A Mobile-Based Tailored Recommendation System for Parents of Children with Overweight or Obesity: A New Tool for Health Care Centers
Abstract
1. Introduction
2. Materials and Methods
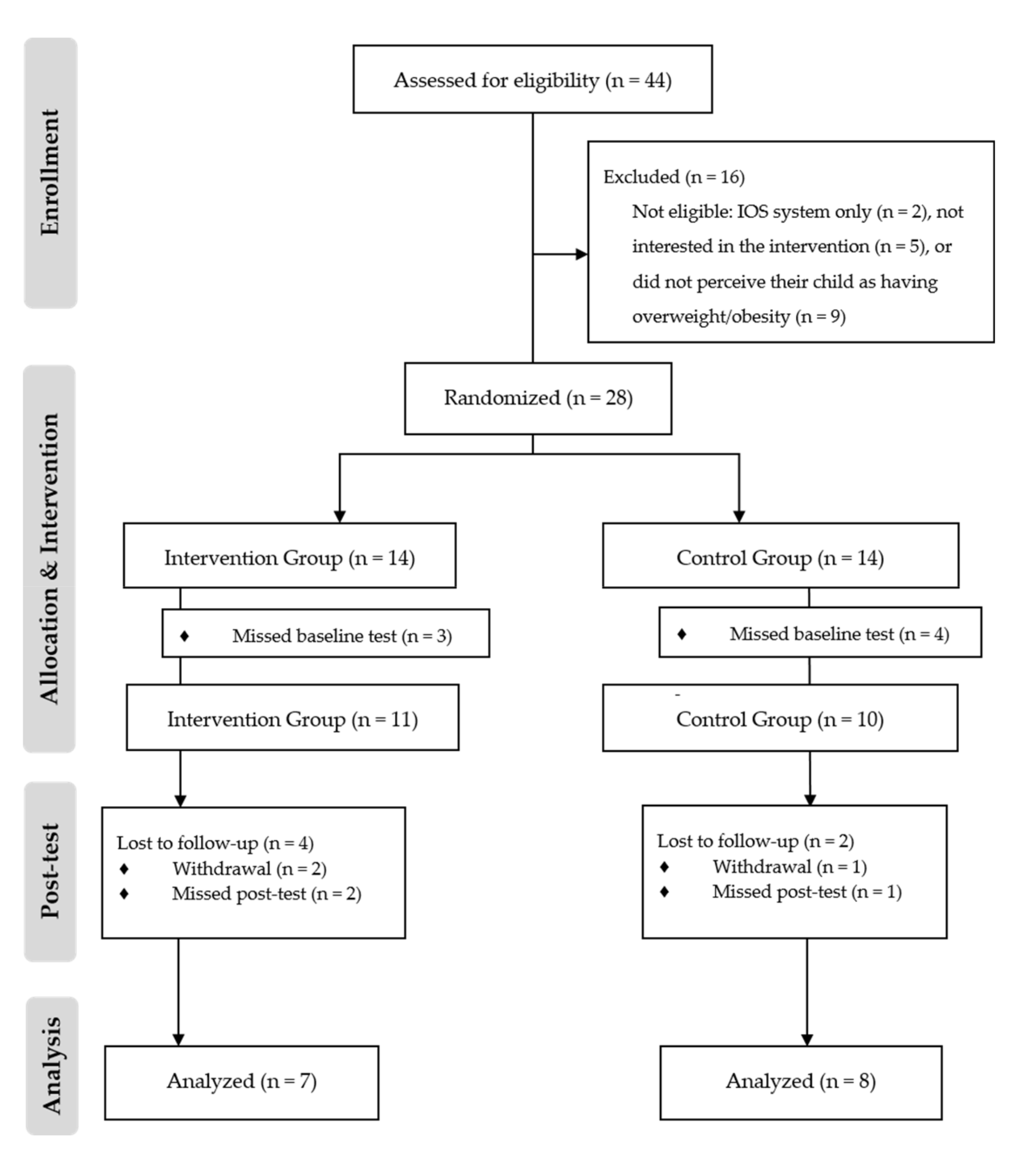
2.1. Study Design
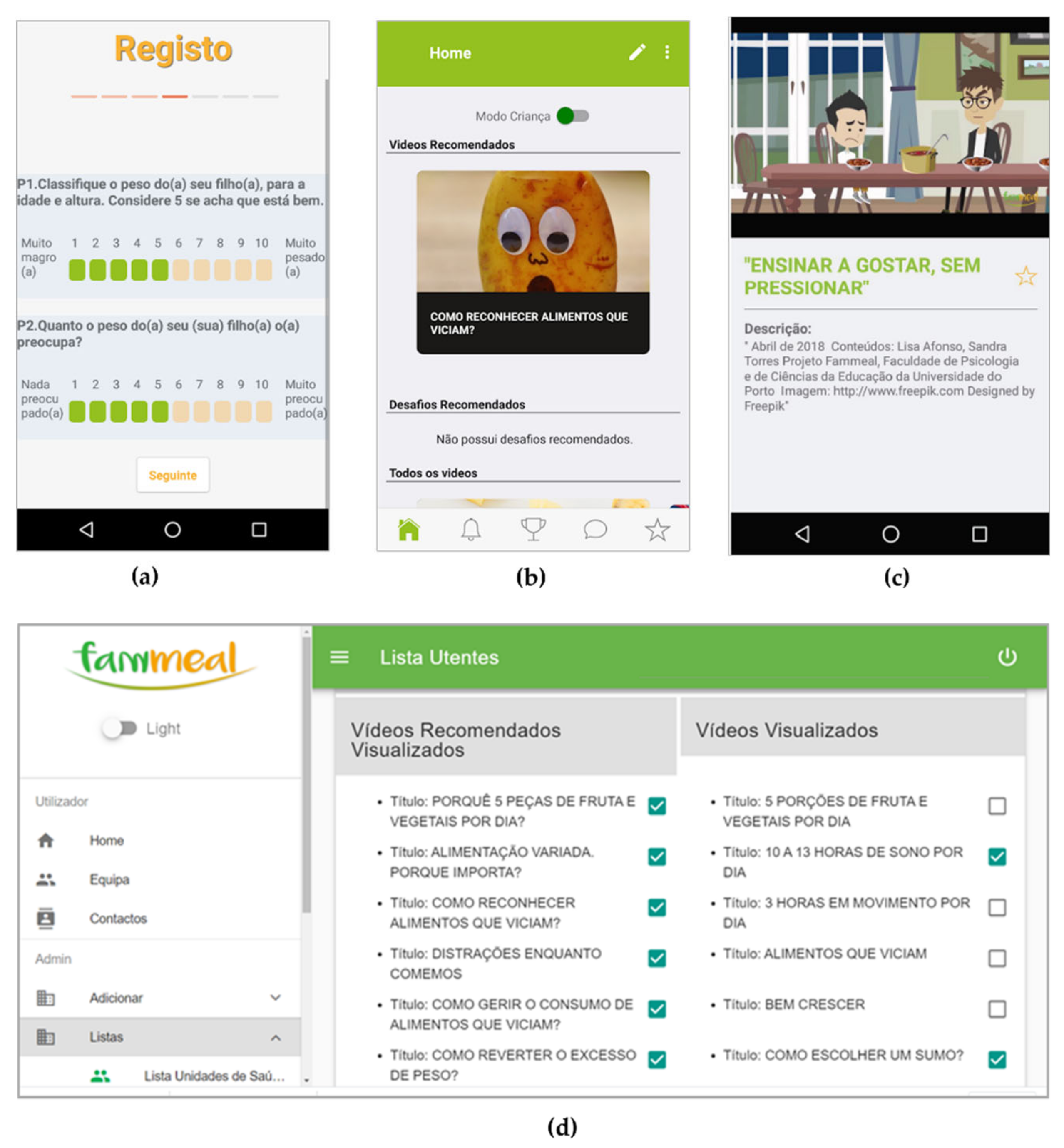
2.2. Recommendation System Development
2.2.1. Defining Recommendations for Parents
- Attitudes, i.e., one’s evaluation of performing an action, highly determined by beliefs related to the behavior;
- Subjective norms, i.e., one’s belief about social expectations; and
- Perceived behavioral control, i.e., one’s perception of the degree of ease and difficulty of the behavior.
- Parents’ perceptions about the children’s weight status and knowledge about the guidelines for their age as determinants of their behavioral beliefs and, consequently, of their attitudes toward the behavior;
- The importance attributed to their children’s weight status and the guidelines for their age, reflecting their attitudes; and
- Practical strategies to improve those outcomes and to improve perceived behavioral control.
2.2.2. Defining the Tailored Recommendation System
2.2.3. Development of the App
2.3. Testing of the Recommendation System
2.3.1. Participants
- Were parents of children with overweight/obesity for their age (according to the World Health Organization criteria [30]);
- Had access to an Android device with an Internet connection;
- Were interested in participating in two interviews in the health care center; and
- Were willing to install the app and use it for four weeks.
2.3.2. Study 1—Test of the Adequacy of the Recommendation System
2.3.3. Study 2—Pilot Study
2.4. Statistical Analysis
3. Results
3.1. Participants
3.2. Study 1—Testing the Adequacy of the Recommendation System
- Regarding weight status, of the three parents who perceived their child’s excessive weight, one (33.3%) was not concerned about it.
- Considering only parents who knew the guidelines, 55.8% of parents (n = 19) reported that their children ate more energy-dense foods, 25.7% (n = 9) that their children drank more sugar-sweetened beverages, and 13.3% (n = 4) that their children moved less than recommended.
- From those parents that knew the guidelines for fruit and vegetable intake (n = 22), 63.6% (n = 14) reported that their children ate less than recommended.
- Regarding water intake, considering only parents who knew the guidelines (n = 5), 60% of the children (n = 3) failed to meet them.
3.3. Study 2—Pilot Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Taking Action on Childhood Obesity; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Ip, E.H.; Marshall, S.A.; Saldana, S.; Skelton, J.A.; Suerken, C.K.; Arcury, T.A.; Quandt, S.A. Determinants of Adiposity Rebound Timing in Children. J. Pediatr. 2017, 184, 151–156. [Google Scholar] [CrossRef]
- O’Brien, A. Web-Based Weight Management Programs for Children and Adolescents: A Systematic Review of Randomized Controlled Trial Studies. ANS Adv. Nurs. Sci. 2010, 33, 2. [Google Scholar] [CrossRef] [PubMed]
- Styne, D.M.; Arslanian, S.A.; Connor, E.L.; Farooqi, I.S.; Murad, M.H.; Silverstein, J.H.; Yanovski, J.A. Pediatric Obesity-Assessment, Treatment, and Prevention: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2017, 102, 709–757. [Google Scholar] [CrossRef]
- World Health Organization and Food and Agriculture Organization. Fruit and Vegetables for Health; Report of a Joint FAO/WHO Workshop (Kobe, Japan, 1–3 September 2004); World Health Organization and Food and Agriculture Organization: Rome, Italy, 2004. [Google Scholar]
- Popkin, B.; D’Anci, K.E.; Rosenberg, I.H. Water, Hydration, and Health. Nutr. Rev. 2010, 68, 439–458. [Google Scholar] [CrossRef] [PubMed]
- Department of Health and Human Services. Physical Activity Guidelines Advisory Committee Scientific Report; Department of Health and Human Services: Washington, DC, USA, 2018.
- Paruthi, S.; Brooks, L.J.; D’Ambrosio, C.; Hall, W.A.; Kotagal, S.; Lloyd, R.M.; Malow, B.A.; Maski, K.; Nichols, C.; Quan, S.F.; et al. Recommended Amount of Sleep for Pediatric Populations: A Consensus Statement of the American Academy of Sleep Medicine. J. Clin. Sleep Med. 2016, 12, 785–786. [Google Scholar] [CrossRef] [PubMed]
- Sargent, G.M.; Pilotto, L.S.; Baur, L.A. Components of Primary Care Interventions to Treat Childhood Overweight and Obesity: A Systematic Review of Effect. Obes. Rev. 2010, 12, e219–e235. [Google Scholar] [CrossRef] [PubMed]
- Sastre, L.R.; Matson, S.; Gruber, K.J.; Haldeman, L. A Qualitative Study Examining Medical Provider Advice, Barriers, and Perceived Effectiveness in Addressing Childhood Obesity to Patients and Families from a Low-Income Community Health Clinic. SAGE Open Med. 2019, 7, 1–9. [Google Scholar] [CrossRef]
- van Gerwen, M.; Franc, C.; Rosman, S.; le Vaillant, M.; Pelletier-Fleury, N. Primary Care Physicians’ Knowledge, Attitudes, Beliefs and Practices Regarding Childhood Obesity: A Systematic Review. Obes. Rev. 2009, 10, 227–236. [Google Scholar] [CrossRef]
- Turner, N.; Shield, J.; Salisbury, C. Practitioners’ Views on Managing Childhood Obesity in Primary Care: A Qualitative Study. Br. J. Gen. Pr. 2009, 59, 856–862. [Google Scholar] [CrossRef][Green Version]
- Galuska, D.A.; Fulton, J.E.; Powell, K.E.; Burgeson, C.R.; Pratt, M.; Elster, A.; Griesemer, B.A. Pediatrician Counseling about Preventive Health Topics: Results from the Physicians’ Practices Survey, 1998–1999. Pediatrics 2002, 109, e83. [Google Scholar] [CrossRef]
- Bradbury, D.; Chisholm, A.; Watson, P.M.; Bundy, C.; Bradbury, N.; Birtwistle, S. Barriers and Facilitators to Health Care Professionals Discussing Child Weight With Parents: A Meta-Synthesis of Qualitative Studies. Br. J. Heal. Psychol. 2018, 23, 701–722. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.; Chater, A.; Lorencatto, F. Effective Behaviour Change Techniques in the Prevention and Management of Childhood Obesity. Int. J. Obes. 2013, 37, 1287–1294. [Google Scholar] [CrossRef] [PubMed]
- Webb, T.L.; Joseph, J.; Yardley, L.; Michie, S.; Kraft, P.; Botelho, R. Using the Internet to Promote Health Behavior Change: A Systematic Review and Meta-analysis of the Impact of Theoretical Basis, Use of Behavior Change Techniques, and Mode of Delivery on Efficacy. J. Med. Int. Res. 2010, 12, e4. [Google Scholar] [CrossRef] [PubMed]
- Godin, G.; Kok, G. The Theory of Planned Behavior: A Review of Its Applications to Health-Related Behaviors. Am. J. Heal. Promot. 1996, 11, 87–98. [Google Scholar] [CrossRef]
- Riebl, S.K.; Estabrooks, P.A.; Dunsmore, J.C.; Savla, J.; Frisard, M.I.; Dietrich, A.M.; Peng, Y.; Zhang, X.; Davy, B. A Systematic Literature Review and Meta-Analysis: The Theory of Planned Behavior’s Application to Understand and Predict Nutrition-Related Behaviors in Youth. Eat. Behav. 2015, 18, 160–178. [Google Scholar] [CrossRef]
- Afonso, L.; Lopes, C.; Severo, M.; Santos, S.; Real, H.; Durão, C.; Moreira, P.; Oliveira, A. Bidirectional Association between Parental Child-Feeding Practices and Body Mass Index at 4 and 7 y of Age. Am. J. Clin. Nutr. 2016, 103, 861–867. [Google Scholar] [CrossRef]
- Jansen, P.W.; Tharner, A.; van der Ende, J.; Wake, M.; Raat, H.; Hofman, A.; Verhulst, F.C.; van Ijzendoorn, M.H.; Jaddoe, V.W.; Tiemeier, H. Feeding Practices and Child Weight: Is the Association Bidirectional in Preschool Children? Am. J. Clin. Nutr. 2014, 100, 1329–1336. [Google Scholar] [CrossRef]
- Vaughn, A.E.; Ward, D.S.; Fisher, J.O.; Faith, M.S.; Hughes, S.O.; Kremers, S.P.; Musher-Eizenman, D.R.; O’Connor, T.M.; Patrick, H.; Power, T.G. Fundamental Constructs in Food Parenting Practices: A Content Map to Guide Future Research. Nutr. Rev. 2016, 74, 98–117. [Google Scholar] [CrossRef]
- Vaughn, A.E.; Dearth-Wesley, T.; Tabak, R.G.; Bryant, M.; Ward, D. Development of a Comprehensive Assessment of Food Parenting Practices: The Home Self-Administered Tool for Environmental Assessment of Activity and Diet Family Food Practices Survey. J. Acad. Nutr. Diet. 2016, 117, 214–227. [Google Scholar] [CrossRef]
- Broekhuizen, K.; Kroeze, W.; van Poppel, M.N.M.; Oenema, A.; Brug, J. A Systematic Review of Randomized Controlled Trials on the Effectiveness of Computer-Tailored Physical Activity and Dietary Behavior Promotion Programs: An Update. Ann. Behav. Med. 2012, 44, 259–286. [Google Scholar] [CrossRef]
- Cheung, K.L.; Durusu, D.; Sui, X.; de Vries, H. How Recommender Systems Could Support and Enhance Computer-Tailored Digital Health Programs: A Scoping Review. Digit. Heal. 2019, 5, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Moore, C.G.; Carter, R.E.; Nietert, P.J.; Stewart, P.W. Recommendations for Planning Pilot Studies in Clinical and Translational Research. Clin. Transl. Sci. 2011, 4, 332–337. [Google Scholar] [CrossRef] [PubMed]
- Júlíusson, P.B.; Roelants, M.; Markestad, T.; Bjerknes, R. Parental Perception of Overweight and Underweight in Children and Adolescents. Acta Paediatr. 2010, 100, 260–265. [Google Scholar] [CrossRef] [PubMed]
- University of Porto. Fammeal Project Website. Available online: https://fammeal.up.pt (accessed on 11 June 2020).
- Bornstein, M.H.; Putnick, D.L.; Lansford, J.E.; Pastorelli, C.; Skinner, A.T.; Sorbring, E.; Tapanya, S.; Tirado, L.M.U.; Zelli, A.; Alampay, L.P.; et al. Mother and Father Socially Desirable Responding in Nine Countries: Two Kinds of Agreement and Relations to Parenting Self-Reports. Int. J. Psychol. 2014, 50, 174–185. [Google Scholar] [CrossRef] [PubMed]
- ClinicalTrials.gov. The System Fammeal With Tailored Recommendations and Gamification for Parents to Counteract Childhood Obesity (Fammeal). ClinicalTrials.gov Identifier: NCT03881280. Available online: https://clinicaltrials.gov/ct2/show/NCT03881280 (accessed on 19 March 2019).
- WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/Height-For-Age, Weight-For-Age, Weight-For-Length, Weight-For-Height and Body Mass Index-For-Age: Methods and Development; WHO Multicentre Growth Reference Study Group: Geneva, Switzerland, 2006. [Google Scholar]
- World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [CrossRef]
- Vilela, S.; Severo, M.; Moreira, T.; Ramos, E.; Lopes, C. Evaluation of a short Food Frequency Questionnaire for Dietary Intake Assessment Among Children. Eur. J. Clin. Nutr. 2018, 73, 679–691. [Google Scholar] [CrossRef] [PubMed]
- IBM Corp. IBM SPSS Statistics for Windows, Version 24.0.; IBM Corp: Armonk, NY, USA, 2016. [Google Scholar]
- Choen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Academic Press: New York, NY, USA, 1988. [Google Scholar]
- Babela, J.R.M.; Nika, E.R.; Milandou, K.G.C.N.; Mandilou, S.V.M.; Bazolana, S.B.A.B.; Monabeka, H.G.; Moyen, G. Knowledge, Attitudes, and Practices of Parents Facing Child and Adolescent Obesity in Brazzaville, Congo. Glob. Pediatr. Heal. 2016, 3, 1–8. [Google Scholar] [CrossRef]
- Nepper, M.J.; Chai, W. Parents’ Barriers and Strategies to Promote Healthy Eating among School-Age Children. Appetite 2016, 103, 157–164. [Google Scholar] [CrossRef]
- Lundahl, A.; Kidwell, K.M.; Nelson, T.D. Parental Underestimates of Child Weight: A Meta-analysis. Pediatrics 2014, 133, 689–703. [Google Scholar] [CrossRef]
- Rietmeijer-Mentink, M.; Paulis, W.; van Middelkoop, M.; Bindels, P.J.; van der Wouden, J.C. Difference between Parental Perception and Actual Weight Status of Children: A Systematic Review. Matern. Child Nutr. 2012, 9, 3–22. [Google Scholar] [CrossRef]
- Borrelli, B.; Tooley, E.M.; Scott-Sheldon, L.A.J. Motivational Interviewing for Parent-child Health Interventions: A Systematic Review and Meta-Analysis. Pediatr. Dent. 2015, 37, 254–265. [Google Scholar] [PubMed]
- Hammersley, M.L.; Jones, R.; Okely, A.D.; Korkalo, L.; Amini, M. Parent-Focused Childhood and Adolescent Overweight and Obesity eHealth Interventions: A Systematic Review and Meta-Analysis. J. Med. Int. Res. 2016, 18, e203. [Google Scholar] [CrossRef] [PubMed]
- Robinson, E. Overweight but Unseen: A Review of the Underestimation of Weight Status and A Visual Normalization Theory. Obes. Rev. 2017, 18, 1200–1209. [Google Scholar] [CrossRef] [PubMed]
- Hudson, E.; McGloin, A.; McConnon, Á. Parental Weight (Mis)Perceptions: Factors Influencing Parents’ Ability to Correctly Categorise Their Child’s Weight Status. Matern. Child Heal. J. 2011, 16, 1801–1809. [Google Scholar] [CrossRef]
- Palad, C.J.; Yarlagadda, S.; Stanford, F.C. Weight Stigma and Its Impact on Paediatric Care. Curr. Opin. Endocrinol. Diabetes Obes. 2019, 26, 19–24. [Google Scholar] [CrossRef]
- Burrows, T.; Hutchesson, M.J.; Chai, L.K.; Rollo, M.; Skinner, G.; Collins, C.E. Nutrition Interventions for Prevention and Management of Childhood Obesity: What Do Parents Want from an eHealth Program? Nutrients 2015, 7, 10469–10479. [Google Scholar] [CrossRef]
| Behavioral Beliefs1 | Attitudes toward the Behavior | Perceived Behavioral Control | |
|---|---|---|---|
| Weight Status | Parents are aware of their children’s excessive weight. | Parents are concerned about their children’s excessive weight. | Parents feel confident about improving their children’s excessive weight. |
| Food and Beverage Intake | Parents know that their children consume less fruit and vegetables, more energy-dense foods, more sugar-sweetened beverages, and less water than recommended. | Parents believe it is important that their children eat and drink as recommended. | Parents feel confident about improving their children’s intake. |
| Physical Activity and Sleep | Parents are aware that their children move less and sleep less than recommended. | Parents recognize that it is important that children move enough. | Parents feel confident about improving their children’s sleeping time. |
| Questions | Cutoff | Recommended Content TPB | ||
|---|---|---|---|---|
| 1. Weight Status | (a) How do you classify the weight of your child for their age, sex, and height?1 | ≤5 | Behavioral Beliefs | |
| (b) How concerned are you about your child’s weight status?2 | ≤5 | Attitudes | ||
| 2. Food and Beverage Intake | (a) What are the guidelines for your child’s age?3 | Fruits (F) (portions per day) | F + V<5 | Behavioral Beliefs |
| Vegetables (V) (portions per day) | ||||
| Energy-dense foods (portions per week) | >3 | |||
| Water (glasses per day) | <8 | |||
| Sugar-sweetened beverages (glasses per week) | >3 | |||
| (b) What is the usual intake of your child?3 | Fruits (F) (portions per day) | F + V<5 | Attitudes and Perceived Behavioral Control | |
| Vegetables (V) (portions per day) | ||||
| Energy-dense foods (portions per week) | >3 | |||
| Water (glasses per day) | <8 | |||
| Sugar-sweetened beverages (glasses per week) | >3 | |||
| 3. Physical Activity and Sleep | (a) What are the guidelines for your child’s age?4 | Moderate to intense PA (periods of 20 min of active play, speed walking, or any sport per day) | <3 | Behavioral Beliefs |
| Sleep (hours of nighttime sleep and napping per day) | <10 | |||
| (a) How long does your child usually spend on each of these activities?4 | Moderate to intense PA (periods of 20 min of active play, speed walking, or any sport per day) | <3 | Attitudes and Perceived Behavioral Control | |
| Sleep (hours of nighttime sleep and napping per day) | <10 | |||
| Theory of Planned Behavior | Food Parenting Practices Map | |||
|---|---|---|---|---|
| Behavioral Beliefs1 | Attitudes2 | Perceived Behavioral Control2 | ||
| Weight Status | Video 1Healthy Development | Video 2Consequences of having overweight | Video 3How to help a child return to a healthy weight3 | ↓ Weight Talk↑ Guided Choices↑ Modeling |
| Food and Beverage Intake | Video 45 portions of fruit and vegetables daily4 | Video 5Why 5 portions of fruit and vegetables a day?3 | Video 6 Teach them to like, without pressure | ↓ Pressure to Eat↑ Availability and Accessibility of Healthy Foods↑ Attractive Presentation of Foods↑ Nutrition Education↑ Modeling↑ Monitoring↑ Rules and Limits↓ Distractions↑ Availability and Accessibility |
| Video 7Eating variety: Why does it matter? | ||||
| Video 8 Addictive foods4 | Video 9 How to recognize addictive foods3 | Video 10 How to regulate the intake of addictive foods | ||
| Video 11 Distractions while eating | ||||
| Video 12Hydration4 | Video 13How to select a juice | |||
| Physical Activity and Sleep | Video 14Move4,5 | |||
| Video 15Sleep4,6 | ||||
| Study 1 (n = 35) | Study 2 | |||
|---|---|---|---|---|
| Intervention Group (n = 11) | Control Group (n = 10) | |||
| Parents/Caregivers | ||||
| Sex | Female, n (%) | 31 (88.6) | 7 (63.6) | 8 (80.0) |
| Male, n (%) | 4 (11.4) | 4(36.4) | 2 (20.0) | |
| Age (years), mean (SD) | 35.2 (4.6) | 36.9 (3.1) | 38.8 (3.7) | |
| With university degree, n (%) | 29 (82.8) | 8 (72.7) | 6 (60.0) | |
| Children | ||||
| Sex | Female, n (%) | 17 (48.6) | 2 (18.2) | 3 (30.0) |
| Male, n (%) | 18 (51.4) | 9 (81.8) | 7 (70.0) | |
| Age (years), mean (SD) | 4.4 (1.1) | 4.9 (1.1) | 5.2 (1.2) | |
| Weight status, n (%) | Underweight | 0 (0.0) | n.a. | n.a. |
| Normal weight | 25 (71.4) | n.a. | n.a. | |
| Overweight | 7 (20.0) | 6 (54.5) | 4 (40.0) | |
| Obesity | 3 (8.6) | 5 (45.5) | 6 (60.0) | |
| Questions | Cutoff | Parents Eligible to Receive Recommendationsn (%) | ||
|---|---|---|---|---|
| 1. Weight Status1 | (a) How do you classify the weight of your child for their age, sex, and height?2 | ≤5 | 7 (70.0) | |
| (b) How concerned are you about your child’s weight status?3 | ≤5 | 6 (60.0) | ||
| 2. Food and Beverage Intake | (a) What are the guidelines for your child’s age?4 | Fruits (F) (portions per day) | F + V<5 | 13 (37.1) |
| Vegetables (V) (portions per day) | ||||
| Energy-dense foods (portions per week) | >3 | 1 (2.9) | ||
| Water (glasses per day) | <8 | 30 (85.7) | ||
| Sugar-sweetened beverages (glasses per week) | >3 | 0 (0.0) | ||
| (b) What is the usual intake of your child?4 | Fruits (F) (portions per day) | F + V<5 | 20 (57.1) | |
| Vegetables (V) (portions per day) | ||||
| Energy-dense foods (portions per week) | >3 | 20 (57.1) | ||
| Water (glasses per day) | <8 | 32 (91.4) | ||
| Sugar-sweetened beverages (glasses per week) | >3 | 9 (25.7) | ||
| 3. Physical Activity and Sleep | (a) What are the guidelines for your child’s age?5 | Moderate to intense PA (periods of 20 min of active play, speed walking, or any sport per day) | <3 | 5 (14.3) |
| Sleep (hours of nighttime sleep and napping per day) | <10 | 14 (40.0) | ||
| (a) How long does your child usually spend on each of these activities?5 | Moderate to intense PA (periods of 20 min of active play, speed walking, or any sport per day) | <3 | 9 (25.7) | |
| Sleep (hours of nighttime sleep and napping per day) | <10 | 16 (45.7) | ||
| Cutoff | Control (n = 8) Median (IQR) | Intervention (n = 7) Median (IQR) | Differences between Groups1 | |||||
|---|---|---|---|---|---|---|---|---|
| Post-Test | Dif. | Post-Test | Dif. | U | p-Value | r2 (effect size) | ||
| Perceptions about the child’s excessive weight2 | ≤5 | 5.5 (1.8) | 0.0 (2.0) | 6.0 (1.0) | 0.0 (1.0) | 28.0 | 0.976 | 0.00 |
| Fruits and vegetables (portions/day)3 | <5 | 5.0 (1.75) | 0.5 (3.0) | 5.0 (3.0) | 2.0 (3.0) | 19.0 | 0.336 | 0.08 |
| Water (glasses/day)3 | <8 | 5.0 (3.0) | 0.0 (2.0) | 8.0 (1.0) | 3.0 (2.0) | 0.0 | <0.001*** | 0.78 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Afonso, L.; Rodrigues, R.; Castro, J.; Parente, N.; Teixeira, C.; Fraga, A.; Torres, S. A Mobile-Based Tailored Recommendation System for Parents of Children with Overweight or Obesity: A New Tool for Health Care Centers. Eur. J. Investig. Health Psychol. Educ. 2020, 10, 779-794. https://doi.org/10.3390/ejihpe10030057
Afonso L, Rodrigues R, Castro J, Parente N, Teixeira C, Fraga A, Torres S. A Mobile-Based Tailored Recommendation System for Parents of Children with Overweight or Obesity: A New Tool for Health Care Centers. European Journal of Investigation in Health, Psychology and Education. 2020; 10(3):779-794. https://doi.org/10.3390/ejihpe10030057
Chicago/Turabian StyleAfonso, Lisa, Rui Rodrigues, Joana Castro, Nuno Parente, Carina Teixeira, Ana Fraga, and Sandra Torres. 2020. "A Mobile-Based Tailored Recommendation System for Parents of Children with Overweight or Obesity: A New Tool for Health Care Centers" European Journal of Investigation in Health, Psychology and Education 10, no. 3: 779-794. https://doi.org/10.3390/ejihpe10030057
APA StyleAfonso, L., Rodrigues, R., Castro, J., Parente, N., Teixeira, C., Fraga, A., & Torres, S. (2020). A Mobile-Based Tailored Recommendation System for Parents of Children with Overweight or Obesity: A New Tool for Health Care Centers. European Journal of Investigation in Health, Psychology and Education, 10(3), 779-794. https://doi.org/10.3390/ejihpe10030057






