1. Introduction
In 2022, there will be approximately 4,820,000 and 2,370,000 new cancer cases, and 3,210,000 and 640,000 cancer deaths, in China and the USA, respectively [
1].Cancer has become a leading cause of death in China with an increasing burden of cancer incidence and mortality observed over the past half century [
2].
Patients with advanced cancer often encounter considerable physical, psychological, and social pressures and the need to adapt to changes in physical, psychological, and social functions resulting from the disease [
3]. For example, a patient’s psychological stress increases with the diagnosis and course of cancer [
4]. Psychological stress can also affect disease development, such as tumor growth, progression, and metastasis [
5]. Psychological stress can suppress immune activity and worsen the disease, especially in chronic diseases such as cancer [
6]. In addition, the literature [
7] demonstrates that effective psychological interventions can improve human immune function. Therefore, how to preserve the psychosocial, spiritual, and existential integrity of people facing an incurable disease is considered one of the main challenges of palliative care [
8].
Palliative care aims to support terminally ill patients and their relatives on a physical, psychological, and spiritual level [
9]. It prevents and relieves suffering through the early identification, correct assessment, and treatment of pain and other problems, whether physical, psychosocial, or spiritual [
10]. However, psychological distress and mental worry are widespread in the end stages of life-threatening illnesses [
11,
12]. Therefore, it is essential to find an effective form of palliative therapy to relieve the psychological pressure and mental worry in the advanced stage of cancer. The most common approach is psychosocial therapy in palliative care, which is categorized into cognitive behavioral therapy (CBT) [
13], mindfulness-based interventions [
14], dignity therapy [
15,
16], life review [
17], meaning-centered interventions (MCIs) [
18], and creative arts-based therapy [
19].
Music in creative arts-based therapy effectively promotes the psycho-spiritual integration of meaning and life experiences in terminally ill patients [
20,
21]. The application of music therapy in multidisciplinary palliative care is in relatively early stages [
22,
23]. In the clinic, music therapy aims to improve quality of life by providing comfort, and promoting communication and spiritual experiences to relieve physical symptoms and psychological difficulties [
24]. Music therapy has a variety of technical categories such as receptive, creative, and entertaining [
25]. There is a clinical emphasis on the benefits of music therapy in end-of-life care [
4]. Most palliative care for music therapy focuses on pain and quality of life [
26], pain relief [
27,
28], physical comfort [
29,
30], psychophysiological health [
31], subjective well-being [
32], emotional distress [
33], and anxiety and mood [
34,
35].
Music therapy also plays a vital role in the treatment of some cancers. For example, it is an alternative therapy that cervical cancer patients can undergo to help reduce the feelings felt by the patient and provide emotional and spiritual support, thereby reducing fatigue caused by treatment [
36]. It offers breast cancer patients a valuable opportunity to reduce negative emotional states and improve their quality of life, and appears to be a promising nonpharmacological treatment option in breast cancer oncology [
37]. For breast or gynecologic malignancies, this therapy may reduce the effects of fatigue due to radiation therapy and effectively reduce symptoms of cancer-related fatigue and depression. It improves the quality of life of women undergoing radiation therapy with breast or gynecologic cancer [
38]. The therapy enhances nausea and vomiting symptoms in patients with gastrointestinal cancer during chemotherapy [
39]. It can be used as an adjuvant drug alongside other treatments to relieve patients’ symptoms [
40]. Music therapy reduces depression and salivary cortisol levels and improves the quality of life in AYA patients undergoing HSCT [
41]. Reference [
42] recommends that music therapy for patients with hematological cancers be considered an intervention that can be used in conjunction with other treatments to reduce fatigue.
However, there are few reports on music therapy’s effect on a patient’s overall state. The above studies on music therapy are all based on meta-analysis or statistical analysis, employed to investigate the working mechanism of music therapy and lay the foundations for developing new music intervention therapy. However, the findings are only provide the statistical validity of some indicators. According to the total experimental sample results, it has a certain validity. Music therapy is similar to other medical methods. Different music can only be applied to different groups of people. The wrong choice of music may make the patient’s symptoms worse. In addition, existing research methods do not reflect the sensitivity of different indicators to their treatment, which also varies from person to person. Moreover, the effect of the same music therapy on patients cannot be shown accurately. Thus, it is difficult for researchers to quickly know whether psychotherapy is effective or not, and it is not helpful to recommend psychotherapy that fits the symptoms of psychological disorders. Here, we use the multiple criteria decision making (MCDM) comprehensive evaluation method to further discuss the result of [
43,
44] by comprehensively evaluating the experimental results of the “Song of Life” (SOL) and quantitatively analyzing its impact based on the overall state of the patients. This method facilitates the selection of the best music therapy among many different types of music therapies.
MCDM methods have been used for diagnosing many cancer cases and the optimal selection of anticancer drugs and treatments. Fahmi et al. proposed the triangular cubic hesitant fuzzy TOPSIS method and defined a new type of cancer patient according to this method [
45]. Hatice et al. proposed an AHP-EMW-TOPSIS model to select the better treatment technique for HER2+ breast cancer from two different treatments and to screen the considered factors and their significance levels when choosing treatment. This model can be used to identify the most effective targeted drug combinations [
46]. A TOPSIS case-based reasoning approach was used to determine the optimal combination of radiotherapy doses for prostate cancer, which will help oncologists make better trade-offs between success and treatment side effects [
47,
48,
49].
The TOPSIS and VIKOR methods were used to choose the best surgical option between mastectomy (complete removal of the breast) and breast-conserving surgery (removal of for breast cancer tumor and some normal surgery). The model considered 19 sub-criteria related to tumor-related, patient-related, and postoperative course [
50]. The ordinal relationship analysis method and TOPSIS were combined to rank four drug regimens and determine the best drug regimen for patients with chronic cancer to avoid possible side effects from increased doses or potent drug use [
51]. When selecting anticancer drugs, applying the AHP-TOPSIS approach has dramatically improved clinical outcomes and reduced financial costs associated with chemotherapy treatment [
52,
53]. Li et al. proposed a novel selection model of surgical treatments for early gastric cancer based on heterogeneous multiple-criteria group decision making (MCGDM), which helps to select the most appropriate surgery in the case of asymmetric information between doctors and patients [
54]. In addition, an ordinary differential equation (ODE) can also be used to evaluate the therapeutic effect of cancer [
55,
56,
57,
58].
This paper will further expand the research of [
43,
44] to evaluate two palliative care methods by the EMW-TOPSIS method. To illustrate the effectiveness of SOL, we will calculate the patient’s overall state changes between pre- and post-intervention. In the
Section 2, we preprocess part of the data and use the collaborative filtering algorithm (CFA) approach to complete some missing data. In the
Section 3, we establish the entropy weight method and the TOPSIS model. Finally, we obtain the state changes before and after the application of data and the recognition of the two methods by patients and their families. It was found that SOL therapy has apparent advantages over traditional methods; however, we also found that not all patients are suitable for our two palliative treatments. The MCDM method provides a new approach to assessing the validity of psychological interventions. This method would be applied in predictive diagnostics and precision medicine by combining machine learning and deep learning methods in our future work.
5. Discussion
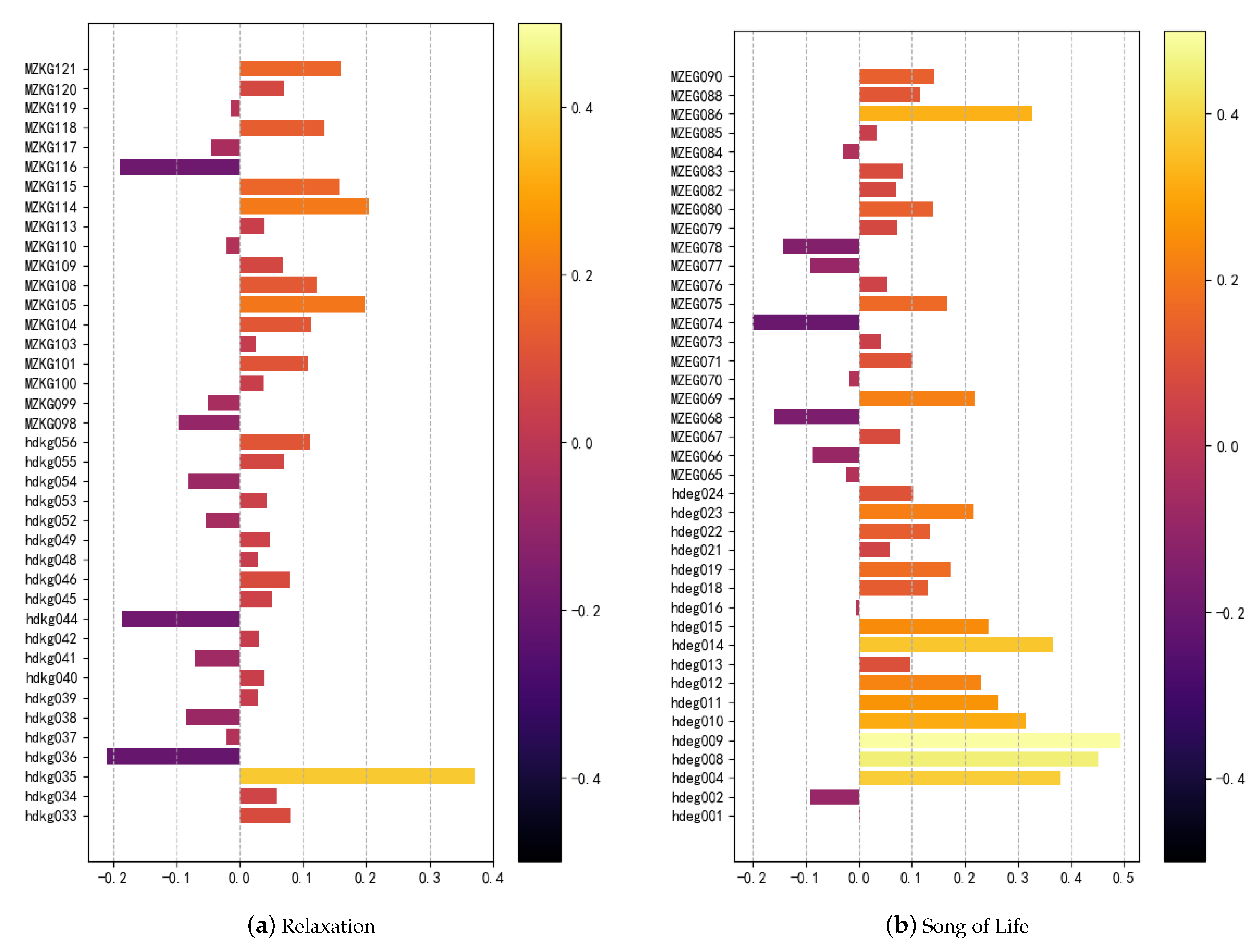
We used EWM-TOPSIS to evaluate the overall state of patients pre- and post-intervention. The results showed that the improvement of the individual’s overall state in the experimental group was better than that of the control group. The questionnaire feedback was used to assist in the accurate evaluation of the efficacy of SOL in changing a patient’s overall state. Based on the analysis of the feedback questionnaire, the effectiveness of SOL was significantly higher than that of relaxation.
In the weight of the index obtained by the entropy weight method, the weight of distress is the largest, with similar results found in psychoneuroendocrinological [
75] and psychosocial [
44] effects research on SOL, indicating that SOL therapy shows a more significant dispersion of the index and that the patient’s response is more sensitive. SOL can be used to recommend therapy to improve distress. The weights of ego-integrity and facit are 0.132 and 0.116, respectively. In the results, SOL therapy showed low sensitivities. If the patient needs to focus on improving these two indicators, this method is not applicable. The follow two comprehensive evaluation results were combined for evaluations. The proportions of
and
were 30% for the control group and 67.5% for the experiment group. The proportions of
and
were 17.5% for the control group and 45% for the experiment group. The proportions of
and
were 5% for the control group and 40% for the experiment group. The results showed that the proportion of the experimental group showed little fluctuation. In contrast, the control group fluctuated greatly, showing the consistency of the direct and indirect assessment of the treatment effect of SOL.This article provides a data analysis foundation for applying machine learning methods in the field of precision medicine.
Previous studies [
75] have found that one particular limitation was the high attrition rate in both salivary and photoplethysmographic sampling by challenges in data collection in palliative care. Therefore, despite analyzing data with an intention-to-treat approach using the available data (AAD) and multiply imputed data (MID) in the sensitivity analysis, the study might still have been statistically underpowered in detecting small differential effects due to missing data. Applying EWM-TOPSIS, the collaborative filtering algorithm (CFA) machine learning algorithm based on samples and attributes will be applied to predict some missing ratings that a patient provides. The merits of this method and the existing method of SOL are demonstrated in
Table 10.
The application ranges of the proposed technique and the existing methodologies are different. The EWM-TOPSIS is a psychological intervention therapy that can be recommended quickly and accurately. The statistical analysis shows the significant effect of factors with group assignments for psychological therapies; therefore, the potential working mechanisms of new psychosocial interventions can be investigated.