Addressing Stunting in Children Under Five: Insights and Opportunities from Nepal, Bangladesh, and Vietnam—A Review of Literature
Abstract
1. Introduction
2. Methods
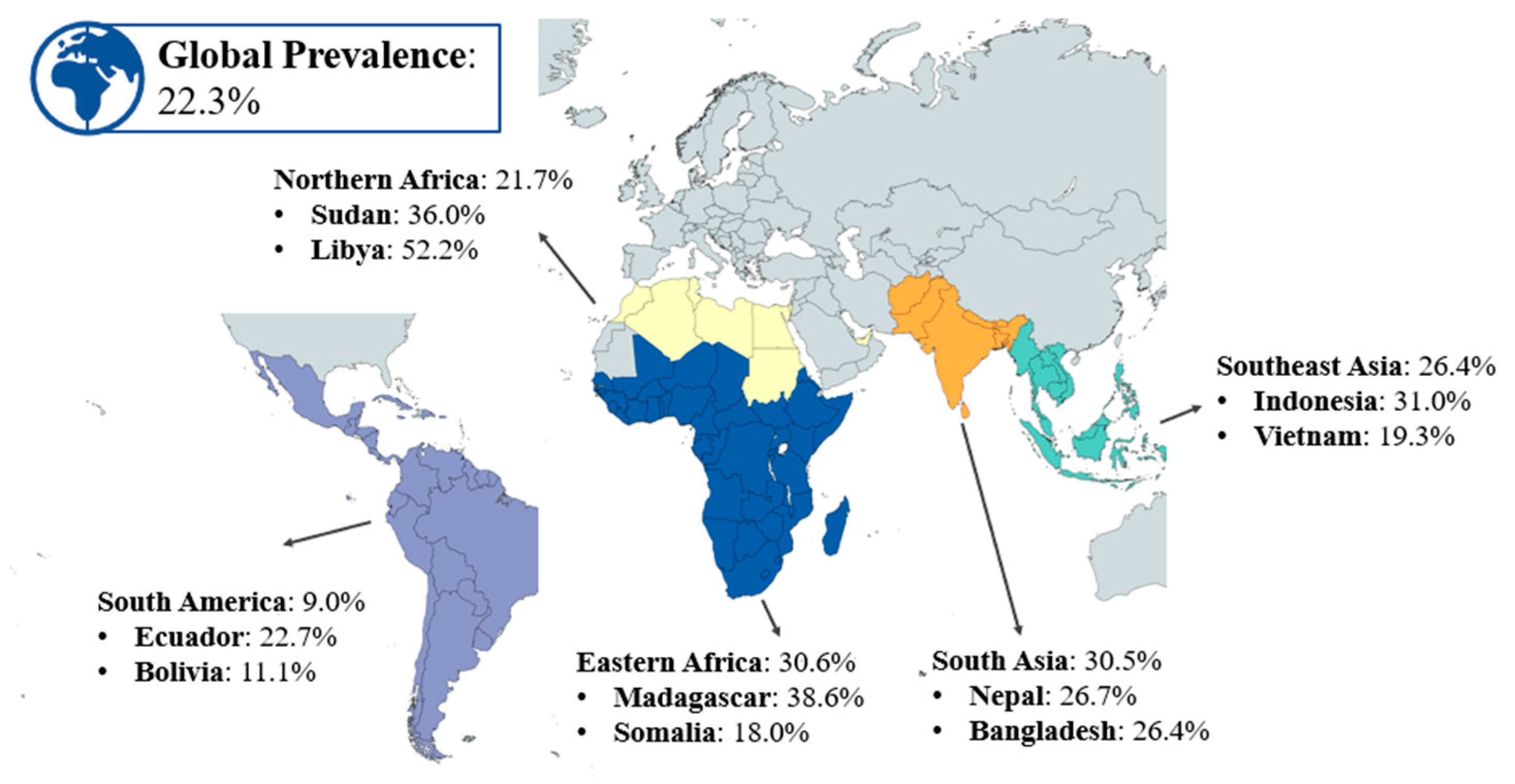
3. Results and Discussion
3.1. Search Results and Included Articles
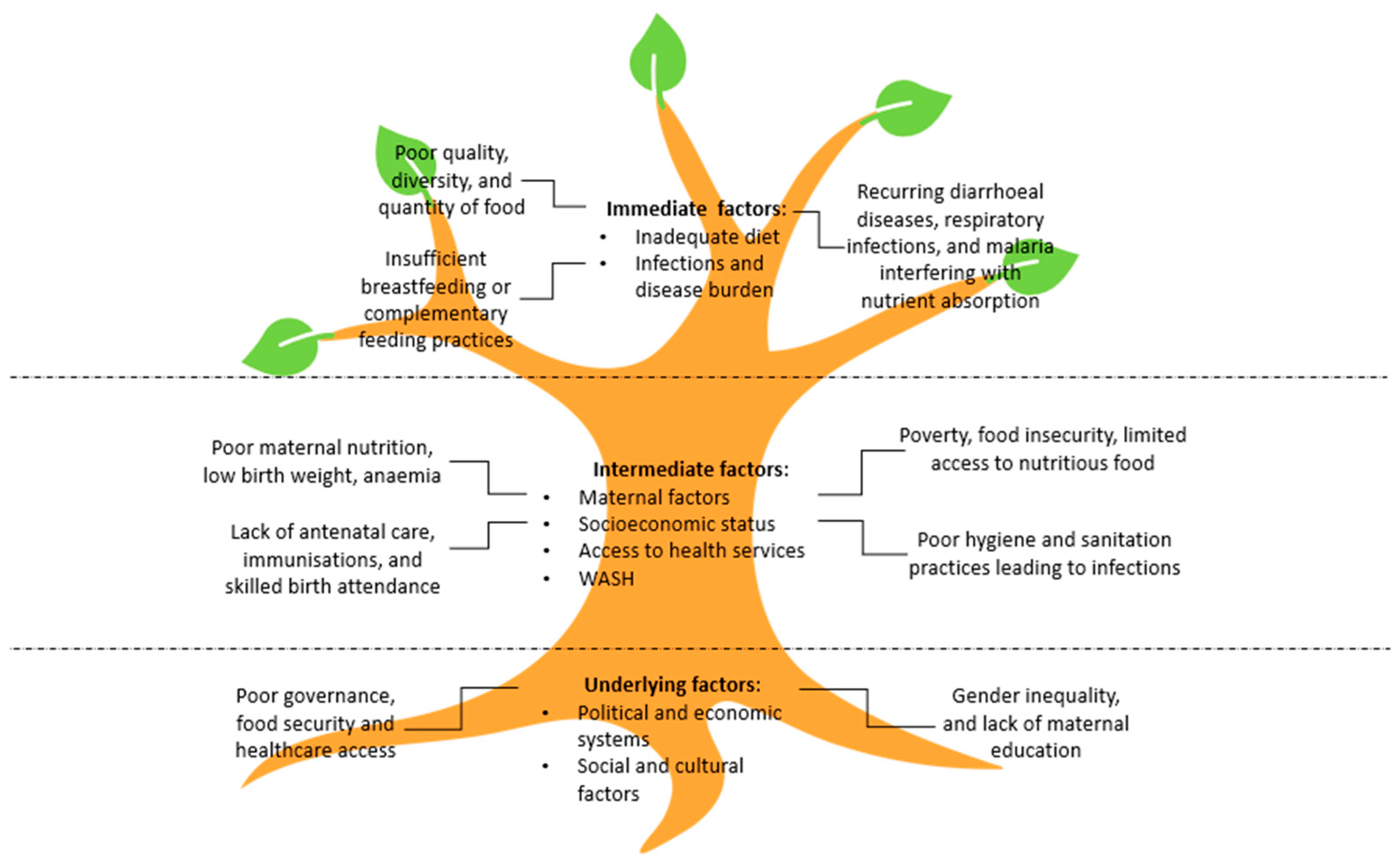
3.2. Determinants of Stunting
3.3. Underlying Factors
3.4. Intermediate Factors
3.5. Immediate Factors
3.6. Children at Risk of Stunting
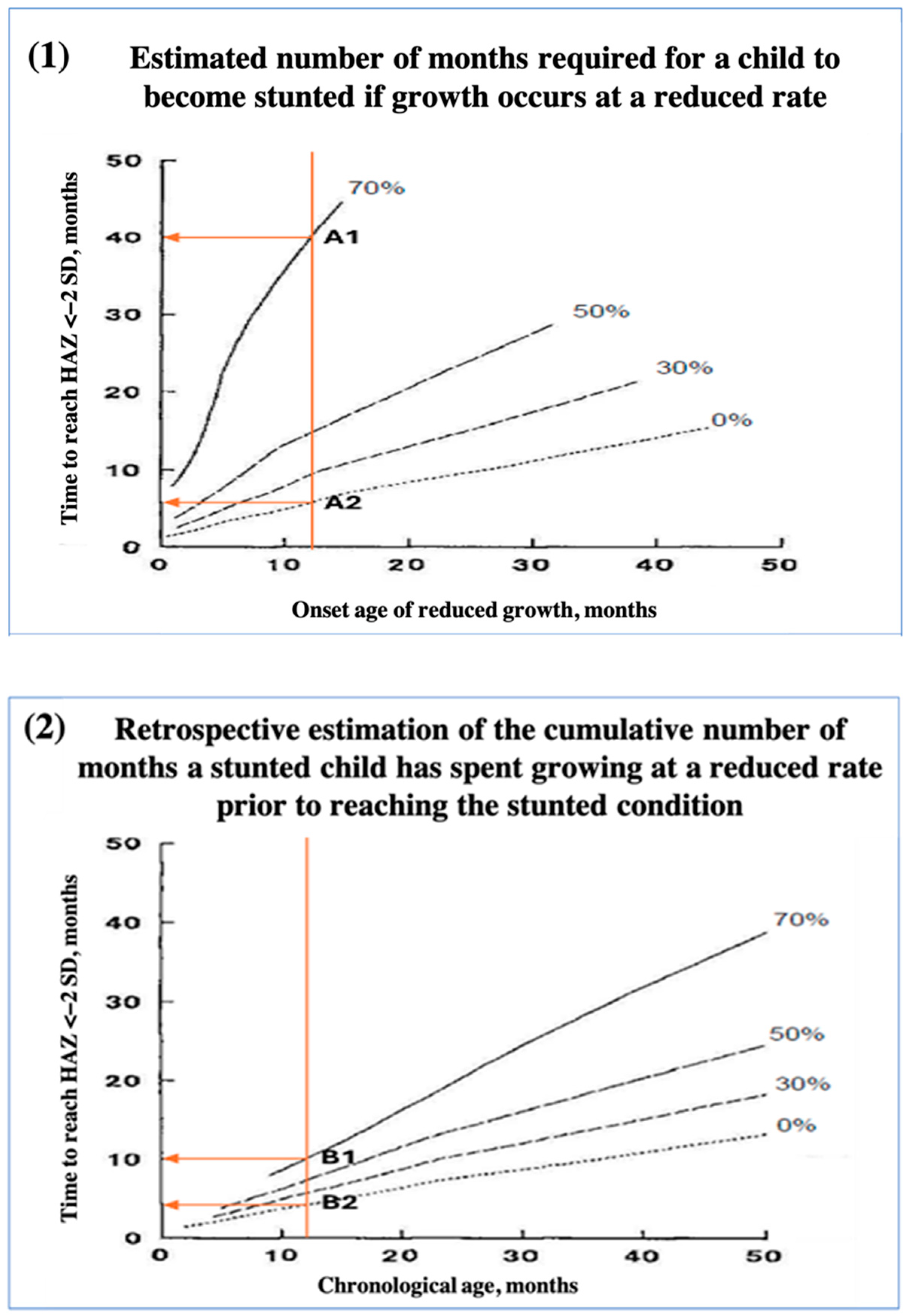
3.6.1. Faltering Growth
3.6.2. Wasting
3.7. Dynamics of Stunted Growth in Children
3.8. Window of Opportunity
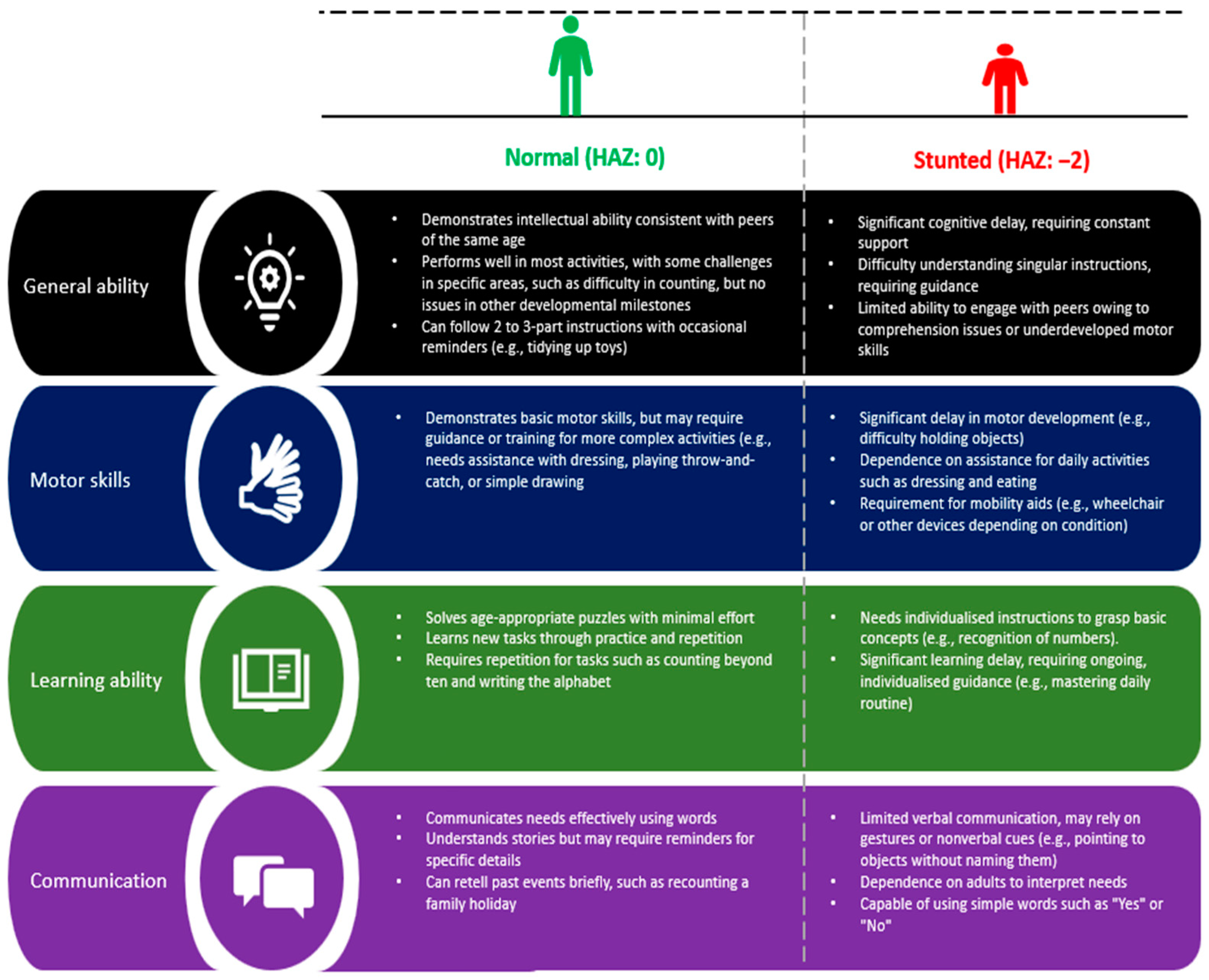
3.9. Consequences of Stunting on Cognitive Function and Human Capital
4. Insights from High-Performing LMICs
4.1. Stunting Prevalence and Progress in LMICs
4.2. Multisystem Approach to Combat Stunting
4.3. Country-Specific Approaches to Stunting Reduction
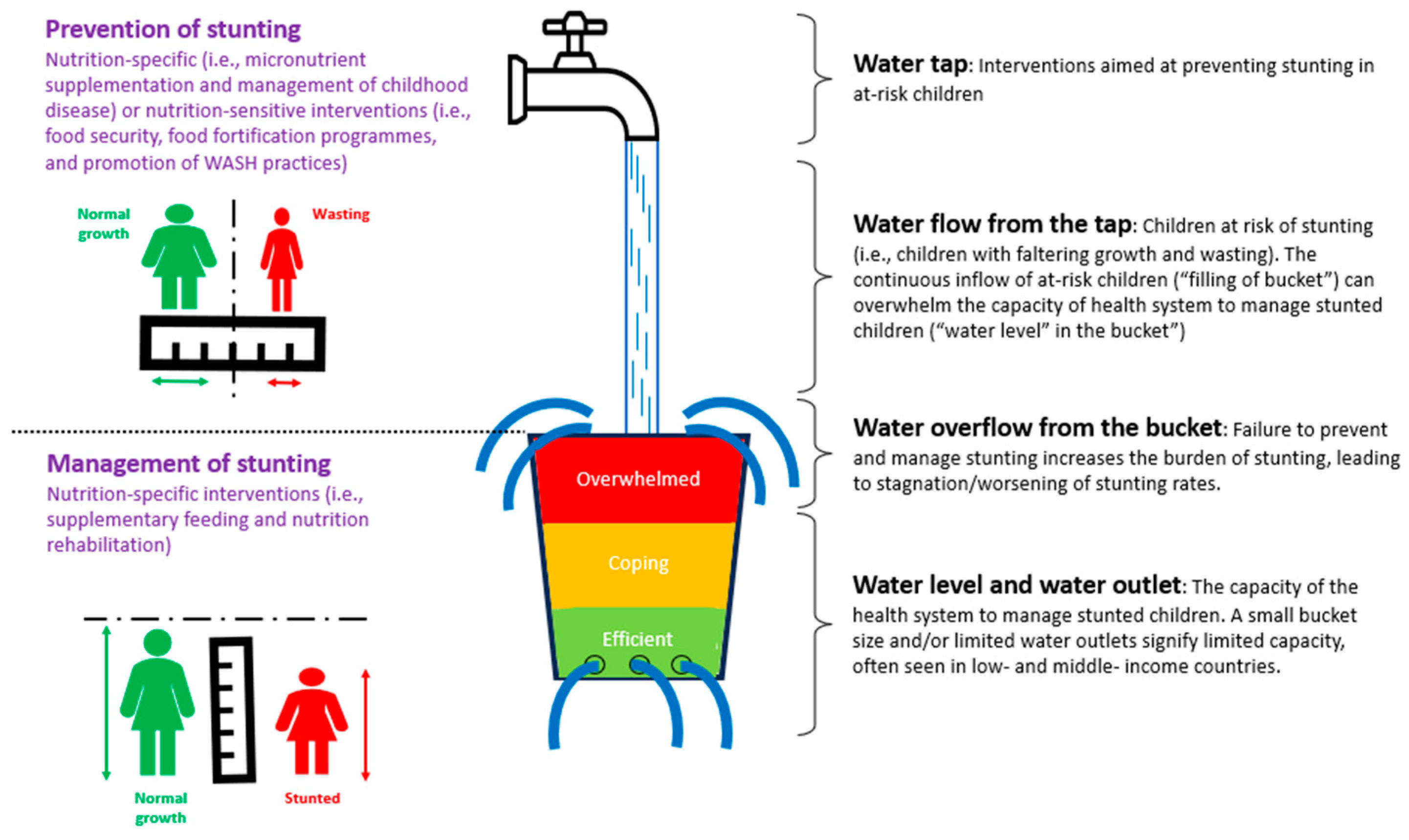
5. Approaches to Managing Stunted Children
6. Suggested Interventions Addressing the Determinants of Stunting
6.1. Underlying Determinants (Socioeconomic Factors)
6.2. Intermediate Determinants (Health, Environment, and Community Factors)
6.3. Immediate Determinants (Nutrition and Health Factors)
7. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Tanner, J.M. Normal growth and techniques of growth assessment. Clin. Endocrinol. Metab. 1986, 15, 411–451. [Google Scholar] [CrossRef] [PubMed]
- Jelenkovic, A.; Sund, R.; Hur, Y.M.; Yokoyama, Y.; Hjelmborg, J.V.; Moller, S.; Honda, C.; Magnusson, P.K.; Pedersen, N.L.; Ooki, S.; et al. Genetic and environmental influences on height from infancy to early adulthood: An individual-based pooled analysis of 45 twin cohorts. Sci. Rep. 2016, 6, 28496. [Google Scholar] [CrossRef] [PubMed]
- Cohen, P.; Rogol, A.D.; Deal, C.L.; Saenger, P.; Reiter, E.O.; Ross, J.L.; Chernausek, S.D.; Savage, M.O.; Wit, J.M. Consensus statement on the diagnosis and treatment of children with idiopathic short stature: A summary of the Growth Hormone Research Society, the Lawson Wilkins Pediatric Endocrine Society, and the European Society for Paediatric Endocrinology Workshop. J. Clin. Endocrinol. Metab. 2008, 93, 4210–4217. [Google Scholar] [CrossRef] [PubMed]
- Grigoletto, V.; Occhipinti, A.A.; Pellegrin, M.C.; Sirchia, F.; Barbi, E.; Tornese, G. Definition and prevalence of familial short stature. Ital. J. Pediatr. 2021, 47, 56. [Google Scholar] [CrossRef]
- Insider, B. Average Human Height by Country. Available online: https://en.wikipedia.org/wiki/Average_human_height_by_country (accessed on 5 January 2025).
- Adair, L.S. Long-term consequences of nutrition and growth in early childhood and possible preventive interventions. Nestle Nutr. Inst. Workshop Ser. 2014, 78, 111–120. [Google Scholar] [CrossRef]
- Wallerich, L.; Fillol, A.; Rivadeneyra, A.; Vandentorren, S.; Wittwer, J.; Cambon, L. Environment and child well-being: A scoping review of reviews to guide policies. Health Promot. Perspect. 2023, 13, 168–182. [Google Scholar] [CrossRef]
- Prendergast, A.J.; Humphrey, J.H. The stunting syndrome in developing countries. Paediatr. Int. Child. Health 2014, 34, 250–265. [Google Scholar] [CrossRef]
- Robinson, P.N.; Arteaga-Solis, E.; Baldock, C.; Collod-Beroud, G.; Booms, P.; De Paepe, A.; Dietz, H.C.; Guo, G.; Handford, P.A.; Judge, D.P.; et al. The molecular genetics of Marfan syndrome and related disorders. J. Med. Genet. 2006, 43, 769–787. [Google Scholar] [CrossRef]
- Giustina, A.; Mazziotti, G.; Canalis, E. Growth hormone, insulin-like growth factors, and the skeleton. Endocr. Rev. 2008, 29, 535–559. [Google Scholar] [CrossRef]
- Mullur, R.; Liu, Y.Y.; Brent, G.A. Thyroid hormone regulation of metabolism. Physiol. Rev. 2014, 94, 355–382. [Google Scholar] [CrossRef]
- Rogol, A.D.; Clark, P.A.; Roemmich, J.N. Growth and pubertal development in children and adolescents: Effects of diet and physical activity. Am. J. Clin. Nutr. 2000, 72, 521S–528S. [Google Scholar] [CrossRef] [PubMed]
- Hvidt, J.J.; Brix, N.; Ernst, A.; Lauridsen, L.L.B.; Ramlau-Hansen, C.H. Size at birth, infant growth, and age at pubertal development in boys and girls. Clin. Epidemiol. 2019, 11, 873–883. [Google Scholar] [CrossRef]
- Gohlke, B.C.; Bettendorf, M.; Binder, G.; Hauffa, B.; Reinehr, T.; Dorr, H.G.; Wolfle, J. Effect of Psychosocial Factors on Growth. Klin. Padiatr. 2022, 234, 61–67. [Google Scholar] [CrossRef]
- Daelmans, B.; Manji, S.A.; Raina, N. Nurturing Care for Early Childhood Development: Global Perspective and Guidance. Indian Pediatr. 2021, 58 (Suppl. 1), S11–S15. [Google Scholar] [CrossRef] [PubMed]
- Gao, Z.; Chen, S.; Sun, H.; Wen, X.; Xiang, P. Physical activity in children’s health and cognition. BioMed Res. Int. 2018, 2018, 8542403. [Google Scholar] [CrossRef]
- Alves, J.G.B.; Alves, G.V. Effects of physical activity on children’s growth. J. Pediatr. 2019, 95, S72–S78. [Google Scholar] [CrossRef]
- Zaffanello, M.; Pietrobelli, A.; Cavarzere, P.; Guzzo, A.; Antoniazzi, F. Complex relationship between growth hormone and sleep in children: Insights, discrepancies, and implications. Front. Endocrinol. 2023, 14, 1332114. [Google Scholar] [CrossRef] [PubMed]
- Sinha, P.; Guerrant, R.L. The Costly Vicious Cycle of Infections and Malnutrition. J. Infect. Dis. 2024, 229, 1611–1613. [Google Scholar] [CrossRef]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Womack, S.R.; Beam, C.R.; Giangrande, E.J.; Scharf, R.J.; Tong, X.; Ponnapalli, M.; Davis, D.W.; Turkheimer, E. Nonlinear Catch-Up Growth in Height, Weight, and Head Circumference from Birth to Adolescence: A Longitudinal Twin Study. Behav. Genet. 2023, 53, 385–403. [Google Scholar] [CrossRef]
- de Onis, M.; Branca, F. Childhood stunting: A global perspective. Matern. Child Nutr. 2016, 12 (Suppl. 1), 12–26. [Google Scholar] [CrossRef] [PubMed]
- Van Beekum, M.; Berger, J.; Van Geystelen, J.; Hondru, G.; Som, S.V.; Theary, C.; Laillou, A.; Poirot, E.; Bork, K.A.; Wieringa, F.T.; et al. The associations between stunting and wasting at 12 months of age and developmental milestones delays in a cohort of Cambodian children. Sci. Rep. 2022, 12, 17859. [Google Scholar] [CrossRef] [PubMed]
- Crookston, B.T.; Schott, W.; Cueto, S.; Dearden, K.A.; Engle, P.; Georgiadis, A.; Lundeen, E.A.; Penny, M.E.; Stein, A.D.; Behrman, J.R. Postinfancy growth, schooling, and cognitive achievement: Young Lives. Am. J. Clin. Nutr. 2013, 98, 1555–1563. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Data Prevalence on Stunting in Children Under 5. Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/gho-jme-stunting-prevalence (accessed on 5 January 2025).
- Liu, Q.; Long, Q.; Garner, P. Growth monitoring and promotion (GMP) for children in low and middle income countries. Cochrane Database Syst. Rev. 2017, 2017, CD010102. [Google Scholar] [CrossRef]
- Kuwabara, R.; Urakami, T. Importance of growth monitoring by a health checkup in detecting growth disorders in young children. Biomed. J. Sci. Tech. Res. 2018, 11, 8489–8491. [Google Scholar]
- Haymond, M.; Kappelgaard, A.M.; Czernichow, P.; Biller, B.M.; Takano, K.; Kiess, W.; Global Advisory Panel Meeting on the Effects of Growth Hormone. Early recognition of growth abnormalities permitting early intervention. Acta Paediatr. 2013, 102, 787–796. [Google Scholar] [CrossRef]
- UNICEF; WHO. UNICEF-WHO-The World Bank: Joint Child Malnutrition Estimates (JME)—Levels and Trends, 2023 ed.; WHO: Geneva, Switzerland, 2023. [Google Scholar]
- Report, G.N. Country Nutrition Profiles Nepal. Available online: https://globalnutritionreport.org/resources/nutrition-profiles/ (accessed on 24 December 2024).
- UNICEF. UNICEF Conceptual Framework on Maternal and Child Nutrition. 2020. Available online: https://www.unicef.org/media/113291/file/UNICEF%20Conceptual%20Framework.pdf (accessed on 18 May 2022).
- Alaoui, E.H. Socio-Economic Inequalities, Gender and Malnutrition in Developing Countries. Ph.D. Thesis, Université de Bordeaux, Talence, France, 2023. [Google Scholar]
- Mandara, F.; Festo, C.; Killel, E.; Lwambura, S.; Mrema, J.; Katunzi, F.; Martin, H.D.; Elisaria, E. The relationship between feeding practices and stunting among children under two years in Tanzania mainland: A mixed-method approach. Bull. Natl. Res. Cent. 2024, 48, 112. [Google Scholar] [CrossRef]
- Raman, S.; Napier-Raman, S.; Pinzón-Segura, M.C. Exploring cultural influences in perinatal and early childhood nutrition. Rev. Salud Pública 2024, 26, 115569. [Google Scholar] [CrossRef]
- Sjarif, D.R.; Yuliarti, K.; Iskandar, W.J. Daily consumption of growing-up milk is associated with less stunting among Indonesian toddlers. Med. J. Indones. 2019, 28, 70–76. [Google Scholar] [CrossRef]
- Ballard, O.; Morrow, A.L. Human milk composition: Nutrients and bioactive factors. Pediatr. Clin. N. Am. 2013, 60, 49–74. [Google Scholar] [CrossRef]
- UNICEF. Nutrition Strategic Direction 2030—North, Middle and East Africa Region; UNICEF: New York, NY, USA, 2024. [Google Scholar]
- Cooke, R.; Goulet, O.; Huysentruyt, K.; Joosten, K.; Khadilkar, A.V.; Mao, M.; Meyer, R.; Prentice, A.M.; Singhal, A. Catch-Up Growth in Infants and Young Children With Faltering Growth: Expert Opinion to Guide General Clinicians. J. Pediatr. Gastroenterol. Nutr. 2023, 77, 7–15. [Google Scholar] [CrossRef]
- Grantham-McGregor, S.; Cheung, Y.B.; Cueto, S.; Glewwe, P.; Richter, L.; Strupp, B. Developmental potential in the first 5 years for children in developing countries. Lancet 2007, 369, 60–70. [Google Scholar] [CrossRef]
- Mertens, A.; Benjamin-Chung, J.; Colford Jr, J.M.; Hubbard, A.E.; van der Laan, M.J.; Coyle, J.; Sofrygin, O.; Cai, W.; Jilek, W.; Rosete, S. Child wasting and concurrent stunting in low-and middle-income countries. Nature 2023, 621, 558–567. [Google Scholar] [CrossRef] [PubMed]
- Thurstans, S.; Sessions, N.; Dolan, C.; Sadler, K.; Cichon, B.; Isanaka, S.; Roberfroid, D.; Stobaugh, H.; Webb, P.; Khara, T. The relationship between wasting and stunting in young children: A systematic review. Matern. Child. Nutr. 2022, 18, e13246. [Google Scholar] [CrossRef]
- UNICEF. Severe Wasting: An Overlooked Child Survival Emergency. UNICEF Child Alert Report. 2022. Available online: https://www.unicef.org/media/120346/file/Wasting%20child%20alert.pdf (accessed on 27 March 2025).
- Golden, M.H.N. Is complete catch-up possible for stunted malnourished children? Eur. J. Clin. Nutr. 1994, 48, 58–71. [Google Scholar]
- Cheung, Y.B. Growth and cognitive function of Indonesian children: Zero-inflated proportion models. Stat. Med. 2006, 25, 3011–3022. [Google Scholar] [CrossRef]
- Alam, M.A.; Richard, S.A.; Fahim, S.M.; Mahfuz, M.; Nahar, B.; Das, S.; Shrestha, B.; Koshy, B.; Mduma, E.; Seidman, J.C. Impact of early-onset persistent stunting on cognitive development at 5 years of age: Results from a multi-country cohort study. PLoS ONE 2020, 15, e0227839. [Google Scholar]
- Ekholuenetale, M.; Barrow, A.; Ekholuenetale, C.E.; Tudeme, G. Impact of stunting on early childhood cognitive development in Benin: Evidence from Demographic and Health Survey. Egypt. Pediatr. Assoc. Gaz. 2020, 68, 31. [Google Scholar] [CrossRef]
- Hoddinott, J.; Behrman, J.R.; Maluccio, J.A.; Melgar, P.; Quisumbing, A.R.; Ramirez-Zea, M.; Stein, A.D.; Yount, K.M.; Martorell, R. Adult consequences of growth failure in early childhood123. Am. J. Clin. Nutr. 2013, 98, 1170–1178. [Google Scholar] [CrossRef]
- Akseer, N.; Tasic, H.; Onah, M.N.; Wigle, J.; Rajakumar, R.; Sanchez-Hernandez, D.; Akuoku, J.; Black, R.E.; Horta, B.L.; Nwuneli, N. Economic costs of childhood stunting to the private sector in low-and middle-income countries. EClinicalMedicine 2022, 45, 101320. [Google Scholar] [CrossRef]
- Vaivada, T.; Akseer, N.; Akseer, S.; Somaskandan, A.; Stefopulos, M.; Bhutta, Z.A. Stunting in childhood: An overview of global burden, trends, determinants, and drivers of decline. Am. J. Clin. Nutr. 2020, 112, 777S–791S. [Google Scholar] [CrossRef] [PubMed]
- Report, G.N. Country Nutrition Profiles Bangladesh. Available online: https://globalnutritionreport.org/resources/nutrition-profiles/asia/southern-asia/bangladesh/ (accessed on 5 January 2025).
- Report, G.N. Country Nutrition Profiles Vietnam. Available online: https://globalnutritionreport.org/resources/nutrition-profiles/asia/south-eastern-asia/viet-nam/ (accessed on 5 January 2025).
- Erlyn, P.; Hidayat, B.; Fatoni, A.; Saksono, H. Nutritional interventions by local governments as an effort to accelerate stunting reduction. J. Bina Praja 2021, 13, 543–553. [Google Scholar] [CrossRef]
- Ruel, M.T.; Alderman, H. Nutrition-sensitive interventions and programmes: How can they help to accelerate progress in improving maternal and child nutrition? Lancet 2013, 382, 536–551. [Google Scholar] [CrossRef]
- Budhathoki, S.S.; Bhandari, A.; Gurung, R.; Gurung, A.; Kc, A. Stunting among under 5-year-olds in Nepal: Trends and risk factors. Matern. Child. Health J. 2020, 24, 39–47. [Google Scholar] [CrossRef] [PubMed]
- FAO. Multi-Sector Nutrition Plan for Accelerating the Reduction of Maternal and Child Under-Nutrition in Nepal 2013–2017. Available online: https://www.fao.org/faolex/results/details/en/c/LEX-FAOC143047/ (accessed on 11 February 2025).
- Exemplars in Global Health. What Nepal Do. Available online: https://www.exemplars.health/topics/stunting/nepal/what-did-nepal-do (accessed on 11 February 2025).
- Siddiqui, M.Z.; Illiyan, A.; Akram, V.; Nigar, K. Revisiting swimming against tide; inequalities in child malnutrition in Nepal. Discov. Glob. Soc. 2024, 2, 26. [Google Scholar] [CrossRef]
- Namirembe, G.; Shrestha, R.; Mezzano, J.; Ausman, L.M.; Davis, D.; Baral, K.; Ghosh, S.; Shively, G.; Webb, P. Effective nutrition governance is correlated with better nutrition outcomes in Nepal. BMC Pediatr. 2021, 21, 434. [Google Scholar] [CrossRef]
- Adhikari, N.; Adhikari, M.; Shrestha, N.; Pradhananga, P.; Poudel, B.; Dhungel, S.; Joshi, P.C.; Ide, N.; Sharma, G.N.; Shrestha, A. Nutrition and food security in Nepal: A narrative review of policies. Nutr. Rev. 2023, 81, 1612–1625. [Google Scholar] [CrossRef] [PubMed]
- Choufani, J.; Jamaluddine, Z.; Cunningham, K. A multisectoral nutrition program in Nepal improves knowledge of dietary diversity, sick child feeding, and handwashing, but not all practices: A program impact pathways mediation analysis. Curr. Dev. Nutr. 2020, 4, nzz135. [Google Scholar] [CrossRef]
- Islam, M.R.; Rahman, M.S.; Rahman, M.M.; Nomura, S.; De Silva, A.; Lanerolle, P.; Jung, J.; Rahman, M.M. Reducing childhood malnutrition in Bangladesh: The importance of addressing socio-economic inequalities. Public Health Nutr. 2020, 23, 72–82. [Google Scholar] [CrossRef]
- Nisbett, N.; Davis, P.; Yosef, S.; Akhtar, N. Bangladesh’s story of change in nutrition: Strong improvements in basic and underlying determinants with an unfinished agenda for direct community level support. Glob. Food Secur. 2017, 13, 21–29. [Google Scholar] [CrossRef]
- Shamim, A.A.; Mistry, S.K.; Irfan, N.M. A Study to Identify the Research Gaps for Effective Implementation of the Second National Plan of Action for Nutrition (NPAN2) in Bangladesh; Bangladesh National Nutrition Council, Governemnt of the People’s Republic: Dhaka, Bangladesh, 2019.
- Reliefweb. JANO’s Nutrition Governance Approach—Multi-Sectoral, Multi-Level and Multi-Stakeholder. Available online: https://reliefweb.int/report/bangladesh/janos-nutrition-governance-approach-multi-sectoral-multi-level-and-multi-stakeholder (accessed on 14 February 2025).
- Anh, N.T.N. Hunger Eradication and Poverty Reduction in Vietnam: Achievements and Challenges. 2015. Available online: https://www.freiheit.org/vietnam/report-vietnam-hunger-eradication-and-poverty-reduction-vietnam-achievements-and-challenges (accessed on 5 January 2025).
- Hall, A.; Hanh, T.T.M.; Farley, K.; Quynh, T.P.N.; Valdivia, F. An evaluation of the impact of a school nutrition programme in Vietnam. Public Health Nutr. 2007, 10, 819–826. [Google Scholar] [CrossRef] [PubMed]
- Phu, P.V.; Hoan, N.V.; Salvignol, B.; Treche, S.; Wieringa, F.T.; Dijkhuizen, M.A.; Khan, N.C.; Tuong, P.D.; Schwartz, H.; Berger, J. A six-month intervention with two different types of micronutrient-fortified complementary foods had distinct short-and long-term effects on linear and ponderal growth of Vietnamese infants. J. Nutr. 2012, 142, 1735–1740. [Google Scholar] [CrossRef]
- Rocha, C.; Yeudall, F.; Moraes, A.; Yuan, Y.; Tenkate, T.; Mendonça, M.; Duong, V.D.; Do Huy, N.; Huyn, P.; Bao Hoa, D.T. Scaling Up Small-Scale Food Processing for Therapeutic and Complementary Foods for Children in Vietnam; Canadian International Food Security Research Fund Project Story: Ottawa, ON, Canada, 2018. [Google Scholar]
- Joshi, G.; Chitekwe, S. A Road Map to Nepal’s Multi Sector Nutrition Plan (MSNP) II 2018–2022. 2019. Available online: https://scalingupnutrition.org/sites/default/files/2021-12/A-Road-Map-to-MSNP-II-in-Nepal.pdf (accessed on 5 January 2025).
- Joshi, A.; Marasini, S.; Sharma, S.; Paneru, B.; Kunwar, S.; Shrestha, A.; Shrestha, A.; Karmacharya, B.M. Scope of work and contributions of female community health volunteers in Nepal’s healthcare sector: A qualitative study. BMJ Open 2024, 14, e082363. [Google Scholar] [CrossRef] [PubMed]
- Ruducha, J.; Bhatia, A.; Mann, C.; Torlesse, H. Multisectoral nutrition planning in Nepal: Evidence from an organizational network analysis. Matern. Child. Nutr. 2022, 18, e13112. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, K.; Singh, A.; Pandey Rana, P.; Brye, L.; Alayon, S.; Lapping, K.; Gautam, B.; Underwood, C.; Klemm, R.D. Suaahara in Nepal: An at-scale, multi-sectoral nutrition program influences knowledge and practices while enhancing equity. Matern. Child. Nutr. 2017, 13, e12415. [Google Scholar] [CrossRef]
- UNICEF. Bangladesh: Nutrition for Growth (N4G) Commitment. Available online: https://www.unicef.org/bangladesh/en/press-releases/government-bangladesh-commits-improving-nutritional-well-being-mothers-and (accessed on 5 January 2025).
- Vietnam National Nutrition Strategy 2021–2030 with Vision to 2040. Available online: https://www.n4d.group/wp-content/uploads/2023/02/Vietnam-National-Nutrition-Strategy.pdf (accessed on 5 January 2025).
- Khatri, R.B.; Mishra, S.R.; Khanal, V. Female community health volunteers in community-based health programs of Nepal: Future perspective. Front. Public Health 2017, 5, 181. [Google Scholar] [CrossRef]
- Jomaa, L.H.; McDonnell, E.; Probart, C. School feeding programs in developing countries: Impacts on children’s health and educational outcomes. Nutr. Rev. 2011, 69, 83–98. [Google Scholar] [CrossRef]
- Berger, J.; Wieringa, F.T.; Laillou, A.; Pham Van, P.; Dijkhuizen, M.A. Strategies to improve micronutrient status of infants and young children with special attention to complementary foods fortified with micronutrients: Perspectives from Vietnam. In Handbook of Food Fortification and Health: From Concepts to Public Health Applications; Springer: Berlin/Heidelberg, Germany, 2013; Volume 2, pp. 335–346. [Google Scholar]
- Hossain, M.S. School Meals and Child Outcomes in Bangladesh. BUFT J. Bus. Econ. (BJBE) 2021, 2, 274–287. [Google Scholar]
- Saha, K.K.; Billah, M.; Menon, P.; El Arifeen, S.; Mbuya, N.V. Bangladesh National Nutrition Services: Assessment of Implementation Status; World Bank Publications: Herndon, VA, USA, 2015. [Google Scholar]
- Nurilah, E.; Futriani, E.S. Effectiveness Of Supplementary Feeding (PMT) Against Height And Weight Gain Of Stunted Toddlers. Int. J. Health Pharm. (IJHP) 2023, 3, 668–671. [Google Scholar] [CrossRef]
- Kristjansson, E.; Francis, D.K.; Liberato, S.; Jandu, M.B.; Welch, V.; Batal, M.; Greenhalgh, T.; Rader, T.; Noonan, E.; Shea, B. Food supplementation for improving the physical and psychosocial health of socio-economically disadvantaged children aged three months to five years: A systematic review. Campbell Syst. Rev. 2015, 11, 1–226. [Google Scholar] [CrossRef]
- Semba, R.D. The rise and fall of protein malnutrition in global health. Ann. Nutr. Metab. 2016, 69, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Kaur, A.; Choudhary, M.; Kapoor, S. Milk as a Functional Food for Health. In Functional Foods; CRC Press: Boca Raton, FL, USA, 2023; pp. 154–176. [Google Scholar]
- Wiley, A.S. Does milk make children grow? Relationships between milk consumption and height in NHANES 1999–2002. Am. J. Hum. Biol. Off. J. Hum. Biol. Assoc. 2005, 17, 425–441. [Google Scholar] [CrossRef]
- Duan, Y.; Pang, X.; Yang, Z.; Wang, J.; Jiang, S.; Bi, Y.; Wang, S.; Zhang, H.; Lai, J. Association between dairy intake and linear growth in Chinese pre-school children. Nutrients 2020, 12, 2576. [Google Scholar] [CrossRef]
- O’Dwyer, M.; Gillam, S. Children discharged following nutritional rehabilitation: A follow-up study. Trop. Dr. 1995, 25, 146–151. [Google Scholar] [CrossRef]
- Sternin, M.; Sternin, J.; Marsh, D. Scaling up a poverty alleviation and nutrition program in Vietnam. In Scaling Up Scaling Down; Routledge: London, UK, 2013; pp. 97–117. [Google Scholar]
- Truong, D.T.T.; Tran, T.H.T.; Nguyen, T.T.T.; Tran, V.H.T. Double burden of malnutrition in ethnic minority school-aged children living in mountainous areas of Vietnam and its association with nutritional behavior. Nutr. Res. Pract. 2022, 16, 658–672. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.; Huynh, P.; Nguyen, H.T.; Hoang, N.; Mai, L.T.; Tuyen, L.D.; Nguyen, P.H. Nobody left behind? Equity and the drivers of stunting reduction in Vietnamese ethnic minority populations. Food Secur. 2021, 13, 803–818. [Google Scholar] [CrossRef]
- Mbuya, N.V.; Atwood, S.J.; Huynh, P.N. Persistent Malnutrition in Ethnic Minority Communities of Vietnam: Issues and Options for Policy and Interventions; World Bank Publications: Herndon, VA, USA, 2019. [Google Scholar]
- Van Minh, H.; Mai, V.Q.; Anh, T.T.; Duyen, N.T.; Tuyen, L.D.; Mai, T.T.; Phuong, H.N.; Mustafa, T.S.; Nwaigwe, F.; Phuong, D.H. The cost of implementing Vietnam’s national plan of action for nutrition for 2017–2020. AIMS Public Health 2019, 6, 276. [Google Scholar] [CrossRef] [PubMed]
- Bhutta, Z.A.; Akseer, N.; Keats, E.C.; Vaivada, T.; Baker, S.; Horton, S.E.; Katz, J.; Menon, P.; Piwoz, E.; Shekar, M. How countries can reduce child stunting at scale: Lessons from exemplar countries. Am. J. Clin. Nutr. 2020, 112, 894S–904S. [Google Scholar] [CrossRef]
- DeTora, L.M.; Toroser, D.; Sykes, A.; Vanderlinden, C.; Plunkett, F.J.; Lane, T.; Hanekamp, E.; Dormer, L.; DiBiasi, F.; Bridges, D.; et al. Good Publication Practice (GPP) Guidelines for Company-Sponsored Biomedical Research: 2022 Update. Ann. Intern. Med. 2022, 175, 1298–1304. [Google Scholar] [CrossRef]
| Factors | Impact on Child Growth |
|---|---|
| Nutrition and environmental influences |
|
| Genetic disorders |
|
| Hormonal regulation |
|
| Psychosocial factors | |
| Physical activity, sleep, and overall health |
|
| Nepal | Bangladesh | Vietnam | |
|---|---|---|---|
| Underlying determinants | |||
| Food security and food fortification programs, BCC initiatives, multisectoral collaboration | ✓ [69,70,71,72] | ✓ [55,61,62,73] | ✓ [66,67,74] |
| Intermediate determinants | |||
| Community-based nutrition programs, promotion of WASH practices, healthcare worker training | ✓ [69,70,72,75] | ✓ [61,62,73] | ✓ [66,68,74,76] |
| Immediate determinants | |||
| Micronutrient supplementation *, exclusive breastfeeding, maternal and child nutrition services † | ✓ [69,70,72] | ✓ [50,61,62,63] | ✓ [74,77] |
| Supplementary feeding (i.e., milk supplementation) | ✓ [78] | ✓ [66] | |
| Management of childhood diseases | ✓ [55,60,70] | ✓ [79] | |
| (A) | ||
| Programs | Key interventions | Key outcome measures |
MSNP and MSNP-II (2013–2022) [51]
| Nutrition-specific [30]:
| |
FCHV Programme (launched in 1988)
| Nutrition-specific [55]:
|
|
Suaahara Project (2011–2016) [72]
| Nutrition-specific:
|
|
| BCC, Behavioral Change Communication; FCHV, Female Community Health Volunteer; IYCF, Infant and Young Child Feeding; MSNP, Multisectoral Nutrition Plan; WASH, Water, Sanitation, and Hygiene. | ||
| (B) | ||
| Programs | Key interventions | Key outcome measures |
The National Nutrition Services (established in 2011) [61,62]
| Nutrition-specific:
|
|
| NPAN and NPAN 2 (1997; 2016–2025) | Nutrition-specific:
| |
New School Milk Program (launched in 2023)
| Nutrition-specific:
|
|
| * Providing food or cash assistance to vulnerable populations to reduce food insecurity. BCC, Behavioral Change Communication; IYCF, Infant and Young Child Feeding; NPAN, National Plan of Action for Nutrition. | ||
| (C) | ||
| Programs | Key interventions | Key outcome measures |
National Nutrition Strategy (2011–2020) [74]
| Nutrition-specific:
|
|
National School Milk Program
| Nutrition-specific:
|
|
| Hunger Eradication and Poverty Reduction Program (initiated in 1992) | Nutrition-sensitive:
| |
| * Fortifying milk with essential nutrients. UN, United Nations; WASH, Water, Sanitation, and Hygiene. | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jalaludin, M.Y.; Fauzi, M.D.; Sidiartha, I.G.L.; John, C.; Aviella, S.; Novery, E.; Permatasari, A.; Muhardi, L. Addressing Stunting in Children Under Five: Insights and Opportunities from Nepal, Bangladesh, and Vietnam—A Review of Literature. Children 2025, 12, 641. https://doi.org/10.3390/children12050641
Jalaludin MY, Fauzi MD, Sidiartha IGL, John C, Aviella S, Novery E, Permatasari A, Muhardi L. Addressing Stunting in Children Under Five: Insights and Opportunities from Nepal, Bangladesh, and Vietnam—A Review of Literature. Children. 2025; 12(5):641. https://doi.org/10.3390/children12050641
Chicago/Turabian StyleJalaludin, Muhammad Yazid, Moretta Damayanti Fauzi, I Gusti Lanang Sidiartha, Collins John, Shamira Aviella, Edy Novery, Annisa Permatasari, and Leilani Muhardi. 2025. "Addressing Stunting in Children Under Five: Insights and Opportunities from Nepal, Bangladesh, and Vietnam—A Review of Literature" Children 12, no. 5: 641. https://doi.org/10.3390/children12050641
APA StyleJalaludin, M. Y., Fauzi, M. D., Sidiartha, I. G. L., John, C., Aviella, S., Novery, E., Permatasari, A., & Muhardi, L. (2025). Addressing Stunting in Children Under Five: Insights and Opportunities from Nepal, Bangladesh, and Vietnam—A Review of Literature. Children, 12(5), 641. https://doi.org/10.3390/children12050641







