Music Therapy for Managing Dental Anxiety in Children: A Systematic Review and Meta-Analysis of Clinical Evidence
Abstract
Highlights
- Music therapy significantly reduces self-reported dental anxiety in children, with moderate effect sizes across randomized controlled trials.
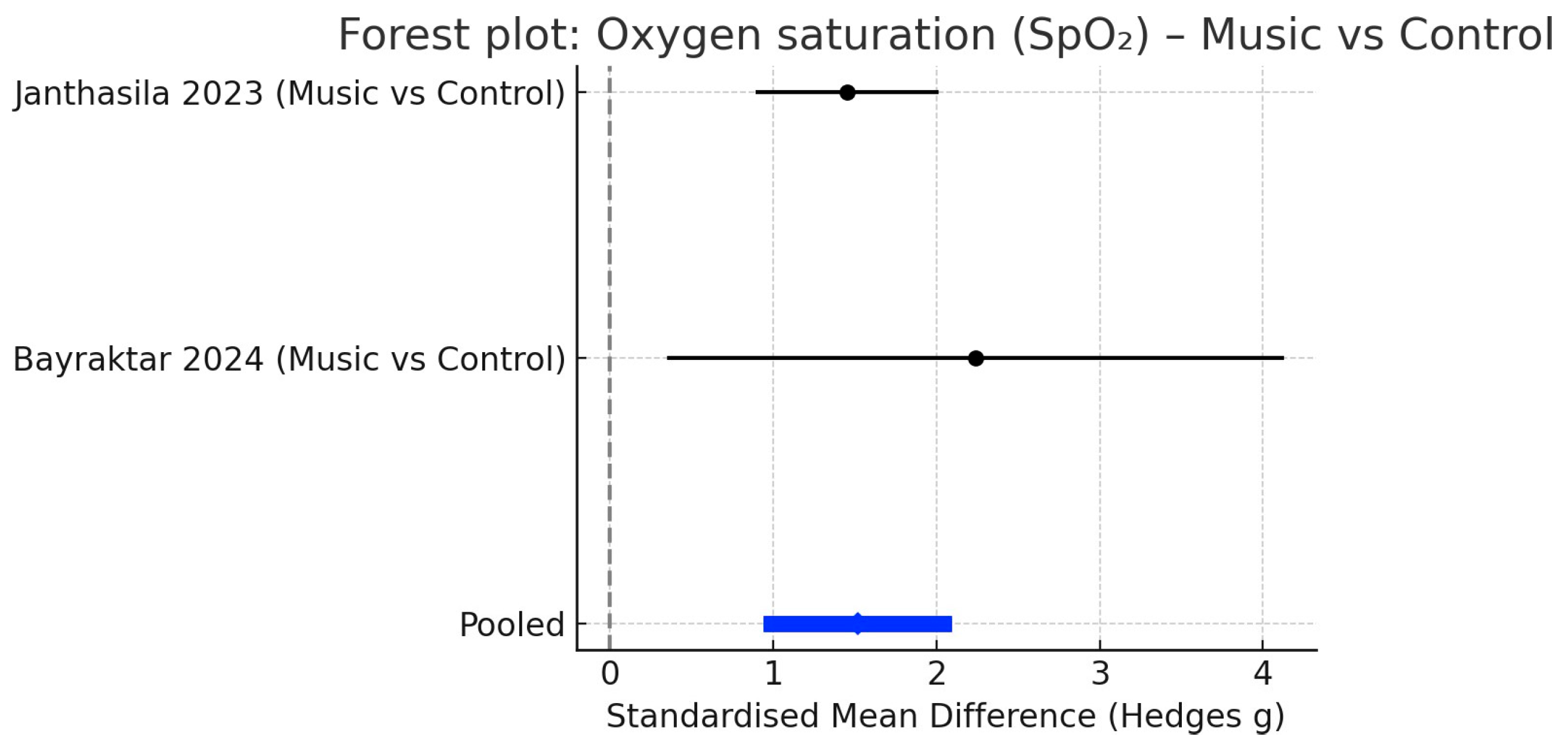
- Heart rate is consistently lowered during treatment, although blood pressure and oxygen saturation show no significant changes.
- Music therapy is a safe, inexpensive, and child-friendly adjunct that can enhance cooperation and improve the overall dental experience.
- Its integration into paediatric dental practice may reduce reliance on pharmacological interventions and support better treatment outcomes.
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Information Sources and Search Strategy
2.4. Data Extraction
2.5. Study Selection and Variables
2.6. Quality Assessment
2.7. Data Synthesis and Statistical Analysis
3. Results
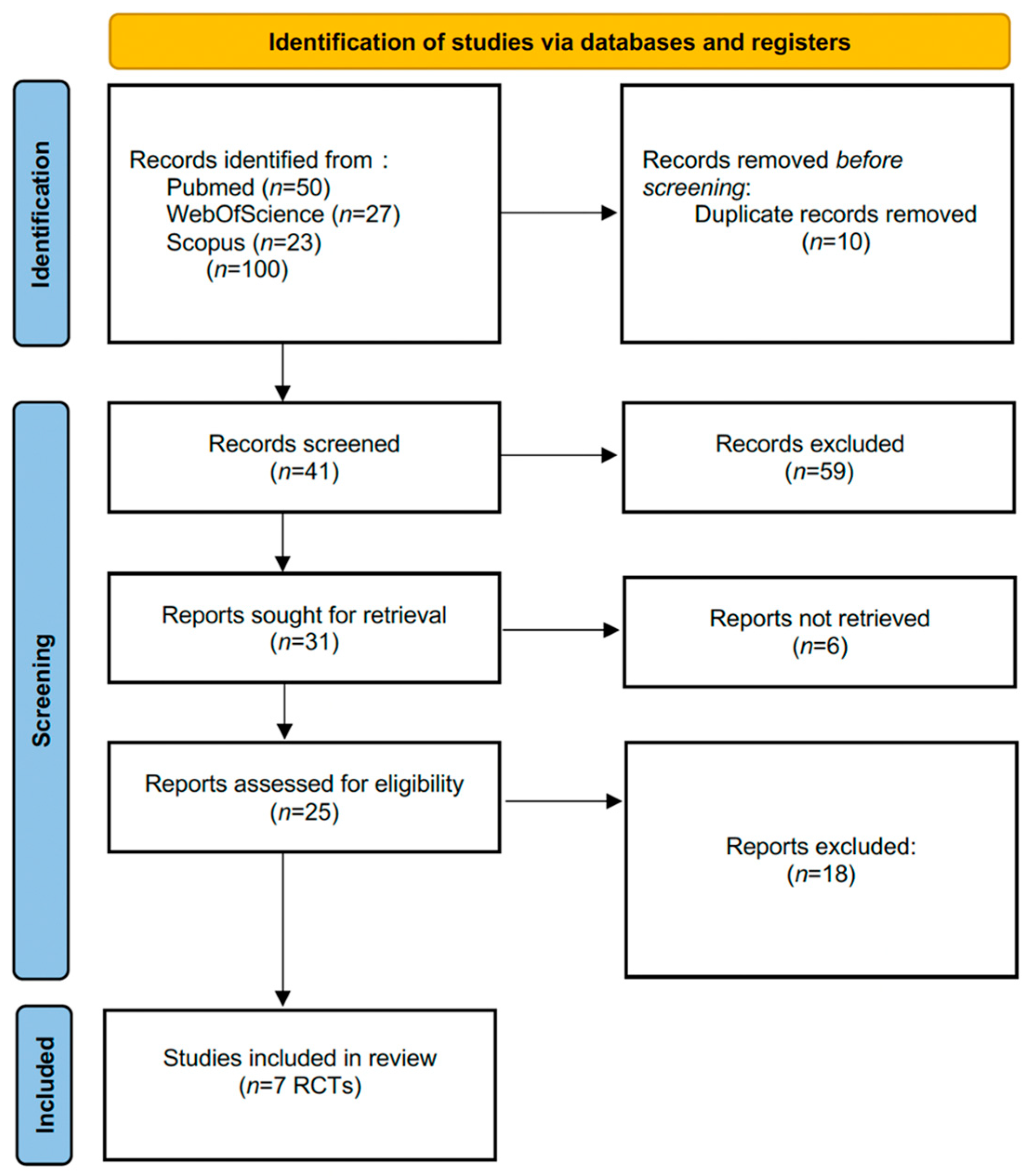
3.1. Study Selection
3.2. Characteristics of Included Studies
3.3. Risk of Bias Assessment
3.4. Quantitative Synthesis
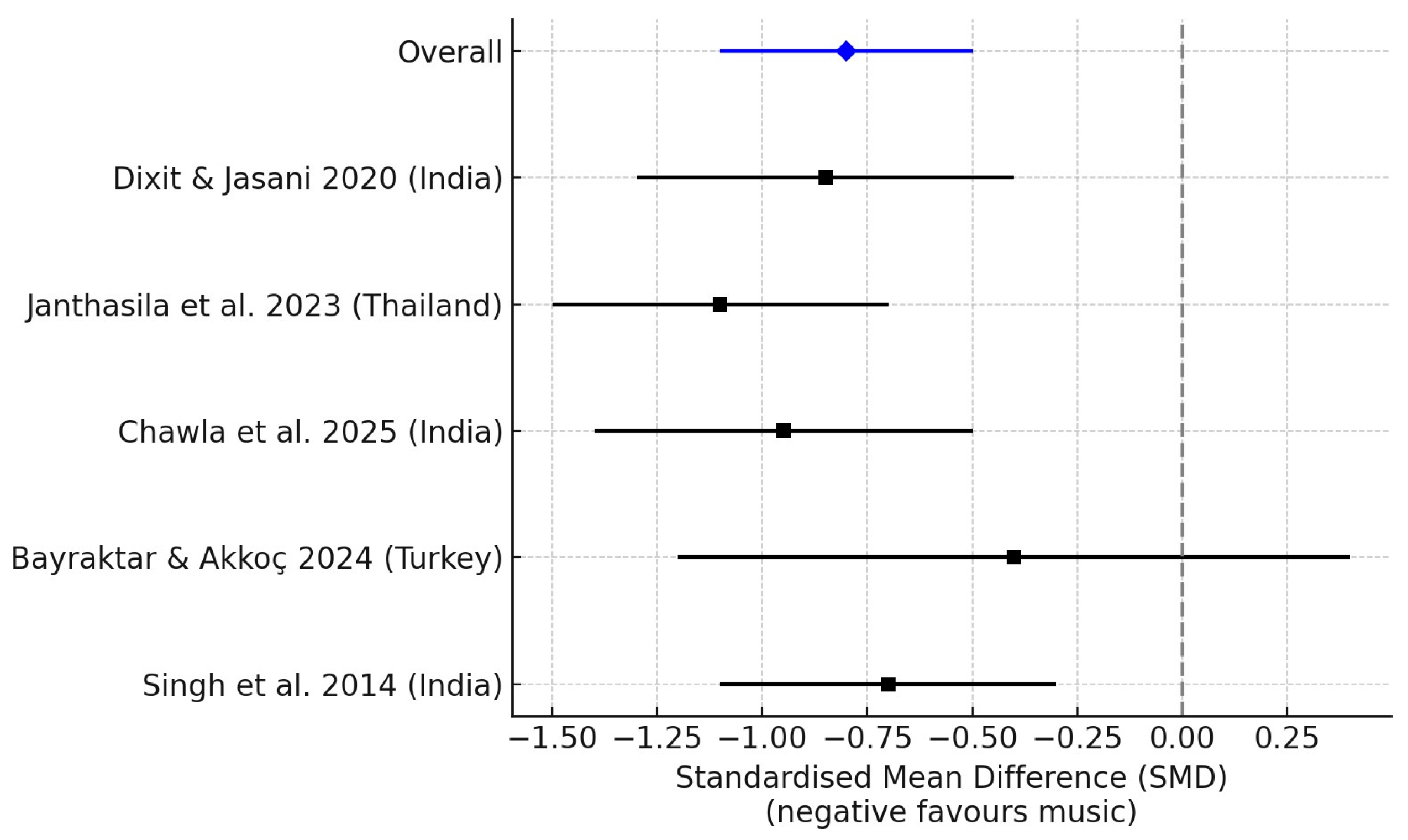
3.4.1. Dental Anxiety (Self-Reported Scales)
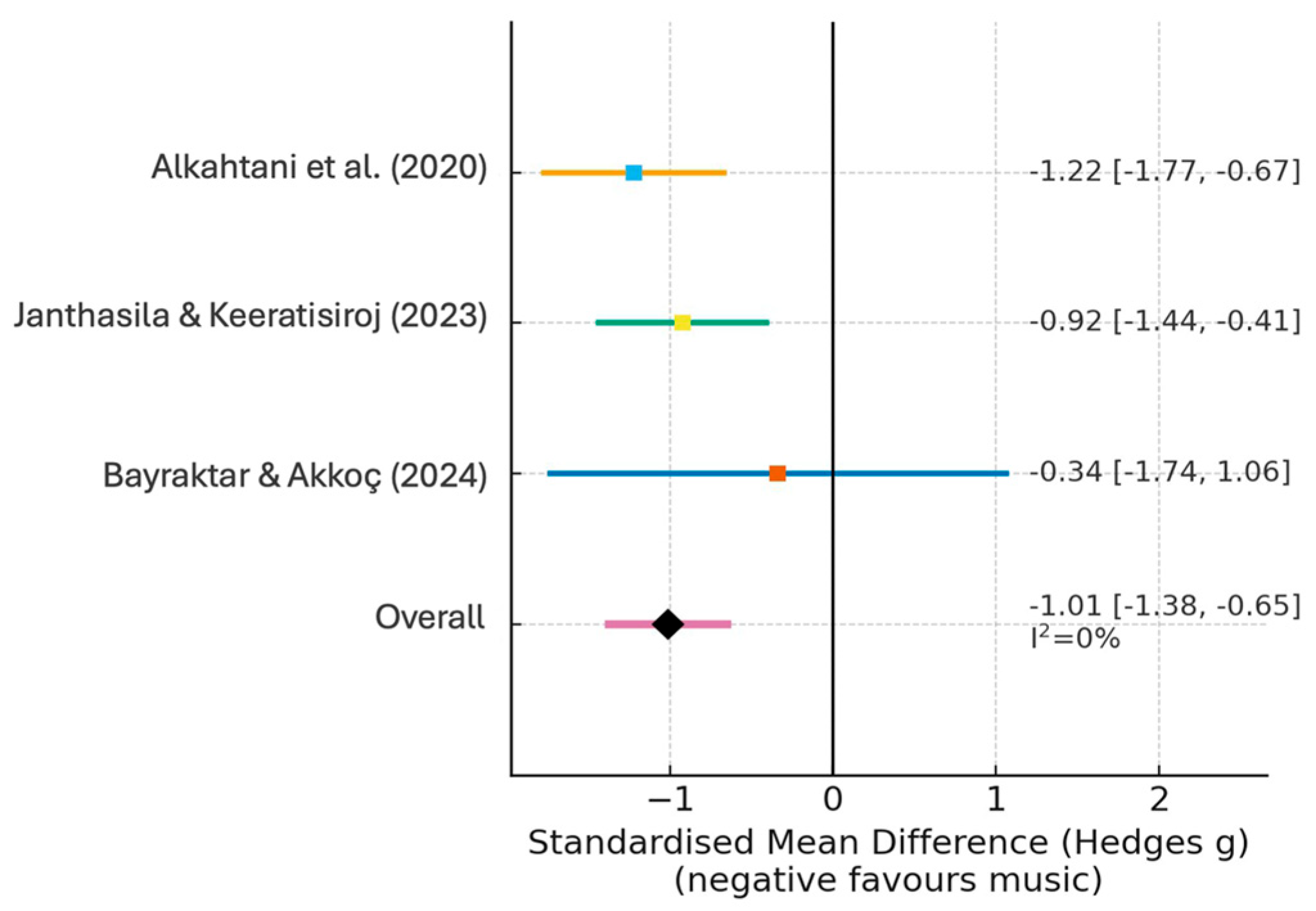
3.4.2. Heart Rate
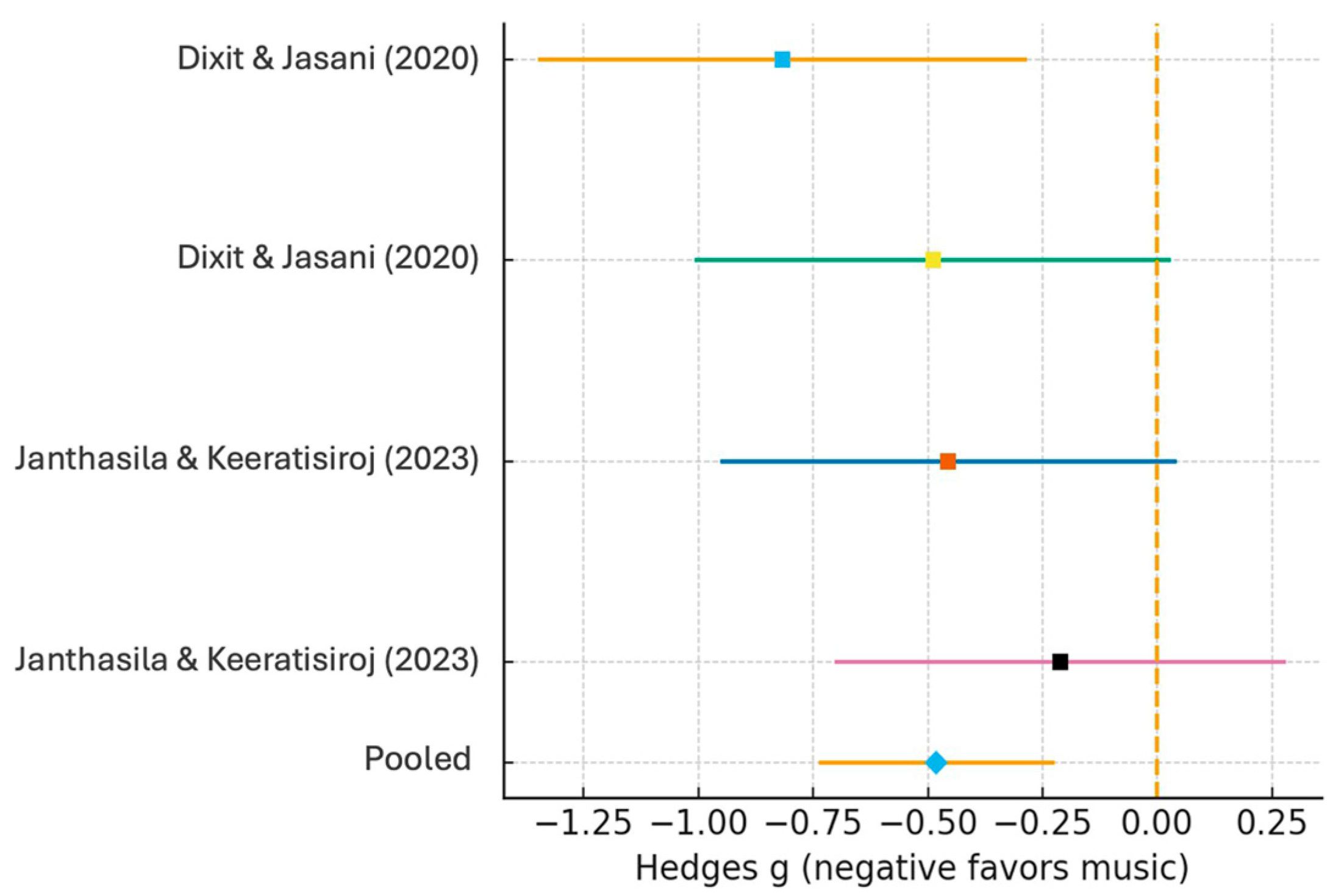
3.4.3. Blood Pressure
3.4.4. Oxygen Saturation
3.4.5. Subgroup Analyses
3.4.6. Sensitivity Analyses
3.4.7. Secondary Outcomes: Child Cooperation and Parental Perception
4. Discussion
4.1. Summary of Evidence
4.2. Comparison with Previous Evidence
4.3. Clinical Implications
4.4. Limitations of the Evidence
4.5. Recommendations for Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Complete Search Strategies
- PubMed:(“music therapy” [MeSH Terms] OR “music therapy” [All Fields] OR “music” [All Fields]) AND (“pediatric dentistry” [MeSH Terms] OR “paediatric dentistry” [All Fields] OR “child dental care” [All Fields]) AND (“dental anxiety” [MeSH Terms] OR “dental fear” [All Fields] OR “stress” [All Fields] OR “behavior management” [All Fields])
- Scopus:(TITLE-ABS-KEY(“music therapy” OR music) AND TITLE-ABS-KEY(“pediatric dentistry” OR “paediatric dentistry” OR “child dental care”) AND TITLE-ABS-KEY(“dental anxiety” OR “dental fear” OR stress OR “behavior management”))
- Web of Science:TS = (“music therapy” OR music) AND TS = (“pediatric dentistry” OR “paediatric dentistry” OR “child dental care”) AND TS = (“dental anxiety” OR “dental fear” OR stress OR “behavior management”)
- Cochrane Library:(“music therapy” OR music) AND (“pediatric dentistry” OR “paediatric dentistry” OR “child dental care”) AND (“dental anxiety” OR “dental fear” OR stress OR “behavior management”) in Title Abstract Keyword.
References
- Petersen, P.E. The World Oral Health Report 2003: Continuous Improvement of Oral Health in the 21st Century. Community Dent. Oral Epidemiol. 2003, 31 (Suppl. S1), 3–24. [Google Scholar] [CrossRef]
- Armfield, J.M.; Heaton, L.J. Management of Fear and Anxiety in the Dental Clinic: A Review. Aust. Dent. J. 2013, 58, 390–407. [Google Scholar] [CrossRef] [PubMed]
- Klassen, J.A.; Liang, Y.; Tjosvold, L.; Klassen, T.P.; Hartling, L. Music for Pain and Anxiety in Children Undergoing Medical Procedures: A Systematic Review of Randomized Controlled Trials. Ambul. Pediatr. 2008, 8, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Chanda, M.L.; Levitin, D.J. The Neurochemistry of Music. Trends Cogn. Sci. 2013, 17, 179–193. [Google Scholar] [CrossRef] [PubMed]
- Uggla, L.; Bonde, L.O.; Svahn, B.M.; Remberger, M.; Wrangsjö, B.; Gustafsson, B. Music Therapy Can Lower the Heart Rates of Severely Sick Children. Eur. J. Cancer Care 2016, 25, 953–959. [Google Scholar] [CrossRef]
- Klingberg, G.; Broberg, A.G. Dental fear/anxiety and dental behaviour management problems in children and adolescents: A review of prevalence and concomitant psychological factors. Int. J. Paediatr. Dent. 2007, 17, 391–406. [Google Scholar] [CrossRef]
- Cianetti, S.; Lombardo, G.; Lupatelli, E.; Pagano, S.; Abraha, I.; Montedori, A.; Caruso, S.; Gatto, R.; De Giorgio, S.; Salvato, R.; et al. Dental fear/anxiety among children and adolescents: A systematic review. Eur. J. Paediatr. Dent. 2017, 18, 121–130. [Google Scholar]
- Kumar, S.; Bhargav, A.; Patel, P.; Bhati, M.; Balasubramanyam, G.; Duraiswamy, P.; Kulkarni, S. Prevalence of dental anxiety among children aged 5–15 years. J. Indian Soc. Pedod. Prev. Dent. 2020, 38, 109–114. [Google Scholar] [CrossRef]
- American Academy of Pediatric Dentistry (AAPD). Behavior guidance for the pediatric dental patient. In Clinical Practice Guidelines; American Academy of Pediatric Dentistry: Chicago, IL, USA, 2021. [Google Scholar]
- Bruscia, K. Defining Music Therapy; Barcelona Publishers: New Braunfels, TX, USA, 2014. [Google Scholar]
- Thoma, M.V.; La Marca, R.; Brönnimann, R.; Finkel, L.; Ehlert, U.; Nater, U.M. The effect of music on the human stress response. PLoS ONE 2013, 8, e70156. [Google Scholar] [CrossRef]
- Van der Weijden, F.N.; Hussain, A.M.; Tang, L.; Slot, D.E. The effect of playing background music during dental treatment on dental anxiety and physiological parameters: A systematic review and meta-analysis. Psychol. Music 2022, 50, 365–388. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Abdalhai, R.; Kouchaji, C.; Alkhatib, R. The effect of aromatherapy with lavender-neroli oil and music in management of pediatric dental anxiety: A randomized control trial. BDJ Open 2024, 10, 5. [Google Scholar] [CrossRef]
- Dixit, U.; Jasani, R. Comparison of the effectiveness of Bach flower therapy and music therapy on dental anxiety in pediatric patients: A randomized controlled study. J. Indian Soc. Pedod. Prev. Dent. 2020, 38, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Janthasila, N.; Keeratisiroj, O. Music therapy and aromatherapy on dental anxiety and fear: A randomized controlled trial. J. Dent. Sci. 2023, 18, 203–210. [Google Scholar] [CrossRef]
- Chawla, T.; Nangia, T.; Srivastava, M.; Kalra, G.; Langpoklakpam, C. Comparative evaluation of effectiveness among various sensory distractors for reducing dental anxiety in pediatric population aged 6–9 years—A randomized controlled trial. J. Indian Soc. Pedod. Prev. Dent. 2025, 43, 104–110. [Google Scholar] [CrossRef]
- Bayraktar, C.; Akkoç, S. Evaluation of the role of music and Bach flower remedies in the management of anxious pediatric dental patients: A randomised clinical trial. Clin. Exp. Health Sci. 2024, 14, 882–888. [Google Scholar] [CrossRef]
- Alkahtani, Z.M.; Zakirulla, M.; Alshehri, E.S.; Alqahtani, A.M. The effect of music on children’s anxiety during dental treatment. J. Res. Med. Dent. Sci. 2020, 8, 39–43. [Google Scholar]
- Singh, D.; Samadi, F.; Jaiswal, J.; Tripathi, A.M. Stress reduction through audio distraction in anxious pediatric dental patients: An adjunctive clinical study. Int. J. Clin. Pediatr. Dent. 2014, 7, 149–152. [Google Scholar] [CrossRef]
- Pradopo, S.; Sinaredi, B.R.; Januarisca, B.V. Pandan leaves (Pandanus amaryllifolius) aromatherapy and relaxation music to reduce dental anxiety of pediatric patients. J. Int. Dent. Med Res. 2017, 10, 933–937. [Google Scholar]
- Gokhale, N.S.; Hugar, S.M.; Saxena, N.; Kohli, N.; Patil, V.H.; Kadam, K.S. Evaluation of the use of music as a distraction technique on dental anxiety of children—A systematic review and meta-analysis. J. Sci. Soc. 2024, 51, 347–355. [Google Scholar] [CrossRef]
- Sin, M.; Dennis, T. Can music therapy and aroma therapy really reduce dental anxiety and fear? Evid.-Based Dent. 2023, 24, 59–60. [Google Scholar] [CrossRef]
| Author (Year) | Country | Design | Sample Size (n) | Age Range (Years) | Intervention Details (Type, Delivery, Timing) | Comparator | Outcomes Measured | Main Findings |
|---|---|---|---|---|---|---|---|---|
| Abdalhai et al. (2024) [15] | Syria | RCT | 56 | 6–10 | Receptive music (relaxing tracks via headphones during treatment) + Aromatherapy | Standard care (no adjunctive therapy) | FIS, HR, BP | Significant reduction in anxiety (FIS) and heart rate vs. control. |
| Alkahtani et al. (2020) [20] | Saudi Arabia | RCT | 40 | 5–11 | Receptive music (instrumental via headphones during treatment) | No music (usual care) | Corah’s Scale, HR, SpO2 | Significant reduction in HR and self-reported anxiety in music group. |
| Bayraktar & Akkoç (2024) [19] | Turkey | RCT | 12 | 6–8 | Receptive music (via headphones for 15 min pre-treatment) vs. Bach flower remedy | No intervention (quiet waiting) | FIS, VPT, HR | No statistically significant differences between groups (very small sample size). |
| Chawla et al. (2025) [18] | India | RCT | 60 | 6–9 | Receptive music (children’s songs via headphones, 10 min pre-op and during treatment) vs. other sensory distractors | No intervention | FIS, SpO2, Anxiety Scales | Music was the most effective distractor, yielding the greatest reduction in anxiety. |
| Dixit & Jasani (2020) [16] | India | RCT | 120 | 4–6 | Receptive music (instrumental via headphones during procedure) vs. Bach flower remedy | No intervention | FIS, Behaviour Rating Scale, HR, BP | Both interventions reduced anxiety; music significantly reduced BP compared to control. |
| Janthasila & Keeratisiroj (2023) [17] | Thailand | RCT | 128 | 10–12 | Receptive music (traditional instrumental during treatment) ± Aromatherapy | Standard care (no dis- traction) | FIS, CFSS-DS, HR, BP, SpO2 | Combined therapy was most effective; music alone also showed significant anxiety reduction. |
| Singh et al. (2014) [21] | India | RCT | 60 | 7–9 | Receptive music (audio distraction via headphones during procedure) | Standard care (silence) | VPT, HR, BP, SpO2 | Significant reduction in anxiety (VPT) and HR; increase in SpO2 in music group. |
 = Low risk;
= Low risk;  = Some concerns;
= Some concerns;  = High risk. Included studies: Abdalhai et al., 2024 [15]; Dixit & Jasani, 2020 [16]; Janthasila & Keera-tisiroj, 2023 [17]; Chawla et al., 2025 [18]; Bayraktar & Ak-koç, 2024 [19]; Alkahtani et al., 2020 [20]; Singh et al., 2014 [21].
= High risk. Included studies: Abdalhai et al., 2024 [15]; Dixit & Jasani, 2020 [16]; Janthasila & Keera-tisiroj, 2023 [17]; Chawla et al., 2025 [18]; Bayraktar & Ak-koç, 2024 [19]; Alkahtani et al., 2020 [20]; Singh et al., 2014 [21].
 = Low risk;
= Low risk;  = Some concerns;
= Some concerns;  = High risk. Included studies: Abdalhai et al., 2024 [15]; Dixit & Jasani, 2020 [16]; Janthasila & Keera-tisiroj, 2023 [17]; Chawla et al., 2025 [18]; Bayraktar & Ak-koç, 2024 [19]; Alkahtani et al., 2020 [20]; Singh et al., 2014 [21].
= High risk. Included studies: Abdalhai et al., 2024 [15]; Dixit & Jasani, 2020 [16]; Janthasila & Keera-tisiroj, 2023 [17]; Chawla et al., 2025 [18]; Bayraktar & Ak-koç, 2024 [19]; Alkahtani et al., 2020 [20]; Singh et al., 2014 [21].| Study (Author, Year) | Randomization Process | Deviations from Intended Interventions | Missing Outcome Data | Measurement of the Outcome | Selection of the Reported Result | Overall Risk of Bias |
|---|---|---|---|---|---|---|
| Abdalhai et al., 2024 |  |  |  |  |  |  |
| Alkahtani et al., 2020 |  |  |  |  |  |  |
| Bayraktar & Akkoç, 2024 |  |  |  |  |  |  |
| Chawla et al., 2025 |  |  |  |  |  |  |
| Dixit & Jasani, 2020 |  |  |  |  |  |  |
| Janthasila & Keera-tisiroj, 2023 |  |  |  |  |  |  |
| Singh et al., 2014 |  |  |  |  |  |  |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marqués-Martínez, L.; Andrés, J.; García-Miralles, E.; Borell-García, C.; Aura-Tormos, J.I.; Barona, C.G. Music Therapy for Managing Dental Anxiety in Children: A Systematic Review and Meta-Analysis of Clinical Evidence. Children 2025, 12, 1382. https://doi.org/10.3390/children12101382
Marqués-Martínez L, Andrés J, García-Miralles E, Borell-García C, Aura-Tormos JI, Barona CG. Music Therapy for Managing Dental Anxiety in Children: A Systematic Review and Meta-Analysis of Clinical Evidence. Children. 2025; 12(10):1382. https://doi.org/10.3390/children12101382
Chicago/Turabian StyleMarqués-Martínez, Laura, Jorge Andrés, Esther García-Miralles, Carla Borell-García, Juan Ignacio Aura-Tormos, and Clara Guinot Barona. 2025. "Music Therapy for Managing Dental Anxiety in Children: A Systematic Review and Meta-Analysis of Clinical Evidence" Children 12, no. 10: 1382. https://doi.org/10.3390/children12101382
APA StyleMarqués-Martínez, L., Andrés, J., García-Miralles, E., Borell-García, C., Aura-Tormos, J. I., & Barona, C. G. (2025). Music Therapy for Managing Dental Anxiety in Children: A Systematic Review and Meta-Analysis of Clinical Evidence. Children, 12(10), 1382. https://doi.org/10.3390/children12101382






