Poikilodermatous Plaque-like Hemangioma: Case Presentation and Literature Review
Abstract
1. Introduction
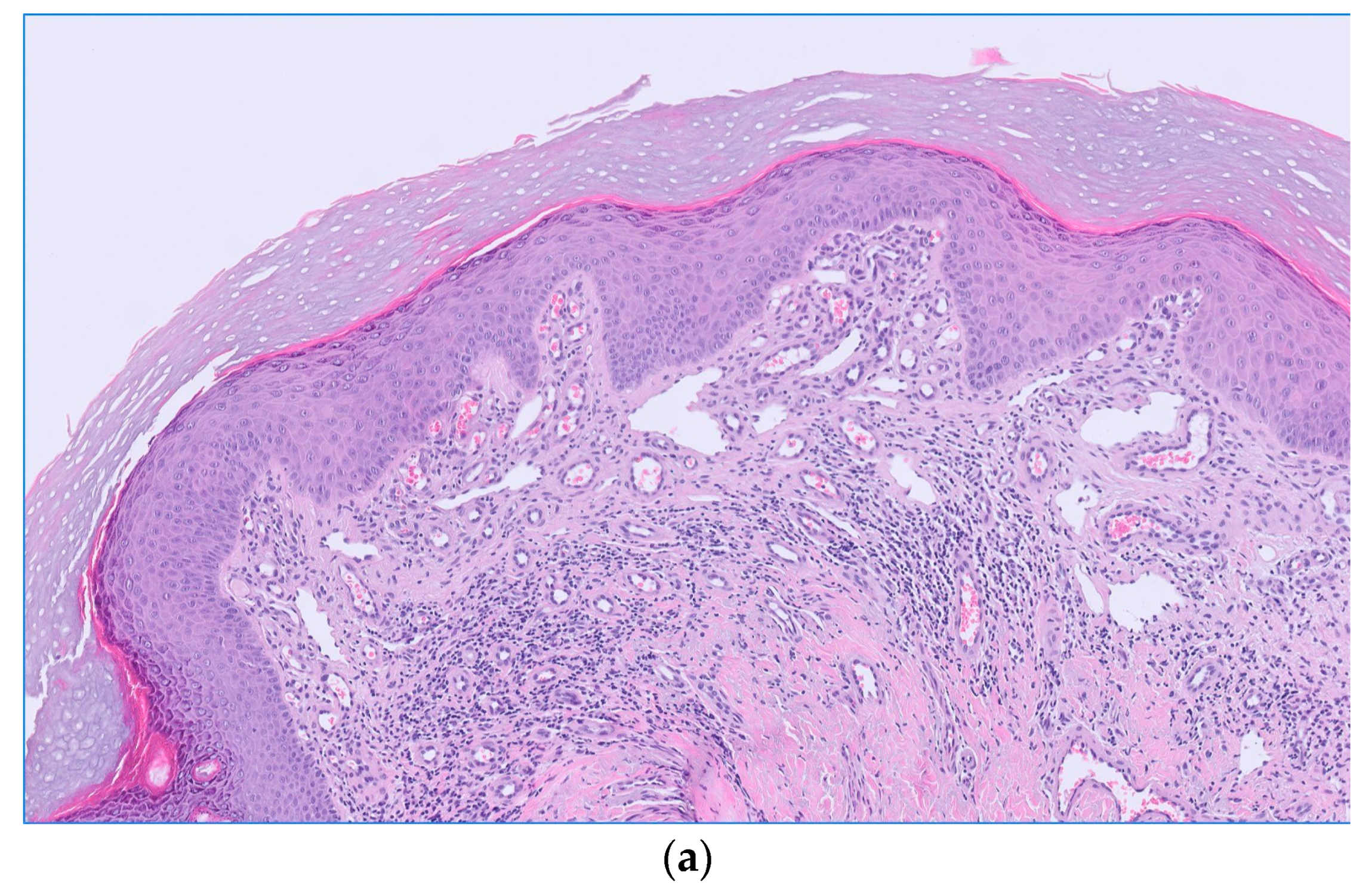
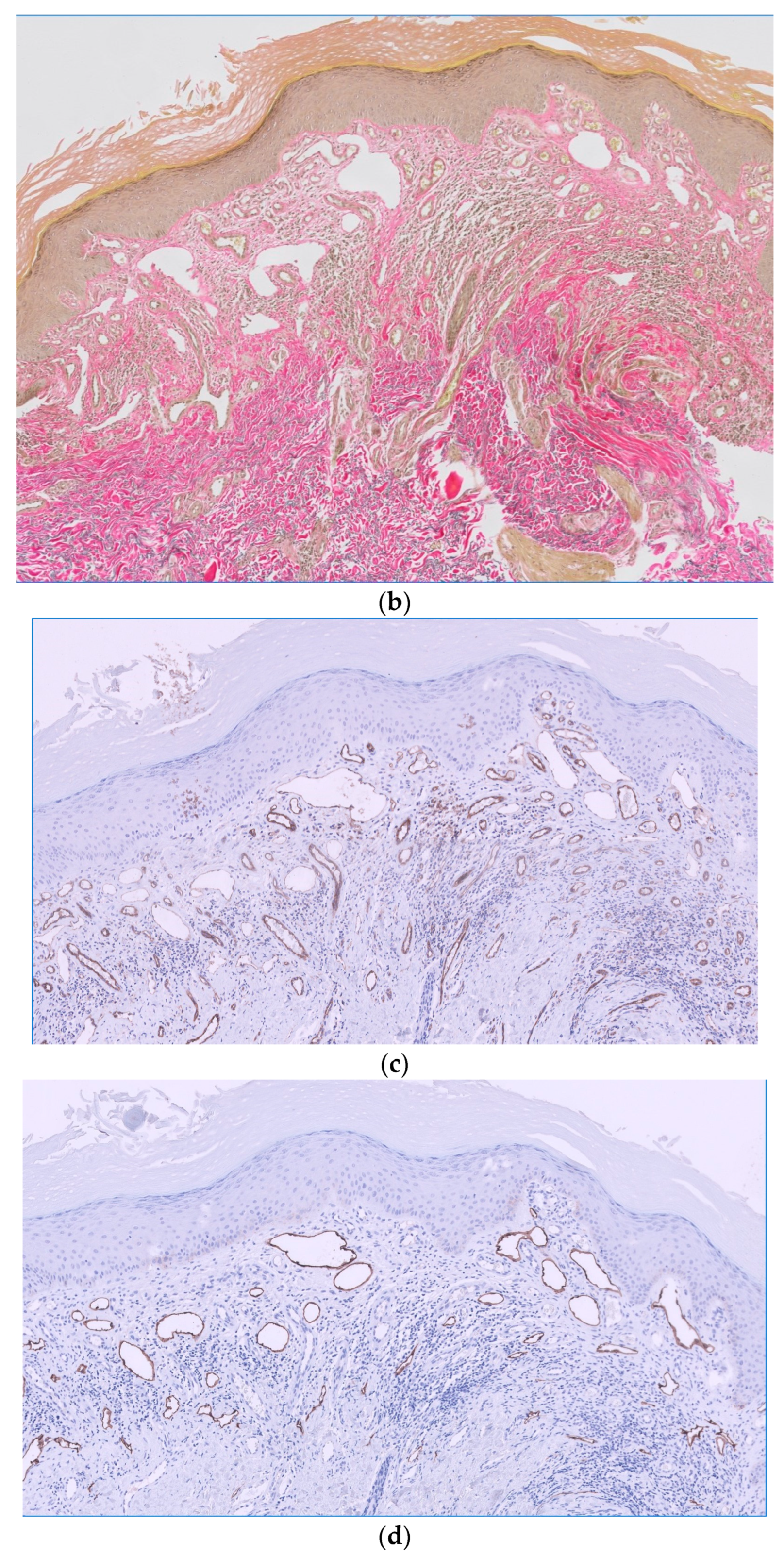
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Semkova, K.; Carr, R.; Grainger, M.; Green, R.; Hafejee, A.; Makrygeorgou, A.; Melly, L.; Motta, L.; Newsham, J.; Owen, C.; et al. Poikilodermatous plaque-like hemangioma: Case series of a newly defined entity. J. Am. Acad. Dermatol. 2019, 81, 1257–1270. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, M.; Hartman, R.; Mahalingam, M. Poikilodermatous plaque-like hemangioma: A benign vasoformative entity with reproducible histopathologic and clinical features. J. Cutan. Pathol. 2020, 47, 950–953. [Google Scholar] [CrossRef] [PubMed]
- Salgüero Fernández, I.; Hospital Gil, M.; Nájera Botello, L.; Roustan Gullón, G. Not All Is Infantile Hemangioma: An Erythematous Plaque in an Adult. Actas Dermosifiliogr. 2022, 113, 717–718. [Google Scholar] [CrossRef] [PubMed]
- Que, S.K.T.; Zwald, F.O.; Schmults, C.D. Cutaneous squamous cell carcinoma: Incidence, risk factors, diagnosis, and staging. J. Am. Acad. Dermatol. 2018, 78, 237–247. [Google Scholar] [CrossRef] [PubMed]
- Nagarajan, P.; Asgari, M.M.; Green, A.C.; Guhan, S.M.; Arron, S.T.; Proby, C.M.; Rollison, D.E.; Harwood, C.A.; Toland, A.E. Keratinocyte Carcinomas: Current Concepts and Future Research Priorities. Clin. Cancer Res. 2019, 25, 2379–2391. [Google Scholar] [CrossRef] [PubMed]
- Jawed, S.I.; Myskowski, P.L.; Horwitz, S.; Moskowitz, A.; Querfeld, C. Primary cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome): Part I. Diagnosis: Clinical and histopathologic features and new molecular and biologic markers. J. Am. Acad. Dermatol. 2014, 70, 205.e1–205.e16. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; John, A.M.; Handler, M.Z.; Schwartz, R.A. Fixed Drug Eruptions: An Update, Emphasizing the Potentially Lethal Generalized Bullous Fixed Drug Eruption. Am. J. Clin. Dermatol. 2020, 21, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Çaytemel, C.; Baykut, B.; Ağırgöl, Ş.; Caf, N.; Demir, F.T.; Türkoğlu, Z.; Uzuner, E.G. Pigmented purpuric dermatosis: Ten years of experience in a tertiary hospital and awareness of mycosis fungoides in differential diagnosis. J. Cutan. Pathol. 2021, 48, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.J.; Hunter, G.R.; Kekes-Szabo, T.; Snyder, S.; Treuth, M.S. Regional fat distribution in women and risk of cardiovascular disease. Am. J. Clin. Nutr. 1997, 65, 855–860. [Google Scholar] [CrossRef] [PubMed]
- Hahnel, E.; Blume-Peytavi, U.; Trojahn, C.; Kottner, J. Associations between skin barrier characteristics, skin conditions and health of aged nursing home residents: A multi-center prevalence and correlational study. BMC Geriatr. 2017, 17, 263. [Google Scholar] [CrossRef] [PubMed]
- Hahnel, E.; Lichterfeld, A.; Blume-Peytavi, U.; Kottner, J. The epidemiology of skin conditions in the aged: A systematic review. J. Tissue Viability 2017, 26, 20–28. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Díaz-Calvillo, P.; Vílchez-Márquez, F.; Ramos-Pleguezuelos, F.M.; Arias-Santiago, S. Poikilodermatous Plaque-like Hemangioma: Case Presentation and Literature Review. Dermatopathology 2024, 11, 147-153. https://doi.org/10.3390/dermatopathology11020015
Díaz-Calvillo P, Vílchez-Márquez F, Ramos-Pleguezuelos FM, Arias-Santiago S. Poikilodermatous Plaque-like Hemangioma: Case Presentation and Literature Review. Dermatopathology. 2024; 11(2):147-153. https://doi.org/10.3390/dermatopathology11020015
Chicago/Turabian StyleDíaz-Calvillo, Pablo, Francisco Vílchez-Márquez, Francisco Manuel Ramos-Pleguezuelos, and Salvador Arias-Santiago. 2024. "Poikilodermatous Plaque-like Hemangioma: Case Presentation and Literature Review" Dermatopathology 11, no. 2: 147-153. https://doi.org/10.3390/dermatopathology11020015
APA StyleDíaz-Calvillo, P., Vílchez-Márquez, F., Ramos-Pleguezuelos, F. M., & Arias-Santiago, S. (2024). Poikilodermatous Plaque-like Hemangioma: Case Presentation and Literature Review. Dermatopathology, 11(2), 147-153. https://doi.org/10.3390/dermatopathology11020015






