Virtual Reality as a Non-Pharmacological Aid for Reducing Anxiety in Pediatric Dental Procedures
Abstract
1. Introduction
2. Materials and Methods
- Aged between 6 and 12 years;
- Scheduled for non-invasive dental procedures, such as dental cleanings, fluoride applications, or examinations for early-stage caries;
- No history of severe dental phobia, epilepsy, vestibular or cognitive disorders, or other neurological conditions that may contraindicate VR use;
- Children with visual or auditory impairments, diagnosed anxiety disorders, or those requiring extensive dental treatments were excluded from the study.
2.1. Data Collection
- o
- EDA (electrodermal activity): Refers to changes in the electrical properties of the skin, primarily due to sweat gland activity. It is measured in microsiemens (μS) and reflects the level of emotional arousal or stress. Higher EDA values typically indicate increased sympathetic nervous system activation.
- o
- BVP (blood volume pulse): Measures changes in blood volume in peripheral circulation, usually obtained through photoplethysmography. It is often represented in arbitrary units and provides information about heart rate and blood flow. BVP patterns can indicate cardiovascular responses to stress or relaxation.
- o
- Stress level: This is not directly measured but inferred from physiological indicators like EDA and BVP. Increased stress is generally associated with higher EDA values, more frequent EDA peaks, and greater variability in BVP patterns. Stress levels are typically described qualitatively (low, medium, high) based on combined analysis.
- Animated cartoons such as SpongeBob SquarePants, Tom and Jerry, etc.;
- Immersive natural scenes, such as beaches, forests, or underwater environments, accompanied by soothing instrumental music.
- Routine dental examinations;
- Fluoride application;
- Professional dental cleanings (supragingival scaling).
2.2. Study Objectives and Purpose
- Quantify physiological effects: Assess the impact of VR on physiological stress indicators, such as heart rate, heart rate variability, and skin-conductance, compared to a control condition without VR. Moreover, to determine whether the use of VR during dental procedures improves the comfort, relaxation, and cooperation of pediatric patients.
- Compare VR to traditional techniques: Contrast the outcomes of VR interventions with traditional approaches for managing pediatric dental anxiety to establish its potential as an alternative or complementary method.
- Support future applications: Provide preliminary evidence to inform the broader adoption of VR in clinical pediatric dentistry and guide future research on its long-term impacts and applicability for more invasive procedures.
2.3. Limitations and Potential Bias
- Sample size and diversity: The study included 120 participants from three clinics, which may not represent broader demographic or geographic variability. Results might differ in other populations or cultural contexts.
- Non-blinded design: Participants and dental practitioners were aware of the intervention (VR use), which could introduce performance or placebo effects.
- Short-term evaluation: The study focused on immediate physiological and behavioral responses during and shortly after the dental procedure. Long-term effects on dental anxiety reduction were not assessed. Moreover, each child participated in only one session with VR and one without, which may not capture the cumulative effects of repeated VR use over time.
- Variability in VR content preferences: Individual differences in preferences for VR content (cartoons vs. natural scenes) could influence engagement levels and outcomes, introducing variability in the results.
- Limited range of dental procedures: The study focused on minor, non-invasive dental procedures, which may not fully represent the anxiety levels experienced during more complex or painful treatments.
- Physiological measurement constraints: Biometric data were collected via wearable devices that, while validated, might have limited accuracy compared to clinical-grade monitoring equipment.
- Potential external influences: Factors such as parental presence, clinic environment, and interactions with dental staff could influence anxiety levels independently of VR use.
- Standardization challenges across clinics: Although efforts were made to maintain consistency, differences in clinic environments, practitioner approaches, or equipment could have introduced variability.
3. Results
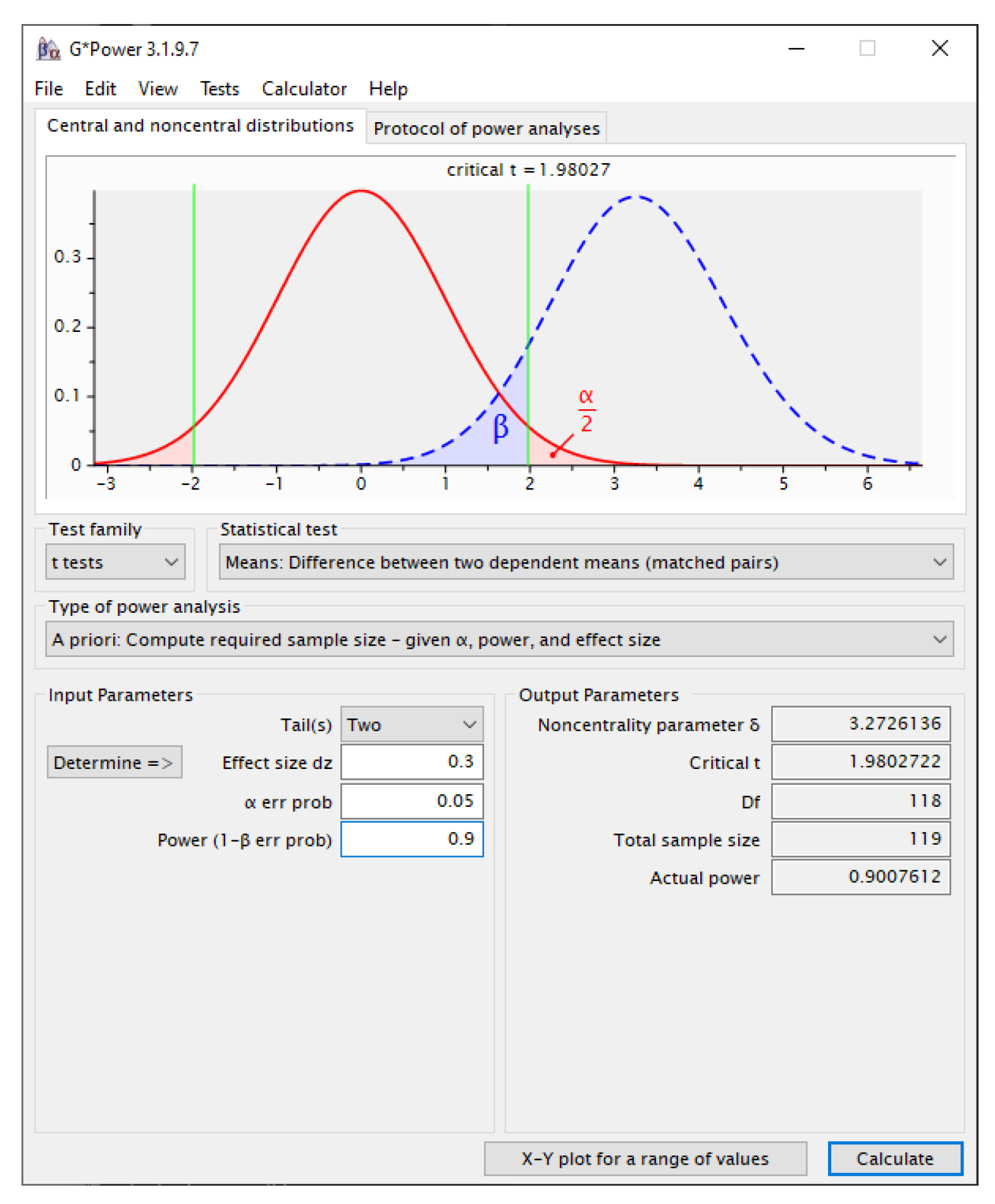
3.1. Sample-Size Determination
- Effect size (d) = 0.30.
- α error probability = 0.05 (two-sided).
- Statistical power (1 − β) = 0.90, ensuring a 10% maximum risk of Type II error.
3.2. Statistical Analysis
3.2.1. Descriptive Statistics
- Electrodermal activity (EDA): Integer counts of skin-conductance responses per session (SCR peaks).
- Blood volume pulse (BVP): Integrated plethysmographic amplitude expressed in device-specific, arbitrary units (30–500).
3.2.2. Inferential Statistics
- Normality check. The distribution of change scores was examined with the Shapiro–Wilk test. Given the large sample (n = 120), the paired-samples t-test was retained even when minor deviations from normality were present.
- Paired comparisons. Two-tailed paired-samples t-tests compared baseline and VR values for EDA and BVP. Statistical significance was set at α = 0.05. The output reported t values, degrees of freedom (df = n − 1), exact p values, and 95% CIs for the mean differences.
- Effect size. Practical importance was quantified with Cohen’s d for dependent means, calculated as d = t/√ n. Benchmarks of 0.20, 0.50, and 0.80 were interpreted as small, medium, and large effects, respectively.
3.3. Statistical Results
3.3.1. Descriptive Statistics
3.3.2. Paired Comparisons
3.3.3. Summary
4. Discussion
5. Conclusions
- Quantifying physiological effects: The data clearly shows a reduction in physiological stress indicators when VR is used. Electrodermal activity (EDA) measurements during VR sessions exhibit lower and more stable readings, with fewer peaks and lower amplitudes compared to the non-VR session. This indicates decreased sympathetic nervous system activation, suggesting improved comfort and relaxation. Blood volume pulse (BVP) data also demonstrate more consistent patterns in VR sessions, reflecting a calmer cardiovascular state. These physiological markers strongly suggest that VR improves patient comfort, relaxation, and potentially cooperation during dental procedures.
- Comparing VR to traditional techniques: While the data does not directly compare VR to other traditional anxiety management techniques, the stark contrast between VR and non-VR sessions implies that VR could be a highly effective alternative or complementary method. The significant reduction in stress indicators during VR sessions suggests that this approach may be superior to some traditional methods in managing pediatric dental anxiety.
- Supporting future applications: The consistent positive results across multiple VR sessions provide compelling preliminary evidence to support the broader adoption of VR in clinical pediatric dentistry. The clear physiological benefits observed in these simple dental procedures offer a strong foundation for future research. These data can guide investigations into VR’s long-term impacts on dental anxiety and its potential applicability in more invasive procedures. The quantifiable nature of the physiological improvements also provides a solid basis for developing standardized protocols for VR use in pediatric dentistry.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grisolia, B.M.; dos Santos, A.P.P.; Dhyppolito, I.M.; Buchanan, H.; Hill, K.; Oliveira, B.H. Prevalence of dental anxiety in children and adolescents globally: A systematic review with meta-analyses. Int. J. Paediatr. Dent. 2021, 31, 168–183. [Google Scholar] [CrossRef] [PubMed]
- Salcudean, A.; Lica, M.M. The Role of Systemic Family Psychotherapy in Glycemic Control for Children with Type 1 Diabetes. Children 2024, 11, 104. [Google Scholar] [CrossRef]
- Lerwick, J.L. Minimizing pediatric healthcare-induced anxiety and trauma. World J. Clin. Pediatr. 2016, 5, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Salcudean, A.; Osz, B.E.; Nan, A.G.; Sasu, A.B.; Cozma, M.M.; Tilinca, M.C.; Bocsak-Pop, A.R.; Strete, E.G. The efficacy of antidepresive treatment on COVID-19 pandemic-related depressive symptoms-A prospective, single-center, questionnaire-based study. Farmacia 2023, 71, 631–637. [Google Scholar] [CrossRef]
- Sălcudean, A.; Truşculescu, L.M.; Popovici, R.A.; Şerb, N.; Paşca, C.; Bodo, C.R.; Crăciun, R.E.; Olariu, I. Dental anxiety—A psychosocial cause affecting the quality of life—A systematic review. Rom. J. Oral Rehab. 2024, 4, 471–483. [Google Scholar]
- Pao, M.; Bosk, A. Anxiety in medically ill children/adolescents. Depress. Anxiety 2011, 28, 40–49. [Google Scholar] [CrossRef]
- Patni, T.; Lee, C.T.; Li, Y.; Kaste, S.; Zhu, L.; Sun, R.; Hudson, M.M.; Ness, K.K.; Neumann, A.; Robison, L.L. Factors for poor oral health in long-term childhood cancer survivors. BMC Oral Health 2023, 23, 73. [Google Scholar] [CrossRef]
- Foster, H.; Fitzgerald, J. Dental disease in children with chronic illness. Arch. Dis. Child. 2005, 90, 703–708. [Google Scholar] [CrossRef] [PubMed]
- Sălcudean, A.; Popovici, R.A.; Pitic, D.E.; Sârbu, D.; Boroghina, A.; Jomaa, M.; Salehi, M.A.; Kher, A.A.M.; Lica, M.M.; Bodo, C.R.; et al. Unraveling the Complex Interplay Between Neuroinflammation and Depression: A Comprehensive Review. Int. J. Mol. Sci. 2025, 26, 1645. [Google Scholar] [CrossRef]
- Cahyani, M.D.; Widyaningsih, V.; Prasetya, H.; Simatupang, N.A. Effect of “Tell Show Do” Method on Dental Anxiety in Pediatrics Dentistry: A Meta Analysis. Indones. J. Med. 2024, 9, 8–17. [Google Scholar] [CrossRef]
- Liu, Y.; Gu, Z.; Wang, Y.; Wu, Q.; Chen, V.; Xu, X.; Zhou, X. Effect of audiovisual distraction on the management of dental anxiety in children: A systematic review. Int. J. Paediatr. Dent. 2019, 29, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, B.; Erwood, K.; Ncomanzi, S.; Fischer, V.; O’Brien, D.; Lee, A. Management strategies for adult patients with dental anxiety in the dental clinic: A systematic review. Aust. Dent. J. 2022, 67 (Suppl. S1), S3–S13. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, S.G.; Kasch, C.; Pereira, B.; Barbosa, C.; Andreoli, G. The Risks versus the Benefits of Pharmacological Intervention in Social Anxiety Disorder in Children. Expert Rev. Neurother. 2025, 25, 299–310. [Google Scholar] [CrossRef]
- Strawn, J.R.; Welge, J.A.; Wehry, A.M.; Keeshin, B.; Rynn, M.A. Efficacy and tolerability of antidepressants in pediatric anxiety disorders: A systematic review and meta-analysis. Depress. Anxiety 2015, 32, 149–157. [Google Scholar] [CrossRef]
- Ghobadi, A.; Moradpoor, H.; Sharini, H.; Khazaie, H.; Moradpoor, P. The effect of virtual reality on reducing patients’ anxiety and pain during dental implant surgery. BMC Oral Health. 2024, 24, 186. [Google Scholar] [CrossRef]
- Wiederhold, M.D.; Gao, K.; Wiederhold, B.K. Clinical Use of Virtual Reality Distraction System to Reduce Anxiety and Pain in Dental Procedures. Cyberpsychol. Behav. Soc. Netw. 2014, 17, 359–365. [Google Scholar] [CrossRef]
- Vlad, T.; Trusculescu, L.-M.; Popovici, R.A.; Salcudean, A.; Bodo, C.R.; Csibi, S.; Folescu, R.N.; Olariu, I. The role of virtual reality therapy in dentistry: A bibliometric analysis of current trends and applications. Rom. J. Oral Rehabil. 2024, 16, 705–715. [Google Scholar] [CrossRef]
- Mouradian, W.E. Ethical principles and the delivery of children’s oral health care. Ambul. Pediatr. 2002, 2 (Suppl. S2), 162–168. [Google Scholar] [CrossRef]
- Suresh, L.R.; Shetty, V. Effect of Virtual Reality Distraction Method on the Level of Salivary Cortisol in Children with Autism Spectrum Disorder During Dental Treatment. J. Autism Dev. Disord. 2024, 55, 1–10. [Google Scholar] [CrossRef]
- Salcudean, A.; Strete, G.; Enatescu, V.R.; Tilinca, M.C.; Sasu, A.B.; Ceana, D.E.; Kiss, M.; Dumache, R.; ŐSZ, B.E.; Teodorescu, D.R.; et al. Pilot Study to evaluate adherence to treatment using the Mars Scale on a sample of Romanian patients with cardiovascular diseases. Farmacia 2024, 72, 66–77. [Google Scholar] [CrossRef]
- Constantini Leopardi, A.; Adanero Velasco, A.; Espí Mayor, M.; Miegimolle Herrero, M. Effectiveness of Virtual Reality Goggles as Distraction for Children in Dental Care—A Narrative Review. Appl. Sci. 2023, 13, 1307. [Google Scholar] [CrossRef]
- Imran, M.A.D.B.; Goh, C.S.Y.; Nisha, V.; Shanmugham, M.; Kuddoos, H.; Leo, C.H.; Rai, B. A Virtual Reality Game-Based Intervention to Enhance Stress Mindset and Performance among Firefighting Trainees from the Singapore Civil Defence Force (SCDF). Virtual Worlds 2024, 3, 256–269. [Google Scholar] [CrossRef]
- Kiș, A.M.; Negru, M.C.; Salcudean, A.; Marian, D.; Anca Lucoiu, A.; Pașca, M.D.; Popovici, R.A.; Olariu, I. From Diagnosis to Treatment: How Comunication Trans-Form Patient Care. Rom. J. Oral Rehabil. 2025, 17, 825–834. [Google Scholar]
- Alabduljabbar, R.; Almutawa, M.; Alkathiri, R.; Alqahtani, A.; Alshamlan, H. An Interactive Augmented and Virtual Reality System for Managing Dental Anxiety among Young Patients: A Pilot Study. Appl. Sci. 2023, 13, 5603. [Google Scholar] [CrossRef]
- Al Kheraif, A.A.; Adam, T.R.; Wasi, A.; Alhassoun, R.K.; Haddadi, R.M.; Alnamlah, M. Impact of Virtual Reality Intervention on Anxiety and Level of Cooperation in Children and Adolescents with Autism Spectrum Disorder during the Dental Examination. J. Clin. Med. 2024, 13, 6093. [Google Scholar] [CrossRef] [PubMed]
- Hutson, J. Social Virtual Reality: Neurodivergence and Inclusivity in the Metaverse. Societies 2022, 12, 102. [Google Scholar] [CrossRef]
- Rosa, A.; Pujia, A.M.; Docimo, R.; Arcuri, C. Managing Dental Phobia in Children with the Use of Virtual Reality: A Systematic Review of the Current Literature. Children 2023, 10, 1763. [Google Scholar] [CrossRef]
- Belengeanu, V.; Marian, D.; Hosszu, T.; Ogodescu, A.S.; Belengeanu, A.D.; Samoilă, C.; Popa, C.; Duma, O.; Caba, L.; Popescu, R.; et al. A comprehensive evaluation of an OFDI syndrome from child to teenager. Rom. J. Morphol. Embryol. Rev. Roum. Morphol. Embryol. 2019, 60, 697–706. [Google Scholar]
- Gómez-Polo, C.; Vilches, A.A.; Ribas, D.; Castaño-Séiquer, A.; Montero, J. Behaviour and Anxiety Management of Paediatric Dental Patients through Virtual Reality: A Randomised Clinical Trial. J. Clin. Med. 2021, 10, 3019. [Google Scholar] [CrossRef]
- Melzack, R.; Wall, P.D. Pain mechanisms: A new theory. Science 1967, 11, 89–90. [Google Scholar]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical Power Analyses Using G*Power 3.1: Tests for Correlation and Regression Analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Norman, G.R.; Sloan, J.A.; Wyrwich, K.W. Interpretation of Changes in Health-related Quality of Life: The Remarkable Universality of Half a Standard Deviation. Med. Care 2003, 41, 582. [Google Scholar] [CrossRef] [PubMed]
- Tsze, D.S.; Hirschfeld, G.; von Baeyer, C.L.; Suarez, L.E.; Dayan, P.S. Changes in Pain Score Associated with Clinically Meaningful Outcomes in Children with Acute Pain. Acad. Emerg. Med. 2019, 26, 1002–1013. [Google Scholar] [CrossRef] [PubMed]
- IBM Corp. IBM SPSS Statistics for Windows, Version 22.0; IBM Corp.: Armonk, NY, USA, 2013.
- American Psychological Association. Publication Manual of the American Psychological Association: The Official Guide to APA Style, Seventh Edition; American Psychological Association: Washington, DC, USA, 2020. [Google Scholar]
- Romero-Ayuso, D.; Toledano-González, A.; Rodríguez-Martínez Mdel, C.; Arroyo-Castillo, P.; Triviño-Juárez, J.M.; González, P.; Ariza-Vega, P.; González, A.D.P.; Segura-Fragoso, A. Effectiveness of Virtual Reality-Based Interventions for Children and Adolescents with ADHD: A Systematic Review and Meta-Analysis. Children 2021, 8, 70. [Google Scholar] [CrossRef]
- Lica, M.M.; Papai, A.; Salcudean, A.; Crainic, M.; Covaciu, C.G.; Mihai, A. Assessment of Psychopathology in Adolescents with Insulin-Dependent Diabetes (IDD) and the Impact on Treatment Management. Children 2021, 8, 414. [Google Scholar] [CrossRef]
- Comparcini, D.; Simonetti, V.; Galli, F.; Saltarella, I.; Altamura, C.; Tomietto, M.; Desaphy, J.-F.; Cicolini, G. Immersive and Non-Immersive Virtual Reality for Pain and Anxiety Management in Pediatric Patients with Hematological or Solid Cancer: A Systematic Review. Cancers 2023, 15, 985. [Google Scholar] [CrossRef] [PubMed]
- Gilboa Pras, Y.; Indursky, A.; Gilboa Pras, S.; Schaffer, O.; Niazov, E.; Zmora, O. Infectious Diseases-Approved Virtual Reality Goggles for Common Procedures in Pediatric Surgical Patients. J. Clin. Med. 2024, 13, 5572. [Google Scholar] [CrossRef]
- Tsolakis, I.A.; Gizani, S.; Panayi, N.; Antonopoulos, G.; Tsolakis, A.I. Three-Dimensional Printing Technology in Orthodontics for Dental Models: A Systematic Review. Children 2022, 9, 1106. [Google Scholar] [CrossRef]
- Valls-Esteve, A.; Adell-Gómez, N.; Pasten, A.; Barber, I.; Munuera, J.; Krauel, L. Exploring the Potential of Three-Dimensional Imaging, Printing, and Modeling in Pediatric Surgical Oncology: A New Era of Precision Surgery. Children 2023, 10, 832. [Google Scholar] [CrossRef]
- Maresca, G.; Leonardi, S.; De Cola, M.C.; Giliberto, S.; Di Cara, M.; Corallo, F.; Quartarone, A.; Pidalà, A. Use of Virtual Reality in Children with Dyslexia. Children 2022, 9, 1621. [Google Scholar] [CrossRef]
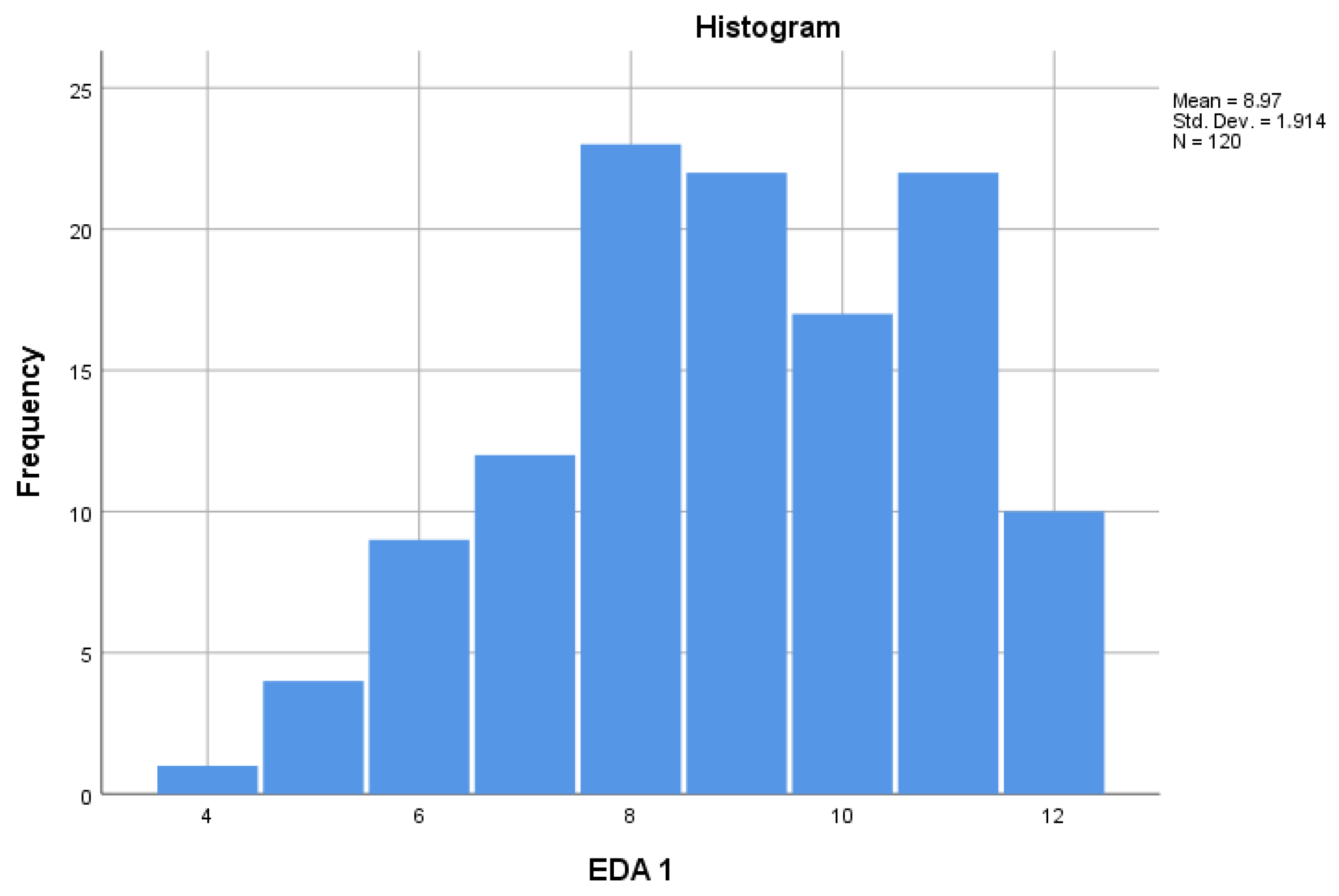
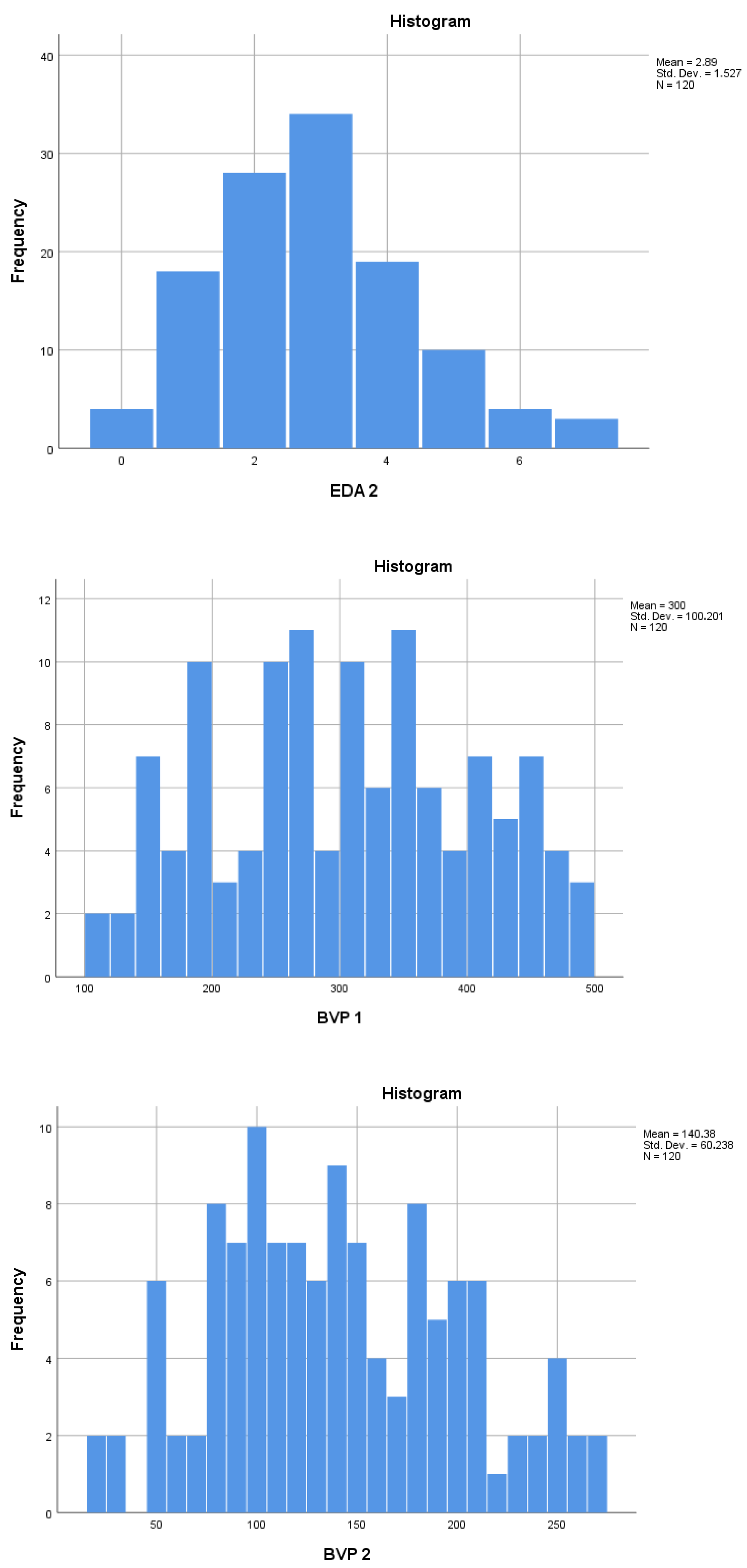
| Mean | N | Std. Deviation | Std. Error Mean | ||
|---|---|---|---|---|---|
| Pair 1 | EDA 1 No-VR | 8.97 | 120 | 1.914 | 0.175 |
| EDA 2 VR | 2.89 | 120 | 1.527 | 0.139 | |
| Pair 2 | BVP 1 No-VR | 300.00 | 120 | 100.201 | 9.147 |
| BVP 2 VR | 140.38 | 120 | 60.238 | 5.499 | |
| Paired Differences | t | df | Sig. (2-Tailed) | Cohen’s d | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Std. Deviation | Std. Error Mean | 95% Confidence Interval of the Difference | |||||||
| Lower | Upper | |||||||||
| Pair 1 | EDA 1–EDA 2 | 6.07 | 1.58 | 0.14 | −3.84 | 6.36 | 42.03 | 119 | 0.00 | −3.84 |
| Pair 2 | BVP 1–BVP 2 | 159.62 | 57.55 | 5.25 | −2.77 | 170.02 | 30.38 | 119 | 0.00 | −2.77 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trusculescu, L.-M.; Pitic, D.E.; Sălcudean, A.; Popovici, R.A.; Forna, N.; Badoiu, S.C.; Enache, A.; Enasoni, S.; Kiș, A.; Cosoroabă, R.M.; et al. Virtual Reality as a Non-Pharmacological Aid for Reducing Anxiety in Pediatric Dental Procedures. Children 2025, 12, 930. https://doi.org/10.3390/children12070930
Trusculescu L-M, Pitic DE, Sălcudean A, Popovici RA, Forna N, Badoiu SC, Enache A, Enasoni S, Kiș A, Cosoroabă RM, et al. Virtual Reality as a Non-Pharmacological Aid for Reducing Anxiety in Pediatric Dental Procedures. Children. 2025; 12(7):930. https://doi.org/10.3390/children12070930
Chicago/Turabian StyleTrusculescu, Laria-Maria, Dana Emanuela Pitic, Andreea Sălcudean, Ramona Amina Popovici, Norina Forna, Silviu Constantin Badoiu, Alexandra Enache, Sorina Enasoni, Andreea Kiș, Raluca Mioara Cosoroabă, and et al. 2025. "Virtual Reality as a Non-Pharmacological Aid for Reducing Anxiety in Pediatric Dental Procedures" Children 12, no. 7: 930. https://doi.org/10.3390/children12070930
APA StyleTrusculescu, L.-M., Pitic, D. E., Sălcudean, A., Popovici, R. A., Forna, N., Badoiu, S. C., Enache, A., Enasoni, S., Kiș, A., Cosoroabă, R. M., Talpos-Niculescu, C. I., Zeicu, C. C., Cozma, M.-M., & Todor, L. (2025). Virtual Reality as a Non-Pharmacological Aid for Reducing Anxiety in Pediatric Dental Procedures. Children, 12(7), 930. https://doi.org/10.3390/children12070930










