Biomechanically and Periodontally-Based Orthodontic Treatment of a Patient with Upper Canine Affected by External Cervical Resorption (ECR): A Case Report
Abstract
1. Introduction
2. Patient Information—Case Presentation
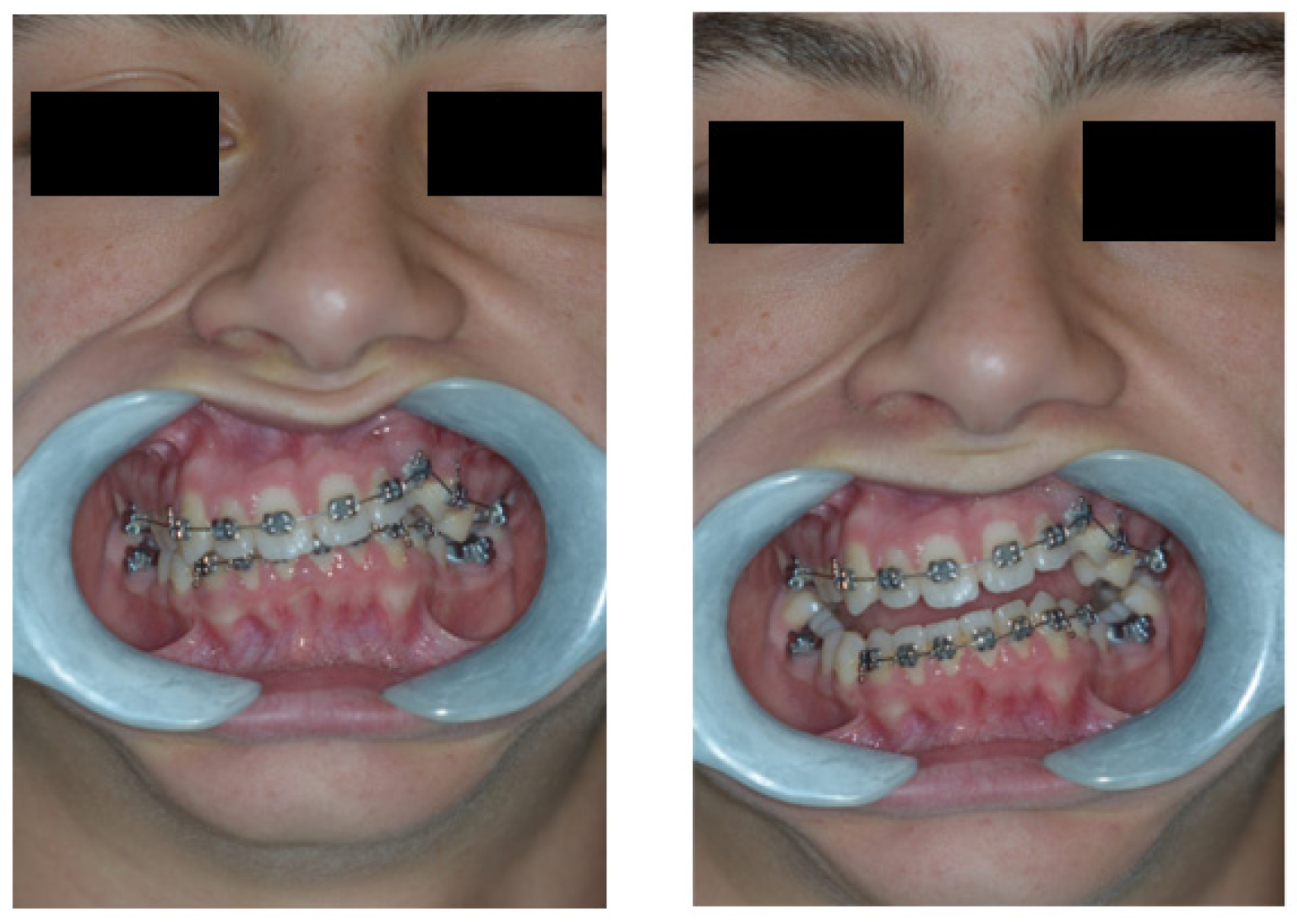
2.1. Clinical Findings
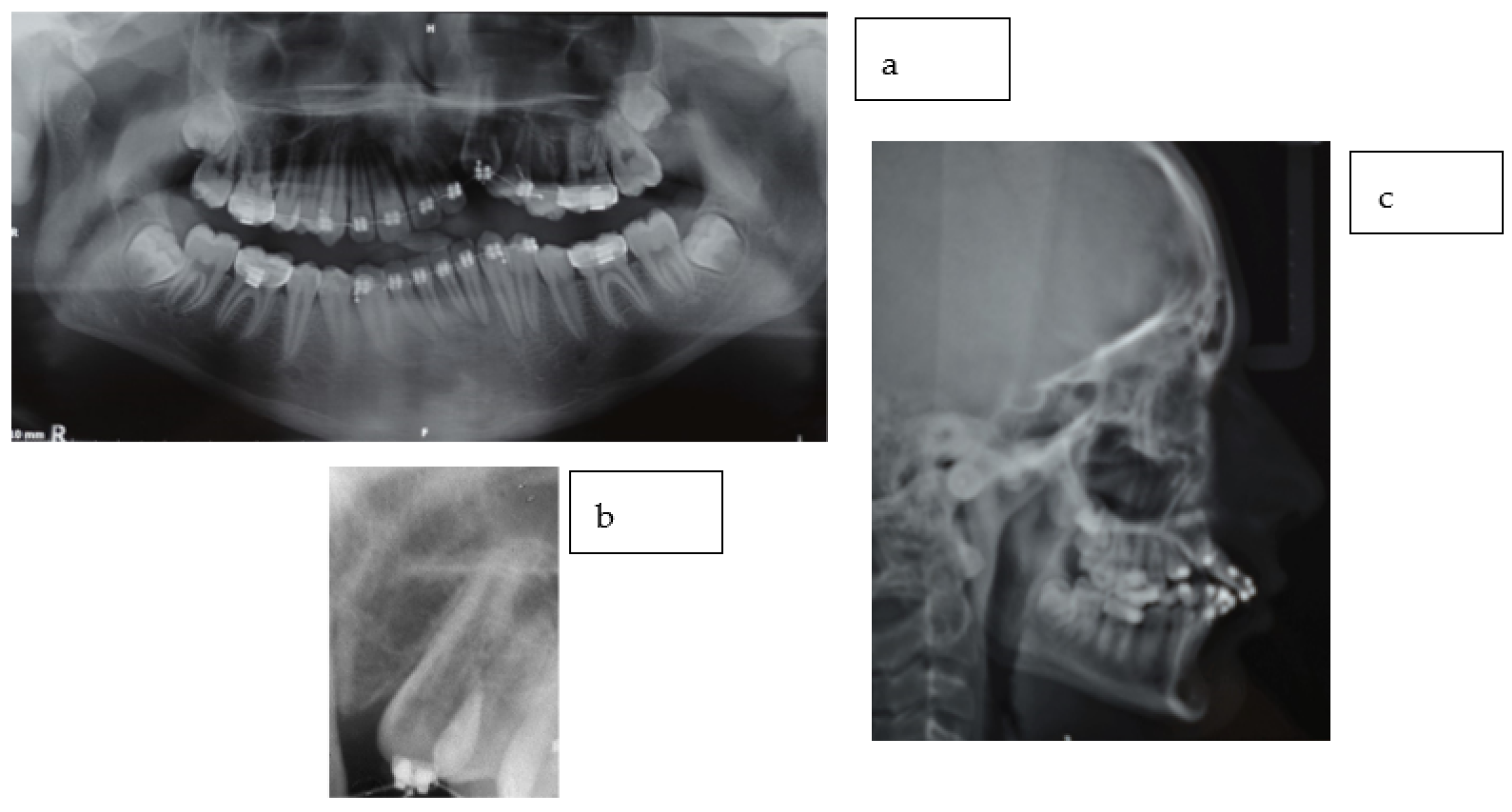
2.2. Radiographic Findings
2.3. Diagnostic Assessment
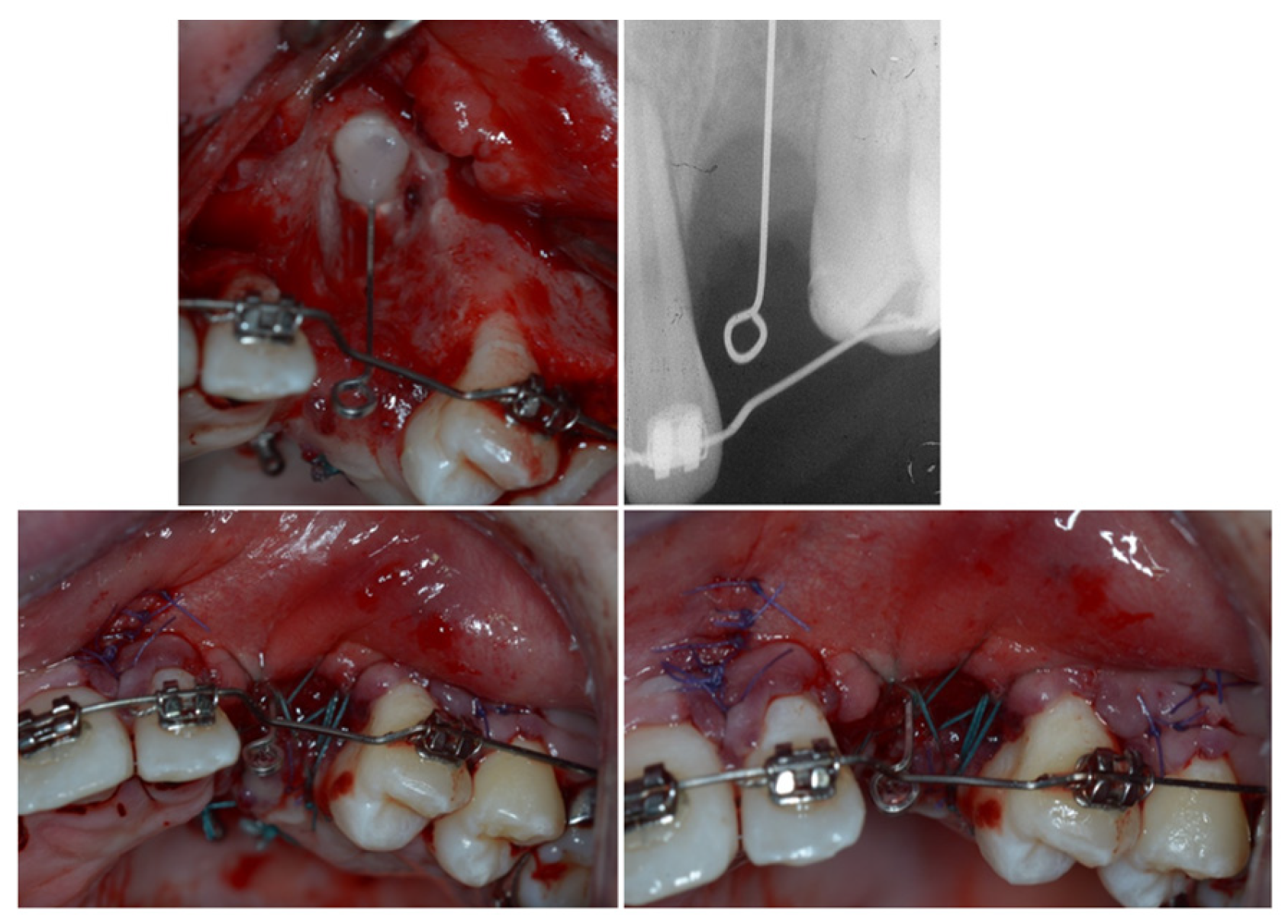
3. Therapeutic Interventions
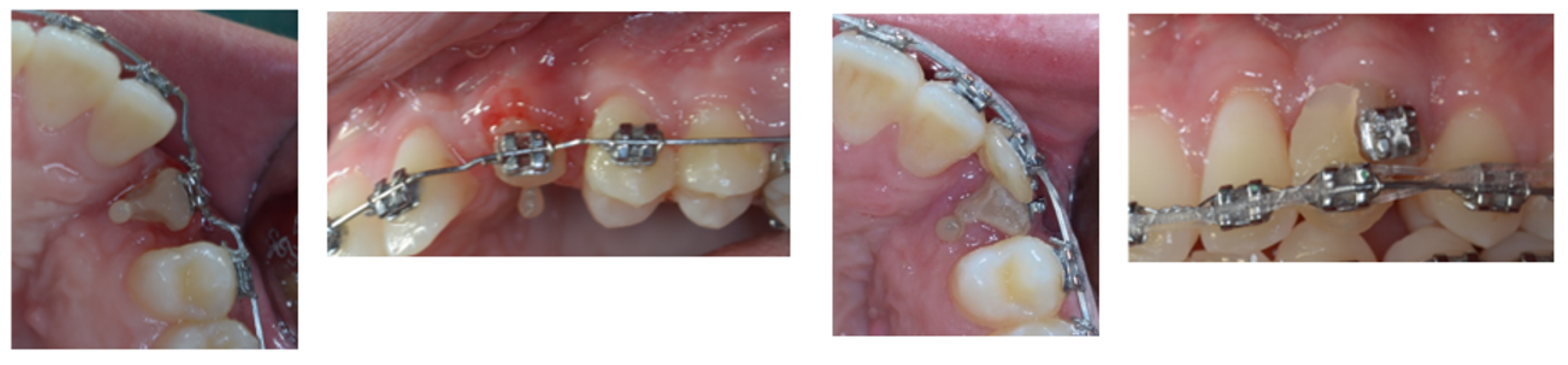
4. Follow-Up and Outcomes
5. Discussion
6. Conclusions
7. Patient Perspective
8. Informed Consent
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A

References
- Ezoddini, A.F.; Sheikhha, M.H.; Ahmadi, H. Prevalence of dental developmental anomalies: A radiographic study. Community Dent. Health 2007, 24, 140–144. [Google Scholar] [PubMed]
- Becker, A.; Chaushu, G.; Chaushu, S. Analysis of failure in the treatment of impacted maxillary canines. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 743–754. [Google Scholar] [CrossRef] [PubMed]
- Becker, A.; Abramovitz, I.; Chaushu, S. Failure of treatment of impacted canines associated with invasive cervical root resorption. Angle Orthod. 2013, 83, 870–876. [Google Scholar] [CrossRef] [PubMed]
- Tronstad, L. Root resorption—Etiology, terminology and clinical manifestations. Dent. Traumatol. 1988, 4, 241–252. [Google Scholar] [CrossRef]
- Patel, S.; Mavridou, A.M.; Lambrechts, P.; Saberi, N. External cervical resorption-part 1: Histopathology, distribution and presentation. Int. Endod. J. 2018, 51, 1205–1223. [Google Scholar] [CrossRef] [PubMed]
- Samandara, A.; Papageorgiou, S.N.; Ioannidou-Marathiotou, I.; Kavvadia-Tsatala, S.; Papadopoulos, M.A. Evaluation of orthodontically induced external root resorption following orthodontic treatment using cone beam computed tomography (CBCT): A systematic review and meta-analysis. Eur. J. Orthod. 2018, 41, 67–79. [Google Scholar] [CrossRef]
- Mavridou, A.M.; Hauben, E.; Wevers, M.; Schepers, E.; Bergmans, L.; Lambrechts, P. Understanding external cervical resorption in vital teeth. J. Endod. 2016, 42, 1737–1751. [Google Scholar] [CrossRef]
- Hammarström, L.; Lindskog, S. Factors regulating and modifying dental root resorption. Proc. Finn. Dent. Soc. 1992, 88 (Suppl. S1), 115–123. [Google Scholar]
- Iqbal, M.K. Clinical and scanning electron microscopic features of invasive cervical resorption in a maxillary molar. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2007, 103, e49–e54. [Google Scholar] [CrossRef]
- Heithersay, G.S. Invasive cervical resorption: An analysis of potential predisposing factors. Quintessence Int. 1999, 30, 83–95. [Google Scholar]
- Kokich, V.O., Jr.; Kiyak, H.A.; Shapiro, P.A. Comparing the perception of dentists and lay people to altered dental esthetics. J. Esthet. Restor. Dent. 1999, 11, 311–324. [Google Scholar] [CrossRef] [PubMed]
- Burstone, C.J. Diagnosis and treatment planning of patients with asymmetries. Semin. Orthod. 1998, 4, 153–164. [Google Scholar] [CrossRef] [PubMed]
- Musilli, M.; Grampone, F.; Melsen, B. A new auxiliary spring for correction of a canted incisal plane. J. Clin. Orthod. 2014, 48, 500–504. [Google Scholar]
- Riley, D.S.; Barber, M.S.; Kienle, G.S.; Aronson, J.K.; von Schoen-Angerer, T.; Tugwell, P.; Kiene, H.; Helfand, M.; Altman, D.G.; Sox, H.; et al. CARE guidelines for case reports: Explanation and elaboration document. J. Clin. Epidemiol. 2017, 89, 218–235. [Google Scholar] [CrossRef] [PubMed]
- Janson, G.; de Lima, K.J.R.S.; Woodside, D.G.; Metaxas, A.; de Freitas, M.R.; Henriques, J.F.C. Class II subdivision malocclusion types and evaluation of their asymmetries. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Fiorelli, G.; Melsen, B. Biomechanics in Orthodontics Rel. 4.0 Online E-Book; IOSS GmbH: Wollerau, Switzerand, 1992. [Google Scholar]
- Korayem, M.; Flores-Mir, C.; Nassar, U.; Olfert, K. Implant Site Development by Orthodontic Extrusion. Angle Orthod. 2008, 78, 752–760. [Google Scholar] [CrossRef] [PubMed]
- Buskin, R.; Castellon, P.; Hochstedler, J.L. Orthodontic extrusion and orthodontic extraction in preprosthetic treatment using implant therapy. Pract. Periodontics Aesthetic Dent. 2000, 12, 213–219. [Google Scholar]
- Salama, H.; Salama, M. The role of orthodontic extrusive remodeling in the enhancement of soft and hard tissue profiles prior to implant placement: A systematic approach to the management of extraction site defects. Int. J. Periodontics Restor. Dent. 1993, 13, 312–333. [Google Scholar]
- Mantzikos, T.; Shamus, I. Forced eruption and implant site development: An osteophysiologic response. Am. J. Orthod. Dentofac. Orthop. 1999, 115, 583–591. [Google Scholar] [CrossRef]
- Mantzikos, T.; Shamus, I. Forced eruption and implant site development: Soft tissue response. Am. J. Orthod. Dentofac. Orthop. 1997, 112, 596–600. [Google Scholar] [CrossRef]
- Tomm, I.; Fontana, P.; Paganelli, C.; Salgarello, S. Orthodontic extrusion and implant site development. J. Dent. Res. 2002, 81, B264. [Google Scholar]
- Ostojic, S.; Sieber, R.; Borer, K.; Lambrecht, J.T. Controlled orthodontic extrusion with subsequent implantation. Schweiz. Monatsschr. Zahnmed. 2005, 115, 222–231. [Google Scholar] [PubMed]
- Bach, N.; Baylard, J.-F.; Voyer, R. Orthodontic extrusion: Periodontal considerations and applications. J. Can. Dent. Assoc. 2004, 70, 775–780. [Google Scholar]
- Zuccati, G.; Bocchieri, A. Implant site development by orthodontic extrusion of teeth with poor prognosis. J. Clin. Orthod. 2003, 37, 307–311. [Google Scholar] [PubMed]
- Mantzikos, T.; Shamus, I. Case report: Forced eruption and implant site development. Angle Orthod. 1998, 68, 179–186. [Google Scholar] [PubMed]
- Nozawa, T.; Sugiyama, T.; Yamaguchi, S.; Ramos, T.; Komatsu, S.; Enomoto, H.; Ito, K. Buccal and coronal bone augmentation using forced eruption and buccal root torque: A case report. Int. J. Periodontics Restor. Dent. 2003, 23, 585–591. [Google Scholar]
- Danesh-Meyer, M.J.; Brice, D.M. Implant site development using orthodontic extrusion: A case report. N. Z. Dent. J. 2000, 96, 18–22. [Google Scholar]
- López, S.G.; Gaya, M.V.O.; Capilla, M.V. Esthetic restoration with orthodontic traction and single-tooth implant: Case report. Int. J. Periodontics Restor. Dent. 2005, 25, 239–245. [Google Scholar]
- Biggs, J.; Beagle, J.R. Pre-implant orthodontics: Achieving vertical bone height without osseous grafts. J. Indiana Dent. Assoc. 2004, 83, 18–19. [Google Scholar]
- Celenza, F. The development of forced eruption as a modality for implant site enhancement. Alpha Omegan 1997, 90, 40–43. [Google Scholar]
- Chambrone, L.; Chambrone, L.A. Forced orthodontic eruption of fractured teeth before implant placement: Case report. J. Can. Dent. Assoc. 2005, 71, 257–261. [Google Scholar] [PubMed]
- Chandler, K.B.; Rongey, W.F. Forced eruption: Review and case reports. Gen. Dent. 2005, 53, 274–277. [Google Scholar] [PubMed]
- Lin, C.-D.; Chang, S.-S.; Liou, C.-S.; Dong, D.-R.; Fu, E. Management of interdental papillae loss with forced eruption, immediate implantation, and root-form pontic. J. Periodontol. 2006, 77, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.-S.; Yi, K.-Y.; Moon, S.-C.; Jung, Y.-C. Immediate loading of an implant following implant site development using forced eruption: A case report. Int. J. Oral Maxillofac. Implants 2005, 20, 621–626. [Google Scholar] [PubMed]
- Salama, H.; Salama, M.; Kelly, J. The orthodontic-periodontal connection in implant site development. Pract. Periodontics Aesthet. Dent. 1996, 8, 923–932. [Google Scholar] [PubMed]
- Kim, Y.I.; Kim, S.S.; Son, W.S.; Park, S.B. Orthodontic treatment of an ankylosed tooth: Application of single tooth osteotomy and alveolar bone distraction osteogenesis. Korean J. Orthod. 2009, 39, 185–198. [Google Scholar] [CrossRef][Green Version]
- Wilmes, B.; Drescher, D. Vertical periodontal ligament distraction—A new method for aligning ankylosed and displaced canines. J. Orofac. Orthop. 2009, 70, 213–223. [Google Scholar] [CrossRef]
- Nyman, S.; Lindhe, J.; Karring, T. Healing following surgical treatment and root demineralization in monkeys with periodontal disease. J. Clin. Periodontol. 1981, 8, 249–258. [Google Scholar] [CrossRef]
- Patel, J.; Beddis, H.P. How to assess and manage external cervical resorption. Br. Dent. J. 2019, 227, 695–701. [Google Scholar] [CrossRef]
- Mavridou, A.M.; Hauben, E.; Wevers, M.; Schepers, E.; Bergmans, L.; Lambrechts, P. Understanding external cervical resorption patterns in endodontically treated teeth. Int. Endod. J. 2017, 50, 1116–1133. [Google Scholar] [CrossRef]
- Liou, E.J.-W.; Mehta, K.; Lin, J.C.-Y. An archwire for non-invasive improvement of occlusal cant and soft tissue chin deviation. APOS Trends Orthod. 2019, 9, 19–25. [Google Scholar] [CrossRef]
- Deluke, M.; Uribe, F.; Nanda, R. Correction of a canted lower incisal plane. J. Clin. Orthod. 2006, 40, 555–559. [Google Scholar] [PubMed]
- van Steenbergen, E.; Nanda, R. Biomechanics of orthodontic correction of dental asymmetries. Am. J. Orthod. Dentofac. Orthop. 1995, 107, 618–624. [Google Scholar] [CrossRef] [PubMed]











Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Musilli, M.; Iuorio, M.T.; Vaia, E.; Vaia, E.; Ramaglia, L.; D’Antò, V. Biomechanically and Periodontally-Based Orthodontic Treatment of a Patient with Upper Canine Affected by External Cervical Resorption (ECR): A Case Report. Dent. J. 2023, 11, 278. https://doi.org/10.3390/dj11120278
Musilli M, Iuorio MT, Vaia E, Vaia E, Ramaglia L, D’Antò V. Biomechanically and Periodontally-Based Orthodontic Treatment of a Patient with Upper Canine Affected by External Cervical Resorption (ECR): A Case Report. Dentistry Journal. 2023; 11(12):278. https://doi.org/10.3390/dj11120278
Chicago/Turabian StyleMusilli, Marino, Morena Tina Iuorio, Emanuele Vaia, Enzo Vaia, Luca Ramaglia, and Vincenzo D’Antò. 2023. "Biomechanically and Periodontally-Based Orthodontic Treatment of a Patient with Upper Canine Affected by External Cervical Resorption (ECR): A Case Report" Dentistry Journal 11, no. 12: 278. https://doi.org/10.3390/dj11120278
APA StyleMusilli, M., Iuorio, M. T., Vaia, E., Vaia, E., Ramaglia, L., & D’Antò, V. (2023). Biomechanically and Periodontally-Based Orthodontic Treatment of a Patient with Upper Canine Affected by External Cervical Resorption (ECR): A Case Report. Dentistry Journal, 11(12), 278. https://doi.org/10.3390/dj11120278







