Oral Implications of Herbst Device Modification: A Case Report
Abstract
1. Introduction
2. Materials and Methods
2.1. Simplified Design of the Herbst Appliance
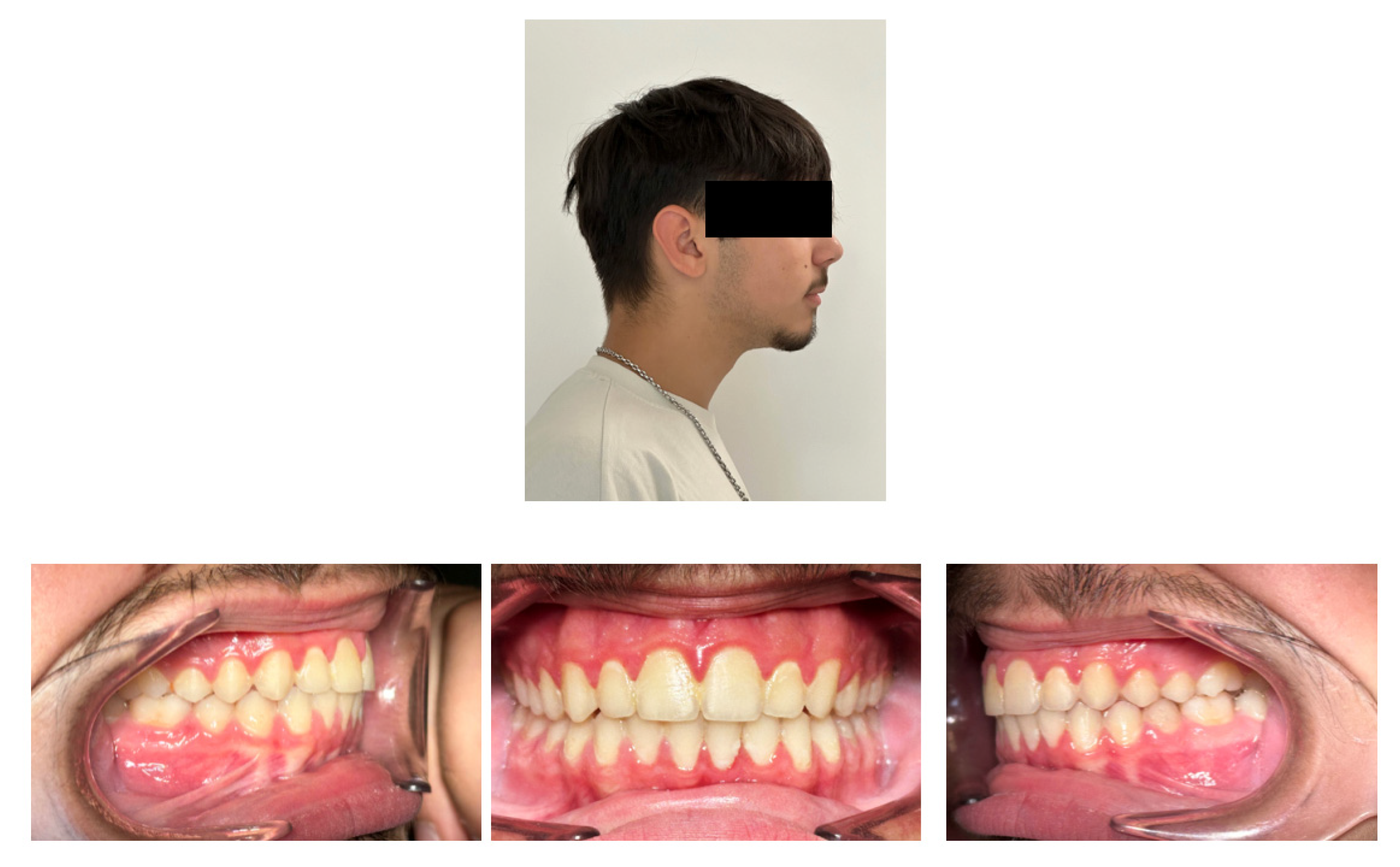
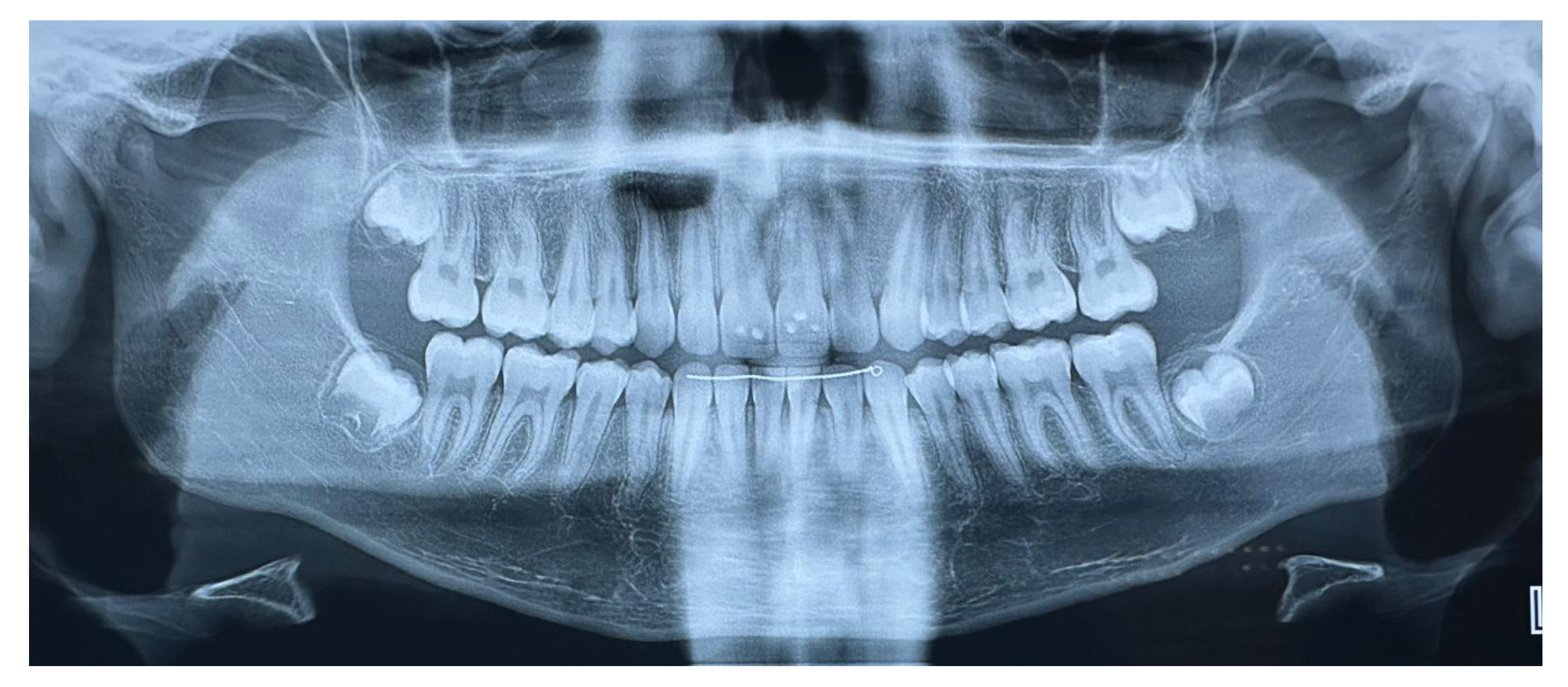
2.2. Case Report Throughout Clinical Phases
3. Results
4. Discussion
4.1. Clinical Observations When Using the Herbst Device
4.2. Clinical Observations After Using the Simplified Design
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Herbst, E. Dreissigjahrige Erfahrungen mit dem retentionsscharnier. Zahnarztl Rundsch. 1934, 43, 1515–1524, 1536–1568, 1611–1616. [Google Scholar]
- Pancherz, H. The effects, limitations, and long-term dentofacial adaptations to treatment with the Herbst appliance. Semin. Orthod. 1997, 3, 232–243. [Google Scholar] [CrossRef] [PubMed]
- Pancherz, H. Treatment of class II malocclusion by jumping the bite with the Herbst appliance. A cephalometric investigation. Am. J. Orthod 1979, 76, 423–442. [Google Scholar] [CrossRef] [PubMed]
- Pancherz, H. Activity of the temporal and masseter muscles in class II, division 1 malocclusions. An electromyographic investigation. Am. J. Orthod. 1980, 77, 679–688. [Google Scholar] [CrossRef]
- Pancherz, H. Vertical dentofacial changes during Herbst appliance treatment. Swed. Dent. J. Suppl. 1982, 15, 189–196. [Google Scholar]
- Ruf, S.; Pancherz, H. Temporomandibular joint growth adaptation in Herbst treatment: A prospective magnetic resonance imaging and cephalometric roentgenographic study. Eur. J. Orthod. 1998, 20, 375–388. [Google Scholar] [CrossRef]
- Serbesis-Tsarudis, C.; Pancherz, H. “Effective” TMJ and chin position changes in Class II treatment. Angle Orthod. 2008, 78, 813–818. [Google Scholar] [CrossRef]
- Cheib Vilefort, P.L.; Farah, L.O.; Gontijo, H.P.; Moro, A.; Ruellas, A.C.O.; Cevidanes, L.H.S.; Nguyen, T.; Franchi, L.; McNamara, J.A., Jr.; Souki, B.Q. Condyle-glenoid fossa relationship after Herbst appliance treatment during two stages of craniofacial skeletal maturation: A retrospective study. Orthod. Craniofac. Res. 2019, 22, 345–353. [Google Scholar] [CrossRef]
- Schwartz, J.P.; Raveli, T.B.; Almeida, K.C.; Schwartz-Filho, H.O.; Raveli, D.B. Cone beam computed tomography study of apical root resorption induced by Herbst appliance. J. Appl. Oral Sci. 2015, 23, 479–485. [Google Scholar] [CrossRef]
- Kinzinger, G.S.M.; Hourfar, J.; Kober, C.; Lisson, J.A. Mandibular fossa morphology during therapy with a fixed functional orthodontic appliance: A magnetic resonance imaging study. J. Orofac. Orthop. 2018, 79, 116–132. [Google Scholar] [CrossRef]
- Nindra, J.; Sidhu, M.S.; Kochhar, A.S.; Dabas, A.; Valletta, R.; Rongo, R.; Spagnuolo, G. Three-Dimensional Evaluation of Condyle-Glenoid Fossa Complex Following Treatment with Herbst Appliance. J. Clin. Med. 2021, 10, 4730. [Google Scholar] [CrossRef] [PubMed]
- Souki, B.Q.; Vilefort, P.L.C.; Oliveira, D.D.; Andrade, I., Jr.; Ruellas, A.C.; Yatabe, M.S.; Nguyen, T.; Franchi, L.; McNamara, J.A., Jr.; Cevidanes, L.H.S. Three-dimensional skeletal mandibular changes associated with Herbst appliance treatment. Orthod. Craniofac. Res. 2017, 20, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Wei, R.Y.; Atresh, A.; Ruellas, A.; Cevidanes, L.H.S.; Nguyen, T.; Larson, B.E.; Mangum, J.E.; Manton, D.J.; Schneider, P.M. Three-dimensional condylar changes from Herbst appliance and multibracket treatment: A comparison with matched Class II elastics. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 505–517. [Google Scholar] [CrossRef] [PubMed]
- Pancherz, H.; Fischer, S. Amount and Direction of Temporomandibular Joint Growth Changes in Herbst Treatment: A Cephalometric Long-Term Investigation. Angle Orthod. 2003, 73, 493–501. [Google Scholar]
- Okano, K.S.; Cevidanes, L.H.S.; Cheib, P.L.; de Oliveira Ruellas, A.C.; Yatabe, M.; Nguyen, T.; Franchi, L.; McNamara, J.A., Jr.; Souki, B.Q. Three-dimensional assessment of the middle cranial fossa and central skull base following Herbst appliance treatment. Angle Orthod. 2018, 88, 757–764. [Google Scholar] [CrossRef]
- Hansen, K.; Pancherz, H.; Petersson, A. Long-term effects of the Herbst appliance on the craniomandibular system with special reference to the TMJ. Eur. J. Orthod. 1990, 12, 244–253. [Google Scholar] [CrossRef]
- Ruf, S.; Bock, N.C. Long-term (≥15 years) effects of Class II treatment: A longitudinal and cross-sectional study on signs and symptoms of temporomandibular disorders. Eur. J. Orthod. 2019, 41, 172–179. [Google Scholar] [CrossRef]
- Pancherz, H.; Ruf, S.; Thomalske-Faubert, C. Mandibular articular disk position changes during Herbst treatment: A prospective longitudinal MRI study. Am. J. Orthod. Dentofa. Orthop. 1999, 116, 207–214. [Google Scholar] [CrossRef]
- Ruf, S.; Pancherz, H. Does bite-jumping damage the TMJ? A prospective longitudinal clinical and MRI study of Herbst patients. Angle Orthod. 2000, 70, 183–199. [Google Scholar] [CrossRef]
- Pancherz, H.; Salé, H.; Bjerklin, K. Signs and symptoms of TMJ disorders in adults after adolescent Herbst therapy: A 6-year and 32-year radiographic and clinical follow-up study. Angle Orthod. 2015, 85, 735–742. [Google Scholar] [CrossRef]
- Minervini, G.; Di Blasio, M.; Franco, R.; Marrapodi, M.M.; Vaienti, B.; Cicciù, M.; Ronsivalle, V. Prevalence of temporomandibular disorders diagnosis in patients treated with Herbst appliance: A systematic review and meta-analysis. BMC Oral Health 2024, 24, 137. [Google Scholar] [CrossRef] [PubMed]
- Isidor, S.; Di Carlo, G.; Cornelis, M.A.; Isidor, F.; Cattaneo, P.M. Three-dimensional evaluation of changes in upper airway volume in growing skeletal Class II patients following mandibular advancement treatment with functional orthopedic appliances. Angle Orthod. 2018, 88, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, S.Y.; Malik, A.M.; Khalid, O.; Mahnoor, M. Comparison of upper pharyngeal airway space in Class II and Class III malocclusion cases. Pak. Orthod. J. 2014, 6, 2–6. [Google Scholar]
- Iwasaki, T.; Sato, H.; Suga, H.; Takemoto, Y.; Inada, E.; Saitoh, I.; Kakuno, K.; Kanomi, R.; Yamasaki, Y. Influence of pharyngeal airway respiration pressure on Class II mandibular retrusion in children: A computational fluid dynamics study of inspiration and expiration. Orthod. Craniofac. Res. 2017, 20, 95–101. [Google Scholar] [CrossRef]
- Gul Amuk, N.; Kurt, G.; Baysal, A.; Turker, G. Changes in pharyngeal airway dimensions following incremental and maximum bite advancement during Herbst-rapid palatal expander appliance therapy in late adolescent and young adult patients: A randomized non-controlled prospective clinical study. Eur. J. Orthod. 2019, 41, 322–330. [Google Scholar] [CrossRef]
- Desai, A.L.; Hegde, M.; Dinesh, M.R.; Amarnath, B.C. Integration of the Herbst and Begg appliance in the management of severe Class II malocclusion. Contemp. Clin. Dent. 2014, 5, 528–531. [Google Scholar] [CrossRef]
- Kabbur, K.J.; Hemanth, M.; Patil, G.S.; Sathyadeep, V.; Shamnur, N.; Harieesha, K.B.; Praveen, G.R. An esthetic treatment outcome of orthognathic surgery and dentofacial orthopedics in class II treatment: A cephalometric study. J. Contemp. Dent. Pract. 2012, 13, 602–606. [Google Scholar] [CrossRef]
- Pancherz, H.; Ruf, S. The Herbst-Appliance, Research-Based Clinical Management, 1st ed.; Quintessence: Batavia, IL, USA, 2008; pp. 1–266. ISBN 978-1-85097-169-6. [Google Scholar]
- Paradowska-Stolarz, A.M.; Ziomek, M.; Sluzalec-Wieckiewicz, K.; Duś-Ilnicka, I. Most common congenital syndromes with facial asymmetry: A narrative review. Dent. Med. Probl. 2024, 61, 925–932. [Google Scholar] [CrossRef]
- Lorenzoni, D.C.; Barbosa, O.T.A.M.; Cury-Saramago, A.A.; Mattos, C.T. Class II subdivision treatment and stability with asymmetric Herbst appliance: A case report. Int. Orthod. 2024, 22, 100838. [Google Scholar] [CrossRef]
- Aiyar, A.; Pedersen, T.K.; Resnick, C.M.; Nørholt, S.E.; Verna, C.; Stoustrup, P.B. Management of unilateral craniofacial microsomia with orthopaedic functional appliances: A systematic literature review. Orthod. Craniofac. Res. 2024, 27, 131–140. [Google Scholar] [CrossRef]
- López, D.F.; Acosta, D.M.; Rivera, D.A.; Mejía, C.M. Hemifacial microsomia: Treatment alternatives-a systematic review of literature. J. Clin. Pediatr. Dent. 2022, 46, 15–30. [Google Scholar] [CrossRef] [PubMed]
- Barenghi, A.; Dell’Oro, A.; Pellegrini, M.; Scribante, A.; Paulsen, H.U.; Spadari, F.; Di Blasio, A. Management of juvenile idiopathic arthritis in a 15-year-old patient: A digitally designed Herbst appliance combined with rapid maxillary expansion for transversal and sagittal correction. Int. Orthod. 2025, 23, 100970. [Google Scholar] [CrossRef] [PubMed]
- von Bremen, J.; Pancherz, H. Efficiency of early and late Class II Division 1 treatment. Am. J. Orthod. Dentofac. Orthop. 2002, 121, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Wigal, T.G.; Dischinger, T.; Martin, C.; Razmus, T.; Gunel, E.; Ngan, P. Stability of Class II treatment with an edgewise crowned Herbst appliance in the early mixed dentition: Skeletal and dental changes. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 210–223. [Google Scholar] [CrossRef]
- Pacha, M.M.; Fleming, P.S.; Pandis, N.; Shagmani, M.; Johal, A. The use of the Hanks Herbst vs. Twin-block in Class II malocclusion: A randomized controlled trial. Am. J. Orthod. Dentofac. Orthop. 2023, 164, 314–324.e1. [Google Scholar] [CrossRef]
- Baysal, A.; Uysal, T. Dentoskeletal effects of Twin Block and Herbst appliances in patients with Class II division 1 mandibular retrognathy. Eur. J. Orthod. 2014, 36, 164–172. [Google Scholar] [CrossRef]
- Macey-Dare, L.V.; Nixon, F. Functional appliances: Mode of action and clinical use. Dent. Update 1999, 26, 240–244, 246. [Google Scholar] [CrossRef]
- O’Brien, K.; Wright, J.; Conboy, F.; Sanjie, Y.; Mandall, N.; Chadwick, S.; Connolly, I.; Cook, P.; Birnie, D.; Hammond, M.; et al. Effectiveness of early orthodontic treatment with the Twin-block appliance: A multicenter, randomized, controlled trial. Part 1: Dental and skeletal effects. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 234–243. [Google Scholar] [CrossRef]
- Ghislanzoni, L.T.; Baccetti, T.; Toll, D.; Defraia, E.; McNamara, J.A., Jr.; Franchi, L. Treatment timing of MARA and fixed appliance therapy of Class II malocclusion. Eur. J. Orthod. 2013, 35, 394–400. [Google Scholar] [CrossRef]
- Franchi, L.; Pavoni, C.; Faltin, K.; McNamara, J.A., Jr.; Cozza, P. Long-term skeletal and dental effects and treatment timing for functional appliances in class II malocclusion. Angle Orthod. 2013, 83, 334–340. [Google Scholar] [CrossRef]
- Purkayastha, S.K.; Rabie, A.B.; Wong, R. Treatment of skeletal class II malocclusion in adults: Stepwise vs. single-step advancement with the Herbst appliance. World J. Orthod. 2008, 9, 233–243. [Google Scholar] [PubMed]
- Bock, N.C.; Reiser, B.; Ruf, S. Class II subdivision treatment with the Herbst appliance. Angle Orthod. 2013, 83, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Karbach, M.; Zöller, C.; Zöller, G.; Wehrbein, H.; Erbe, C. The Herbst appliance and its modifications—Prevalence and individuality. Head Face Med. 2021, 17, 15. [Google Scholar] [CrossRef] [PubMed]
- Metzner, R.; Schwestka-Polly, R.; Helms, H.J.; Wiechmann, D. Comparison of anchorage reinforcement with temporary anchorage devices or a Herbst appliance during lingual orthodontic protraction of mandibular molars without maxillary counterbalance extraction. Head Face Med. 2015, 11, 22. [Google Scholar] [CrossRef]
- Marchi, L.C.; de Arruda Aidar, L.A.; Tortamano, A.; Dominguez, G.C. The skeletal and dental effects of two kinds of Herbst appliances. J. World Fed. Orthod. 2016, 5, 28–34. [Google Scholar] [CrossRef]
- Pancherz, H. The mechanism of Class II correction in Herbst appliance treatment. A cephalometric investigation. Am. J. Orthod. 1982, 82, 104–113. [Google Scholar] [CrossRef]
- Lai, M.; McNamara, J.A., Jr. An evaluation of two-phase treatment with the Herbst appliance and preadjusted edgewise therapy. Semin. Orthod. 1998, 4, 46–58. [Google Scholar] [CrossRef]
- Marchi, P.G.B.; Muñoz, J.F.M.; de Arruda Aidar, L.A.; Marchi, L.C.; Dominguez, G.C.; Raveli, D.B. Dental changes induced by a modified Herbst appliance followed by fixed appliances: A digital dental model analysis. J. World Fed. Orthod. 2023, 12, 131–137. [Google Scholar] [CrossRef]
- Yang, X.; Zhu, Y.; Long, H.; Zhou, Y.; Jian, F.; Ye, N.; Gao, M.; Lai, W. The effectiveness of the Herbst appliance for patients with Class II malocclusion: A meta-analysis. Eur. J. Orthod. 2016, 38, 324–333. [Google Scholar] [CrossRef]
- Farouk, K.; Eissa, O.; Ghoneima, A.; El-Bedwehi, A.; Abdel-Fattah, E.; Hussein, F.; El-Bialy, T. Treatment effects of Herbst appliance in skeletal Class II cases during pre-pubertal and post-pubertal periods: A cone-beam computed tomographic study. Sci. Rep. 2023, 13, 11342. [Google Scholar] [CrossRef]
- Zymperdikas, V.F.; Koretsi, V.; Papageorgiou, S.N.; Papadopoulos, M.A. Treatment effects of fixed functional appliances in patients with Class II malocclusion: A systematic review and meta-analysis. Eur. J. Orthod. 2016, 38, 113–126. [Google Scholar] [CrossRef] [PubMed]
- Burkhardt, D.R.; McNamara, J.A., Jr.; Baccetti, T. Maxillary molar distalization or mandibular enhancement: A cephalometric comparison of comprehensive orthodontic treatment including the pendulum and the Herbst appliances. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Sangalli, K.L.; Dutra-Horstmann, K.L.; Correr, G.M.; Topolski, F.; Flores-Mir, C.; Lagravère, M.O.; Moro, A. Three-dimensional skeletal and dentoalveolar sagittal and vertical changes associated with cantilever Herbst appliance in prepubertal patients with Class II malocclusion. Am. J. Orthod. Dentofac. Orthop. 2022, 161, 638–651.e1. [Google Scholar] [CrossRef] [PubMed]
- Konik, M.; Pancherz, H.; Hansen, K. The mechanism of Class II correction in late Herbst treatment. Am. J. Orthod. Dentofac. Orthop. 1997, 112, 87–91. [Google Scholar] [CrossRef]
- Nelson, B.; Hansen, K.; Hägg, U. Class II correction in patients treated with class II elastics and with fixed functional appliances: A comparative study. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 142–149. [Google Scholar] [CrossRef]
- Tomblyn, T.; Rogers, M.; Andrews, L., 2nd; Martin, C.; Tremont, T.; Gunel, E.; Ngan, P. Cephalometric study of Class II Division 1 patients treated with an extended-duration, reinforced, banded Herbst appliance followed by fixed appliances. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 818–830. [Google Scholar] [CrossRef]
- Macrì, M.; Toniato, E.; Murmura, G.; Varvara, G.; Festa, F. Midpalatal suture density as a function of sex and growth-pattern-related variability via CBCT evaluations of 392 adolescents treated with a rapid maxillary expander appliance. Appl. Sci. 2022, 12, 2221. [Google Scholar] [CrossRef]
- Amuk, N.G.; Baysal, A.; Coskun, R.; Kurt, G. Effectiveness of incremental vs maximum bite advancement during Herbst appliance therapy in late adolescent and young adult patients. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 48–56. [Google Scholar] [CrossRef]
- Xu, F.; Fang, Y.; Sui, X.; Yao, Y. Comparison of Twin Block appliance and Herbst appliance in the treatment of Class II malocclusion among children: A meta-analysis. BMC Oral Health 2024, 24, 78. [Google Scholar] [CrossRef]
- Wu, Y.; Yu, Q.; Xia, Y.; Wang, B.; Chen, S.; Gu, K.; Zhang, B.; Zhu, M. Does mandibular advancement with clear aligners have the same skeletal and dentoalveolar effects as traditional functional appliances? BMC Oral Health 2023, 23, 65. [Google Scholar] [CrossRef]
- Hosseini, H.R.; Ngan, P.; Tai, S.K.; Andrews, L.J., 2nd; Xiang, J. A comparison of skeletal and dental changes in patients with a Class II relationship treated with clear aligner mandibular advancement and Herbst appliance followed by comprehensive orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2024, 165, 205–219. [Google Scholar] [CrossRef] [PubMed]
- Illing, H.M.; Morris, D.O.; Lee, R.T. A prospective evaluation of Bass, Bionator and Twin Block appliances. Part I—The hard tissues. Eur. J. Orthod. 1998, 20, 501–516. [Google Scholar] [CrossRef] [PubMed]
- Verma, N.; Gar, A.; Sahu, S.; Choudhary, A.S.; Baghel, S. Fixed functional appliance—A Bird’s Eyeview. IOSR J. Dent. Med. Sci. 2019, 18, 67–83. [Google Scholar]
- Tahmasbi, S.; Seifi, M.; Soleymani, A.A.; Mohamadian, F.; Alam, M. Comparative study of changes in the airway dimensions following the treatment of Class II malocclusion patients with the twin-block and Seifi appliances. Dent. Med. Probl. 2023, 60, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, P.M.; Cheib-Vilefort, P.L.; de Pársia Gontijo, H.; Melgaço, C.A.; Franchi, L.; McNamara, J.A., Jr.; Souki, B.Q. Three-dimensional changes of the upper airway in patients with Class II malocclusion treated with the Herbst appliance: A cone-beam computed tomography study. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 205–211. [Google Scholar] [CrossRef]








| Traditional Design | Simplified Design | |
|---|---|---|
| Total number of bands per arch | 4 | 2 |
| First molar bands | Normal | Partial occlusal coverage |
| Goshgarin trans-palatal bar | Present | Present |
| Welded lingual arch | Present | Present |
| Welded arm extension from molar to first premolar | Present | Absent |
| Left and right telescopic tube | Present | Present |
| Reference Values | T0 Measurements | T1 Measurements | |
|---|---|---|---|
| SNA angle | 82° | 82.5° | 82° |
| SNB angle | 80° | 75° | 79.5° |
| ANB angle | 2° | 5° | 2.5° |
| Wits appraisal | 0 mm | 4 mm | 2 mm |
| SN-GoMe angle | 32° | 35° | 36° |
| SN-SnaSnp angle | 8° | 7° | 6° |
| SnaSnp-GoMe angle | 26° | 28° | 30° |
| p.O.-GoMe angle | 16° | 19.5° | 17° |
| GoMe-GoPc angle | 126° | 128° | 122° |
| GoMe-GoN angle | 73° | 71° | 73° |
| GoN-GoPc angle | 53° | 57° | 49° |
| SGn-SN angle | 67° | 68° | 69° |
| SGo/NMe | 62% | 62% | 63% |
| I+/I− angle | 131° | 106° | 130° |
| SnaSnp-I+ angle | 109° | 126° | 105° |
| GoMe-I− angle | 90° | 102° | 102° |
| Overjet | 2 mm | 9 mm | 2.5 mm |
| NB-LsPgC angle | 8° | 17° | 11.5° |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Macrì, M.; Di Carmine, M.; Scarano, A.; Festa, F. Oral Implications of Herbst Device Modification: A Case Report. Children 2025, 12, 531. https://doi.org/10.3390/children12050531
Macrì M, Di Carmine M, Scarano A, Festa F. Oral Implications of Herbst Device Modification: A Case Report. Children. 2025; 12(5):531. https://doi.org/10.3390/children12050531
Chicago/Turabian StyleMacrì, Monica, Mariastella Di Carmine, Antonio Scarano, and Felice Festa. 2025. "Oral Implications of Herbst Device Modification: A Case Report" Children 12, no. 5: 531. https://doi.org/10.3390/children12050531
APA StyleMacrì, M., Di Carmine, M., Scarano, A., & Festa, F. (2025). Oral Implications of Herbst Device Modification: A Case Report. Children, 12(5), 531. https://doi.org/10.3390/children12050531






