Dispositional Resilience as Mediator in Psychological Stress on Healthcare Workers: A Multi-Group Analysis of Frontline and Non-Frontline Workers
Abstract
:1. Introduction
2. Method
2.1. Participants and Procedure
2.2. Measures
2.2.1. Depression Anxiety Stress Scales (DASS-21)
2.2.2. Professional Quality of Life Scale (ProQoL)
2.2.3. Dispositional Resilience Scale
2.3. Data Analysis
3. Results
3.1. Descriptive Statistic, Correlation, and Reliability
3.2. CFA to Test the Model
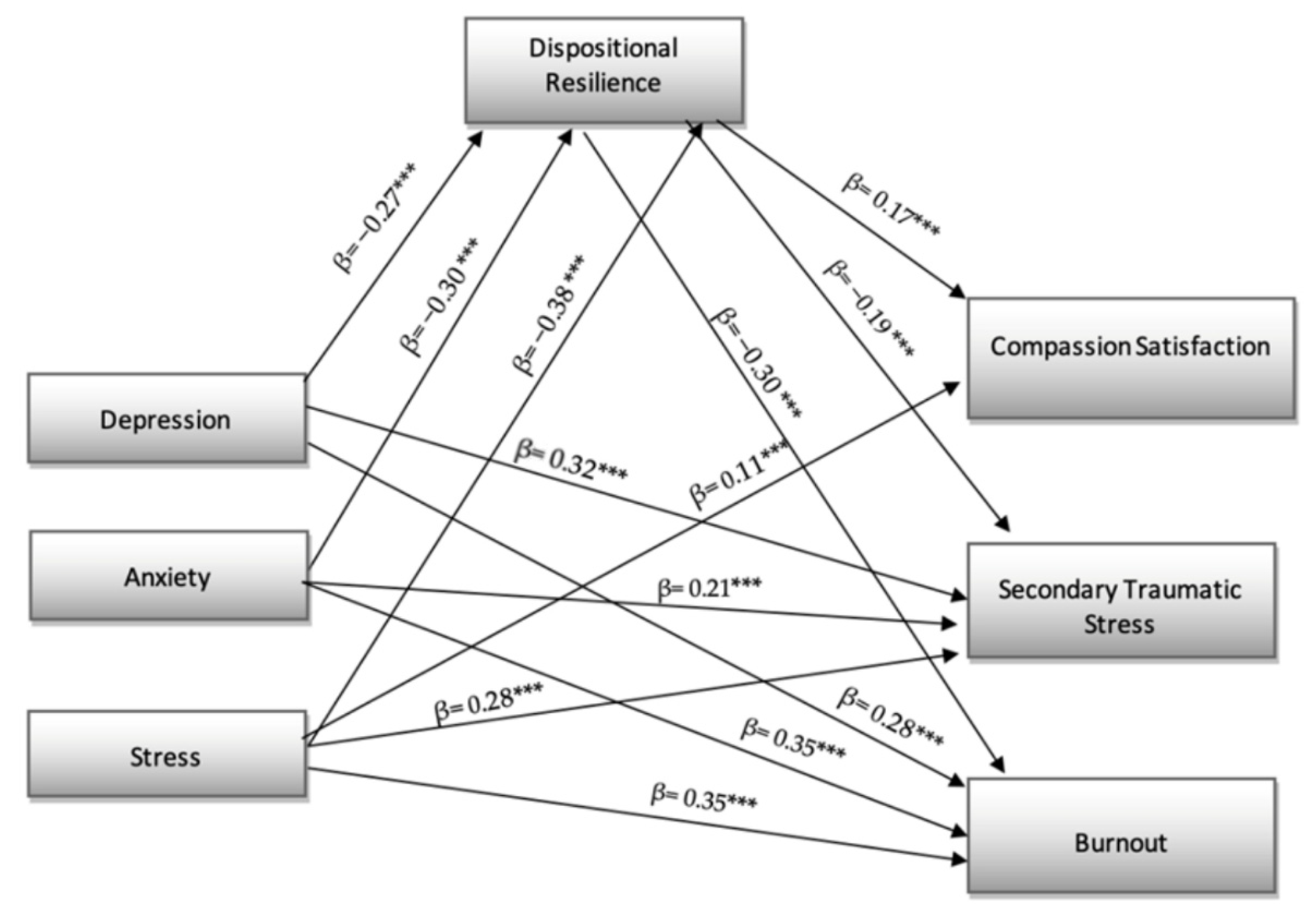
3.3. Structural Model
3.4. Directed Effect
3.5. The Mediation of Dispositional Resilience
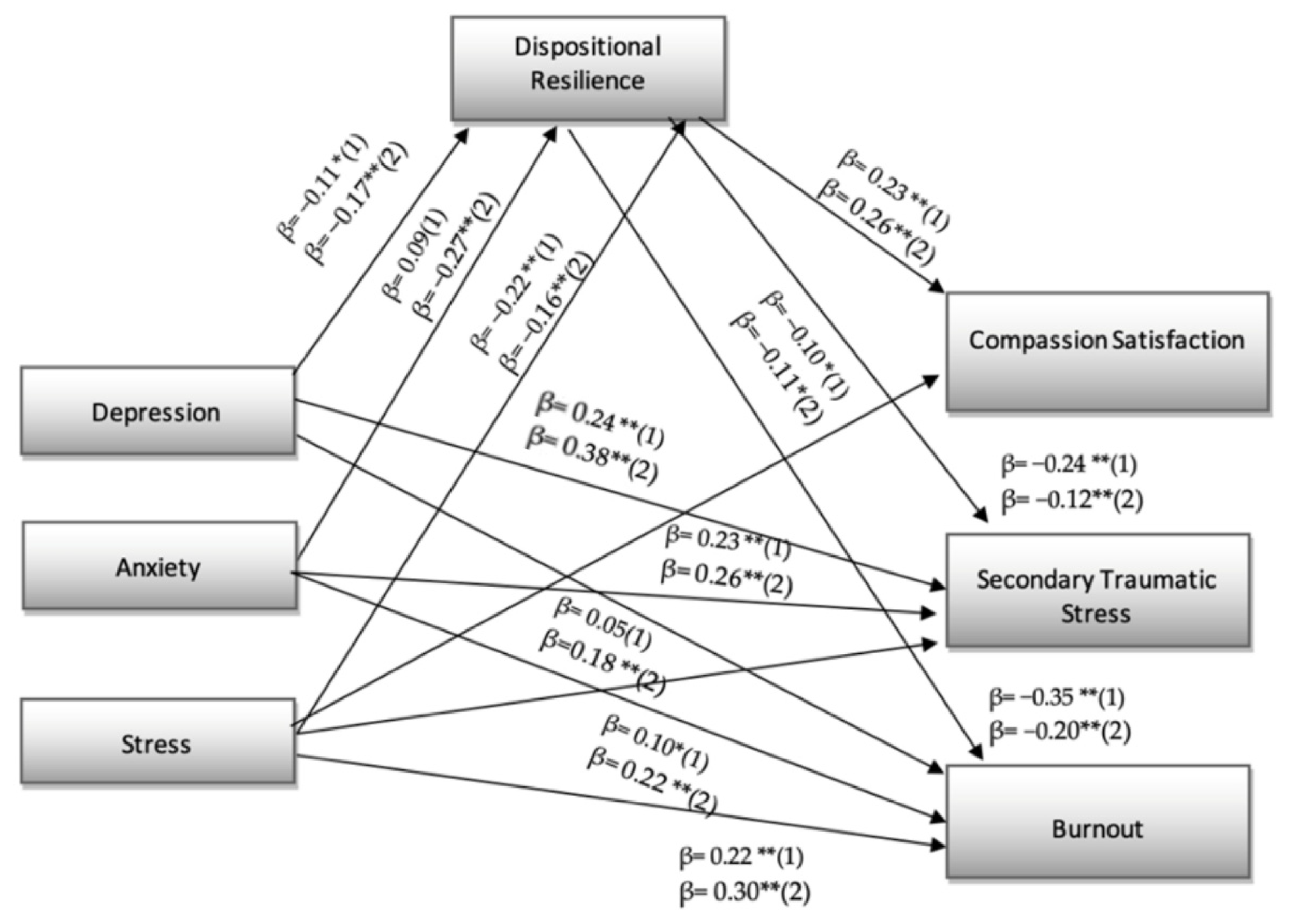
3.6. Multigroup Analysis
4. Discussion
5. Conclusions
Limits and Practical Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Mansueto, G.; Lopes, F.L.; Grassi, L.; Cosci, F. Impact of COVID-19 outbreak on Italian healthcare workers versus general population: Results from an online survey. Clin. Psychol. Psychother. 2021, 28, 1334–1345. [Google Scholar] [CrossRef] [PubMed]
- Vicentini, S.; Mercurio, A.; Romascu, C.; Battaglia, M.; Tribbia, N.; Siviero, F.; Grossi, A.; Martucci, M.M.; De Leo, D. Critical Issues of Working during the COVID-19 Pandemic: Italian Healthcare Workers’ Experience. Int. J. Environ. Res. Public Health 2022, 19, 927. [Google Scholar] [CrossRef] [PubMed]
- Felice, C.; Di Tanna, G.L.; Zanus, G.; Grossi, U. Impact of COVID-19 outbreak on healthcare workers in Italy: Results from a national E-survey. J. Community Health 2020, 45, 675–683. [Google Scholar] [CrossRef] [PubMed]
- Barello, S.; Palamenghi, L.; Graffigna, G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. 2020, 290, 113129. [Google Scholar] [CrossRef]
- Benfante, A.; Di Tella, M.; Romeo, A.; Castelli, L. Traumatic stress in healthcare workers during COVID-19 pandemic: A review of the immediate impact. Front. Psychol. 2020, 11, 569935. [Google Scholar] [CrossRef]
- Bruno, G.; Panzeri, A.; Granziol, U.; Alivernini, F.; Chirico, A.; Galli, F.; Lucidi, F.; Spoto, A.; Vidotto, G.; Bertamini, M. The Italian COVID-19 Psychological Research Consortium (IT C19PRC): General Overview and Replication of the UK Study. J. Clin. Med. 2021, 10, 52. [Google Scholar] [CrossRef]
- Chersich, M.F.; Gray, G.; Fairlie, L.; Eichbaum, Q.; Mayhew, S.; Allwood, B.; English, R.; Scorgie, F.; Luchters, S.; Simpson, G.; et al. COVID-19 in Africa: Care and protection for frontline healthcare workers. Glob. Health 2020, 16, 46. [Google Scholar] [CrossRef]
- Garfin, D.R.; Thompson, R.R.; Holman, E.A. Acute stress and subsequent health outcomes: A systematic review. J. Psychosom. Res. 2018, 112, 107–113. [Google Scholar] [CrossRef]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated with Mental Health Outcomes among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, 203976. [Google Scholar] [CrossRef]
- Elbay, R.Y.; Kurtulmuş, A.; Arpacıoğlu, S.; Karadere, E. Depression, anxiety, stress levels of physicians and associated factors in COVID-19 pandemics. Psychiatry Res. 2020, 290, 113130. [Google Scholar] [CrossRef]
- Bettinsoli, M.L.; Napier, J.L.; Di Riso, D.; Moretti, L.; Delmedico, M.; Piazzolla, A.; Moretti, B.; Bettinsoli, P. Mental Health Conditions of Italian Healthcare Professionals during the COVID-19 Disease Outbreak. Appl. Psychol. Health Well-Being 2020, 12, 1054–1073. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Sun, C.; Chen, J.J.; Jen, H.J.; Kang, X.L.; Kao, C.C.; Chou, K.R. A Large-Scale Survey on Trauma, Burnout, and Posttraumatic Growth among Nurses during the COVID-19 Pandemic. Int. J. Ment. Health Nurs. 2021, 30, 102–116. [Google Scholar] [CrossRef] [PubMed]
- Folkman, S.; Lazarus, R.S. Coping as a mediator of emotion. J. Pers. Soc. Psychol. 1988, 54, 466–475. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Kang, W.S.; Cho, A.R.; Kim, T.; Park, J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantine dh emodialysis patients. Comp. Psychiatry 2018, 87, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Rice, V.; Glass, N.; Ogle, K.R.; Parsian, N. Exploring physical health perceptions, fatigue and stress among health care professionals. J. Multidiscip. Healthc. 2014, 7, 155–161. [Google Scholar] [CrossRef]
- Buselli, R.; Corsi, M.; Baldanzi, S.; Chiumiento, M.; Del Lupo, E.; Dell’Oste, V.; Bertelloni, C.A.; Massimetti, G.; Dell’Osso, L.; Cristaudo, A.; et al. Professional Quality of Life and Mental Health Outcomes among Health Care Workers Exposed to SARS-CoV-2 (COVID-19). Int. J. Environ. Res. Public Health. 2020, 17, 6180. [Google Scholar] [CrossRef]
- Kang, L.; Li, Y.; Hu, S.; Chen, M.; Yang, C.; Yang, B.X.; Wang, Y.; Hu, J.; Lai, J.; Ma, X.; et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry 2020, 7, e14. [Google Scholar] [CrossRef]
- Lu, P.; Li, X.; Lu, L.; Zhang, Y. The psychological states of people after Wuhan eased the lockdown. PLoS ONE 2020, 15, e0241173. [Google Scholar] [CrossRef]
- Gasparro, R.; Scandurra, C.; Maldonato, N.M.; Dolce, P.; Bochicchio, V.; Valletta, A.; Sammartino, G.; Sammartin, P.; Mariniello, M.; Espedito di Lauro, A.; et al. Perceived job insecurity and depressive symptoms among Italian dentists: The moderating role of fear of COVID-19. Int. J. Environ. Res. 2020, 17, 5338. [Google Scholar] [CrossRef]
- Wańkowicz, P.; Szylińska, A.; Rotter, I. Assessment of mental health factors among health professionals depending on their contact with COVID-19 patients. Int. J. Environ. Res. 2020, 17, 5849. [Google Scholar] [CrossRef]
- Mo, Y.; Deng, L.; Zhang, L.; Lang, Q.; Liao, C.; Wang, N.; Qin, M.; Huang, H. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J. Nurs. Manag. 2020, 28, 1002–1009. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Wei, J.; Zhu, H.; Duan, Y.; Geng, W.; Hong, X.; Jiang, J.; Zhao, X.; Zhu, B. A Study of Basic Needs and Psychological Wellbeing of Medical Workers in the Fever Clinic of a Tertiary General Hospital in Beijing during the COVID-19 Outbreak. Psychother. Psychosom. 2020, 89, 252–254. [Google Scholar] [CrossRef] [PubMed]
- Sun, N.; Wei, L.; Shi, S.; Jiao, D.; Song, R.; Ma, L.; Wang, H.; Wang, C.; Wang, Z.; You, Y.; et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am. J. Infect. Control. 2020, 48, 592–598. [Google Scholar] [CrossRef] [PubMed]
- Oginska-Bulik, N. The role of coping strategies in posttraumatic growth in medical rescue workers. Med. Pract. 2014, 65, 209–217. [Google Scholar] [CrossRef]
- Oginska-Bulik, N.; Zadworna-Cieslak, M. The role of resiliency and coping strategies in occurrence of positive changes in medical rescue workers. Int. Emerg. Nurs. 2018, 39, 40–45. [Google Scholar] [CrossRef]
- Russo, S.J.; Murrough, J.W.; Han, M.H.; Charney, D.S.; Nestler, E.J. Neurobiology of resilience. Nat. Neurosci. 2012, 15, 1475–1484. [Google Scholar] [CrossRef]
- Serrão, C.; Duarte, I.; Castro, L.; Teixeira, A. Burnout and depression in portuguese healthcare workers during the covid-19 pandemic—The mediating role of psychological resilience. Int. J. Environ. Res. 2021, 18, 636. [Google Scholar] [CrossRef]
- Schneiderman, N.; Ironson, G.; Siegel, S.D. Stress and health: Psychological, behavioral, and biological determinants. Annu. Rev. Clin. Psychol. 2005, 1, 607. [Google Scholar] [CrossRef]
- Platania, S.; Paolillo, A. Validation and Measurement Invariance of the Compound PsyCap Scale (CPC-12): A Short Universal Measure of Psychological Capital. An. Psicol. 2022, 38, 63–75. [Google Scholar] [CrossRef]
- Platania, S.; Castellano, S.; Petralia, M.C.; Digrandi, F.; Coco, M.; Pizzo, M.; Di Nuovo, S. The moderating effect of the dispositional resilience on the relationship between Post-traumatic Stress Disorder and the professional quality of life of the military returning from the peacekeeping operations. Mediterr. J. Clin. Psychol. 2020, 8, 1–21. [Google Scholar] [CrossRef]
- Magnano, P.; Paolillo, A.; Platania, S.; Santisi, G. Courage as a potential mediator between personality and coping. Pers. Individ. Differ. 2017, 111, 13–18. [Google Scholar] [CrossRef]
- Platania, S.; Castellano, S.; Petralia, M.C.; Santisi, G. L’effetto Mediatore Dell’impatto Della Qualità Della Vita Nella Relazione Tra Qualità Di Vita Professionale e Stress Percepito Dei Caregiver Formali. Psicol. Della Salut. 2019, 1, 64–83. [Google Scholar] [CrossRef]
- Rushton, C.H.; Batcheller, J.; Schroeder, K.; Donohue, P. Burnout and resilience among nurses practicing in high-intensity settings. Am. J. Crit. Care 2015, 24, 412–420. [Google Scholar] [CrossRef] [PubMed]
- Luthans, F. The need for and meaning of positive organizational behavior. J. Organ. Behav. 2002, 23, 695–706. [Google Scholar] [CrossRef]
- Fredrickson, B.L.; Tugade, M.M.; Waugh, C.E.; Larkin, G.R. What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. J. Pers Soc. Psychol. 2003, 84, 365–376. [Google Scholar] [CrossRef]
- Tugade, M.M.; Fredrickson, B.L. Resilient individuals use positive emotions to bounce back from negative emotional experiences. J. Pers Soc. Psychol. 2004, 86, 320–333. [Google Scholar] [CrossRef]
- Wagnild, G.M.; Young, H.M. Development and psychometric evaluation of the Resilience Scale. J. Nurs. Meas. 1993, 1, 165–178. [Google Scholar]
- Arrogante, O.; Aparicio-Zaldivar, E. Burnout and health among critical care professionals: The mediational role of resilience. Intensive Crit. Care Nurs. 2017, 42, 110–115. [Google Scholar] [CrossRef]
- Shi, M.; Wang, X.; Bian, Y.; Wang, L. The mediating role of resilience in the relationship between stress and life satisfaction among Chinese medical students: A cross-sectional study. BMC Med. Educ. 2015, 15, 16. [Google Scholar] [CrossRef]
- Lovibond, S.H.; Lovibond, P.F. Manual for the Depression Anxiety & Stress Scales, 2nd ed.; Psychology Foundation: Sydney, Australia, 1995. [Google Scholar]
- Henry, J.D.; Crawford, J.R. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2005, 44, 227–239. [Google Scholar] [CrossRef]
- Stamm, B.H. The Pro-QOL Manual: The Professional Quality of Life Scale: Compassion Satisfaction, Burnout & Compassion Fatigue/Secondary Trauma Scales; Sidran Press: Baltimore, MD, USA, 2005. [Google Scholar]
- Stamm, B.H. The ProQOL Test Manual, 2nd ed.; Sidran Press and the ProQOL.org.: Towson, MD, USA, 2008. [Google Scholar]
- Kobasa, S.C. Stressful life events, personality, and health: An inquiry into hardiness. J. Pers. Soc. Psychol. 1979, 37, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Kobasa, S.C.; Maddi, S.R.; Kahn, S. Hardiness and health: A prospective study. J. Pers. Soc. Psychol. 1982, 42, 168–177. [Google Scholar] [CrossRef] [PubMed]
- Picardi, A.; Bartone, P.T.; Querci, R.; Bitetti, D.; Tarsitani, L.; Roselli, V.; Maraone, A.; Fabi, E.; De Michele, F.; Gaviano, I.; et al. Development and validation of the Italian version of the 15-item Dispositional Resilience Scale. Riv. Psichiatr. 2012, 3, 231–237. [Google Scholar] [CrossRef]
- Byrne, B.M. Structural Equation Modeling with AMOS, EQS, and LISREL: Comparative Approaches to Testing for the Factorial Validity of a Measuring Instrument. Int. J. Test. 2001, 1, 55–86. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Arbuckle, J.L.; Wothke, W. Amos 4.0 User’s Guide; Marketing Department, SPSS Inc.: Chicago, IL, USA, 1999. [Google Scholar]
- Hayes, A.F.; Scharkow, M. The Relative Trustworthiness of Inferential Tests of the Indirect Effect in Statistical Differences in Analysis: Does Method Really Matter? Psychol. Sci. 2013, 24, 1918–1927. [Google Scholar] [CrossRef] [PubMed]
- Malhotra, N.K.; Kim, S.S.; Patil, A. Common method variance in IS research: A comparison of alternative approaches and a reanalysis of past research. Manag. Sci. 2006, 52, 1865–1883. [Google Scholar] [CrossRef]
- James, L.R.; Mulaik, S.A.; Brett, J.M. A Tale of Two Methods. Organ. Res. Methods 2006, 9, 233–244. [Google Scholar] [CrossRef]
- Shrout, P.E.; Bolger, N. Mediation in Experimental and Nonexperimental Studies: New Procedures and Recommendations. Psychol. Methods 2002, 7, 422–445. [Google Scholar] [CrossRef]
- Cheung, G.W.; Rensvold, R.B. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct. Equ. Model. 2002, 9, 233–255. [Google Scholar] [CrossRef]
- Platania, S.; Morando, M.; Santisi, G. Organisational Climate, Diversity Climate and Job Dissatisfaction: A Multi-Group Analysis of High and Low Cynicism. Sustainability 2022, 14, 4458. [Google Scholar] [CrossRef]
- Yadollahi, M.; Razmjooei, A.; Jamali, K.; Niakan, M.H.; Ghahramani, Z. The Relationship Between Professional Quality of Life (ProQol) and General Health in Rajaee Trauma Hospital Staff of Shiraz, Iran. Shiraz E-Med. J. 2016, 17, e39253. [Google Scholar] [CrossRef]
- Tan, B.Y.Q.; Chew, N.W.S.; Lee, G.K.H.; Jing, M.; Goh, Y.; Yeo, L.L.L.; Ka, Z.; Chin, H.; Ahmas, A.; Khan, F.; et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann. Intern. Med. 2020, 173, 317–320. [Google Scholar] [CrossRef] [PubMed]
- Hu, D.; Kong, Y.; Li, W.; Han, Q.; Zhang, X.; Zhu, L.; Wan, S.W.; Liu, Z.; Shen, Q.; Yang, J.; et al. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: A large-scale cross-sectional study. E Clin. Med. 2020, 24, 100424. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef]
- Wang, Y.X.; Guo, H.T.; Du, X.W.; Song, W.; Lu, C.; Hao, W.N. Factors associated with post-traumatic stress disorder of nurses exposed to corona virus disease 2019 in China. Medicine 2020, 99, e20965. [Google Scholar] [CrossRef] [PubMed]
- Ozen, S.; Sir, A. Frequency of PTSD in a group of search and rescue workers two months after 2003 Bingol (Turkey) earthquake. J. Nerv. Ment. Des. 2004, 192, 573–575. [Google Scholar] [CrossRef]
- Fjeldheim, C.B.; Nöthling, J.; Pretorius, K.; Basson, M.; Ganasen, K.; Heneke, R.; Cloete, K.J.; Seedat, S. Trauma exposure, posttraumatic stress disorder and the effect of explanatory variables in paramedic trainees. BMC Emerg. Med. 2014, 14, 11. [Google Scholar] [CrossRef]
- Xu, Y.; Zhang, K.R.; Xue, Y.Z. Study on the post-traumatic stress response of medical staff in the first line of SARS. Chin. Nursing Res. 2004, 18, 179–181. [Google Scholar]
- Chan, A.O.; Huak, C.Y. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup. Med. 2004, 54, 190–196. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Bradley, K.A.; Wipf, J.E.; Back, A.L. Burnout and self-reported patient care in an internal medicine residency program. Ann. Intern. Med. 2002, 136, 358–367. [Google Scholar] [CrossRef] [PubMed]
- Marôco, J.; Maroco, A.L.; Leite, E.; Bastos, C.; Vazão, M.J.; Campos, J. Burnout em profissionais da saúde portugueses: Uma análise a nível nacional. Acta Med. Port. 2016, 29, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Schaufeli, W.B.; Leiter, M.P. Job burnout. Annu. Rev. Psychol. 2001, 52, 397–422. [Google Scholar] [CrossRef] [PubMed]
- Rossi, R.; Socci, V.; Pacitti, F.; Di Lorenzo, G.; Di Marco, A.; Siracusano, A.; Rossi, A. Mental Health Outcomes among Frontline and Second-Line Health Care Workers during the Coronavirus Disease 2019 (COVID-19) Pandemic in Italy. JAMA Netw. Open 2020, 3, e2010185. [Google Scholar] [CrossRef] [PubMed]
- Kang, L.; Ma, S.; Chen, M.; Yang, J.; Wang, Y.; Li, R.; Yao, L.; Bai, H.; Cai, Z.; Xiang Yang, B.; et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav. Immun. 2020, 87, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Lu, W.; Wang, H.; Lin, Y.; Li, L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020, 288, 112936. [Google Scholar] [CrossRef] [PubMed]
- Dosil, M.; Ozamiz-Etxebarria, N.; Redondo, I.; Picaza, M.; Jaureguizar, J. Psychological Symptoms in Health Professionals in Spain After the First Wave of the COVID-19 Pandemic. Front. Psychol. 2020, 11, 606121. [Google Scholar] [CrossRef]
- Wee, D.; Myers, D. Compassion satisfaction, compassion fatigue, and critical incident stress management. Int. J. Emerg. Ment. Health 2003, 5, 33–37. [Google Scholar]
- Martínez-López, J.Á.; Lázaro-Pérez, C.; Gómez-Galán, J.; Fernández-Martínez, M.D.M. Psychological Impact of COVID-19 Emergency on Health Professionals: Burnout Incidence at the Most Critical Period in Spain. J. Clin. Med. 2020, 9, 3029. [Google Scholar] [CrossRef]
- Zhizhong, W.; Koenig, H.G.; Yan, T.; Jing, W.; Mu, S.; Hongyu, L.; Guangtian, L. Psychometric Properties of the Moral Injury Symptom Scale among Chinese Health Professionals during the COVID-19 Pandemic. BMC Psychiatry 2020, 20, 556. [Google Scholar] [CrossRef]
- Lange, M.; Joo, S.; Couette, P.-A.; de Jaegher, S.; Joly, F.; Humbert, X. Impact on Mental Health of the COVID-19 Outbreak among Community Pharmacists during the Sanitary Lockdown Period. Ann. Pharm. Fr. 2020, 78, 459–463. [Google Scholar] [CrossRef] [PubMed]
- Soto-Rubio, A.; Giménez-Espert, M.D.C.; Prado-Gascó, V. Effect of Emotional Intelligence and Psychosocial Risks on Burnout, Job Satisfaction, and Nurses’ Health during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 7998. [Google Scholar] [CrossRef] [PubMed]
- Jose, S.; Dhandapani, M.; Cyriac, M.C. Burnout and Resilience among Frontline Nurses during COVID-19 Pandemic: A Cross-Sectional Study in the Emergency Department of a Tertiary Care Center, North India. Indian J. Crit. Care Med. 2020, 24, 1081–1088. [Google Scholar] [CrossRef] [PubMed]
- Aebischer, O.; Weilenmann, S.; Gachoud, D.; Méan, M.; Spiller, T.R. Physical and Psychological Health of Medical Students Involved in the Coronavirus Disease 2019 Response in Switzerland. Swiss. Med. Wkly. 2020, 150, w20418. [Google Scholar] [CrossRef] [PubMed]
- Dimitriu, M.C.T.; Pantea-Stoian, A.; Smaranda, A.C.; Nica, A.A.; Carap, A.C.; Constantin, V.D.; Davitoiu, A.M.; Cirstoveanu, C.; Bacalbasa, N.; Bratu, O.G.; et al. Burnout Syndrome in Romanian Medical Residents in Time of the COVID-19 Pandemic. Med. Hypotheses 2020, 144, 109972. [Google Scholar] [CrossRef]
- American Psychological Association Building Your Resilience. Available online: https://www.apa.org/topics/resilience (accessed on 27 May 2022).
- Gao, T.; Ding, X.; Chai, J.; Zhang, Z.; Zhang, H.; Kong, Y.; Mei, S. The influence of resilience on mental health: The role of general well-being. Int. J. Nurs. Pract. 2017, 23, e12535. [Google Scholar] [CrossRef]
- Keeton, K.; Fenner, D.E.; Johnson, T.R.; Hayward, R.A. Predictors of physician career satisfaction, work-life balance, and burnout. Obstet. Gynecol. 2007, 109, 949–955. [Google Scholar] [CrossRef]
- Dunn, L.B.; Iglewicz, A.; Moutier, C. A conceptual model of medical student well-being: Promoting resilience and preventing burnout. Acad. Psychiatry 2008, 32, 44–53. [Google Scholar] [CrossRef]
- West, C.P.; Dyrbye, L.N.; Sinsky, C.; Trockel, M.; Tutty, M.; Nedelec, L.; Carlasare, L.E.; Shanafelt, T.D. Resilience and Burnout Among Physicians and the General US Working Population. JAMA Netw. Open 2020, 3, e209385. [Google Scholar] [CrossRef]
- Lluch, C.; Galiana, L.; Doménech, P.; Sansó, N. The Impact of the COVID-19 Pandemic on Burnout, Compassion Fatigue, and Compassion Satisfaction in Healthcare Personnel: A Systematic Review of the Literature Published during the First Year of the Pandemic. Healthcare 2022, 10, 364. [Google Scholar] [CrossRef]
- Platania, S.; Caponnetto, P.; Morando, M.; Maglia, M.; Auditore, R.; Santisi, G. Cross-Cultural Adaptation, Psychometric Properties and Measurement Invariance of the Italian Version of the Job Satisfaction Scale. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 1073–1087. [Google Scholar] [CrossRef]
- Caponnetto, P.; Platania, S.; Maglia, M.; Morando, M.; Gruttadauria, S.V.; Auditore, R.; Ledda, C.; Rapisarda, V.; Santisi, G. Health Occupation and Job Satisfaction: The Impact of Psychological Capital in the Management of Clinical Psychological Stressors of Healthcare Workers in the COVID-19 Era. Int. J. Environ. Res. Public Health 2022, 19, 6134. [Google Scholar] [CrossRef] [PubMed]
- Isralowitz, R.; Konstantinov, V.; Gritsenko, V.; Vorobeva, E.; Reznik, A. First and Second Wave COVID-19 Impact on Russian Medical Student Fear, Mental Health and Substance Use. J. Loss Trauma. 2021, 26, 94–96. [Google Scholar] [CrossRef]
- Kotera, Y.; Ozaki, A.; Miyatake, H.; Tsunetoshi, C.; Nishikawa, Y.; Tanimoto, T. Mental health of medical workers in Japan during COVID-19: Relationships with loneliness, hope and self-compassion. Curr. Psychol. 2021, 40, 6271–6274. [Google Scholar] [CrossRef] [PubMed]
- Platania, S.; Morando, M.; Caruso, A.; Scuderi, V. The effect of psychosocial safety climate on engagement and psychological distress: A multilevel study on health care sector. Safety 2022, 28, 691–708. [Google Scholar]
| M | SD | α | AVE | CR | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Secondary traumatic stress | 17.1 | 5.2 | 0.92 | 0.70 | 0.88 | 1 | |||||
| 2. Burnout | 25.7 | 4.9 | 0.89 | 0.64 | 0.82 | 0.49 ** | 1 | ||||
| 3. Resilience | 25.1 | 4.6 | 0.79 | 0.66 | 0.87 | −0.22 ** | −0.61 ** | 1 | |||
| 4. Depression | 4.3 | 1.3 | 0.82 | 0.60 | 0.81 | 0.41 ** | 0.21 ** | −0.14 ** | 1 | ||
| 5. Anxiety | 3.8 | 1.2 | 0.71 | 0.72 | 0.91 | 0.45 ** | 0.14 * | −0.18 ** | 0.29 ** | 1 | |
| 6. Compassion satisfaction | 29.5 | 8.7 | 0.78 | 0.65 | 0.85 | −0.35 ** | −0.20 ** | 0.25 ** | −0.22 ** | −0.13 * | 1 |
| 7. Stress | 8.2 | 2.3 | 0.85 | 0.63 | 0.82 | 0.59 ** | 0.28 ** | −0.34 ** | 0.32 ** | 0.36 ** | −0.37 ** |
| Predictor | Mediator | Outcome | β | SE | BC 95% CI | |
|---|---|---|---|---|---|---|
| LL | UL | |||||
| Depression → | Dispositional Resilience → | Compassion satisfaction | 0.04 ** | 0.03 | 0.158 | 0.414 |
| Depression → | Dispositional Resilience → | Secondary traumatic stress | 0.06 *** | 0.03 | 0.162 | 0.718 |
| Depression → | Dispositional Resilience → | Burnout | 0.04 ** | 0.02 | 0.265 | 0.476 |
| Anxiety → | Dispositional Resilience → | Secondary traumatic stress | 0.07 *** | 0.05 | 0.043 | 0.189 |
| Anxiety → | Dispositional Resilience → | Burnout | 0.05 ** | 0.03 | 0.056 | 0.041 |
| Stress → | Dispositional Resilience → | Compassion satisfaction | 0.07 *** | 0.05 | 0.125 | 0.369 |
| Stress→ | Dispositional Resilience → | Secondary traumatic stress | 0.06 ** | 0.04 | 0.168 | 0.412 |
| Stress → | Dispositional Resilience → | Burnout | 0.06 *** | 0.04 | 0.197 | 0.368 |
| Measurement Model | χ2 | df | ∆χ2 | ∆df | NFI | CFI | RMSEA |
|---|---|---|---|---|---|---|---|
| Multigroup model for the total sample | 125.84 | 107 | - | 0.90 | 0.96 | 0.051 | |
| Unconstrained model | 134.91 | 116 | 9.07 | 9 | 0.90 | 0.96 | 0.049 |
| Measurement model | 145.91 | 128 | 20.07 | 21 | 0.89 | 0.95 | 0.049 |
| Structural model | 166.15 | 135 * | 40.31 *** | 28 | 0.88 | 94 | 0.052 |
| Structural Model | χ2 | df | ∆χ2 | ∆df |
|---|---|---|---|---|
| Model 1: Baseline model | 149.01 | 130 | - | - |
| Model 2: Factor loadings and all path coefficients invariant | 165.32 | 135 | 16.31 ** | 5 |
| Model 3: Path coefficient DE→ DR unconstrained | 158.31 | 134 | 7.01 ** | 1 |
| Model 4: Path coefficient DE→ CS unconstrained | 160.25 | 134 | 1.94 | 1 |
| Model 5: Path coefficient DE→ STS unconstrained | 162.11 | 134 | 1.86 | 1 |
| Model 6: Path coefficient DE→ BO unconstrained | 157.54 | 134 | 4.57 * | 1 |
| Model 7: Path coefficient ANX→ DR unconstrained | 163.24 | 134 | 5.7 ** | 1 |
| Model 8: Path coefficient ANX→ CS unconstrained | 158.25 | 134 | 4.99 * | 1 |
| Model 9: Path coefficient ANX→ STS unconstrained | 162.78 | 134 | 4.53 * | 1 |
| Model 10: Path coefficient Stress → DR unconstrained | 165.84 | 134 | 3.06 * | 1 |
| Model 11: Path coefficient Stress → CS unconstrained | 163.14 | 134 | 2.7 | 1 |
| Model 12: Path coefficient Stress → STS unconstrained | 165.25 | 134 | 2.11 | 1 |
| Model 13: Path coefficient Stress → BO unconstrained | 162.36 | 134 | 2.89 | 1 |
| Model 11: Path coefficient DR → CS unconstrained | 165.84 | 134 | 3.48 * | 1 |
| Model 11: Path coefficient DR→ STS unconstrained | 160.25 | 134 | 5.59 ** | 1 |
| Model 11: Path coefficient DR→ BO unconstrained | 155.89 | 134 | 4.36 * | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Platania, S.; Gruttadauria, S.V.; Morando, M. Dispositional Resilience as Mediator in Psychological Stress on Healthcare Workers: A Multi-Group Analysis of Frontline and Non-Frontline Workers. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 1285-1299. https://doi.org/10.3390/ejihpe12090089
Platania S, Gruttadauria SV, Morando M. Dispositional Resilience as Mediator in Psychological Stress on Healthcare Workers: A Multi-Group Analysis of Frontline and Non-Frontline Workers. European Journal of Investigation in Health, Psychology and Education. 2022; 12(9):1285-1299. https://doi.org/10.3390/ejihpe12090089
Chicago/Turabian StylePlatania, Silvia, Stefania Valeria Gruttadauria, and Martina Morando. 2022. "Dispositional Resilience as Mediator in Psychological Stress on Healthcare Workers: A Multi-Group Analysis of Frontline and Non-Frontline Workers" European Journal of Investigation in Health, Psychology and Education 12, no. 9: 1285-1299. https://doi.org/10.3390/ejihpe12090089
APA StylePlatania, S., Gruttadauria, S. V., & Morando, M. (2022). Dispositional Resilience as Mediator in Psychological Stress on Healthcare Workers: A Multi-Group Analysis of Frontline and Non-Frontline Workers. European Journal of Investigation in Health, Psychology and Education, 12(9), 1285-1299. https://doi.org/10.3390/ejihpe12090089










