Misinformation and disinformation are prevalent across society today, their rise to prominence developed mainly through the expansion of social media. Misinformation is considered to present false information, presented as fact, regardless of intent to deceive; whereas disinformation is a type of misinformation that is intentionally false and intended to deceive or mislead [
1]. They bring with them particular complexities for health and social care for both the patient/consumer and the care professional.
Communication between people is recognised in health and care settings as the most important element between those who are receiving care (patients) and those delivering, managing, and evaluating care (healthcare professionals). The coronavirus pandemic has highlighted the significance we all place on communication in all its forms, which are commonly considered as verbal, non-verbal and para-verbal [
2]. This paper will explore communication through the perception of true or false information formed following the personal selection of influencers through digital media alongside developed bias and try to determine how such impacts upon patient care.
Human communication is often perceived as an exchange of information between two or more individuals [
3] through live conversations in person or via a telephone/video or through written media such as letters. Today, communication may include the use of digital devices, allowing for a diversity of communication applications such as searching for information (e.g., Google, Baidu, Shenma), meetings in groups (e.g., Zoom, WeChat, WhatsApp, Instagram, TikTok), keeping up with the latest comments (e.g., Facebook, Twitter, Sina Weibo, News agencies).
The core of the exploration in this paper will consider whether the array of information sources available have the possibility to develop bias in individuals and especially as to whether this has the potential to affect the way in which nurses and all healthcare professionals are able to help those in their care through maintaining a lack of bias when communicating with patients. We know, through health professional regulatory body standards, that it is important as health professionals to provide unbiased care to those to whom we attend but in a time of digital influencers, the question to be addressed is how can bias be reduced to meet patient need in practice?
To live as an individual, a member of a family, or within a community, or profession, we all need information, and this information forms the basis of our being [
4]. Following a constructivist path [
5], since birth, gathering information has been key to our development, from crawling to move somewhere else, to gaining new knowledge and skills throughout childhood and beyond. In all these developmental activities, we have all been influenced by those around us which has led to us making decisions based upon our acceptance or rejection of these influencers [
6].
In exploring this further, it is generally accepted that most entering adulthood have a considerable history of life events and this is unique to each person. A great deal of personal history has been influenced by those around them and as the days, weeks, months and years go by, more choices will need to be made in the paths each person chooses to follow and whether biased views are a challenge to living and learning [
7].
In recent years, it appears as though the mass of information available to us through various online platforms has driven many to be selective in their choice of influence. According to Chaffey [
8],
Social media users are now spending an average of 2 h and 24 min per day multi-networking across an average of eight social networks and messaging apps. There is an awareness that pretty much everything we do online is tracked in some way or other and that privacy laws have been slow to protect us all from feeding the ‘big data’ machine. When shopping online, we know that on subsequent digital platforms we are likely to see adverts for similar items. this, we have learnt over a very short period of time. However, have we started to think about our use of smart technologies in our homes and how our choices in the use of technologies such as virtual assistants, smart fridges, smart televisions—the list is endless—will influence our choice options in the future? Of course, it is not a one direction issue, there will be many benefits as well as challenges in the way we live as we progress further into the 21st Century, the pandemic in 2020 clearly demonstrated the need for agility and resilience in our daily lives as patients or health professionals, or both.
To explore the issues further and to frame the theme of the paper it might be useful to consider a humanistic information model as a representation of information ‘flows’ of individuals, be they those in our care as patients or those in our care as colleagues or family. Pictorially, the model is shown as
Figure 1.
Although shown as static on the page, it is important that you consider the four cogs as turning, as turning cogs generate power. The four cogs can represent an individual, or a team, department, professional discipline, or organisation, but for now, the individual use version will be considered.
Every waking moment we receive information through all our senses, the acquisition cog is constantly turning, which drives the other cogs and commonly, this information comes to us with pre-determined values (jagged line). That is, from sources which place their value on the information, such as news bulletins, conversations with friends; or, bland (straight line) with no values added, such as, for example, a certain aroma from a candle, although this may evoke memories within us.
The acquisition cog is connected to the processing cog and the dissemination cog, this allows for information passage which is either discarded immediately or processed. The processing cog is the key link between new information and stored information, where the latter contains our life history, including decisions we have made at different points in our lives which have made us the person we are. Within the processing cog is a moveable line dividing conscious and unconscious thought. During our life history we have learnt, for example, how doors work, thus, most times we do not consciously think about going through doorways; however, if we are blocked, then the thought level crosses the line into conscious thought, and we read ‘pull’ whilst we have been pushing the door. The position of the line determines just how much conscious or unconscious thought we place upon new information and the influence of stored information has in the determination of the position of the line, in health and care settings the line for a professional member of the care team may be quite high (unconscious level, almost automatic), as such, a conversation with a patient has been carried out before, whereas for the patient all the information has the potential to be new and so the line is low (conscious level, listening hard, trying to take it all in) as new knowledge is being processed.
The next cog is the storage cog, this holds us, our memories, and our lived experiences. It is this cog that influences the way we deal with new information based upon experiences and knowledge developed along the life path to date. As time goes by, there can be difficulty in raising memories to the conscious level and this is acutely seen in those suffering with dementia, as access to memory reduces over time until just the physical presence of the individual is left. Such memory loss and ability to filter at conscious and unconscious levels how information is processed, suggests that stored information is important to progress through life.
Finally, the dissemination cog, linking to the storage cog and the acquisition cog. There are two routes that information can move, either into the acquisition cog where additional information can be sought to add to that already held (seeking evidence); or, disseminated externally with individual values amassed during the process. Just the facial expression, way of standing or walking towards or away will signal your values/biases as to whether that is intended or not.
Today, the plethora of information available to us through all forms of media, devices and people we meet is vast. Below, taken from the 2019 World Economic Forum [
10], are estimates of data that are accessed/uploaded every day:
500 million tweets are sent;
294 billion emails are sent;
Four petabytes of data are created on Facebook;
Four terabytes of data are created from each connected car;
65 billion messages are sent on WhatsApp;
Five billion searches are made.
Indeed, recent reports have suggested that due to reduced airplane traffic linked to the coronavirus pandemic and the lack of constant information received from sensors in-flight, that predicting the weather forecast has become less accurate [
11]. There have been tales of individuals using You Tube
TM to build a house from scratch or making sourdough bread with no baking experience, let alone finding information on health-related material available on multiple social media platforms. The difficulty, particularly in relation to health and social influencers, is how individuals, patients and professionals, can determine the reliability and robustness of the information they find. Saigal [
12] considered the access to health information at the outset of the COVID-19 pandemic, particularly in western cultures, where some 74% of knowledge influence came from news organisations, with only around 1% being drawn from official health and science sites which led to incorrect understanding and potential dissemination of false knowledge, misinformation or disinformation.
A perfect storm would appear to be on the horizon based upon the level of ability of individuals to process influencing information at the conscious or unconscious level, the word ‘infodemic’ has been introduced into our language to describe a mass of information which may mislead and polarise opinions [
13]. Within the realms of health and care professional working, there is a distinct need to calm the storm and enable practitioners not only to be digitally capable but also intelligently influence knowledgeable which necessitates an understanding by the health professional of the patient’s view and checking their perceptions of the information being exchanged in a care setting.
Building upon an individual’s stored information, their life history, and making sure that the line between conscious and unconscious processing is appropriately positioned are complex issues but necessary to promote smart knowledge influence. It is relatively simple, after many years of professional practice, to assess someone in your care and have a ‘sixth sense’ that a deeper view of the situation needs to be taken, but how can such professional curiosity be developed in a healthcare student who is facing such a situation for the first time or, indeed, a patient facing a new diagnosis or changes to their long time condition? This is where education comes in for both the practitioner and the patient and now that there is such a close relationship between human communication and information technology, maybe it is time to blend the two?
We know that the emerging Fourth Industrial Revolution (Industry 4.0) [
14] will change the way in which information is sourced, filtered, and used. In the past thirty years we have changed logistics in manufacturing from bulk ordering to just-in-time supply chains, could this become a basis for re-thinking undergraduate learning? It has been argued that ‘just-in-time’ (JIT) learning strengthens effectiveness and productivity [
15] but it is equally acknowledged that this is not the silver bullet, and as such, requires JIT to be used appropriately where it will have most relevance and impact for the individual whether they be a patient, healthcare professional student, or where the ‘student’ could be a patient or health provider [
16]. Chute and French [
17] developed a personal perspective for individuals which they cite as Care 4.0, using aspects of Industry 4.0 to demonstrate the ways in which healthcare can be transformed to meet the needs of individuals through digital technologies.
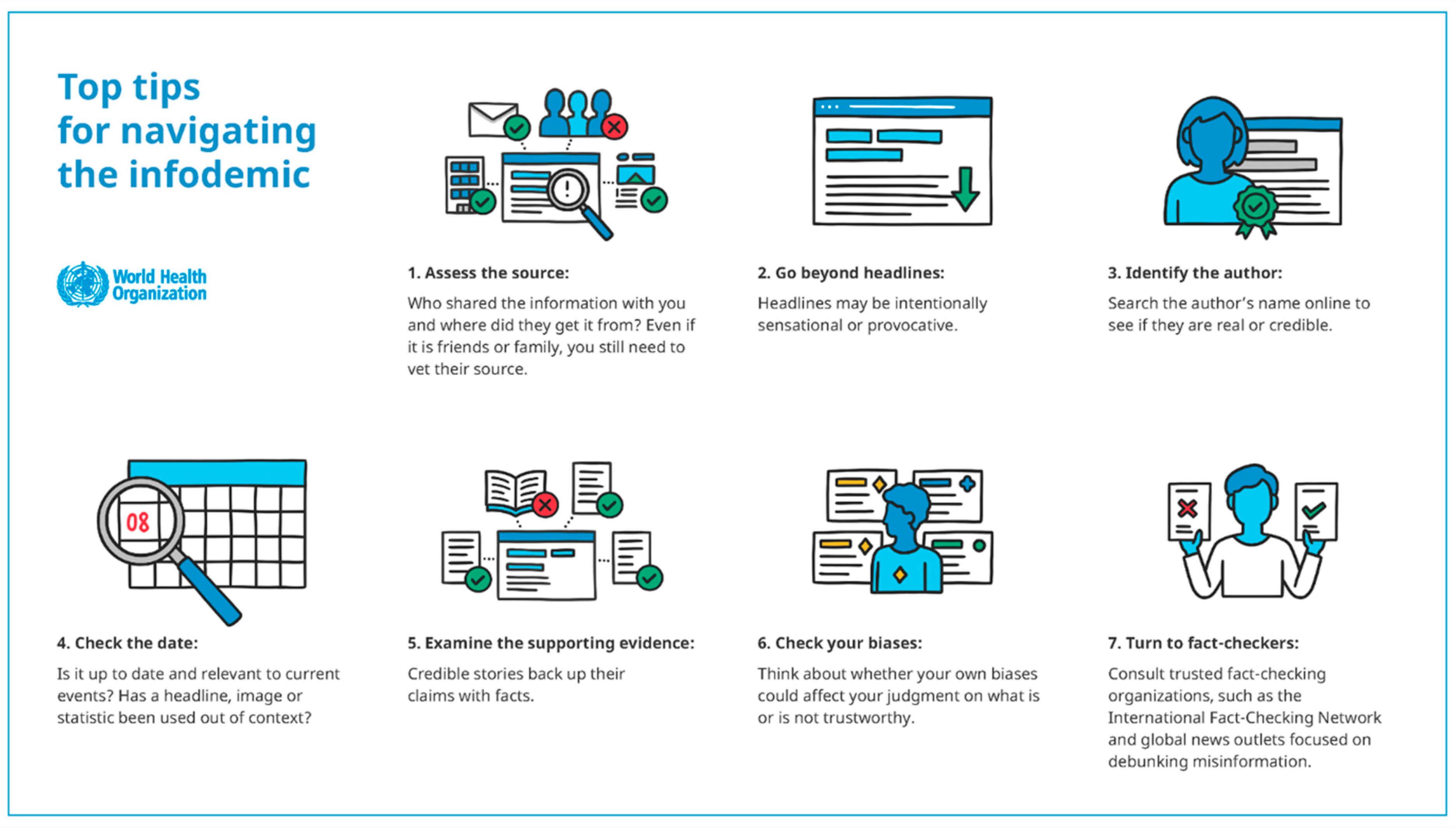
The ownership of learning and the building of knowledge through information gathering belongs to the individual, be that, in this instance, a patient or a member of the professional health and care team, gathering information from any source across the information intensive world in which we now live, individuals need to be information ‘smart’. The World Health Organisation [
18] offers seven tips for navigating the infodemic as shown in
Figure 2:
Social media has opened opportunities for each of us, patient and/or health professional, to align ourselves to personally selected influencers and this reduces the diversity of information sharing. Is there an automatic assumption made by those receiving care (consumers of care) that those providing care must be qualified to do so and have the best interests of the patient at the centre of all they do? Points 1 and 3 above are concerned with this issue.
An instance from an educational setting is offered to explore this aspect further. The digital managed learning environment, used locally, allows for statistical reports on student use as part of everyday processes; out of interest I recently explored one undergraduate unit of learning, which started in October 2020 with 751 students enrolled. The total hits recorded were 8528 up until 18 December 2020 and of these, no accesses to staff information were made. Such a lack of enquiry about the author(s) of the learning content maybe suggests that there is a stored rationale that someone ‘teaching’ or offering knowledge information must be knowledgeable and credible. Such lack of interest in those teaching appears to be very different to the magnetism social media influencers generate. Is the same rationale transferred to other situations, particularly related to patients or their relatives and friends where information is exchanged and if it is, how can this cycle be broken allowing for authorship credibility to be assured between both the patient and the healthcare professional?
As considered earlier, each of us have developed our own biases during our lifetime and when talking with patients, their relatives and friends, do we consider how our own biases might affect our communication of information? For the patient, is there an automatic acceptance that the healthcare professional is giving the appropriate information for the patient’s condition or does the patient bring with them information gained from different sources through digital media that conflict with the professional guidance and how might this impact upon the trust in the care relationship? What measure of effectiveness of communication trustworthiness should be employed? There are certainly a lot to choose from, for example, Merk and Rosman [
19] and their thoughts on epistemic trustworthiness through to the work of Best [
20], who outlines elements of trust and responsibilities of information givers in the form of a blog. In any conversation there may be sensitivities (biases) that are not obvious until the conversation ‘touches’ one of those sensitivities. How do such biases, in terms of gateways to health care practice and trustworthiness, affect information exchange/communication in such settings? The coronavirus hospitalisations have demonstrated, once again, just how important communication is in the caring environment, is there a case now for an outreach approach to be taken by healthcare professionals using social media to extend the information and care support to those with whom therapeutic relationships have been formed beyond the hospital walls as was initially considered through using information prescriptions [
21,
22]? Point 6 in the above image concerns this issue.
From the image, Points 2, 4 and 5 require health and care professionals to become smart knowledge influencers where those in their care can be assured that the information exchanged is up to date, evidence based and has a depth that is appropriate to allow for full understanding of the communication encounter. Health and care professionals need to take a key role in helping those in their care to be assured that the information contained in any communication is correct, and as such, act as ‘fact-checkers’ along with the overarching regulations such as privacy and data protection legislation.
Information and communication often appear as simple concepts and indeed they are at a basic level, however, with the emergence of social media and greater access to information anytime and commonly anywhere, the possibilities for misinformation amongst patients are high. Such access is a complicating factor entering biases that all health and care practitioners need to understand, the humanistic information model relates both to professional activity communicating with those in their care and all individuals determining their conscious and unconscious processing of information, which may affect their understanding of the care offered. Technology will become more sophisticated and require us to be more discerning in the uptake of influenced information, the emerging ‘deepfake’ [
23] computer generated versions of trusted individuals. As the focus of health care becomes more patient/consumer centric, it is vital that the role of influencers through social media is acknowledged in their presentation of a diverse range of views, accurately or inaccurately, which in turn, has the potential to create bias for both the patient and the healthcare professional, thus, complicating and blurring the communication processes.
It is unlikely that there is a way of halting the infodemic, but there are ways of managing it. In this paper, some of the points for consideration by health and care professionals as they communicate with patients have been outlined. It is acknowledged that further work needs to be undertaken in this area to ensure that there is recognition of 21st Century patient care information, misinformation, disinformation, and the role of influencers in determining health and care bias amongst patients and professional health care givers.