Intratarsal Keratinous Cyst Clinically Misdiagnosed as a Chalazion
Abstract
1. Introduction
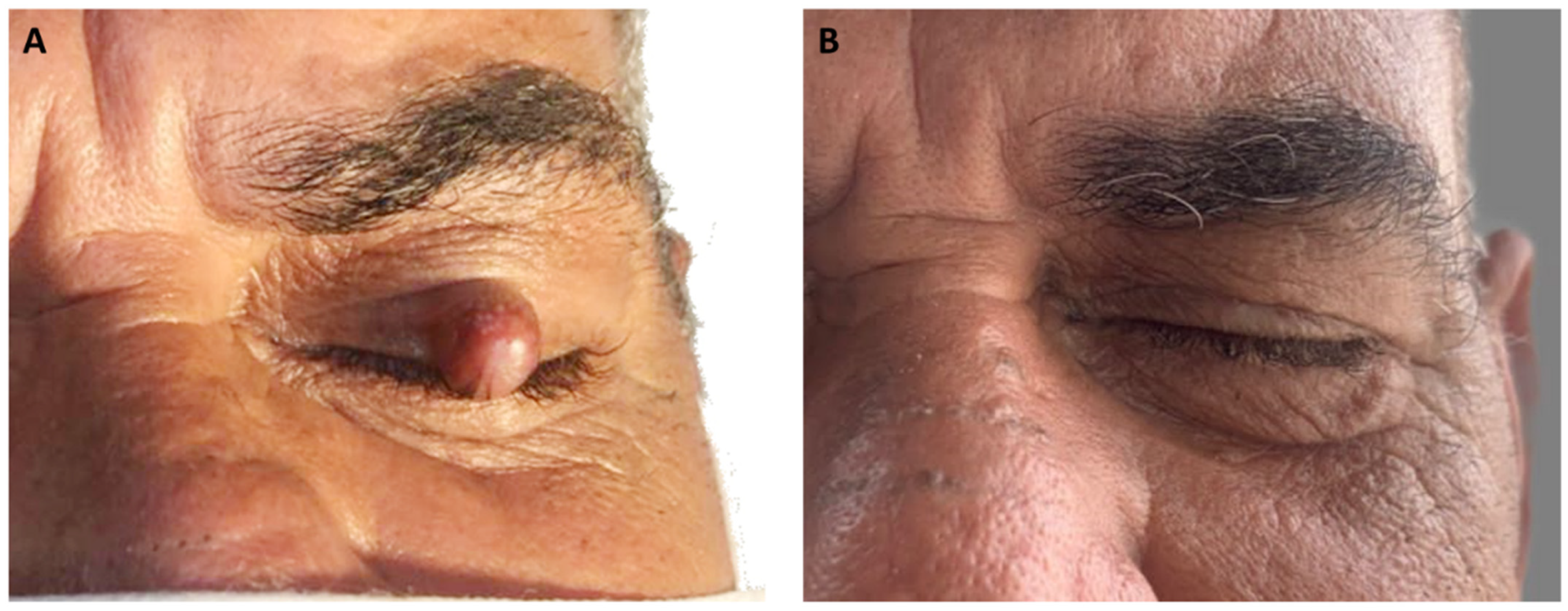
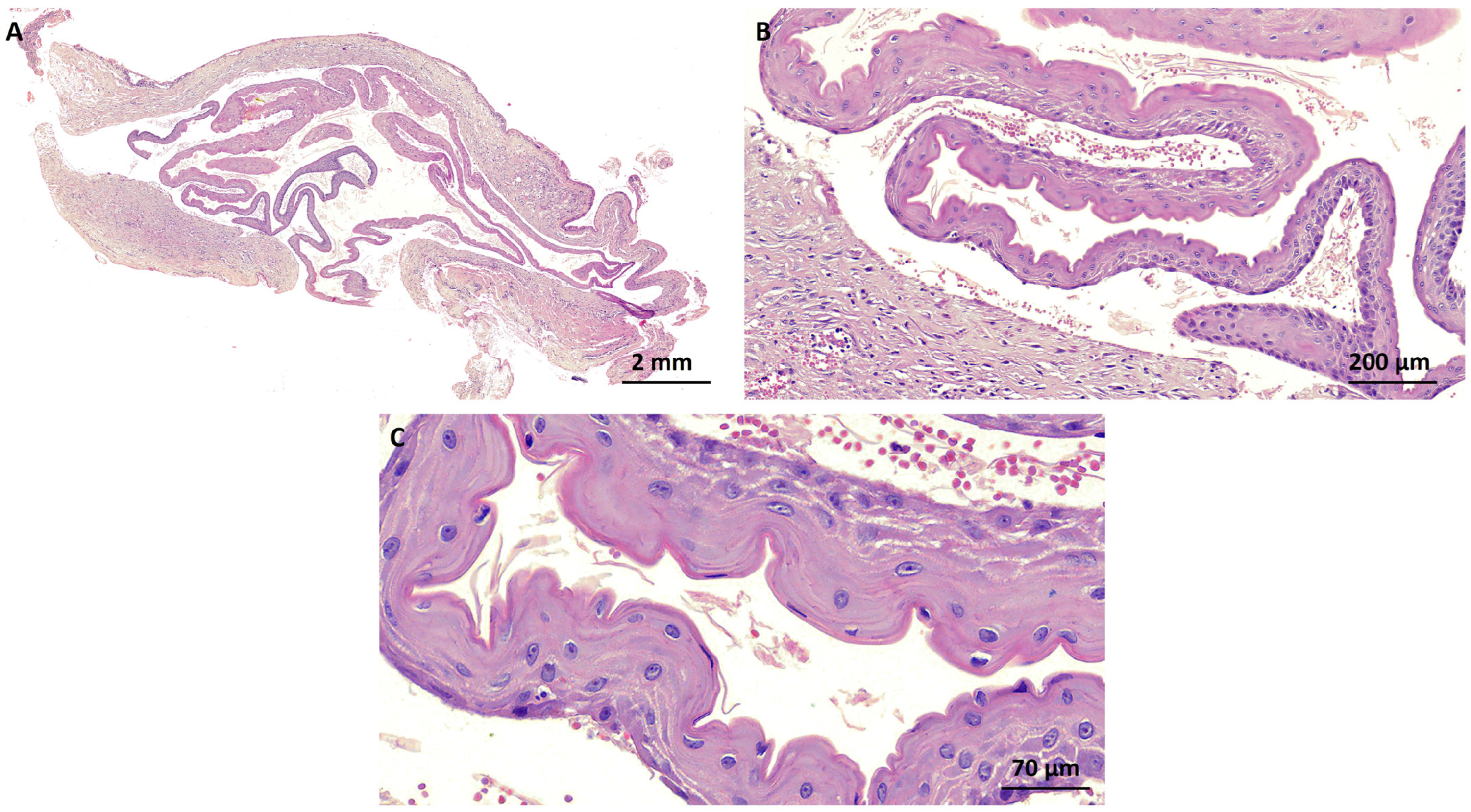
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jakobiec, F.A.; Mehta, M.; Iwamoto, M.; Hatton, M.P.; Thakker, M.; Fay, A. Intratarsal Keratinous Cysts of the Meibomian Gland: Distinctive Clinicopathologic and Immunohistochemical Features in 6 Cases. Am. J. Ophthalmol. 2010, 149, 82–94. [Google Scholar] [CrossRef] [PubMed]
- Jakobiec, F.A.; Cortes Barrantes, P.; Ma, L.; Lee, N.G. Complex Intratarsal Cyst with a Mixed Ciliated Respiratory-Type and Squamous Epithelial Lining. Ocul. Oncol. Pathol. 2020, 6, 151–158. [Google Scholar] [CrossRef] [PubMed]
- AlRubaian, A.; Alkatan, H.M.; Al-Faky, Y.H.; Alsuhaibani, A.H. Tarsal-related cysts: Different diagnoses with similar presentations. Saudi J. Ophthalmol. 2019, 33, 209–213. [Google Scholar] [CrossRef] [PubMed]
- Tang, T.; Brownstein, S.; Chen, H.; Jordan, D.R.; Iacob, C.E.; Blanco, P.; Farmer, J. Histopathological Study on the Proposed Pathogenesis of Intratarsal Keratinous Cysts. Ophthalmic Plast. Reconstr. Surg. 2019, 35, 365–368. [Google Scholar] [CrossRef] [PubMed]
- AlRubaian, A.; Alkatan, H.M.; Al-Faky, Y.H.; Alsuhaibani, A.H. Clinical features differentiating intratarsal keratinous cyst from chalazion. Int. Ophthalmol. 2020, 40, 2041–2045. [Google Scholar] [CrossRef] [PubMed]
- Wolkow, P.; Jakobiec, F.A.; Yoon, M.K. Intratarsal keratinous eyelid cysts in Gorlin syndrome: A review and reappraisal. Surv. Ophthalmol. 2018, 63, 711–718. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.A.; Kim, N.; Choung, H.K.; Lee, M.J.; Lee, C.; Khwarg, S.I. Clinical features of intratarsal keratinous cysts. Eye 2016, 30, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.S.; Meyer, D.R.; Carlson, J.A. Intratarsal keratinous cysts of the meibomian gland (a sebaceous duct cyst): Report of 2 cases. Am. J. Dermatopathol. 2011, 33, 624–627. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.D.; Li, X.; Li, M.; Zhao, J.; Zhou, K.J.; Qu, J. Clinicopathological features and surgical treatment of intratarsal keratinous cysts. Am. J. Dermatopathol. 2013, 35, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Wojno, T.H.; Grossniklaus, H.E. Multiple intratarsal keratinous cysts of the eyelid. Ophthalmic Plast. Reconstr. Surg. 2012, 28, e116. [Google Scholar] [CrossRef] [PubMed]
- Cunha, J.L.S.; Andrade, A.O.; Cavalcante, I.L.; Barros, C.C.D.S.; Sousa Neto, S.S.; Barros, J.M.; Leite, L.S.D.S.; Félix, F.A.; Turatti, E.; Carvalho, F.S.R.; et al. Clinicopathologic analysis of oral dermoid and epidermoid cysts: A Brazilian multicenter study. Braz. Oral Res. 2023, 37, e107. [Google Scholar] [CrossRef] [PubMed]
- Raza Rizvi, S.A.; Alam, M.S.; Akhtar, K. Eyelid sebaceous gland carcinoma: Varied presentations and reconstruction outcome. Oman J. Ophthalmol. 2018, 11, 21–27. [Google Scholar] [PubMed]
- Rajak, S.N.; James, C.; Selva, D. The clinical, histological and immunohistochemical characteristics and nomenclature of meibomian gland ductal cysts (intratarsal keratinous cysts) and eyelid steatocystomas. Eye 2017, 31, 736–740. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Charles, N.C.; Jakobiec, F.A.; Sherwood, P.; Belinsky, I. Multicameral Steatocystoma Simplex of the Caruncle. Ophthalmic Plast. Reconstr. Surg. 2021, 37, e107–e109. [Google Scholar] [CrossRef] [PubMed]
- Rajaii, F.; Ghafourian, A.; Eberhart, C.G. Intratarsal keratinous cyst—An emerging entity. Case Rep. Ophthalmol. 2013, 4, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.; Chang, S.E.; Choi, J.H.; Sung, K.J.; Moon, K.C.; Koh, J.K. Clinical and histologic features of 64 cases of steatocystoma multiplex. J. Dermatol. 2002, 29, 152–156. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cunha, J.L.S.; Andrade, C.E.S.; da Cunha Filho, F.A.P.; da Paz, A.R.; Gordón-Núñez, M.A.; Alves, P.M.; Nonaka, C.F.W. Intratarsal Keratinous Cyst Clinically Misdiagnosed as a Chalazion. Dermatopathology 2024, 11, 142-146. https://doi.org/10.3390/dermatopathology11020014
Cunha JLS, Andrade CES, da Cunha Filho FAP, da Paz AR, Gordón-Núñez MA, Alves PM, Nonaka CFW. Intratarsal Keratinous Cyst Clinically Misdiagnosed as a Chalazion. Dermatopathology. 2024; 11(2):142-146. https://doi.org/10.3390/dermatopathology11020014
Chicago/Turabian StyleCunha, John Lennon Silva, Clenia E. S. Andrade, Fernando A. P. da Cunha Filho, Alexandre R. da Paz, Manuel A. Gordón-Núñez, Pollianna M. Alves, and Cassiano F. W. Nonaka. 2024. "Intratarsal Keratinous Cyst Clinically Misdiagnosed as a Chalazion" Dermatopathology 11, no. 2: 142-146. https://doi.org/10.3390/dermatopathology11020014
APA StyleCunha, J. L. S., Andrade, C. E. S., da Cunha Filho, F. A. P., da Paz, A. R., Gordón-Núñez, M. A., Alves, P. M., & Nonaka, C. F. W. (2024). Intratarsal Keratinous Cyst Clinically Misdiagnosed as a Chalazion. Dermatopathology, 11(2), 142-146. https://doi.org/10.3390/dermatopathology11020014






