Validation of an Inverse Fitting Method of Diffuse Reflectance Spectroscopy to Quantify Multi-Layered Skin Optical Properties
Abstract
1. Introduction
2. Materials and Methods
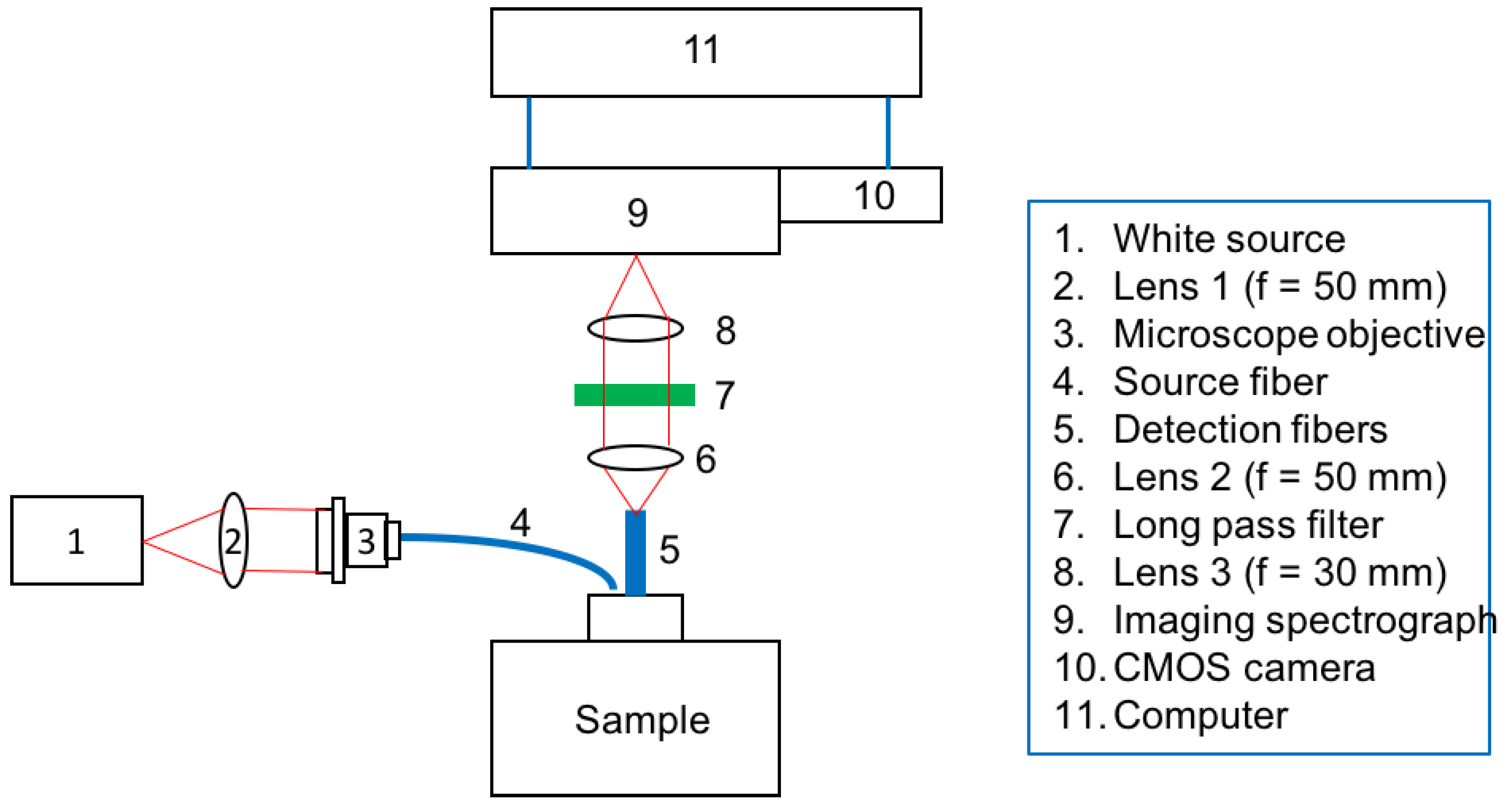
2.1. Spatially-Resolved Diffuse Reflectance Spectroscopy (SRDRS) System
2.2. Tissue Model
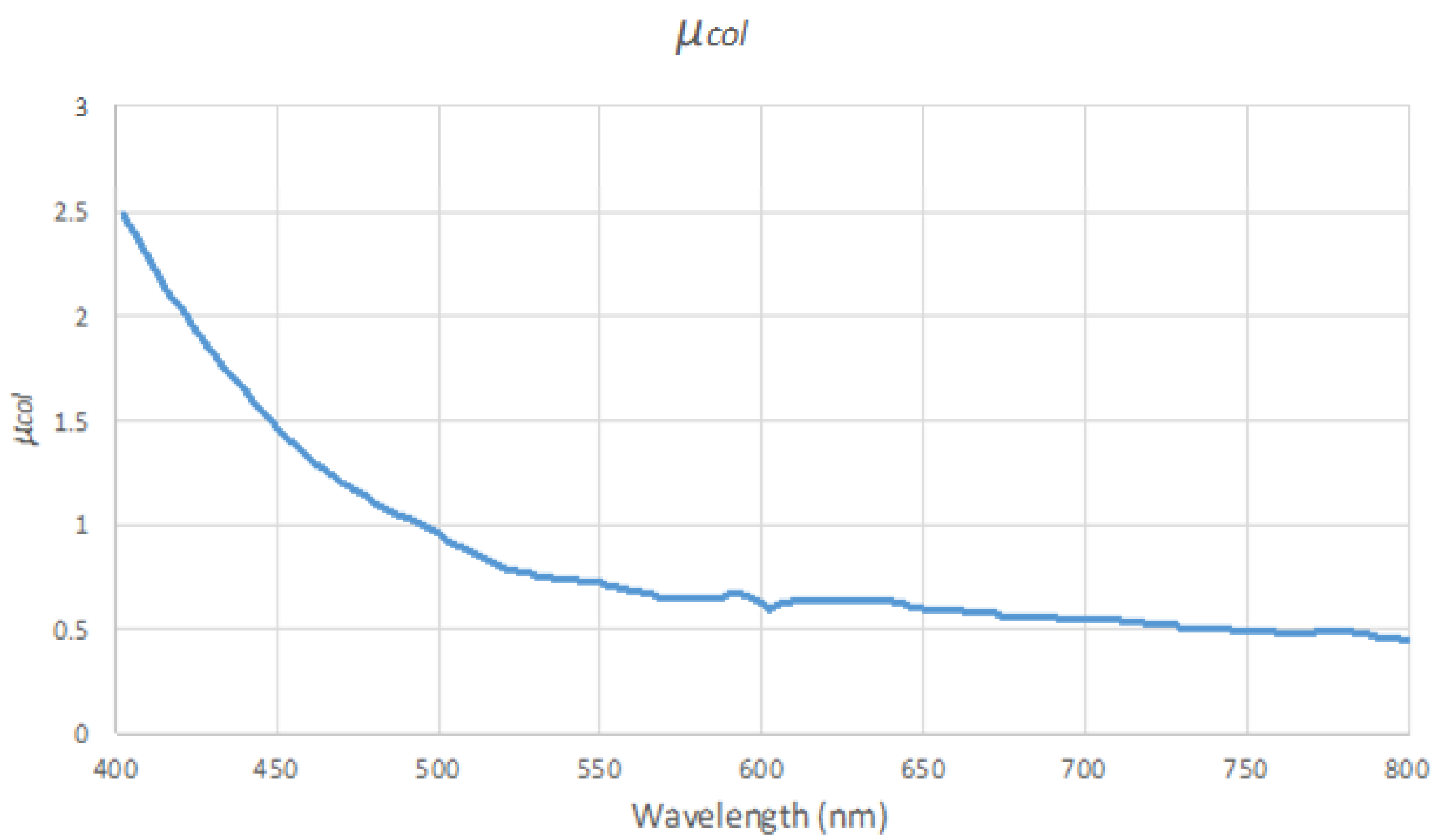
2.3. Pre-Simulated Reflectance Database and forward ANN Models
2.4. Inverse Fitting Procedures
- Compare the target spectra to 1000 sets of spectra pre-calculated with MC simulations using randomly assigned parameters, and calculate the rmse between the target and the pre-calculated spectra.
- Choose three pre-calculated spectra with the lowest rmse, and the corresponding parameter sets were chosen as the initial parameter sets. Repeat step 3 for each of the three initial parameter sets.
- Do iterative curve fitting of the target spectra according to one of the following procedures
- Procedure X: Only fit the target spectra in wavelength ranges 410–440 nm and 530–580 nm where hemoglobin absorption is prominent.
- Procedure Y: Do procedure X, constrain the boundary of fblood and α to be within ±10% of the results after procedure X, and fit the target spectra in full wavelength range (401–590 nm).
- Procedure Z: Only fit the target spectra in the full wavelength range (401–590 nm).
- Find the lowest reflectance value of each spectrum in the wavelength range of 401–480 nm, and adjust fblood to make the lowest values of modeled spectra best match those of the target spectra.
- Adjust α to minimize the rmse between the modeled and the target spectra in the wavelength range of 520–583 nm.
- Choose the optimal result as the one with the lowest rmse among the three fitting trials to avoid local minimum.
- Scenario A: Thicknesses of the two epidermal layers, th1 and th2, are unknown,
- Scenario B: The sum of th1 and th2 is known.
2.5. In Vivo Cuff Occlusion Experiments and Calibration of Spectra
3. Results
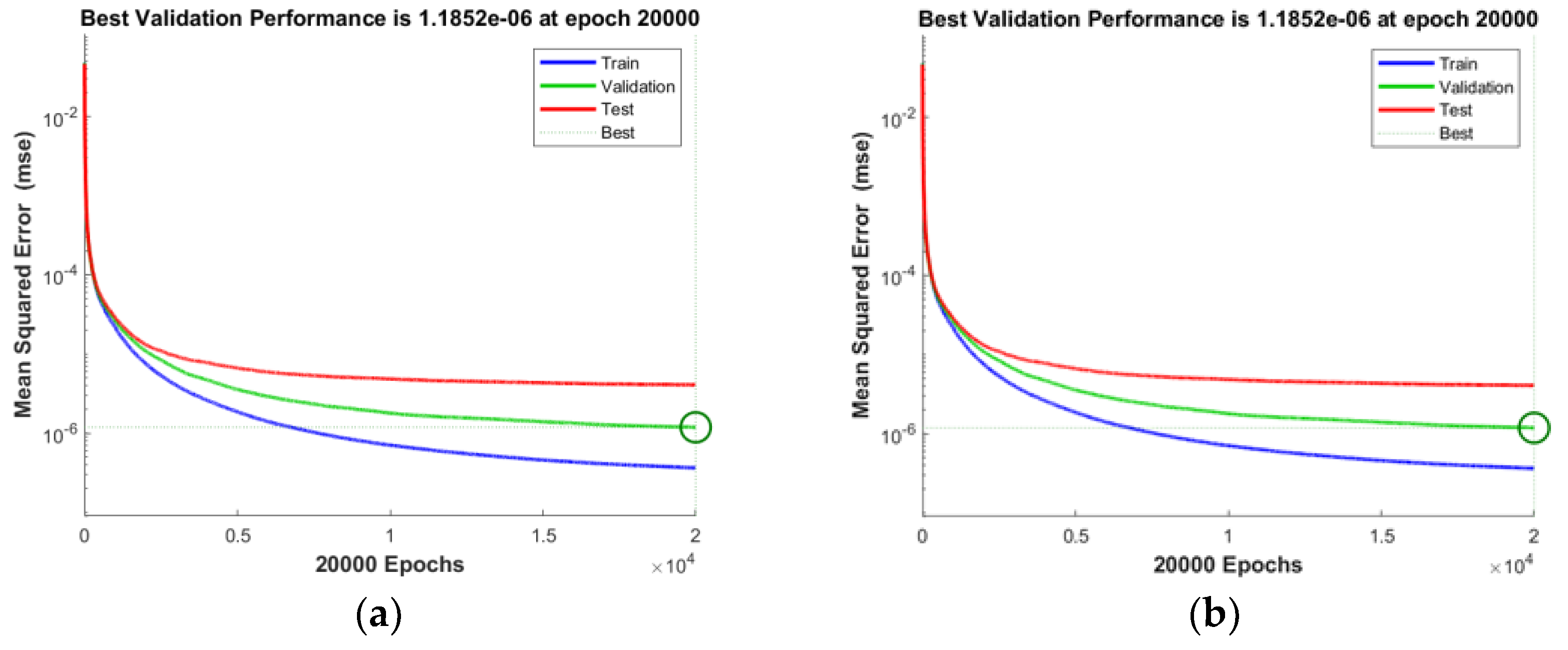
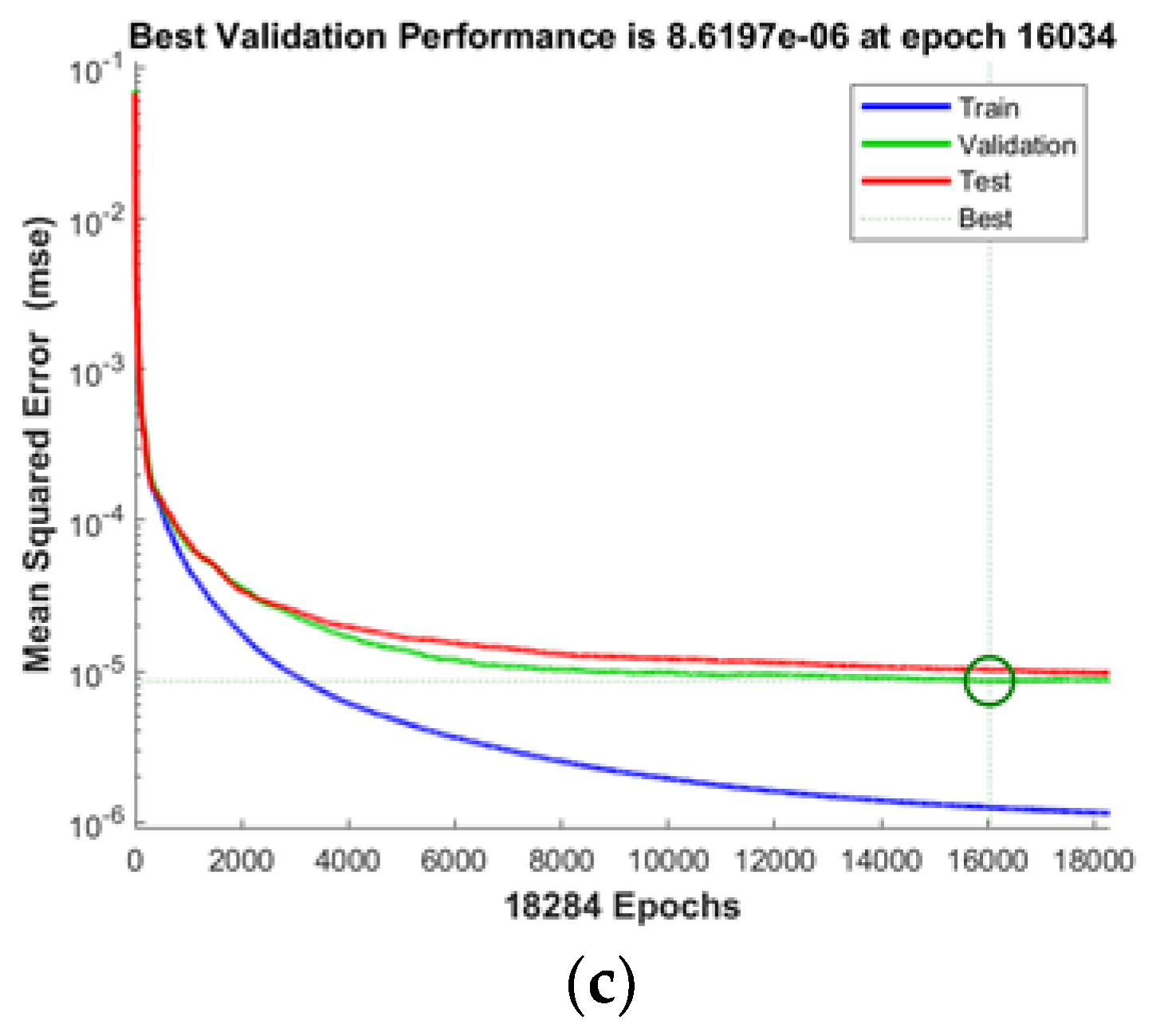
3.1. ANN Training Results
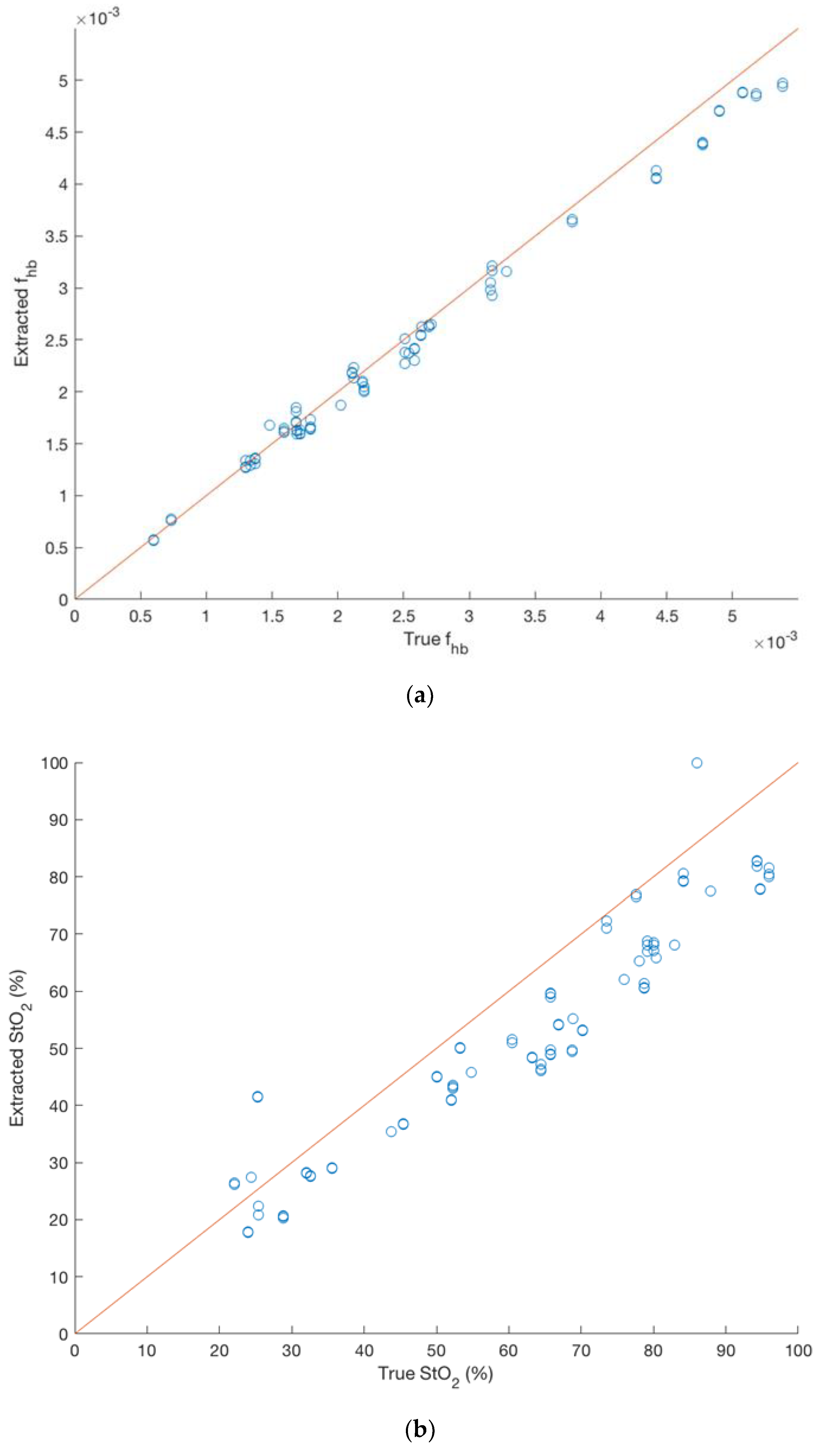
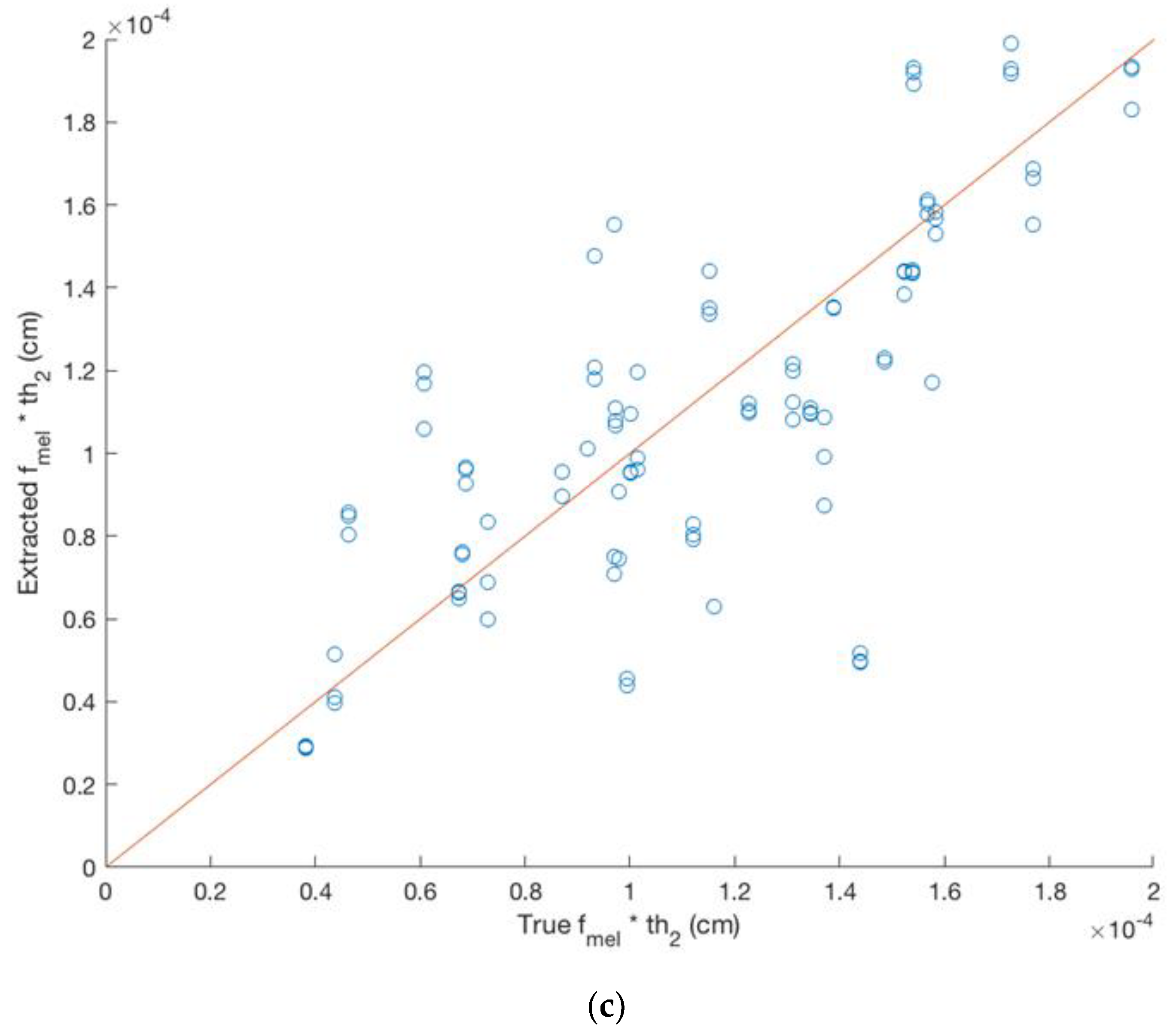
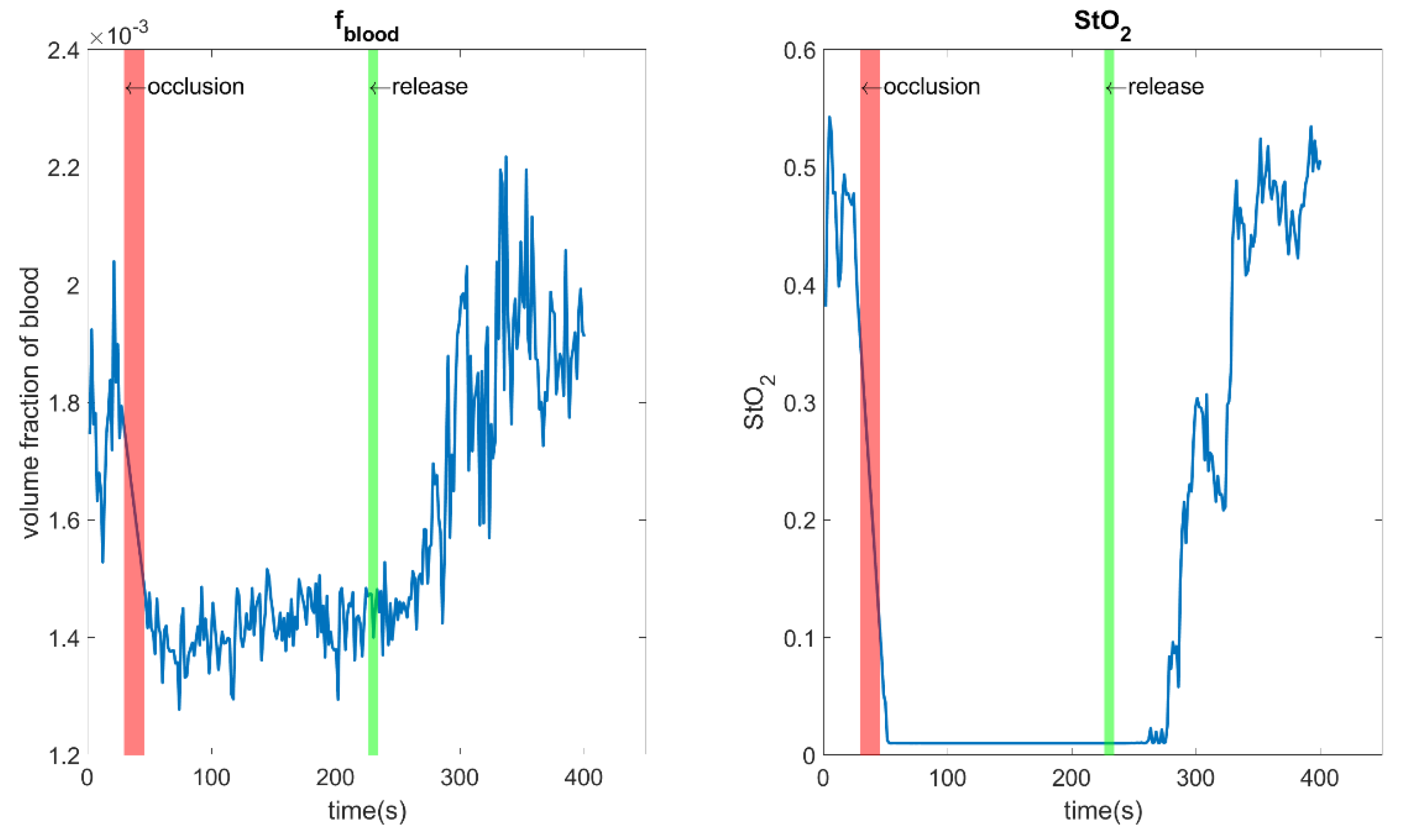
3.2. Inverse Fitting of Simulated SRDRS Data with Various Fitting Procedures
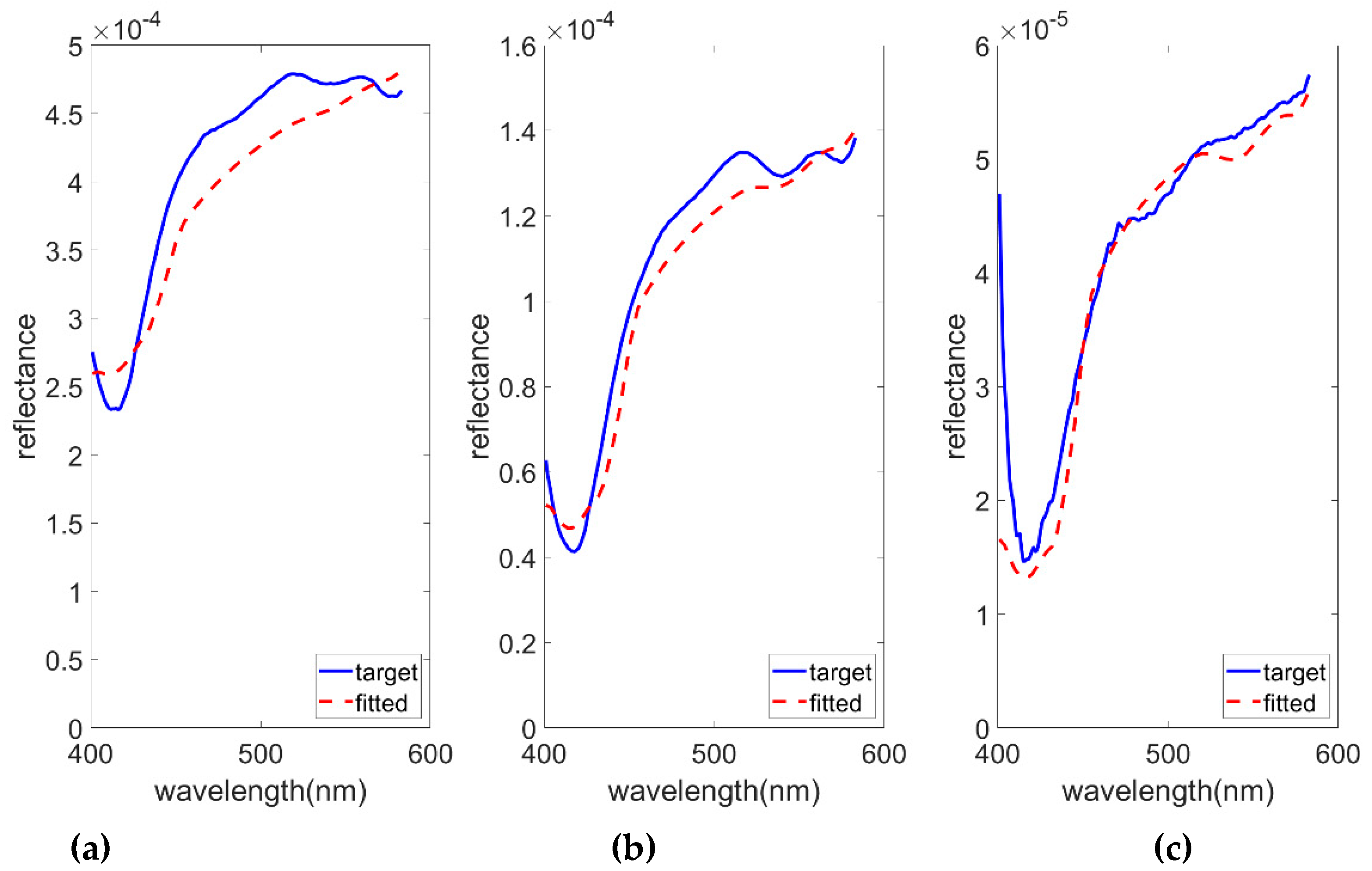
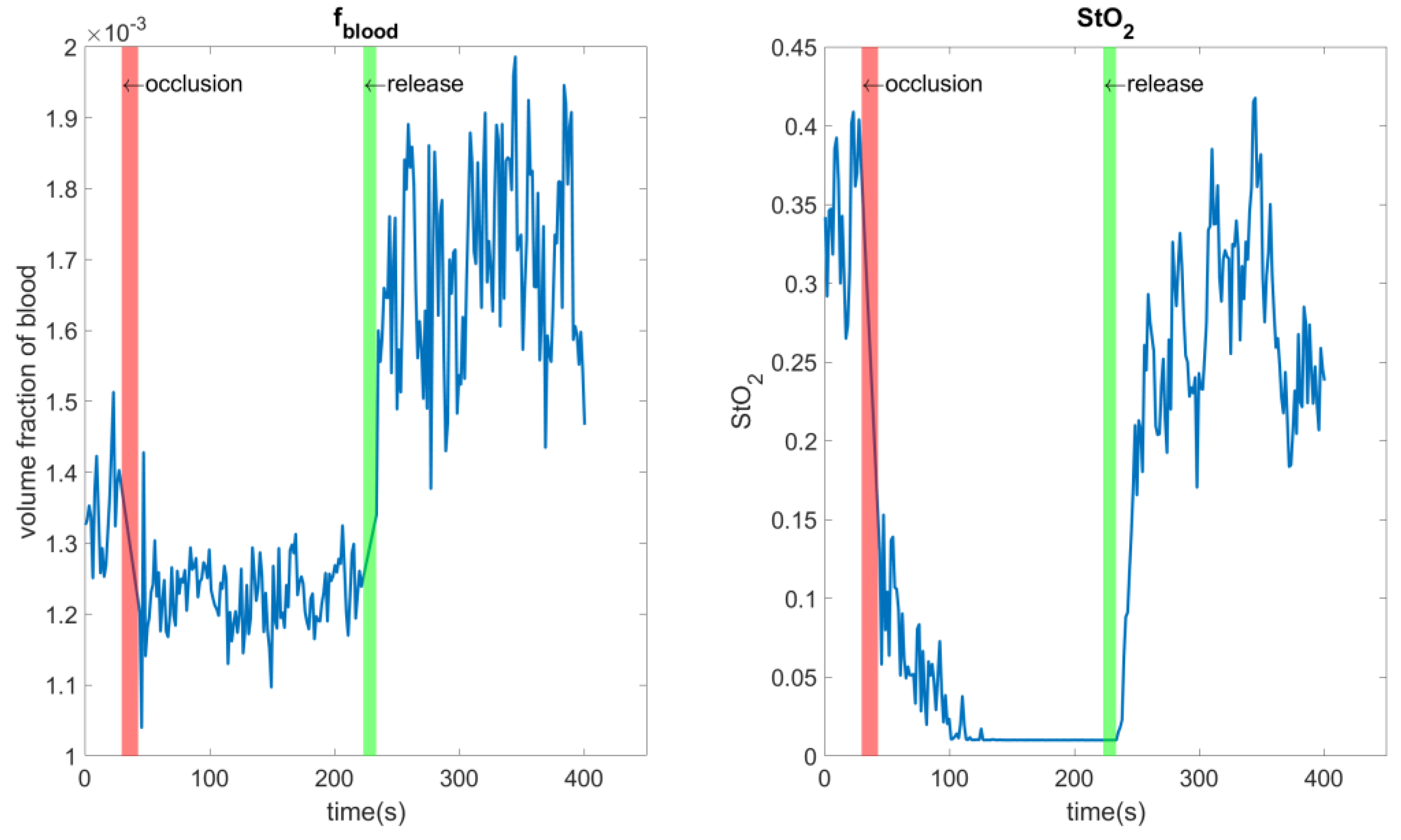
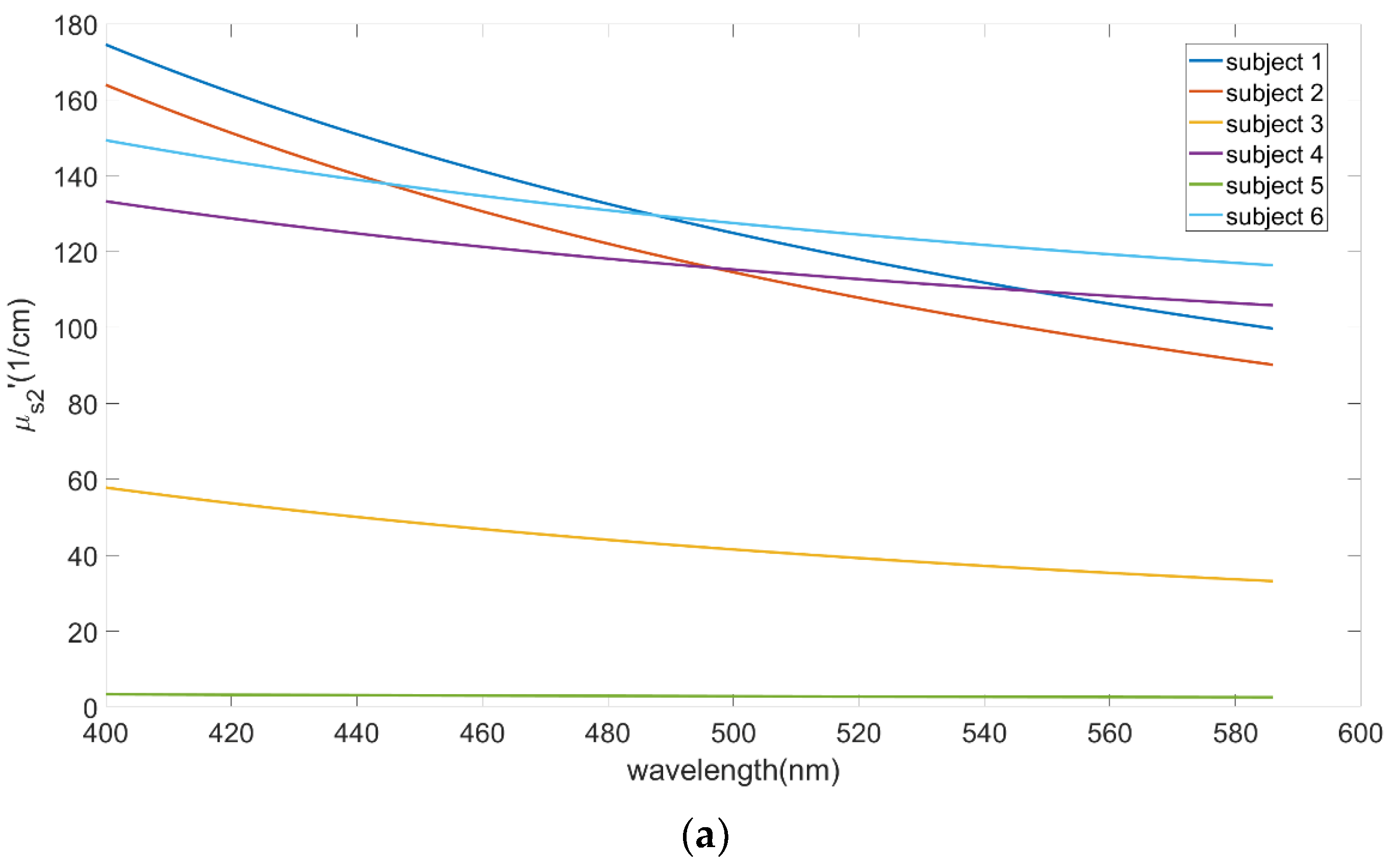
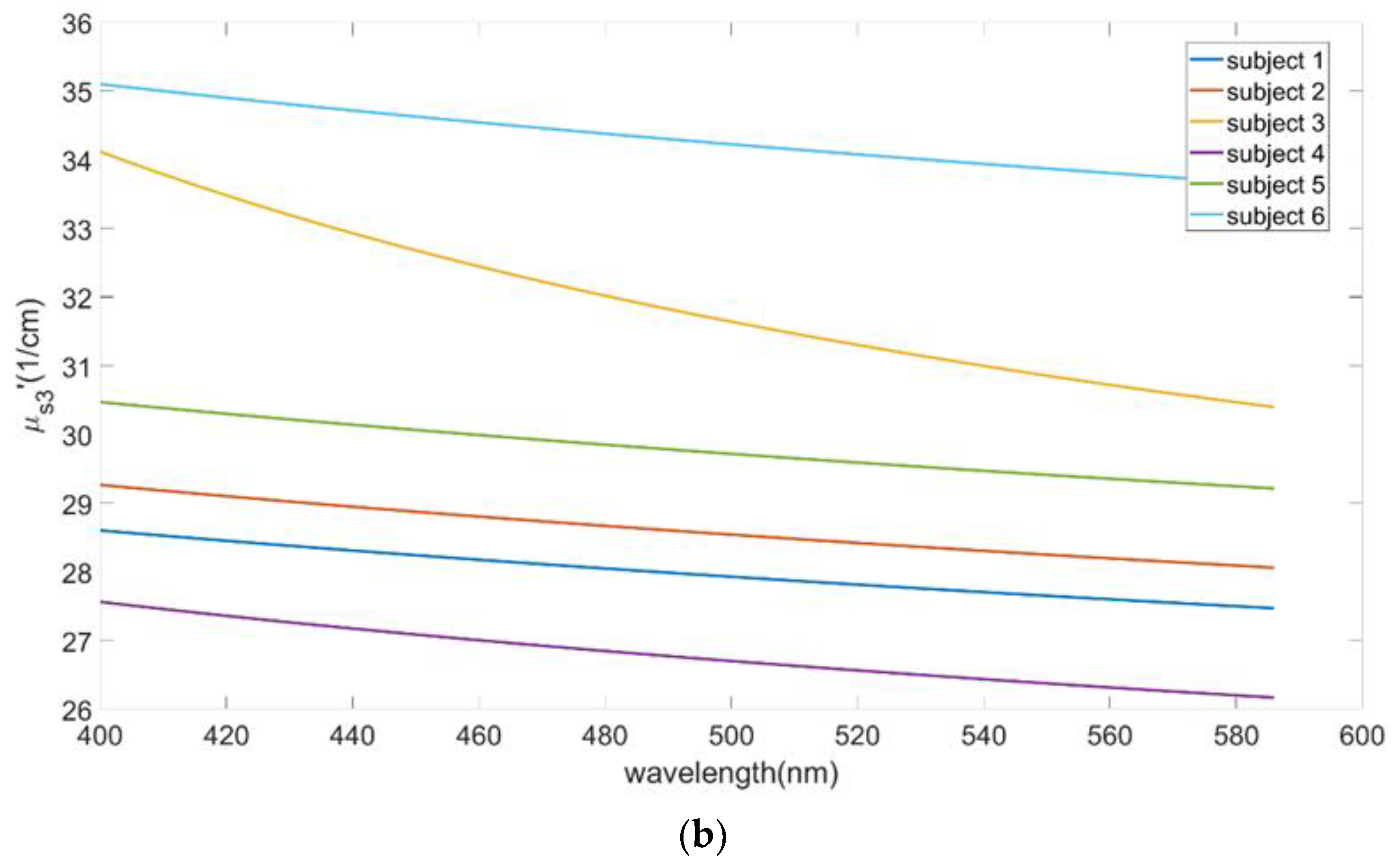
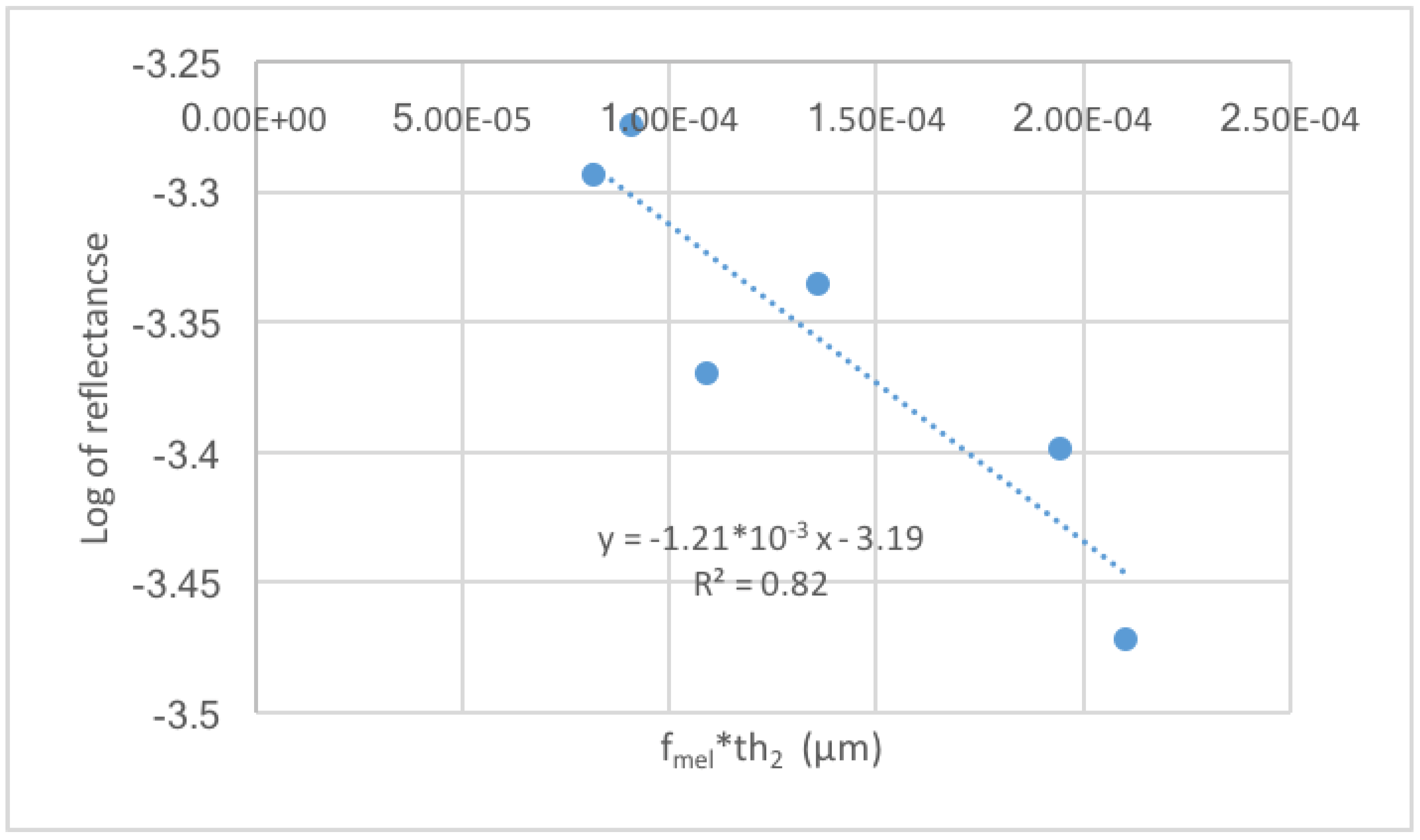
3.3. In-Vivo Cuff Occlusion Experiment Results
3.4. Comparison of Inverse Fitting Using One Term or Two Terms in the Inverse Power Law Function of μs′(λ)
4. Discussion and Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bigio, I.J.; Mourant, J.R. Ultraviolet and visible spectroscopies for tissue diagnostics: Fluorescence spectroscopy and elastic-scattering spectroscopy. Phys. Med. Biol. 1997, 42, 803–814. [Google Scholar] [CrossRef] [PubMed]
- Utzinger, U.; Richards-Kortum, R.R. Fiber optic probes for biomedical optical spectroscopy. J. Biomed. Opt. 2003, 8, 121–147. [Google Scholar] [CrossRef]
- Bigio, I.J.; Bown, S.G. Spectroscopic sensing of cancer and cancer therapy: Current status of translational research. Cancer Biol. Ther. 2004, 3, 259–267. [Google Scholar] [CrossRef]
- Zonios, G.; Dimou, A.; Bassukas, I.; Galaris, D.; Tsolakidis, A.; Kaxiras, E. Melanin absorption spectroscopy: New method for noninvasive skin investigation and melanoma detection. J. Biomed. Opt. 2008, 13, 014017. [Google Scholar] [CrossRef] [PubMed]
- Tuchin, V.V. Tissue Optics: Light Scattering Methods and Instruments for Medical Diagnosis; SPIE: Bellingham, WA, USA, 2015. [Google Scholar]
- Groenhuis, R.A.J.; Ferwerda, H.A.; Bosch, J.J.T. Scattering and absorption of turbid materials determined from reflection measurements. 1: Theory. Appl. Opt. 1983, 22, 2456–2462. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Jacques, S.L.; Zheng, L. MCML–Monte Carlo modeling of light transport in multi-layered tissues. Comput. Methods Programs Biomed. 1995, 47, 131–146. [Google Scholar] [CrossRef]
- Zhu, C.; Liu, Q. Review of Monte Carlo modeling of light transport in tissues. J. Biomed. Opt. 2013, 18, 50902. [Google Scholar] [CrossRef] [PubMed]
- Kienle, A.; Patterson, M.S. Determination of the optical properties of turbid media from a single Monte Carlo simulation. Phys. Med. Biol. 1996, 41, 2221. [Google Scholar] [CrossRef] [PubMed]
- Yudovsky, D.; Pilon, L. Simple and accurate expressions for diffuse reflectance of semi-infinite and two-layer absorbing and scattering media. Appl. Opt. 2009, 48, 6670–6683. [Google Scholar] [CrossRef]
- Yudovsky, D.; Pilon, L. Rapid and accurate estimation of blood saturation, melanin content, and epidermis thickness from spectral diffuse reflectance. Appl. Opt. 2010, 49, 1707–1719. [Google Scholar] [CrossRef]
- Fredriksson, I.; Larsson, M.; Strömberg, T. Inverse Monte Carlo method in a multilayered tissue model for diffuse reflectance spectroscopy. J. Biomed. Opt. 2012, 17, 047004. [Google Scholar] [CrossRef] [PubMed]
- Yudovsky, D.; Laurent, P. Retrieving skin properties from in vivo spectral reflectance measurements. J. Biophotonics 2011, 4, 305–314. [Google Scholar] [CrossRef]
- Nishidate, I.; Aizu, Y.; Mishina, H. Estimation of melanin and hemoglobin in skin tissue using multiple regression analysis aided by Monte Carlo simulation. J. Biomed. Opt. 2004, 9, 700–711. [Google Scholar] [CrossRef] [PubMed]
- Zhong, X.; Wen, X.; Zhu, D. Lookup-table-based inverse model for human skin reflectance spectroscopy: Two-layered Monte Carlo simulations and experiments. Opt. Express 2014, 22, 1852–1864. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M.; Hennessy, R.; Markey, M.K.; Tunnell, J.W. Verification of a two-layer inverse Monte Carlo absorption model using multiple source-detector separation diffuse reflectance spectroscopy. Biomed. Opt. Express 2014, 5, 40–53. [Google Scholar] [CrossRef]
- Wang, Q.; Le, D.; Ramella-Roman, J.; Pfefer, J. Broadband ultraviolet-visible optical property measurement in layered turbid media. Biomed. Opt. Express 2012, 3, 1226–1240. [Google Scholar] [CrossRef]
- Yudovsky, D.; Durkin, A.J. Spatial frequency domain spectroscopy of two layer media. J. Biomed. Opt. 2011, 16, 107005. [Google Scholar] [CrossRef]
- Yudovsky, D.; Nguyen, J.Q.; Durkin, A.J. In Vivo spatial frequency domain spectroscopy of two layer media. J. Biomed. Opt. 2012, 17, 107006. [Google Scholar] [CrossRef]
- Tsui, S.-Y.; Wang, C.-Y.; Huang, T.-H.; Sung, K.-B. Modelling spatially-resolved diffuse reflectance spectra of a multi-layered skin model by artificial neural networks trained with Monte Carlo simulations. Biomed. Opt. Express 2018, 9, 1531–1544. [Google Scholar] [CrossRef]
- Hsieh, H.-P.; Ko, F.-H.; Sung, K.-B. Hybrid method to estimate two-layered superficial tissue optical properties from simulated data of diffuse reflectance spectroscopy. Appl. Opt. 2018, 57, 3038–3046. [Google Scholar] [CrossRef]
- Doronin, A.; Meglinski, I.; Bykov, A.V.; Rushmeier, H. Determination of human skin optical properties from hyper spectral data with deep-learning neural networks (conference presentation). In Optical Biopsy XVI: Toward Real-Time Spectroscopic Imaging and Diagnosis; International Society for Optics and Photonics: Bellingham, WA, USA, 2018; Volume 10489. [Google Scholar]
- Qu, J.; MacAulay, C.; Lam, S.; Palcic, B. Optical properties of normal and carcinomatous bronchial tissue. Appl. Opt. 1994, 33, 7397–7405. [Google Scholar] [CrossRef] [PubMed]
- Jacques, S.L.; McAuliffe, D.J. The melanosome: Threshold temperature for explosive vaporization and internal absorption coefficient during pulsed laser irradiation. Photochem. Photobiol. 1991, 53, 769–775. [Google Scholar] [CrossRef] [PubMed]
- Jacques, S.L. Optical properties of biological tissues: A review. Phys. Med. Biol. 2013, 58, R37. [Google Scholar] [CrossRef]
- Buiteveld, H.; Hakvoort, J.; Donze, M. Optical Properties of Pure Water. In Ocean Optics XII; International Society for Optics and Photonics: Bellingham, WA, USA, 1994. [Google Scholar]
- Nunez, A.S. A Physical Model of Human Skin and Its Application for Search and Rescue; Air Force Inst of Tech Wright-Patterson Afb oh School of Engineering: Greene County, OH, USA, 2009. [Google Scholar]
- Prahl, S. Optical Absorption of Hemoglobin. Available online: http://omlc.ogi.edu/spectra/hemoglobin/hemestruct/index.html (accessed on 8 January 2018).
- Bashkatov, A.N.; Genina, E.A.; Tuchin, V.V. Optical properties of skin, subcutaneous, and muscle tissues: A review. J. Innov. Opt. Health Sci. 2011, 4, 9–38. [Google Scholar] [CrossRef]
- Su, J.-W.; Hsu, W.-C.; Tjiu, J.-V.; Chiang, C.-P.; Huang, C.-W.; Sung, K.B. Investigation of influences of the paraformaldehyde fixation and paraffin embedding removal process on refractive indices and scattering properties of epithelial cells. J. Biomed. Opt. 2014, 19, 075007. [Google Scholar] [CrossRef]
- Alerstam, E.; Tomas, S.; Stefan, A.-E. Parallel computing with graphics processing units for high-speed Monte Carlo simulation of photon migration. J. Biomed. Opt. 2008, 13, 060504. [Google Scholar] [CrossRef]
- Chopra, K.; Calva, D.; Sosin, M.; Tadisina, K.K.; Banda, A.; De La Cruz, C.; Chaudhry, M.R.; Legesse, T.; Drachenberg, C.B.; Manson, P.N.; et al. A comprehensive examination of topographic thickness of skin in the human face. Aesthet. Surg. J. 2015, 35, 1007–1013. [Google Scholar] [CrossRef]
- Broxterman, R.M.; Ade, C.J.; Craig, J.C.; Wilcox, S.L.; Schlup, S.J.; Barstow, T.J. Influence of blood flow occlusion on muscle oxygenation characteristics and the parameters of the power-duration relationship. J. Appl. Physiol. 2015, 118, 880–889. [Google Scholar] [CrossRef]
- Martelli, F.; Del Bianco, S.; Zaccanti, G.; Pifferi, A.; Torricelli, A.; Bassi, A.; Taroni, P.; Cubeddu, R. Phantom validation and in vivo application of an inversion procedure for retrieving the optical properties of diffusive layered media from time-resolved reflectance measurements. Opt. Lett. 2004, 29, 2037–2039. [Google Scholar] [CrossRef]
- Abay, T.Y.; Kyriacou, P.A. Photoplethysmography for blood volumes and oxygenation changes during intermittent vascular occlusions. J. Clin. Monit. Comput. 2018, 32, 447–455. [Google Scholar] [CrossRef]
- Abay, T.Y.; Kyriacou, P.A. Reflectance photoplethysmography as noninvasive monitoring of tissue blood perfusion. IEEE Trans. Biomed. Eng. 2015, 62, 2187–2195. [Google Scholar] [CrossRef]
- Chatterjee, S.; Abay, T.Y.; Phillips, J.P.; Kyriacou, P.A. Investigating optical path and differential pathlength factor in reflectance photoplethysmography for the assessment of perfusion. J. Biomed. Opt. 2018, 23, 075005. [Google Scholar] [CrossRef]
- Tuncali, B.; Boya, H.; Kayhan, Z.; Arac, S. Tourniquet pressure settings based on limb occlusion pressure determination or arterial occlusion pressure estimation in total knee arthroplasty? A prospective, randomized, double blind trial. Acta Orthopaedica et Traumatologica Turcica 2018, 52, 256–260. [Google Scholar] [CrossRef]
- Sung, K.B.; Shih, K.W.; Hsu, F.W.; Hsieh, H.P.; Chuang, M.J.; Hsiao, Y.H.; Su, Y.H.; Tien, G.H. Accurate extraction of optical properties and top layer thickness of two-layered mucosal tissue phantoms from spatially resolved reflectance spectra. J. Biomed. Opt. 2014, 19, 077002. [Google Scholar] [CrossRef]
- Suzuki, S.; Takasaki, S.; Ozaki, T.; Kobayashi, Y. Tissue oxygenation monitor using NIR spatially resolved spectroscopy. In Optical Tomography and Spectroscopy of Tissue III; International Society for Optics and Photonics: Bellingham, WA, USA, 1999; Volume 3597. [Google Scholar]
- Jonasson, H.; Fredriksson, I.; Bergstrand, S.; Östgren, C.J.; Larsson, M.; Strömberg, T. In Vivo characterization of light scattering properties of human skin in the 475- to 850-nm wavelength range in a Swedish cohort. J. Biomed. Opt. 2018, 23, 121608. [Google Scholar] [CrossRef]
- Strömberg, T.; Sjöberg, F.; Bergstrand, S. Temporal and spatiotemporal variability in comprehensive forearm skin microcirculation assessment during occlusion protocols. Microvasc. Res. 2017, 113, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Sung, K.-B.; Chen, H.-H. Enhancing the sensitivity to scattering coefficient of the epithelium in a two-layered tissue model by oblique optical fibers: Monte Carlo study. J. Biomed. Opt. 2012, 17, 107003. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, R.A.; Arifler, D.; Chang, S.K.; Pavlova, I.; Hussain, I.A.; Mack, V.; Knight, B.; Richards-Kortum, R.; Gillenwater, A.M. Ball lens coupled fiber-optic probe for depth-resolved spectroscopy of epithelial tissue. Opt. Lett. 2005, 30, 1159–1161. [Google Scholar] [CrossRef]
| thx (μm) | μax (cm−1) | μsx (cm−1) | gx | |
|---|---|---|---|---|
| Upper epidermis (x = 1) | 10–60 | 0.1–5.0 | fixed at 1.3 × μs2 | 0.835 |
| Lower epidermis (x = 2) | 10–60 | 1–350 | 10–700 | 0.75 |
| Dermis (x = 3) | Inf | 0.01–16 | 10–500 | 0.715 |
| Inverse Procedure | fblood | StO2 | fmel × th2 | μs2′ | μs3′ | th1 + th2 |
|---|---|---|---|---|---|---|
| YA | 5.3% (5.4%) | 10.1% (16.3%) | 20.4% (28.5%) | 43.1% (33.4%) | 1.9% (2.1%) | 34.8% (52.4%) |
| ZA | 6.3% (4.5%) | 10.1% (16.5%) | 25.3% (29.7%) | 46.2% (29.0%) | 1.6% (1.2%) | 35.6% (47.9%) |
| YB | 6.1% (5.9%) | 10.1% (16.1%) | 23.4% (28.8%) | 28.5% (24.5%) | 2.4% (2.2%) | − |
| ZB | 7.1% (5.6%) | 9.9% (16.0%) | 28.4% (38.7%) | 18.3% (18.1%) | 1.9% (1.1%) | − |
| Ender | Age | fblood | StO2 | fmel × th2 (μm) | th1 (μm) | th2 (μm) | |
|---|---|---|---|---|---|---|---|
| subject 1 | Male | 23 | 0.129% | 99% | 0.804 | 27.1 | 48.1 |
| subject 2 | Male | 23 | 0.217% | 62% | 1.630 | 17.9 | 46.5 |
| subject 3 | Male | 23 | 0.284% | 54% | 1.059 | 35.8 | 45.3 |
| subject 4 | Female | 23 | 0.244% | 37% | 0.223 | 39.0 | 18.9 |
| subject 5 | Male | 23 | 0.140% | 99% | 3.846 | 10.4 | 36.9 |
| subject 6 | Male | 45 | 0.155% | 40% | 1.360 | 12.5 | 47.8 |
| Reference | fblood | StO2 | fmel | μs2′ | μs3′ |
|---|---|---|---|---|---|
| [18] | 0.78–2.06% | 34–64% | 4.8–24% | - | - |
| [19] | 0.23–0.35% | 51.6–60.3% | 11–16% | - | - |
| [20] | 0.14–0.27% | 84–100% | 7.6–17.2% | 12.5–200 cm−1 | 5.7–57 cm−1 |
| [43] | - | - | - | 10–40 cm−1 | 10–40 cm−1 |
| [44] | 1.742 | 47% | - | - | - |
| This study | 0.09–0.28% | 37–99% | 1.3–10% | 5–180 cm−1 | 26–36 cm−1 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, C.-Y.; Kao, T.-C.; Chen, Y.-F.; Su, W.-W.; Shen, H.-J.; Sung, K.-B. Validation of an Inverse Fitting Method of Diffuse Reflectance Spectroscopy to Quantify Multi-Layered Skin Optical Properties. Photonics 2019, 6, 61. https://doi.org/10.3390/photonics6020061
Wang C-Y, Kao T-C, Chen Y-F, Su W-W, Shen H-J, Sung K-B. Validation of an Inverse Fitting Method of Diffuse Reflectance Spectroscopy to Quantify Multi-Layered Skin Optical Properties. Photonics. 2019; 6(2):61. https://doi.org/10.3390/photonics6020061
Chicago/Turabian StyleWang, Chiao-Yi, Tzu-Chia Kao, Yin-Fu Chen, Wen-Wei Su, Hsin-Jou Shen, and Kung-Bin Sung. 2019. "Validation of an Inverse Fitting Method of Diffuse Reflectance Spectroscopy to Quantify Multi-Layered Skin Optical Properties" Photonics 6, no. 2: 61. https://doi.org/10.3390/photonics6020061
APA StyleWang, C.-Y., Kao, T.-C., Chen, Y.-F., Su, W.-W., Shen, H.-J., & Sung, K.-B. (2019). Validation of an Inverse Fitting Method of Diffuse Reflectance Spectroscopy to Quantify Multi-Layered Skin Optical Properties. Photonics, 6(2), 61. https://doi.org/10.3390/photonics6020061




