Limited Utility of SIRS Criteria for Identifying Serious Infections in Febrile Young Infants
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting
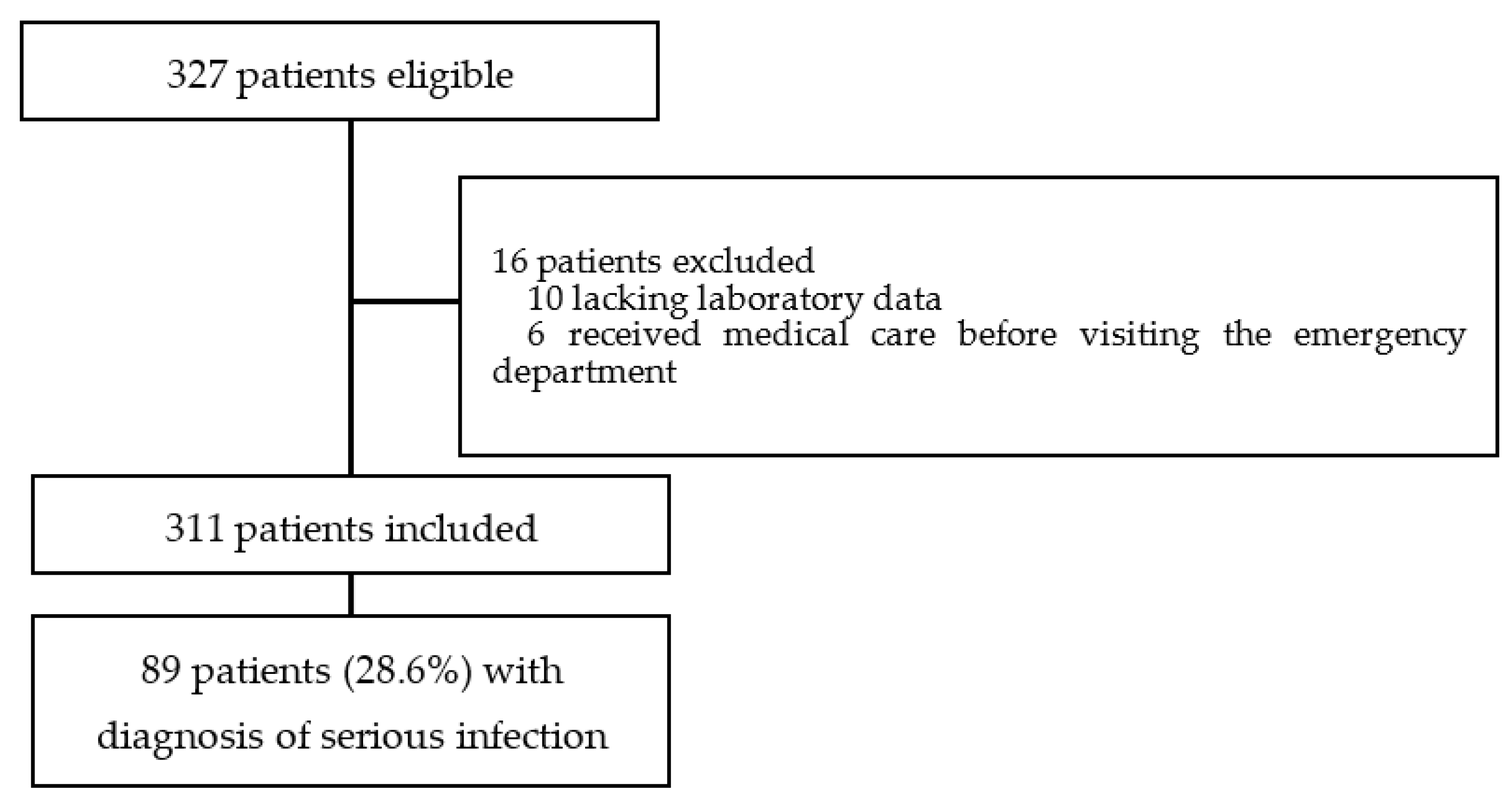
2.2. Study Design and Selection of Participants
2.3. Data Collection
2.4. Definition
- (1)
- Septicemia (including bacteremia and viremia): pathogenic bacteria isolated from a blood culture or a pathogenic virus detected by real-time PCR.
- (2)
- Meningitis: identification of bacteria or a virus in cerebrospinal fluid.
- (3)
- Pneumonia: infiltrate on chest X-ray.
- (4)
- Soft tissue infection: acute suppurative inflammation of subcutaneous tissue.
- (5)
- Urinary tract infection: >positive urine culture with a single species of pathogen and systemic symptoms such as fever.
- (6)
- Bronchiolitis due to RSV or human metapneumovirus requiring emergency intervention and/or evidence of organ failure.
2.5. Analysis
3. Results
3.1. Patient Characteristics
3.2. Performance of the SIRS Criteria
3.3. Predictive Factors for Serious Infection
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pediatric, F.; Mace, S.E.; Gemme, S.R.; Valente, J.H.; Eskin, B.; Bakes, K.; Brecher, D.; Brown, M.D. Clinical Policy for Well-Appearing Infants and Children Younger Than 2 Years of Age Presenting to the Emergency Department with Fever. Ann. Emerg. Med. 2016, 67, 625–639. [Google Scholar]
- Pantell, R.H.; Roberts, K.B.; Adams, W.G.; Dreyer, B.P.; Kuppermann, N.; O’Leary, S.T.; Okechukwu, K.; Woods, C.R. Evaluation and management of well-appearing febrile infants 8 to 60 days old. Pediatrics 2021, 148, 2021052228. [Google Scholar] [CrossRef] [PubMed]
- Ralston, S.L.; Lieberthal, A.S.; Meissner, H.C.; Alverson, B.K.; Baley, J.E.; Gadomski, A.M.; Johnson, D.W.; Light, M.J.; Maraqa, N.F.; Mendonca, E.A.; et al. Clinical practice guideline: The diagnosis, management, and prevention of bronchiolitis. Pediatrics 2014, 134, 1474–1502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayakawa, I.; Nomura, O.; Uda, K.; Funakoshi, Y.; Sakakibara, H.; Horikoshi, Y. Incidence and aetiology of serious viral infections in young febrile infants. J. Paediatr. Child Health 2020, 56, 586–589. [Google Scholar] [CrossRef] [PubMed]
- Oades, P.J.; Ladhani, S. Enteroviral meningoencephalitis in an infant: An increasingly recognised infection. Arch. Dis. Child. 2015, 100, 208. [Google Scholar] [CrossRef]
- Britton, P.N.; Dale, R.C.; Nissen, M.D.; Crawford, N.; Elliott, E.; Macartney, K.; Khandaker, G.; Booy, R.; Jones, C.A. Parechovirus encephalitis and neurodevelopmental outcomes. Pediatrics 2016, 137, 20152848. [Google Scholar] [CrossRef] [Green Version]
- Rogan, D.T.; Kochar, M.S.; Yang, S.; Quinn, J.V. Impact of Rapid Molecular Respiratory Virus Testing on Real-Time Decision Making in a Pediatric Emergency Department. J. Mol. Diagn. 2017, 19, 460–467. [Google Scholar] [CrossRef] [Green Version]
- DePorre, A.G.; Aronson, P.L.; McCulloh, R.J. Facing the ongoing challenge of the febrile young infant. Crit. Care 2017, 21, 68. [Google Scholar] [CrossRef] [Green Version]
- Yun, K.W.; Choi, E.H.; Cheon, D.S.; Lee, J.; Choi, C.W.; Hwang, H.; Kim, B.l.; Park, K.Y.; Park, S.S.; Lee, H.J. Enteroviral meningitis without pleocytosis in children. Arch. Dis. Child. 2012, 97, 874–878. [Google Scholar] [CrossRef]
- Vos-Kerkhof, E.; Gomez, B.; Milcent, K.; Steyerberg, E.W.; Nijman, R.G.; Smit, F.J.; Mintegi, S.; Moll, H.A.; Gajdos, V.; Oostenbrink, R. Clinical prediction models for young febrile infants at the emergency department: An international validation study. Arch. Dis. Child. 2018, 103, 1033–1041. [Google Scholar] [CrossRef]
- Huppler, A.R.; Eickhoff, J.C.; Wald, E.R. Performance of low-risk criteria in the evaluation of young infants with fever: Review of the literature. Pediatrics 2010, 125, 228–233. [Google Scholar] [CrossRef] [Green Version]
- Bonsu, B.K.; Harper, M.B. Identifying febrile young infants with bacteremia: Is the peripheral white blood cell count an accurate screen? Ann. Emerg. Med. 2003, 42, 216–225. [Google Scholar] [CrossRef]
- Mintegi, S.; Gomez, B.; Martinez-Virumbrales, L.; Morientes, O.; Benito, J. Outpatient management of selected young febrile infants without antibiotics. Arch. Dis. Child. 2017, 102, 244–249. [Google Scholar] [CrossRef]
- Mintegi, S.; Gomez, B.; Carro, A.; Diaz, H.; Benito, J. Invasive bacterial infections in young afebrile infants with a history of fever. Arch. Dis. Child. 2018, 103, 665–669. [Google Scholar] [CrossRef]
- Singh, P.; Arora, A.; Strand, T.A.; Sommerfelt, H.; Lodha, R.; Kabra, S.K.; Aneja, S.; Natchu, U.C.M.; Chandra, J.; Rath, B.; et al. Predictors of death in infants with probable serious bacterial infection. Pediatr. Res. 2018, 83, 784–790. [Google Scholar] [CrossRef]
- Larsen, G.Y.; Mecham, N.; Greenberg, R. An emergency department septic shock protocol and care guideline for children initiated at triage. Pediatrics 2011, 127, 1585–1592. [Google Scholar] [CrossRef] [PubMed]
- Lukacs, S.L.; Schrag, S.J. Clinical sepsis in neonates and young infants, United States, 1988–2006. J. Pediatr. 2012, 160, 960–965. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, B.; Giroir, B.; Randolph, A. International pediatric sepsis consensus conference: Definitions for sepsis and organ dysfunction in pediatrics. Pediatr. Crit. Care Med. 2005, 6, 2–8. [Google Scholar] [CrossRef] [Green Version]
- Scott, H.F.; Greenwald, E.E.; Bajaj, L.; Davies, S.J.D.; Brou, L.; Kempe, A. The Sensitivity of Clinician Diagnosis of Sepsis in Tertiary and Community-Based Emergency Settings. J. Pediatr. 2018, 195, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Takei, H.; Nomura, O.; Hagiwara, Y.; Inoue, N. The management of pediatric genital injuries at a pediatric emergency department in Japan. Pediatr. Emerg. Care 2021, 37, 73–76. [Google Scholar] [CrossRef]
- Van den Bruel, A.; Haj-Hassan, T.; Thompson, M.; Buntinx, F.; Mant, D.; European Research Network on Recognising Serious Infection investigators. Diagnostic value of clinical features at presentation to identify serious infection in children in developed countries: A systematic review. Lancet 2010, 375, 834–845. [Google Scholar] [CrossRef]
- Nomura, O.; Ihara, T.; Sakakibara, H.; Hirokoshi, Y.; Inoue, N. Predicting serious bacterial infection in febrile young infants utilizing body temperature. Pediatr. Int. 2019, 61, 449–452. [Google Scholar] [CrossRef]
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017, 43, 304–377. [Google Scholar] [CrossRef]
- Matics, T.J.; Sanchez-Pinto, L.N. Adaptation and Validation of a Pediatric Sequential Organ Failure Assessment Score and Evaluation of the Sepsis-3 Definitions in Critically Ill Children. JAMA Pediatr. 2017, 171, 172352. [Google Scholar] [CrossRef]
- Raith, E.P.; Udy, A.A.; Bailey, M.; McGloughlin, S.; MacIsaac, C.; Bellomo, R.; Pilcher, D.V. Prognostic Accuracy of the SOFA Score, SIRS Criteria, and qSOFA Score for In-Hospital Mortality Among Adults with Suspected Infection Admitted to the Intensive Care Unit. JAMA 2017, 317, 290–300. [Google Scholar] [CrossRef]
- Coggins, S.; Harris, M.C.; Grundmeier, R.; Kalb, E.; Nawab, U.; Srinivasan, L. Performance of pediatric systemic inflammatory response syndrome and organ dysfunction criteria in late-onset sepsis in a quaternary neonatal intensive care unit: A case-control study. J. Pediatr. 2020, 219, 133–139. [Google Scholar] [CrossRef]
- Schroeder, A.R.; Shen, M.W.; Biondi, E.A.; Bendel-Stenzel, M.; Chen, C.N.; French, J.; Lee, V.; Evans, R.C.; Jerardi, K.E.; Mischler, M.; et al. Bacteraemic urinary tract infection: Management and outcomes in young infants. Arch. Dis. Child. 2016, 101, 125–130. [Google Scholar] [CrossRef]
- Shah, S.N.; Bachur, R.G.; Simel, D.L.; Neuman, M.I. Does This Child Have Pneumonia? The Rational Clinical Examination Systematic Review. JAMA 2017, 318, 462–471. [Google Scholar] [CrossRef] [PubMed]
- Scott, H.F.; Brou, L.; Deakyne, S.J.; Kempe, A.; Fairclough, D.L.; Bajaj, L. Association Between Early Lactate Levels and 30-Day Mortality in Clinically Suspected Sepsis in Children. JAMA Pediatr. 2017, 171, 249–255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sorokan, S.T.; Finlay, J.C.; Jefferies, A.L. Newborn male circumcision. Paediatr. Child. Health 2015, 20, 311–320. [Google Scholar] [CrossRef]
| Variables | Mean (SD) or % (n) |
|---|---|
| Demographics | |
| Age, days | 52.6 ± 23.7 |
| Age | |
| 0–27 days-old | 19.3 (60) |
| 28–60 days-old | 37.0 (115) |
| 61–89 days-old | 43.7 (136) |
| Male | 53.7 (167) |
| Gestational age, mean (SD), week | 38.6 (1.5) |
| Birth weight, mean (SD), g, n = 310 (0.3% missing) | 3008.8 (450.4) |
| Vital signs | |
| Core body temperature, mean (SD), °C | 38.6 (0.5) |
| Heart rate, mean (SD), beats per minute | 170.1 (19.5) |
| Respiratory rate, mean (SD), breaths per minute | 38.1 (10.7) |
| Oxygen saturation, mean (SD), % | 98.3 (2.2) |
| Physical examinations | |
| Peripheral poor perfusion, % (n) | 40.8 (127) |
| Capillary refilling time ≥ 2 s, % (n) | 22.8 (71) |
| Laboratory examinations | |
| WBC count, mean (SD), ×103 | 10.5 (4.6) |
| Neutrophils percentage, mean, % | 43.6 |
| Lymphocytes percentage, mean, % | 43.3 |
| Monocytes percentage, mean, % | 10.4 |
| WBC > 12,000/μl, % (n) | 92 (29.6) |
| WBC < 4000/μl, % (n) | 7 (2.3) |
| Band > 10% with normal WBC, % (n) | 5 (1.6) |
| Venous lactate (SD), mmol/L | 2.7 (0.9) |
| Systemic Inflammatory Response Syndrome, % (n) | 35.7 (114) |
| Clinical diagnosis | |
| Serious infections, % (n) | 28.6 (89) |
| Serious bacterial infections, % (n) * | 13.2 (41) |
| Serious viral infections, % (n) ** | 15.4 (48) |
| Disposition following the first visits | |
| Hospitalization in wards, % (n) | 56.9(177) |
| Discharged from the emergency department, % (n) | 40.8 (127) |
| Intensive care unit admission, % (n) | 2.3 (7) |
| 28-day mortality, % (n) | 0 (0) |
| Sensitivity, % (95% CI) | Specificity, % (95% CI) | Positive Predictive Value, % (95% CI) | Negative Predictive Value, % (95% CI) | Positive Likelihood Ratio, (95% CI) | Negative Likelihood Ratio, (95% CI) | |
|---|---|---|---|---|---|---|
| value (95%CI) | 47.2 (36.6–58.0) | 68.0 (61.4–74.0) | 37.2 (28.4–46.8) | 76.3 (69.6–81.9) | 1.5 (1.1–2.0) | 0.8 (0.6–0.9) |
| Variables | Serious Infection (n = 89) | No Serious Infection (n = 222) | p |
|---|---|---|---|
| Age, days, Mean (SD) | 49.2 (25.2) | 54.1 (23.0) | 0.101 |
| Male, % (n) | 68.5 (61) | 47.7 (106) | 0.001 |
| Gestational age, mean (SD), week | 38.6 (1.6) | 38.6 (1.5) | 0.796 |
| Birth weight, mean (SD), g | 3053.5 (421.6) | 2990.5 (461.5) | 0.253 |
| Vital signs | |||
| Core body temperature, mean (SD), °C | 38.7 (0.5) | 38.5 (0.4) | 0.004 |
| Heart rate, mean (SD), beats per minute | 175.6 (20.9) | 167.9 (18.4) | 0.001 |
| Respiratory rate, mean (SD), breaths per minute | 38.8 (11.2) | 37.8 (10.4) | 0.429 |
| Oxygen saturation, mean (SD), % | 97.9 (3.2) | 98.5 (1.6) | 0.015 |
| Physical findings | |||
| Peripheral poor perfusion, % (n) | 51.7 (46) | 36.5 (81) | 0.016 |
| Capillary refilling time ≥ 2 s, % (n) | 31.5 (28) | 19.4 (43) | 0.025 |
| Laboratory examinations | |||
| WBC count, mean (SD), ×103 | 10.6 (4.9) | 10.4 (4.5) | 0.801 |
| Neutrophils, mean, % | 48.0 | 42.2 | 0.006 |
| Lymphocytes, mean, % | 39.3 | 44.5 | 0.008 |
| Monocytes, mean, % | 9.8 | 10.6 | 0.208 |
| Venous lactate (SD), mmol/L | 2.6 (0.9) | 2.7 (0.9) | 0.362 |
| Characteristics | Odds Ratio | 95% CI | p |
|---|---|---|---|
| Male | 2.45 | 1.41–4.28 | 0.002 |
| Core body temperature ≥ 38.5 °C | 2.34 | 1.32–4.13 | 0.003 |
| Heart rate ≥ 178 bpm | 2.21 | 1.28–3.83 | 0.005 |
| Age ≤ 50 days | 2.13 | 1.21–3.77 | 0.009 |
| Oxygen saturation ≤ 96% | 1.89 | 0.92–3.87 | 0.083 |
| WBC count ≥ 14.0 × 103 | 1.49 | 0.76–2.92 | 0.249 |
| Respiratory rate ≥ 50/min | 1.44 | 0.71–2.95 | 0.316 |
| Venous lactate ≥ 3.7 mmol/L | 1.03 | 0.50–2.13 | 0.939 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nomura, O.; Morikawa, Y.; Mori, T.; Hagiwara, Y.; Sakakibara, H.; Horikoshi, Y.; Inoue, N. Limited Utility of SIRS Criteria for Identifying Serious Infections in Febrile Young Infants. Children 2021, 8, 1003. https://doi.org/10.3390/children8111003
Nomura O, Morikawa Y, Mori T, Hagiwara Y, Sakakibara H, Horikoshi Y, Inoue N. Limited Utility of SIRS Criteria for Identifying Serious Infections in Febrile Young Infants. Children. 2021; 8(11):1003. https://doi.org/10.3390/children8111003
Chicago/Turabian StyleNomura, Osamu, Yoshihiko Morikawa, Takaaki Mori, Yusuke Hagiwara, Hiroshi Sakakibara, Yuho Horikoshi, and Nobuaki Inoue. 2021. "Limited Utility of SIRS Criteria for Identifying Serious Infections in Febrile Young Infants" Children 8, no. 11: 1003. https://doi.org/10.3390/children8111003
APA StyleNomura, O., Morikawa, Y., Mori, T., Hagiwara, Y., Sakakibara, H., Horikoshi, Y., & Inoue, N. (2021). Limited Utility of SIRS Criteria for Identifying Serious Infections in Febrile Young Infants. Children, 8(11), 1003. https://doi.org/10.3390/children8111003






