Creating a Pediatric Prehospital Destination Decision Tool Using a Modified Delphi Method
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Systematic Review of the Literature
2.3. First in-Person Meeting (Round 1)
2.4. Item Specifications and Verbiage (Round 2)
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Shah, M.N.; Cushman, J.T.; Davis, C.O.; Bazarian, J.J.; Auinger, P.; Friedman, B. The epidemiology of emergency medical services use by children: An analysis of the National Hospital Ambulatory Medical Care Survey. Prehosp. Emerg. Care 2008, 12, 269–276. [Google Scholar] [CrossRef] [Green Version]
- Fishe, J.N.; Psoter, K.J.; Klein, B.L.; Anders, J.F. Retrospective Evaluation of Risk Factors for Pediatric Secondary Transport. Prehosp. Emerg. Care 2018, 22, 41–49. [Google Scholar] [CrossRef]
- Franca, U.; McManus, M.L. Availability of Definitive Hospital Care for Children. JAMA Pediatr. 2017, 171, e171096. [Google Scholar] [CrossRef] [PubMed]
- Grube, M.E. The big squeeze in search of a sustainable future for suburban community hospitals. Healthc. Financ. Manag. 2006, 60, 56–65. [Google Scholar]
- Stroud, M.H.; Trautman, M.S.; Meyer, K.; Moss, M.M.; Schwartz, H.P.; Bigham, M.T.; Tsarouhas, N.; Douglas, W.P.; Romito, J.; Hauft, S. Pediatric and Neonatal Interfacility Transport: Results from a National Consensus Conference. Pediatrics 2013, 132, 359–366. [Google Scholar] [CrossRef] [Green Version]
- Li, J.; Monuteaux, M.C.; Bachur, R. Interfacility Transfers of Noncritically Ill Children to Academic Pediatric Emergency Departments. Pediatrics 2012, 130, 83–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Odetola, F.O.; Mann, N.C.; Hansen, K.W.; Patrick, S.; Bratton, S.L. Source of admission and outcomes for criti-cally injured children in the mountain states. Arch. Pediatr. Adolesc. Med. 2010, 164, 277–282. [Google Scholar] [CrossRef] [Green Version]
- Anders, J.F.; Adelgais, K.; Hoyle, J.D.J.R.; Olsen, C.; Jaffe, D.M.; Leonard, J.C. Comparison of outcomes for children with cervical spine injury based on destination hospital from scene of injury. Acad. Emerg. Med. 2014, 21, 55–64. [Google Scholar] [CrossRef] [Green Version]
- Cook, S.H.; Fielding, J.R.; Phillips, J.D. Repeat abdominal computed tomography scans after pediatric blunt abdominal trauma: Missed injuries, extra costs and unnecessary radiation exposure. J. Pediatr. Surg. 2010, 45, 2019–2024. [Google Scholar] [CrossRef]
- Orr, R.A.; Venkataraman, S.T.; Cinoman, M.I.; Hogue, B.L.; Singleton, C.A.; McCloskey, K.A. Pretransport Pediatric Risk of Mortality (PRISM) score underestimates the requirement for intensive care or major interventions during interhospital transport. Crit. Care Med. 1994, 22, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Kanter, R.K.; Boeing, N.M.; Hannan, W.P.; Kanter, D.L. Excess morbidity associated with interhospital transport. Pediatrics 1992, 90, 893–898. [Google Scholar]
- Ammon, A.A.; Fath, J.J.; Brautigan, M.; Mehta, R.; Matthews, J. Transferring patients to a pediatric trauma center: The trans-ferring hospital’s perspective. Pediatr. Emerg. Care 2000, 16, 332–334. [Google Scholar] [CrossRef]
- Harrison, T.; Thomas, S.H.; Wedel, S.K. Interhospital aeromedical transports: Air medical activation intervals in adult and pediatric trauma patients. Am. J. Emerg. Med. 1997, 15, 122–124. [Google Scholar] [CrossRef]
- Walls, T.A.; Chamberlain, J.M.; Strohm-Farber, J.; Klein, B.L. Improving pretransport care of pediatric emergency patients: An assessment of referring hospital care. Pediatr. Emerg. Care 2010, 26, 567–570. [Google Scholar] [CrossRef]
- Brinkman, A.S.; Gill, K.G.; Leys, C.M.; Gosain, A. Computed tomography-related radiation exposure in chil-dren transferred to a Level I pediatric trauma center. J. Trauma Acute Care Surg. 2015, 78, 1134–1137. [Google Scholar] [CrossRef] [Green Version]
- McManus, K.; Finlay, E.; Palmer, S.; Anders, J.F.; Hendry, P.; Fishe, J.N. A Statewide Analysis of Reason for EMS’ Pediatric Destination Choice. Prehosp. Emerg. Care 2020, 24, 672–682. [Google Scholar] [CrossRef] [PubMed]
- Sasser, S.M.; Hunt, R.C.; Faul, M.; Sugerman, D.; Pearson, W.S.; Dulski, T.; Wald, M.M.; Jurkovich, G.J.; Newgard, C.D.; Lerner, E.B. Guidelines for field triage of injured patients: Recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm. Rep. 2012, 61, 1–20. [Google Scholar]
- Le May, M.R.; So, D.Y.; Dionne, R.; Glover, C.A.; Froeschl, M.P.; Wells, G.A.; Davies, R.F.; Maloney, J.; Marquis, J.-F.; Labinaz, M. A citywide protocol for primary PCI in ST-segment elevation myocardial infarction. N. Engl. J. Med. 2008, 358, 231–240. [Google Scholar] [CrossRef] [Green Version]
- Kidwell, C.S.; Starkman, S.; Eckstein, M.; Weems, K.; Saver, J.L. Identifying stroke in the field. Prospective validation of the Los Angeles prehospital stroke screen (LAPSS). Stroke 2000, 31, 71–76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leleu, H.; Capuano, F.; Ferrua, M.; Nitenberg, G.; Minvielle, E.; Schiele, F. Symptom-to-needle times in ST-segment elevation myocardial infarction: Shortest route to a primary coronary intervention facility. Arch. Cardiovasc. Dis. 2013, 106, 162–168. [Google Scholar] [CrossRef]
- Cheney, P.; Haddock, T.; Sanchez, L.; Ernst, A.; Weiss, S. Safety and compliance with an emergency medical service direct psychiatric center transport protocol. Am. J. Emerg. Med. 2008, 26, 750–756. [Google Scholar] [CrossRef]
- Vicente, V.; Sjöstrand, F.; Sundström, B.W.; Svensson, L.; Castren, M. Developing a decision support system for geriatric patients in prehospital care. Eur. J. Emerg. Med. 2013, 20, 240–247. [Google Scholar] [CrossRef]
- Jollis, J.G.; Roettig, M.L.; Aluko, A.O.; Anstrom, K.J.; Applegate, R.J.; Babb, J.D.; Berger, P.B.; Bohle, D.J.; Fletcher, S.M.; Garvey, J.L. Implementation of a Statewide System for Coronary Reperfusion for ST-Segment Elevation Myocardial Infarction. JAMA 2007, 298, 2371–2380. [Google Scholar] [CrossRef] [Green Version]
- Le May, M.R.; Wells, G.A.; So, D.Y.; Glover, C.A.; Froeschl, M.; Maloney, J.; Dionne, R.; Marquis, J.-F.; O’Brien, E.R.; Labinaz, M. Reduction in mortality as a result of direct transport from the field to a receiving center for primary percutaneous coronary intervention. J. Am. Coll. Cardiol. 2012, 60, 1223–1230. [Google Scholar] [CrossRef] [Green Version]
- Maryland Institute for EMS Systems. Trauma Decision Tree (Page 174) Maryland Protocols for Pre-Hospital Providers. Available online: https://www.miemss.org/home/Portals/0/Docs/Guidelines_Protocols/MD-Medical-Protocols-2019.pdf (accessed on 27 June 2021).
- Lerner, E.B.; Cushman, J.T.; Drendel, A.L.; Badawy, M.; Shah, M.N.; Guse, C.E.; Cooper, A. Effect of the 2011 Revisions to the Field Triage Guidelines on Under- and Over-Triage Rates for Pediatric Trauma Patients. Prehosp. Emerg. Care 2017, 21, 456–460. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.K.; Black, N.A.; Lamping, D.L.; McKee, C.M.; Sanderson, C.F.; Askham, J.; Marteau, T. Consensus development methods, and their use in clinical guideline development: A review. Health Technol. Assess. 1998, 2, 1–88. [Google Scholar] [CrossRef] [Green Version]
- Eubank, B.H.; Mohtadi, N.G.; Lafave, M.R.; Wiley, J.P.; Bois, A.J.; Boorman, R.S.; Sheps, D.M. Using the modified Delphi method to establish clinical con-sensus for the diagnosis and treatment of patients with rotator cuff pathology. BMC Med. Res. Methodol. 2016, 16, 56. [Google Scholar] [CrossRef] [Green Version]
- Kunz, D.; Pariyadath, M.; Wittler, M.; Askew, K.; Manthey, D.; Hartman, N. Derivation of a Performance Checklist for Ultrasound-Guided Arthrocentesis Using the Modified Delphi Method. J. Ultrasound Med. 2017, 36, 1147–1152. [Google Scholar] [CrossRef] [Green Version]
- Browne, L.R.; Shah, M.I.; Studnek, J.R.; Farrell, B.M.; Mattrisch, L.M.; Reynolds, S.; Ostermayer, D.G.; Brousseau, D.C.; Lerner, E.B. 2015 Pediatric Research Priorities in Prehospital Care. Prehosp. Emerg. Care 2016, 20, 311–316. [Google Scholar] [CrossRef]
- Studnek, J.R.; Lerner, E.B.; Shah, M.I.; Browne, L.R.; Brousseau, D.C.; Cushman, J.T.; Dayan, P.S.; Drayna, P.C.; Kahn, C.A.; Stanley, R.M. Consensus-based Criterion Standard for the Identification of Pe-diatric Patients Who Need Emergency Medical Services Transport to a Hospital with Higher-level Pedi-atric Resources. Acad. Emerg. Med. 2018, 25, 1409–1414. [Google Scholar] [CrossRef] [Green Version]
- Custer, R.L.; Scarcella, J.A.; Stewart, B.R. The Modified Delphi Technique—A Rotational Modification. J. Career Tech Educ. 1999, 15, 50–58. [Google Scholar] [CrossRef]
- Fratta, K.A.; Fishe, J.N. EMS Pediatric Transport Safety and Secondary Transport. Available online: https://www.ncbi.nlm.nih.gov/books/NBK513234/ (accessed on 23 June 2021).
- Aledhaim, A.; Fishe, J.N.; Hirshon, J.M.; Anders, J.F. Pediatric Conditions Requiring Interfacility Transport from Emergency Departments: A Statewide Study of Regionalization. Pediatric Emerg. Care 2021, 37, e319–e323. [Google Scholar] [CrossRef]
- Gausche-Hill, M.; Eckstein, M.; Horeczko, T.; McGrath, N.; Kurobe, A.; Ullum, L.; Kaji, A.H.; Lewis, R.J. Paramedics Accurately Apply the Pediatric Assessment Triangle to Drive Management. Prehosp. Emerg. Care 2014, 18, 520–530. [Google Scholar] [CrossRef] [PubMed]
- Sahyoun, C.; Fleegler, E.; Kleinman, M.; Monuteaux, M.C.; Bachur, R. Early Identification of Children at Risk for Critical Care: Standardizing Communication for Inter–Emergency Department Transfers. Pediatr. Emerg. Care 2013, 29, 419–424. [Google Scholar] [CrossRef]
- Freire, G.; Kuppermann, N.; Zemek, R.; Plint, A.C.; Babl, F.E.; Dalziel, S.R.; Freedman, S.; Atenafu, E.G.; Stephens, D.; Steele, D.W. Predicting Escalated Care in Infants with Bronchiolitis. Pediatrics 2018, 142, e20174253. [Google Scholar] [CrossRef] [Green Version]
- Baker, J.; Cole, J. EMS, Medical Oversight of Systems. Available online: https://www.ncbi.nlm.nih.gov/books/NBK526093/ (accessed on 25 June 2021).
- American Burn Association. Burn Center Referral Criteria. Available online: https://ameriburn.org/wp-content/uploads/2017/05/burncenterreferralcriteria.pdf (accessed on 20 July 2021).
- Jones, C.M.C.; Cushman, J.T.; Lerner, E.B.; Fisher, S.G.; Seplaki, C.L.; Veazie, P.J.; Wasserman, E.B.; Dozier, A.; Shah, M.N. Prehospital Trauma Triage Decision-making: A Model of What Happens between the 9–1-1 Call and the Hospital. Prehosp. Emerg. Care 2016, 20, 6–14. [Google Scholar] [CrossRef] [Green Version]
- Newgard, C.D.; Rudser, K.; Atkins, D.L.; Berg, R.; Osmond, M.H.; Bulger, E.M.; Davis, D.P.; Schreiber, M.A.; Warden, C.; ROC Investigator. The availability and use of out-of-hospital physiologic infor-mation to identify high-risk injured children in a multisite, population-based cohort. Prehosp. Emerg. Care. 2009, 13, 420–431. [Google Scholar] [CrossRef] [Green Version]
- Fleming, S.; Gill, P.; Jones, C.; Taylor, J.A.; Van den Bruel, A.; Heneghan, C.; Roberts, N.; Thompson, M. The Diagnostic Value of Capillary Refill Time for Detecting Serious Ill-ness in Children: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0138155. [Google Scholar] [CrossRef] [Green Version]
- Studnek, J.R.; Brown, L.R.; Shah, M.I.; Fumo, N.; Hansen, M.; Lerner, E.B. Validity of the Pediatric Early Warning Score and the Bedside Pediatric Early Warning Score in Classifying Patients who Reguiqre the Resources of a Higher Level Pediatric Hospital. Prehosp. Emerg. Care 2020, 24, 341–348. [Google Scholar] [CrossRef]
- Lang, E.S.; Spaite, D.W.; Oliver, Z.J.; Gotschall, C.S.; Swor, R.A.; Dawson, D.E.; Hunt, R.C. A National Model for Developing, Implementing, and Evaluating Evidence-based Guidelines for Prehospital Care. Acad. Emerg. Med. 2012, 19, 201–209. [Google Scholar] [CrossRef]
- Institute of Medicine (U.S.). Committee on the Future of Emergency Care in the United States Health System. In Emergency Care for Children: Growing Pains; National Academies Press: Washington, DC, USA, 2007. [Google Scholar]
- Institute of Medicine (U.S.). Committee on the Future of Emergency Care in the United States Health System. In Hospital-Based Emergency Care: At the Breaking Point; National Academies Press: Washington, DC, USA, 2007. [Google Scholar]
- Tennessee Department of Health Board for Licensing of Health Care Facilities. Standards for Pediatric Emergency Care Facilities. 2016. Available online: http://cecatn.org/wp-content/uploads/2018/04/Standards-for-Peds-Emergency-Care-Facilities.pdf (accessed on 27 June 2021).
- Camargo, A.; Boggs, K.M.; Auerbach, M.; Freid, R.D.; Sullivan, A.F.; Espinola, J.A.; Camargo, C.A., Jr. National Study of Self-reported Pediatric Areas in United States General Emergency Departments. Acad. Emerg. Med. 2018, 25, 1458–1462. [Google Scholar] [CrossRef] [Green Version]
- Gausche-Hill, M.; Wiebe, R.A. Guidelines for preparedness of emergency departments that care for children: A call to action. Pediatrics 2001, 107, 773–774. [Google Scholar] [CrossRef]
| MeSH Terms Used in Literature Search, Grouped by Category |
|---|
| Adolescent Child Infant Pediatrics |
| Ambulance Emergency Medical Services Emergency Medical Technicians |
| Critical Illness Critical Care Intensive Care Unit Intensive Care Unit, Pediatric |
| Hospitalization Referral and Consultation Tertiary Care Centers |
| Patient Transfer Patient Transport Time-to-treatment Secondary Transport |
| Predictive Value of Tests Triage Vital Signs |
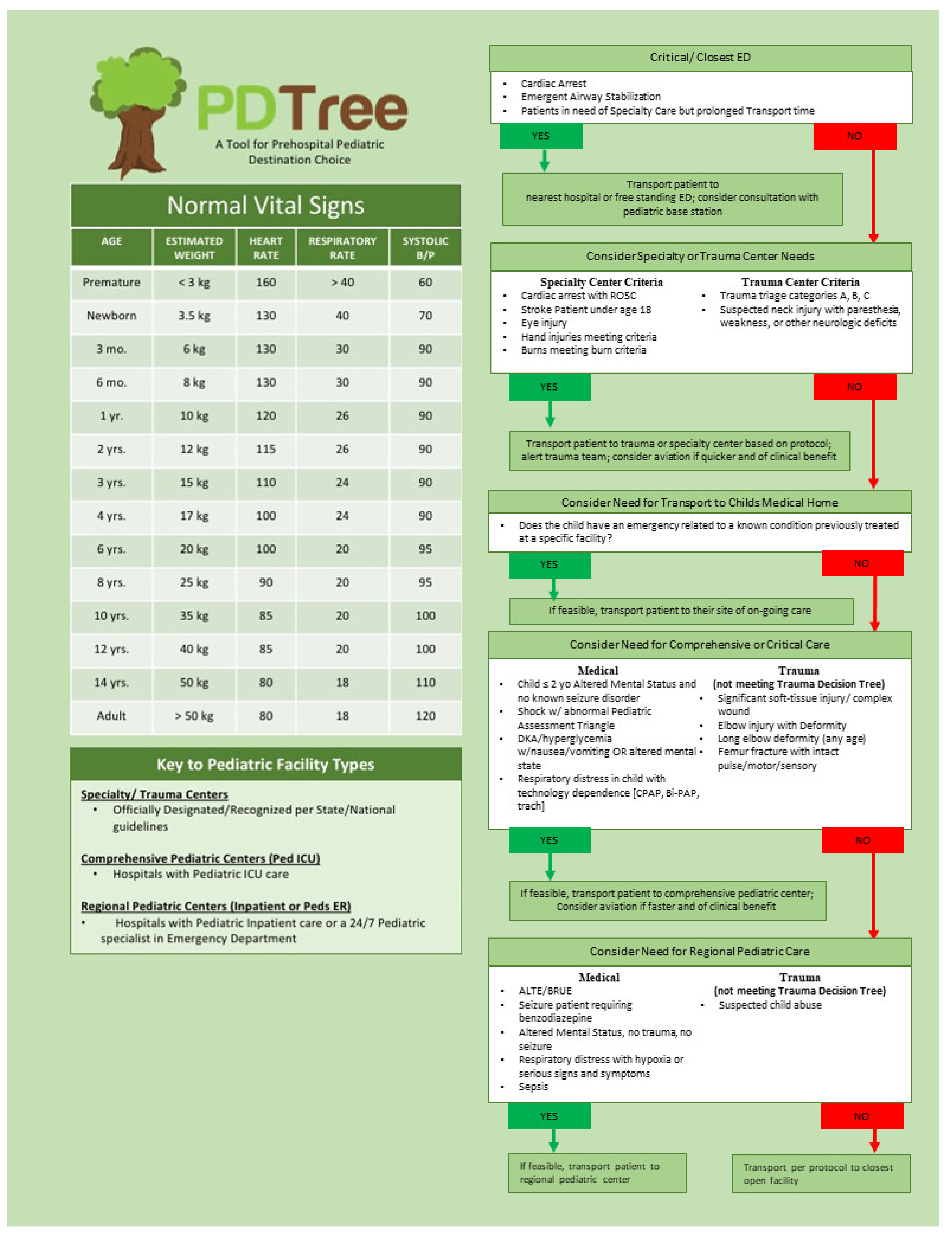
| Hospital Classification | Pediatric Capabilities |
|---|---|
| Specialty Center | Trauma, burn, or other specialty center for pediatrics as certified by state or national governing body |
| Comprehensive Center | The presence of a Pediatric Intensive Care Unit and Pediatric OR/anesthesia services |
| Regional Center | The presence of a pediatric inpatient unit or pediatric physician present on site 24-h per day |
| Closest Facility | All other open facilities, including freestanding ED |
| # | Condition | Round 1 Consensus for Inclusion | Pediatric Facility Capability Level | Round 2 Consensus for Inclusion | Pediatric Facility Capability Level |
|---|---|---|---|---|---|
| 1 | Femur Fracture | Yes | Comprehensive | ||
| 2 | Long Bone Fracture with Deformity | Yes | Comprehensive | ||
| 3 | Suspected C-spine Injury | Yes | Trauma/Specialty Center | ||
| 4 | Respiratory Distress with Oxygen Requirement | No | N/A | Yes-reworded | Regional |
| 5 | Respiratory Distress with Tracheostomy | Yes | Comprehensive | ||
| 6 | Non-traumatic Altered Level of Consciousness | Yes | No Level of Care Determined | Yes-dichotomized by age | <2 years old-Comprehensive |
| >2 years old-Regional | |||||
| 7 | ALTE/BRUE | Yes | No Level of Care Determined | Yes | Regional |
| 8 | Sepsis High Risk | Yes | Comprehensive | ||
| 9 | Sepsis Low Risk | Yes | Regional | ||
| 10 | Complex Wound | Yes | No Level of Care Determined | Yes-reworded | Comprehensive |
| 11 | Eye Injury | Yes | Trauma/Specialty Center | ||
| 12 | Children with Special Health Care Needs | Yes | Comprehensive | ||
| 13 | Suspected Child Abuse | Yes | No Level of Care Determined | Yes | Regional |
| 14 | DKA/Hyperglycemia | Yes | Comprehensive | ||
| 15 | Shock | Yes | No Level of Care Determined | Yes-Reworded | Comprehensive |
| 16 | Hypoxia | Yes | Do not include | ||
| 17 | Seizure with Medication Administration by EMS | Yes | No Level of Care Determined | Yes-Reworded | Regional |
| Original Wording (Round 1) | Revised Wording (Round 2) |
|---|---|
| Seizure Requiring Medication Administration by EMS | Seizure Requiring Benzodiazepine |
| Complex Wound | Significant soft-tissue injury/complex wound |
| Non-Trauma Altered Mental Status with no known seizure disorder | Dichotomized by age <2 yo and ≥2 yo |
| Shock | Shock with Abnormal Pediatric Assessment Triangle |
| Respiratory Distress with Oxygen Requirement | Respiratory Distress with Hypoxia or Serious Signs and Symptoms |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anders, J.F.; Fishe, J.N.; Fratta, K.A.; Katznelson, J.H.; Levy, M.J.; Lichenstein, R.; Milin, M.G.; Simpson, J.N.; Walls, T.A.; Winger, H.L. Creating a Pediatric Prehospital Destination Decision Tool Using a Modified Delphi Method. Children 2021, 8, 658. https://doi.org/10.3390/children8080658
Anders JF, Fishe JN, Fratta KA, Katznelson JH, Levy MJ, Lichenstein R, Milin MG, Simpson JN, Walls TA, Winger HL. Creating a Pediatric Prehospital Destination Decision Tool Using a Modified Delphi Method. Children. 2021; 8(8):658. https://doi.org/10.3390/children8080658
Chicago/Turabian StyleAnders, Jennifer F., Jennifer N. Fishe, Kyle A. Fratta, Jessica H. Katznelson, Matthew J. Levy, Richard Lichenstein, Michael G. Milin, Joelle N. Simpson, Theresa A. Walls, and Heather L. Winger. 2021. "Creating a Pediatric Prehospital Destination Decision Tool Using a Modified Delphi Method" Children 8, no. 8: 658. https://doi.org/10.3390/children8080658
APA StyleAnders, J. F., Fishe, J. N., Fratta, K. A., Katznelson, J. H., Levy, M. J., Lichenstein, R., Milin, M. G., Simpson, J. N., Walls, T. A., & Winger, H. L. (2021). Creating a Pediatric Prehospital Destination Decision Tool Using a Modified Delphi Method. Children, 8(8), 658. https://doi.org/10.3390/children8080658







