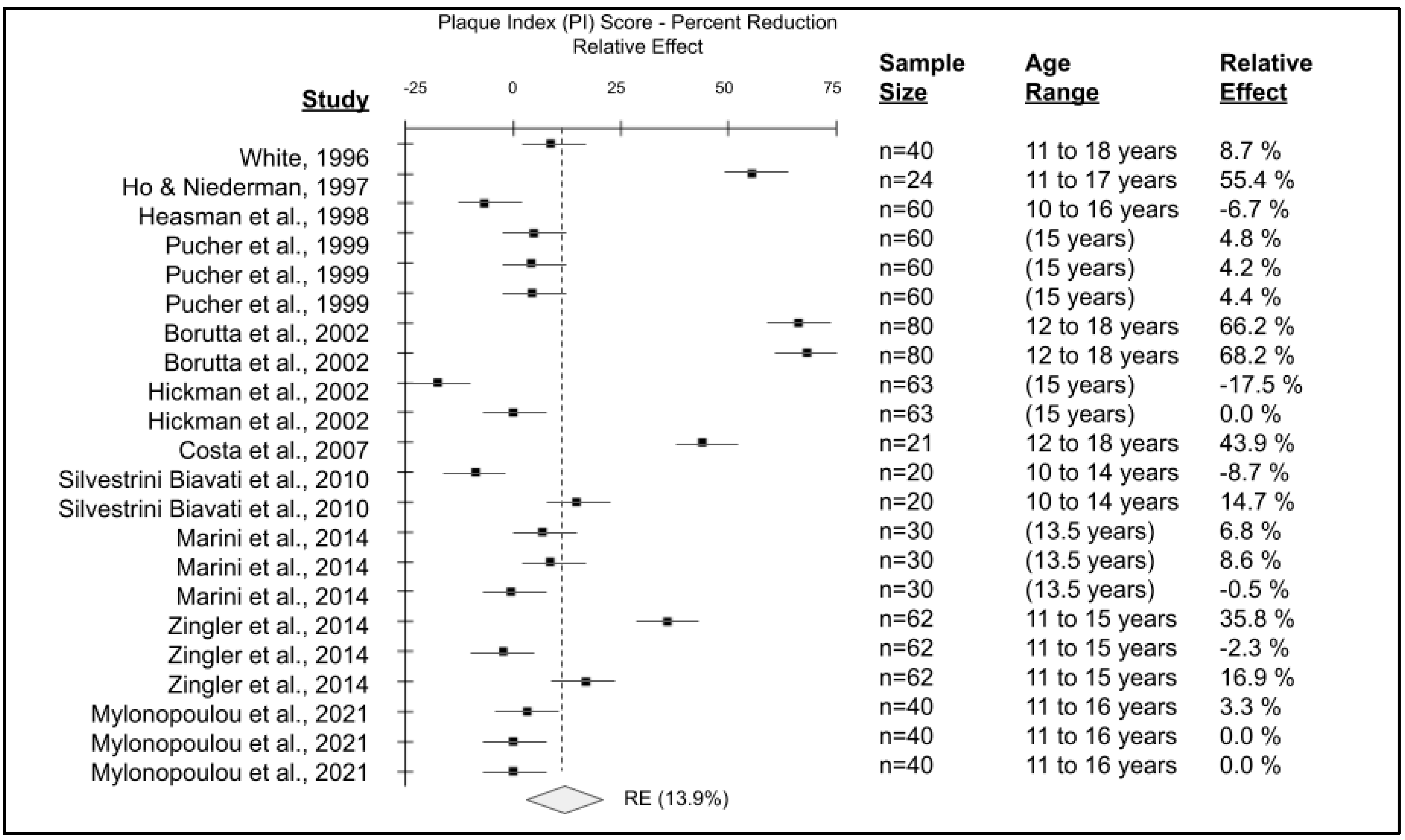
Full text reviews of all orthodontic pediatric studies (n = 11) were completed (Table 2). Analysis of these studies revealed a range of publication dates between 1996 and 2021. Sample sizes from each study were also evaluated, which ranged from n = 20 to n = 80, averaging n = 45.5, and yielding a total combined sample size of n = 500. Finally, the comparison of control (manual) and experimental (electric/powered) groups using various plaque indexes, including the Silness-Loe plaque index (SLPI) and the Turesky et al. Modification of the Quigley Hein Plaque Index (TQHPI), demonstrated relative effects on plaque index scores for orthodontic patients ranging from −17.5% to 68.2% that averaged 13.9%.

Table 2.
Characteristics of pediatric, orthodontic inclusion studies.
The data from the final articles included for pediatric, orthodontic studies were combined to create the forest plot of plaque index score reductions comparing electric versus manual toothbrushes (Figure 7). Detailed analysis of the outcome variable has revealed variable reductions in plaque index scores among pediatric orthodontic patients using electric toothbrushes compared with manual toothbrushes. Comparison of the baseline measurements compared with the manual toothbrush orthodontic endpoint measurements revealed no statistical significance (p = 0.12), but comparison of baseline measurements with electric toothbrush orthodontic endpoint measurements revealed statistically significant results (p = 0.035). Changes in plaque index scores from these RCT demonstrated comparative reductions in plaque with electric versus manual toothbrushes ranging from −17.5% to 68.2%, yielding an average reduction or relative effect (RE) of 13.9%.
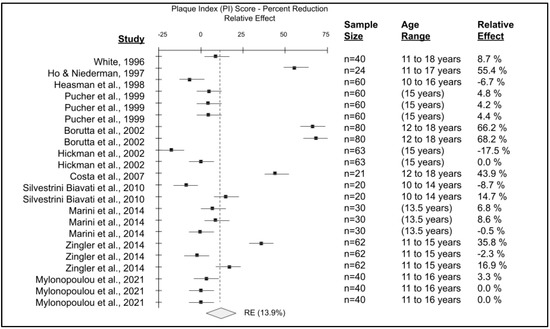
Figure 7.
Forest plot of pediatric, orthodontic studies of manual versus electric toothbrushing comparing plaque index (PI). A total of n = 11 studies were evaluated with sample sizes ranging from n = 20 to n = 80 were plotted to determine an average reduction in plaque index or relative effect (RE) with electric toothbrush use of approximately 13.9%, p = 0.035 [49,50,51,52,53,54,55,56,57,58,59].
Most of the studies had patients with similar ages, with the youngest patients in each RCT between 10 and 16 years of age and the oldest between 12 and 17.9 years of age. Analysis of study sample age and plaque index outcomes revealed no significant associations (R2 = 0.043). Similarly, analysis of sample size with plaque index outcomes revealed no significant association (R2 = 0.029), as most of the sample sizes were relatively small (between n = 20 and n = 80).
To evaluate the potential bias in all of the studies (non-orthodontic, orthodontic), specific characteristics of each study were extracted for comparison (Table 3). These data demonstrated that the majority of studies (n = 25/38 or 65.7%) included in this review had low selection bias (randomized controlled trials), although some studies did use randomized selection from a convenience sample (n = 12/38 or 34.2%). In addition, the vast majority (n = 36/38 or 94.7%) had low or very low attrition rates, which provides evidence that completion bias was not a significant influence on the results of these studies. Finally, most studies used two or more blinded operators for the evaluation of patients, with some studies using the same blinded operator (not knowing which group the patient belonged to).

Table 3.
Potential bias of all pediatric inclusion studies.
4. Discussion
To date, few studies have systematically reviewed all relevant evidence to evaluate the clinical question regarding the relative effect of electric versus manual toothbrushes to reduce plaque indices within the pediatric patient population [18]. This review significantly increases the total number of subjects evaluated by nearly 1000 [22,23,24,28,32,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59]. In addition, by focusing on this specific outcome measure (plaque index scores) the current systematic review also provides a more direct and meaningful comparison of clinical patient outcomes—an estimate of the average plaque coverage of all tooth surfaces expressed as either a numeric percentage or on a predefined scale (e.g., 0 to 3 or 0 to 5) [60,61].
These results suggest that even among children as young as two years of age, use of electric toothbrushes can provide significant improvements in plaque index score [6,18]. Moreover, these data suggest that these improvements appear to remain constant over the age range evaluated (2 to 17 years of age), which suggests that even very young patients may experience clinical improvements in plaque reduction from early introduction to powered toothbrushes [12,18]. In addition, the separate analysis of study length also suggests that clinically relevant reductions in plaque can be demonstrated as early as the first day, which continue regardless of the time period evaluated [60,61,62,63]
The results of this study also provided subgroup analysis of orthodontic pediatric patients from randomized controlled trials that also demonstrated clinical reduction in plaque index scores among non-orthodontic patients. These data confirm previous observations from systematic reviews and meta analyses, although the most recent of these focusing exclusively on pediatric patients was completed in 2008 [62,63]. Moreover, these results provide further support for the most recent published guidelines and recommendations from clinical practitioners regarding the recommendation for electric or powered toothbrushes for pediatric patients [13,64,65].
Despite the significance of these findings and the relevance of having an updated and expanded systematic review and meta analysis of these outcomes, there are some limitations implicit in this study that should also be considered. For example, many of these studies used different types of toothbrushes that may have influenced the specific outcomes in those RCT [66,67]. In addition, some of these studies also included hygiene instruction and other behavioral interventions that may have the potential to impact the outcomes measured in these trials [68,69]. Finally, differences in the study design, such as the number of clinical observers or operators, as well as minor differences in the type of plaque indices used, such as the percentage-based Simplified Oral Health Index or the scale-based indices including the Rustogi Modified Navy Plaque Index (RMNPI), Silness-Loe plaque index (SLPI), and the original or Turesky modification of the Quigley Hein Plaque Index (TQHPI) may produce small variations in outcome measurements [70].
5. Conclusions
This systematic review combines the results of multiple non-orthodontic and orthodontic studies to provide an updated and more expansive evaluation of the relative effectiveness of electric versus manual toothbrushes among pediatric patients. This analysis demonstrates the clinical utility of using electric toothbrushes among patients as young as two years of age—with strong evidence that these effects may be consistent up to age seventeen.
Author Contributions
A.G., T.G., M.K., and KK. were responsible for methodology, data curation, investigation, formal analysis, writing—original draft preparation, and writing—review and editing. K.K. was responsible for conceptualization, methodology, resources, data curation, formal analysis, supervision, and writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
The APC was funded by the Office of Research at the University of Nevada, Las Vegas—School of Dental Medicine and the Department of Advanced Education—Pediatric Dental Residency Program. Karl Kingsley is co-investigator on the National Institute of Health (NIH) grant R15DE028431.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and was reviewed and approved by the University of Nevada, Las Vegas (UNLV) Institutional review board (IRB) under protocol [1619329-1] titled “Retrospective analysis of Oral Health Status of Dental Population” on 24 July 2020. This retrospective analysis of previously published data regarding pediatric patient populations was deemed exempt pursuant to the Basic Health and Human Services (HHS) Policy for the Protection of Human Research Subjects (46.101) regarding IRB exemption for research that involves the study of existing data, documents or records that currently exist and are not prospectively collected and in which 1. participants cannot be directly identified and 2. participants cannot be identified through identifiers linked to them.
Informed Consent Statement
Informed Consent was waived due to the exemption to retrospective human subjects research (46.101) regarding IRB exemption for research involving existing samples in which subjects cannot be identified directly or through identifiers.
Data Availability Statement
The data presented in this study are publicly available from PubMed. All of the study data are indexed and were accessed by the study authors online.
Acknowledgments
The authors would like to acknowledge the presentation of preliminary data from this manuscript by T.G. at the International Association for Dental Research (IADR) conference in 2021.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Grender, J.; Goyal, C.R.; Qaqish, J.; Timm, H.; Adam, R. A 12-Week Randomized Controlled Trial Comparing a Novel Electric Toothbrush with an Extra Gentle Brush Head to a Manual Toothbrush for Plaque and Gingivitis Reduction. Compend. Contin. Educ. Dent. 2022, 43, f20–f29. [Google Scholar] [PubMed]
- Nevins, M.; Chen, C.Y.; Kerr, E.; Mendoza-Azpur, G.; Isola, G.; Soto, C.P.; Stacchi, C.; Lombardi, T.; Kim, D.; Rocchietta, I. Comparison of a Novel Sonic Toothbrush to Manual Brushing on Plaque Control and Gingival Inflammation: A Multicenter, Randomized, Controlled Clinical Trial. Int. J. Periodontics Restor. Dent. 2021, 41, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Adam, R.; Grender, J.; Timm, H.; Qaqish, J.; Goyal, C.R. Anti-gingivitis and Anti-plaque Efficacy of an Oral Hygiene System: Results from a 12-Week Randomized Controlled Trial. Compend. Contin. Educ. Dent. 2021, 42, e1–e4. [Google Scholar] [PubMed]
- Zini, A.; Mazor, S.; Timm, H.; Barker, M.L.; Grender, J.M.; Gerlach, R.W.; Biesbrock, A.R. Effects of an oral hygiene regimen on progression of gingivitis/early periodontitis: A randomized controlled trial. Can. J. Dent. Hyg. 2021, 55, 85–94. [Google Scholar]
- Ramseier, C.A.; Petitat, C.; Trepp, S.; Lang, N.P.; Eick, S.; Adam, R.; Ccahuana-Vasquez, R.A.; Barker, M.L.; Timm, H.; Klukowska, M.; et al. Clinical Parameters and Oral Fluid Biomarkers in Gingivitis Subjects using an Electric Toothbrush with Irrigator vs. a Manual Toothbrush Alone over 8 Weeks: A Randomised Controlled Clinical Trial. Oral Health Prev. Dent. 2021, 19, 137–147. [Google Scholar] [CrossRef]
- Thomassen, T.M.; Van der Weijden, F.G.; Slot, D.E. The efficacy of powered toothbrushes: A systematic review and network meta-analysis. Int. J. Dent. Hyg. 2022, 20, 3–17. [Google Scholar] [CrossRef]
- Ying, Y.; Nicolau, B. Oscillating-rotating electric toothbrushes may have a better effect on gingivitis and plaque control than sonic and manual toothbrushes in adults. J. Evid. Based Dent. Pract. 2021, 21, 101575. [Google Scholar] [CrossRef]
- Grender, J.; Adam, R.; Zou, Y. The effects of oscillating-rotating electric toothbrushes on plaque and gingival health: A meta-analysis. Am. J. Dent. 2020, 33, 3–11. [Google Scholar]
- Nathoo, S.; Mankodi, S.; Mateo, L.R.; Chaknis, P.; Panagakos, F. A clinical study comparing the supragingival plaque and gingivitis efficacy of a specially engineered sonic powered toothbrush with unique sensing and control technologies to a commercially available manual flat-trim toothbrush. J. Clin. Dent. 2012, 23, A11–A16. [Google Scholar]
- Farhadian, N.; Bidgoli, M.; Jafari, F.; Mahmoudzadeh, M.; Yaghobi, M.; Miresmaeili, A. Comparison of Electric Toothbrush, Persica and Chlorhexidine Mouthwashes on Reduction of Gingival Enlargement in Orthodontic Patients: A Randomised Clinical Trial. Oral Health Prev. Dent. 2015, 13, 301–307. [Google Scholar] [CrossRef]
- Clerehugh, V.; Williams, P.; Shaw, W.C.; Worthington, H.V.; Warren, P. A practice-based randomised controlled trial of the efficacy of an electric and a manual toothbrush on gingival health in patients with fixed orthodontic appliances. J. Dent. 1998, 26, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Sivaramakrishnan, G.; Alsobaiei, M.; Sridharan, K. Powered toothbrushes for plaque control in fixed orthodontic patients: A network meta-analysis. Aust. Dent. J. 2021, 66, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Preda, C.; Butera, A.; Pelle, S.; Pautasso, E.; Chiesa, A.; Esposito, F.; Oldoini, G.; Scribante, A.; Genovesi, A.M.; Cosola, S. The Efficacy of Powered Oscillating Heads vs. Powered Sonic Action Heads Toothbrushes to Maintain Periodontal and Peri-Implant Health: A Narrative Review. Int. J. Environ. Res. Public Health 2021, 18, 1468. [Google Scholar] [CrossRef]
- Nathoo, S.; Mateo, L.R.; Chaknism, P.; Kemp, J.H.; Gatzemeyer, J.; Morrison, B.M., Jr.; Panagakos, F. Efficacy of two different toothbrush heads on a sonic power toothbrush compared to a manual toothbrush on established gingivitis and plaque. J. Clin. Dent. 2014, 25, 65–70. [Google Scholar] [PubMed]
- Chicalé-Ferreira, A.B.; Palma-Dibb, R.G.; Faraoni, J.J.; Gatón-Hernández, P.; Silva, L.A.D.; Silva, R.A.D.; de Queiroz, A.M.; Lucisano, M.P.; Nelson-Filho, P. Effect of manual and electrical brushing on the enamel of sound primary teeth and teeth with induced white spot lesions. Am. J. Dent. 2020, 33, 25–28. [Google Scholar] [PubMed]
- Davidovich, E.; Grender, J.; Zini, A. Factors Associated with Dental Plaque, Gingivitis, and Caries in a Pediatric Population: A Records-Based Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 8595. [Google Scholar] [CrossRef]
- Nagy, P.; Kövér, K.; Gera, I.; Horváth, A. Elektromos és kézi fogkefék hatékonyságának összehasonlítása az orális prevencióban. Irodalmi áttekintés, systematic review, meta-analízis [Evaluation of the efficacy of powered and manual toothbrushes in preventing oral diseases (Systematic review with meta-analysis)]. Fogorv. Szle. 2016, 109, 3–22. [Google Scholar]
- Davidovich, E.; Shafir, S.; Shay, B.; Zini, A. Plaque Removal by a Powered Toothbrush Versus a Manual Toothbrush in Children: A Systematic Review and Meta-Analysis. Pediatr. Dent. 2020, 42, 280–287. [Google Scholar]
- Cugini, M.; Thompson, M.; Warren, P.R. Correlations between two plaque indices in assessment of toothbrush effectiveness. J. Contemp. Dent. Pract. 2006, 7, 1–9. [Google Scholar] [CrossRef]
- Agnihotry, A.; Fedorowicz, Z.; Worthington, H.V.; Manheimer, E.; Stevenson, R.G. Systematic reviews in oral health: A quality imperative. J. Evid. Based Med. 2016, 9, 47–52. [Google Scholar] [CrossRef]
- Rader, T.; Mann, M.; Stansfield, C.; Cooper, C.; Sampson, M. Methods for documenting systematic review searches: A discussion of common issues. Res. Synth. Methods 2014, 5, 98–115. [Google Scholar] [CrossRef] [PubMed]
- Ritsert, E.F.; Binns, W.H., Jr. Adolescents brush better with an electric toothbrush. J. Dent. Child. 1967, 34, 354–358. [Google Scholar]
- Owen, T.L. A clinical evaluation of electric and manual toothbrushing by children with primary dentitions. ASDC J. Dent. Child. 1972, 39, 15–21. [Google Scholar] [PubMed]
- Crawford, A.N.; McAllan, L.H.; Murray, J.J.; Brook, A.H. Oral hygiene instruction and motivation in children using manual and electric toothbrushes. Community Dent. Oral Epidemiol. 1975, 3, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Yankell, S.L.; Emling, R.C. A thirty-day evaluation of the Rowenta Dentiphant powered toothbrush in children for safety and efficacy. J. Clin. Dent. 1996, 7, 96–100. [Google Scholar] [PubMed]
- Borutta, A. Plaque removal efficacy of a newly developed powered toothbrush in the primary dentition of pre-school children. J. Clin. Dent. 1997, 8, 151–155. [Google Scholar] [PubMed]
- Jongenelis, A.P.; Wiedemann, W. A comparison of plaque removal effectiveness of an electric versus a manual toothbrush in children. ASDC J. Dent. Child. 1997, 64, 176–182. [Google Scholar]
- Grossman, E.; Proskin, H. A comparison of the efficacy and safety of an electric and a manual children’s toothbrush. J. Am. Dent. Assoc. 1997, 128, 469–474. [Google Scholar] [CrossRef]
- Zimmer, S.; Didner, B.; Roulet, J.F. Clinical study on the plaque-removing ability of a new triple-headed toothbrush. J. Clin. Periodontol. 1999, 26, 281–285. [Google Scholar] [CrossRef]
- da Costa, C.C.; da Costa Filho, L.C.; Sória, M.L.; Mainardi, A.P. Plaque removal by manual and electric toothbrushing among children. Pesqui. Odontológica Bras. 2001, 15, 296–301. [Google Scholar] [CrossRef]
- García-Godoy, F.; Marcushamer, M.; Cugini, M.; Warren, P.R. The safety and efficacy of a children’s power toothbrush and a manual toothbrush in 6–11 year-olds. Am. J. Dent. 2001, 14, 195–199. [Google Scholar] [PubMed]
- Nourallah, A.W.; Splieth, C.H. Efficacy of occlusal plaque removal in erupting molars: A comparison of an electric toothbrush and the cross-toothbrushing technique. Caries Res. 2004, 38, 91–94. [Google Scholar] [CrossRef] [PubMed]
- Silverman, J.; Rosivack, R.G.; Matheson, P.B.; Houpt, M.I. Comparison of powered and manual toothbrushes for plaque removal by 4- to 5-year-old children. Pediatr. Dent. 2004, 26, 225–230. [Google Scholar]
- Mascarenhas, A.K.; Soparkar, P.; Al-Mutawaa, S.; Udani, T.M. Plaque removal using a battery-powered toothbrush compared to a manual toothbrush. J. Clin. Dent. 2005, 16, 23–25. [Google Scholar]
- Sun, D.F.; Wang, Y.J.; Hu, W.Q.; Qu, H.X.; Ni, X.K. The efficacy of dental plaque removed by using sonic electric toothbrush in children. Shanghai Kou Qiang Yi Xue 2006, 15, 28–30. (In Chinese) [Google Scholar] [PubMed]
- Kallar, S.; Pandit, I.K.; Srivastava, N.; Gugnani, N. Plaque removal efficacy of powered and manual toothbrushes under supervised and unsupervised conditions: A comparative clinical study. J. Indian Soc. Pedod. Prev. Dent. 2011, 29, 235–238. [Google Scholar] [CrossRef] [PubMed]
- Taschner, M.; Rumi, K.; Master, A.S.; Wei, J.; Strate, J.; Pelka, M. Comparing efficacy of plaque removal using professionally applied manual and power toothbrushes in 4- to 7-year-old children. Pediatr. Dent. 2012, 34, 61–65. [Google Scholar] [PubMed]
- Ghassemi, A.; Vorwerk, L.; Hooper, W.; Patel, V.; Sharma, N.; Qaqish, J. Comparative plaque removal efficacy of a new children’s powered toothbrush and a manual toothbrush. J. Clin. Dent. 2013, 24, 1–4. [Google Scholar]
- Mazzoleni, S.; Bonaldo, G.; Pontarolo, E.; Zuccon, A.; De Francesco, M.; Stellini, E. Experimental assessment of oral hygiene achieved by children wearing rapid palatal expanders, comparing manual and electric toothbrushes. Int. J. Dent. Hyg. 2014, 12, 187–192. [Google Scholar] [CrossRef]
- Davidovich, E.; Ccahuana-Vasquez, R.A.; Timm, H.; Grender, J.; Cunningham, P.; Zini, A. Randomised clinical study of plaque removal efficacy of a power toothbrush in a paediatric population. Int. J. Paediatr. Dent. 2017, 27, 558–567. [Google Scholar] [CrossRef]
- Zhao, S.M.; Chen, H.; Yu, P.B.; Wang, J. A clinical investigation of plaque control efficacy and safety of Sonicare toothbrush in children. Shanghai Kou Qiang Yi Xue 2018, 27, 313–317. (In Chinese) [Google Scholar] [PubMed]
- Erbe, C.; Klees, V.; Ferrari-Peron, P.; Ccahuana-Vasquez, R.A.; Timm, H.; Grender, J.; Cunningham, P.; Adam, R.; Farrell, S.; Wehrbein, H. A comparative assessment of plaque removal and toothbrushing compliance between a manual and an interactive power toothbrush among adolescents: A single-center, single-blind randomized controlled trial. BMC Oral Health 2018, 18, 130. [Google Scholar] [CrossRef] [PubMed]
- Chandra, S.; Jain, N.; Garg, R.; Dhawan, P.; Tuli, A.; Kumar, G. Ionic vs. Manual Toothbrushes: Effect on Plaque and Oral Hygiene Status in Children. Int. J. Clin. Pediatr. Dent. 2019, 12, 375–378. [Google Scholar] [CrossRef] [PubMed]
- Kerr, R.; Claman, D.; Amini, H.; Alexy, E.; Kumar, A.; Casamassimo, P.S. Evaluation of the Ability of Five- to 11-Year-Olds to Brush Their Teeth Effectively with Manual and Electric Toothbrushing. Pediatr. Dent. 2019, 41, 20–24. [Google Scholar] [PubMed]
- Aggarwal, N.; Gupta, S.; Grover, R.; Sadana, G.; Bansal, K. Plaque Removal Efficacy of Different Toothbrushes: A Comparative Study. Int. J. Clin. Pediatr. Dent. 2019, 12, 385–390. [Google Scholar] [CrossRef]
- Davidovich, E.; Ccahuana-Vasquez, R.A.; Timm, H.; Grender, J.; Zini, A. Randomised clinical study of plaque removal efficacy of an electric toothbrush in primary and mixed dentition. Int. J. Paediatr. Dent. 2021, 31, 657–663. [Google Scholar] [CrossRef]
- Purushotham, P.M.; Rao, A.; Natarajan, S.; Shrikrishna, S.B. Comparison of the efficacy of parental brushing using powered versus manual tooth brush: A randomized, four-period, two-treatment, single-blinded crossover study. J. Indian Soc. Pedod. Prev. Dent. 2021, 39, 95–100. [Google Scholar] [CrossRef]
- Francis, M.; Hooper, W.J.; Worob, D.; Huy, G.; Santos, S.; Goyal, C.R.; Qaqish, K.; Qaqish, J.G.; Ghassemi, A. Comparative plaque removal efficacy of a new children’s powered toothbrush and a manual toothbrush: Randomized, single use clinical study. Am. J. Dent. 2021, 34, 338–344. [Google Scholar]
- White, L.W. Efficacy of a sonic toothbrush in reducing plaque and gingivitis in adolescent patients. J. Clin. Orthod. 1996, 30, 85–90. [Google Scholar]
- Ho, H.P.; Niederman, R. Effectiveness of the Sonicare sonic toothbrush on reduction of plaque, gingivitis, probing pocket depth and subgingival bacteria in adolescent orthodontic patients. J. Clin. Dent. 1997, 8, 15–19. [Google Scholar]
- Heasman, P.; Wilson, Z.; Macgregor, I.; Kelly, P. Comparative study of electric and manual toothbrushes in patients with fixed orthodontic appliances. Am. J. Orthod. Dentofac. Orthop. 1998, 114, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Pucher, J.J.; Lamendola-Sitenga, K.; Ferguson, D.; Van Swoll, R. The effectiveness of an ionic toothbrush in the removal of dental plaque and reduction on gingivitis in orthodontic patients. J. West. Soc. Periodontol. Periodontal Abstr. 1999, 47, 101–107. [Google Scholar] [PubMed]
- Borutta, A.; Pala, E.; Fischer, T. Effectiveness of a powered toothbrush compared with a manual toothbrush for orthodontic patients with fixed appliances. J. Clin. Dent. 2002, 13, 131–137. [Google Scholar] [PubMed]
- Hickman, J.; Millett, D.T.; Sander, L.; Brown, E.; Love, J. Powered vs. manual tooth brushing in fixed appliance patients: A short term randomized clinical trial. Angle Orthod. 2002, 72, 135–140. [Google Scholar] [CrossRef]
- Costa, M.R.; Silva, V.C.; Miqui, M.N.; Sakima, T.; Spolidorio, D.M.P.; Cirelli, J.A. Efficacy of ultrasonic, electric and manual toothbrushes in patients with fixed orthodontic appliances. Angle Orthod. 2007, 77, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Biavati, A.S.; Gastaldo, L.; Dessi, M.; Biavati, F.S.; Migliorati, M. Manual orthodontic vs. oscillating-rotating electric toothbrush in orthodontic patients: A randomised clinical trial. Eur. J. Paediatr. Dent. 2010, 11, 200–202. [Google Scholar]
- Marini, I.; Bortolotti, F.; Parenti, S.I.; Gatto, M.R.; Bonetti, G.A. Combined effects of repeated oral hygiene motivation and type of toothbrush on orthodontic patients: A blind randomized clinical trial. Angle Orthod. 2014, 84, 896–901. [Google Scholar] [CrossRef] [PubMed]
- Zingler, S.; Pritsch, M.; Wrede, D.J.; Ludwig, B.; Bister, D.; Kneist, S.; Lux, C.J. A randomized clinical trial comparing the impact of different oral hygiene protocols and sealant applications on plaque, gingival, and caries index scores. Eur. J. Orthod. 2014, 36, 150–163. [Google Scholar] [CrossRef]
- Mylonopoulou, I.M.; Pepelassi, E.; Madianos, P.; Halazonetis, D.J. A randomized, 3-month, parallel-group clinical trial to compare the efficacy of electric 3-dimensional toothbrushes vs. manual toothbrushes in maintaining oral health in patients with fixed orthodontic appliances. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 648–658. [Google Scholar] [CrossRef]
- Li, L.W.; Wong, H.M.; Sun, L.; Wen, Y.F.; McGrath, C.P. Anthropometric measurements and periodontal diseases in children and adolescents: A systematic review and meta-analysis. Adv. Nutr. 2015, 6, 828–841. [Google Scholar] [CrossRef] [PubMed]
- Li, L.W.; Wong, H.M.; Peng, S.M.; McGrath, C.P. Anthropometric measurements and dental caries in children: A systematic review of longitudinal studies. Adv. Nutr. 2015, 6, 52–63. [Google Scholar] [CrossRef] [PubMed]
- Boyd, R.L. Clinical and laboratory evaluation of powered electric toothbrushes: Review of the literature. J. Clin. Dent. 1997, 8, 67–71. [Google Scholar] [PubMed]
- Kaklamanos, E.G.; Kalfas, S. Meta-analysis on the effectiveness of powered toothbrushes for orthodontic patients. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 187.e1–187.e14. [Google Scholar] [CrossRef]
- Bain, C.; Sayed, A.A.; Kaklamanos, E.G.; Kazi, H.A. Toothbrushing-Should We Advise Mechanical or Power Brushes? Results of an International Delphi Conference. J. Contemp. Dent. Pract. 2018, 19, 1169–1173. [Google Scholar] [CrossRef]
- Hollaar, V.R.Y. Effectiviteit van plaqueverwijdering met elektrische of handtandenborstel bij vaste orthodontische apparatuur Effectiveness of electric or manual toothbrush in dental plaque removal in patients with fixed orthodontic appliances. Ned. Tijdschr. Voor Tandheelkd. 2021, 128, 475–478. [Google Scholar] [CrossRef]
- Pabel, S.O.; Freitag, F.; Hrasky, V.; Zapf, A.; Wiegand, A. Randomised controlled trial on differential learning of toothbrushing in 6- to 9-year-old children. Clin. Oral Investig. 2018, 22, 2219–2228. [Google Scholar] [CrossRef]
- Collett, B.R.; Huebner, C.E.; Seminario, A.L.; Wallace, E.; Gray, K.E.; Speltz, M.L. Observed child and parent toothbrushing behaviors and child oral health. Int. J. Paediatr. Dent. 2016, 26, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Joufi, A.I.; Claiborne, D.M.; Shuman, D. Oral Health Education and Promotion Activities by Early Head Start Programs in the United States: A systematic review. J. Dent. Hyg. 2021, 95, 14–21. [Google Scholar] [PubMed]
- Aksoy, M.; Topsakal, K.G. YouTube™ for information on paediatric oral health instructions. Int. J. Dent. Hyg. 2022, 20, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Escribano, M.; Figuero, E.; Martin, C.; Tobias, A.; Serrano, J.; Roldan, S.; Herrera, D. Efficacy of adjunctive anti-plaque chemical agents: A systematic review and network meta-analyses of the Turesky modification of the Quigley and Hein plaque index. J. Clin. Periodontol. 2016, 43, 1059–1073. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).