Comparative Analysis of Sleep Hygiene and Patterns among Adolescents in Two Russian Arctic Regions: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Cohort Characteristics
3.2. Sleep Parameters on Schooldays and on Weekends
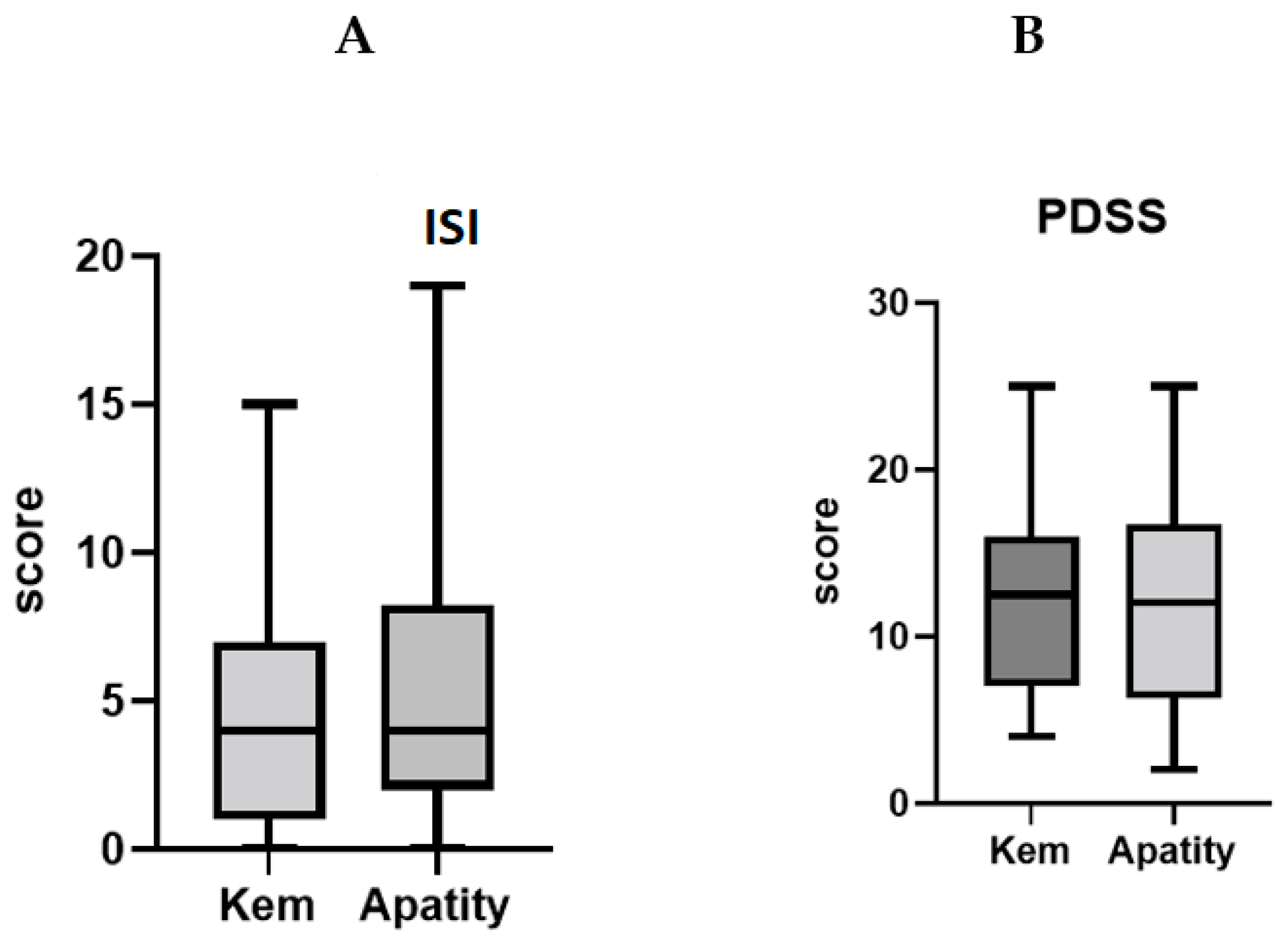
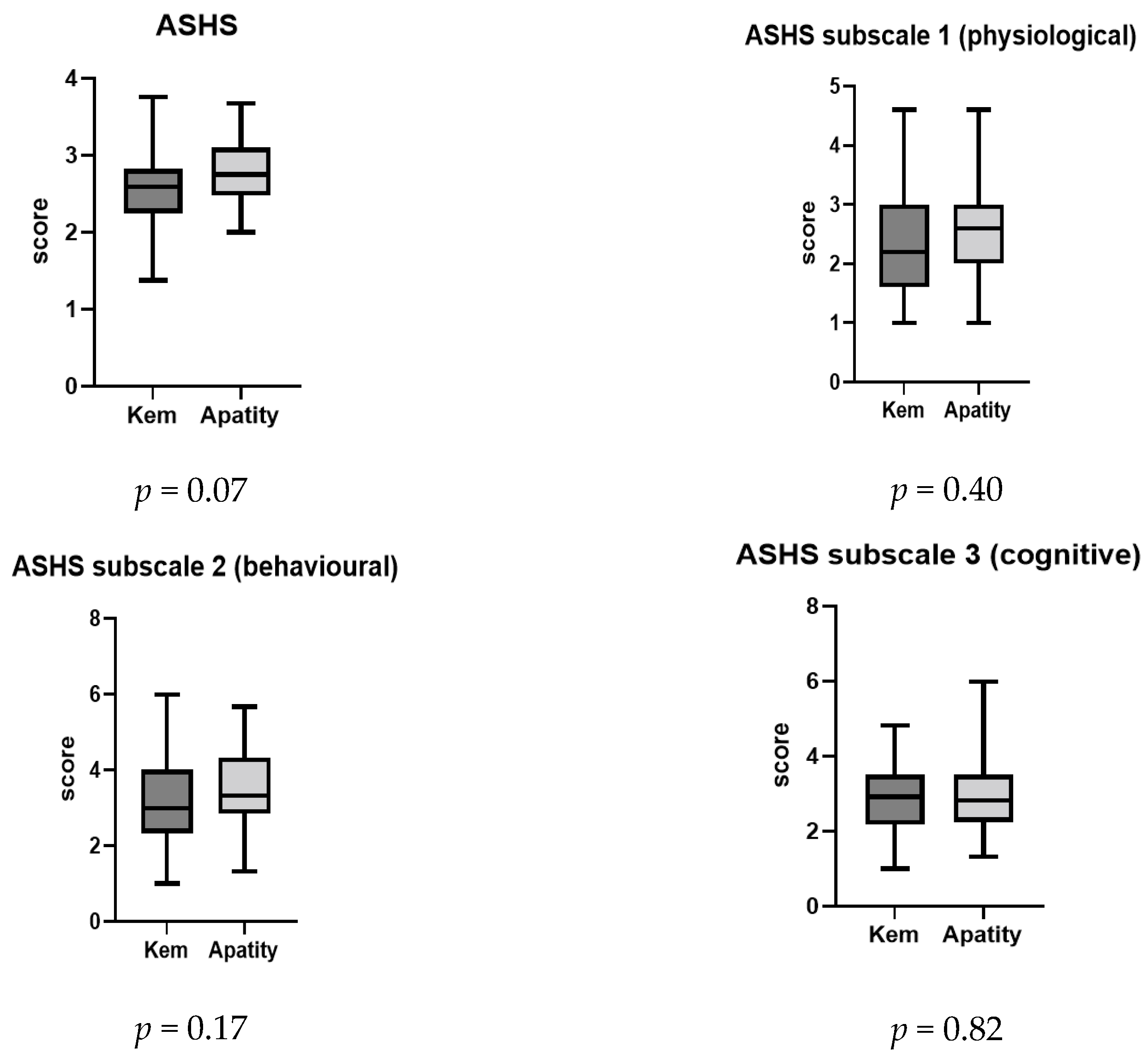
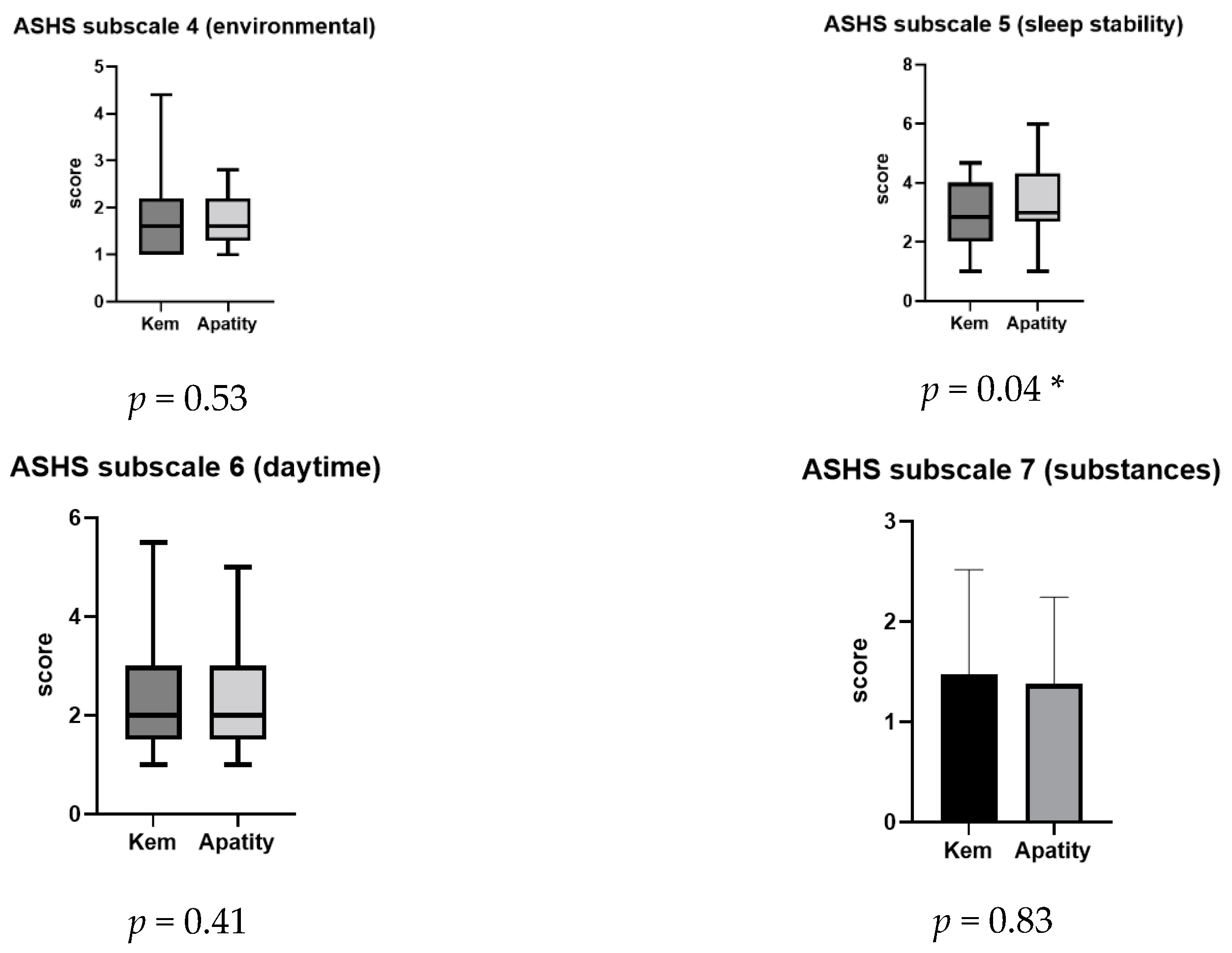
3.3. Sleep Complaints and Sleep Disorders in Schoolchildren
3.4. The Association between Academic Achievements and Sleep Parameters
4. Discussion
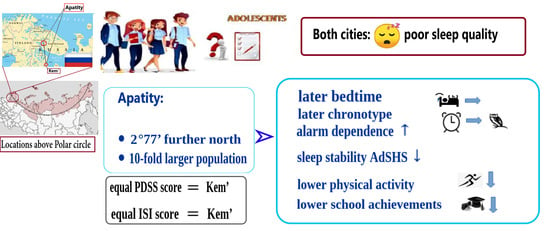
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arendt, J. Biological rhythms during residence in polar regions. Chronobiol. Int. 2012, 29, 379–394. [Google Scholar] [CrossRef]
- Hasnulin, V.I.; Hasnulina, A.V. Psycho-emotional stress and meteoreacton as systemic manifestations of human disadaptation under changing climatic conditions in the North of Russia. Ekol. Cheloveka (Hum. Ecol.) 2012, 19, 3–7. [Google Scholar]
- Palinkas, L.A.; Fuentes, D.; Finno, M.; Garcia, A.; Holloway, I.W.; Chamberlain, P. Inter-organizational collaboration in the implementation of evidence-based practices among public agencies serving abused and neglected youth. Adm. Policy Ment. Health 2014, 41, 74–85. [Google Scholar] [CrossRef] [PubMed]
- Park, D.H.; Kripke, D.F.; Cole, R.J. More prominent reactivity in mood than activity and sleep induced by differential light exposure due to seasonal and local differences. Chronobiol. Int. 2007, 24, 905–920. [Google Scholar] [CrossRef] [PubMed]
- Honma, K.; Honma, S.; Nakamura, K.; Sasaki, M.; Endo, T.; Takahashi, T. Differential effects of bright light and social cues on reentrainment of human circadian rhythms. Am. J. Physiol. 1995, 268, R528–R535. [Google Scholar] [CrossRef] [PubMed]
- Duffy, J.F.; Kronauer, R.E.; Czeisler, C.A. Phase-shifting human circadian rhythms: Influence of sleep timing, social contact and light exposure. J. Physiol. 1996, 15, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Diekelmann, S.; Born, J. The memory function of sleep. Nat. Rev. Neurosci. 2010, 11, 114–126. [Google Scholar] [CrossRef] [PubMed]
- Crowley, S.J.; Acebo, C.; Carskadon, M.A. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Med. 2007, 8, 602–612. [Google Scholar] [CrossRef]
- Fallone, G.; Seifer, R.; Acebo, C.; Carskadon, M.A. How well do school-aged children comply with imposed sleep schedules at home? Sleep 2002, 25, 739–745. [Google Scholar] [CrossRef]
- Sadeh, A.; Mindell, J.; Rivera, L. “My child has a sleep problem”: A cross-cultural comparison of parental definitions. Sleep Med. 2011, 12, 478–482. [Google Scholar] [CrossRef]
- Dorofaeff, T.; Bandini, R.M.; Lipman, J.; Ballot, D.E.; Roberts, J.A.; Parker, S.L. Uncertainty in Antibiotic Dosing in Critically Ill Neonate and Pediatric Patients: Can Microsampling Provide the Answers? Clin. Ther. 2016, 38, 1961–1975. [Google Scholar] [CrossRef]
- Wittmann, M.; Dinich, J.; Merrow, M.; Roenneberg, T. Social jetlag: Misalignment of biological and social time. Chronobiol. Int. 2006, 23, 497–509. [Google Scholar] [CrossRef]
- Walch, O.J.; Cochran, A.; Forger, D.B. A global quantification of “normal” sleep schedules using smartphone data. Sci. Adv. 2016, 2, e1501705. [Google Scholar] [CrossRef] [PubMed]
- Friborg, O.; Bjorvatn, B.; Amponsah, B. Associations between seasonal variations in day length (photoperiod), sleep timing, sleep quality and mood: A comparison between Ghana (5 degrees) and Norway (69 degrees). J. Sleep Res. 2012, 21, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Miguel, M.; Oliveira, V.C.; Pereira, D.; Pedrazzoli, M. Detecting chronotype differences associated to latitude: A comparison between Horne--Östberg and Munich Chronotype questionnaires. Ann. Hum. Biol. 2014, 41, 105–108. [Google Scholar] [CrossRef] [PubMed]
- Randler, C. Morningness-eveningness comparison in adolescents from different countries around the world. Chronobiol. Int. 2008, 25, 1017–1028. [Google Scholar] [CrossRef]
- Tonetti, L.; Fabbri, M.; Martoni, M.; Natale, V. Circadian type and mood seasonality in adolescents. Psychiatry Clin. Neurosci. 2012, 66, 157–159. [Google Scholar] [CrossRef]
- Benedito-Silva, A.A.; Pires, M.L.; Calil, H.M. Seasonal variation of suicide in Brazil. Chronobiol. Int. 2007, 24, 727–737. [Google Scholar] [CrossRef]
- Borisenkov, M.F.; Perminova, E.V.; Kosova, A.L. Chronotype, sleep length, and school achievement of 11-to 23-year-old students in northern European Russia. Chronobiol. Int. 2010, 27, 1259–1270. [Google Scholar] [CrossRef]
- Masal, E.; Randler, C.; Beşoluk, Ş.; Önder, İ.; Horzum, M.B.; Vollmer, C. Effects of longitude, latitude and social factors on chronotype in Turkish students. Pers. Individ. Differ. 2015, 86, 73–81. [Google Scholar] [CrossRef]
- Sluggett, L.; Wagner, S.L.; Hardy, C.; Harris, R.L. Associations between Sleep Duration and Indicators of Cardiometabolic Disease in Canadian Children and Adolescents: Analyses of the 2007–2009 Canadian Health Measures Survey. Child. Obes. 2016, 12, 325–333. [Google Scholar] [CrossRef]
- Sayin, F.K.; Buyukinan, M. Sleep Duration and Media Time Have a Major Impact on Insulin Resistance and Metabolic Risk Factors in Obese Children and Adolescents. Child. Obes. 2016, 12, 272–278. [Google Scholar] [CrossRef] [PubMed]
- Simon, S.L.; Field, J.; Miller, L.E.; DiFrancesco, M.; Beebe, D.W. Sweet/dessert foods are more appealing to adolescents after sleep restriction. PLoS ONE 2015, 10, e0115434. [Google Scholar] [CrossRef] [PubMed]
- Schneider, A.M.; Randler, C. Daytime sleepiness during transition into daylight saving time in adolescents: Are owls higher at risk? Sleep Med. 2009, 10, 1047–1050. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.M.; Lin, F.W.; Spielman, A.J. A standard procedure enhances the correlation between subjective and objective measures of sleepiness. Sleep 2004, 27, 329–332. [Google Scholar] [CrossRef][Green Version]
- Boulos, M.I.; Murray, B.J. Current evaluation and management of excessive daytime sleepiness. Can. J. Neurol. Sci. 2010, 37, 167–176. [Google Scholar] [CrossRef]
- Qureshi, A.I.; Giles, W.H.; Croft, J.B.; Bliwise, D.L. Habitual sleep patterns and risk for stroke and coronary heart disease: A 10-year follow-up from NHANES I. Neurology 1997, 48, 904–911. [Google Scholar] [CrossRef]
- Dedov, I.I.; Shestakova, M.V.; Vikulova, O.K.; Zheleznyakova, A.V.; Isakov, M.A.; Sazonova, D.V.; Mokrysheva, N.G. Diabetes mellitus in the Russian Federation: Dynamics of epidemiological indicators according to the Federal Register of Diabetes Mellitus for the period 2010–2022. Diabetes Mellit. 2023, 26, 104–123. [Google Scholar] [CrossRef]
- Roenneberg, T.; Chua, E.J.; Bernardo, R.; Mendoza, E. Modelling biological rhythms. Curr. Biol. 2008, 18, R826–R835. [Google Scholar] [CrossRef] [PubMed]
- Borisenkov, M.F.; Kosova, A.L.; Kasyanova, O.N. Impact of perinatal photoperiod on the chronotype of 11 to 18-year-olds in northern European Russia. Chronobiol. Int. 2012, 29, 305–310. [Google Scholar] [CrossRef]
- Drake, C.; Nickel, C.; Burduvali, E.; Roth, T.; Jefferson, C.; Pietro, B. The pediatric daytime sleepiness scale (PDSS): Sleep habits and school outcomes in middle-school children. Sleep 2003, 26, 455–458. [Google Scholar]
- Randler, C.; Kolomeichuk, S.N.; Morozov, A.V.; Petrashova, D.A.; Pozharskaya, V.V.; Martynova, A.A.; Korostovtseva, L.S.; Bochkarev, M.V.; Sviryaev, Y.V.; Polouektov, M.G.; et al. Psychometric properties of the Russian version of the Pediatric Daytime Sleepiness Scale (PDSS). Heliyon 2019, 5, e02134. [Google Scholar] [CrossRef]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Rasskazova, E.I. Violations of Psychological Self-Regulation in Neurotic Insomnia. Ph.D. Thesis, Moscow State University, Moscow, Russia, 2008. (In Russian). [Google Scholar]
- LeBourgeois, M.K.; Giannotti, F.; Cortesi, F.; Wolfson, A.R.; Harsh, J. The relationship between reported sleep quality and sleep hygiene in Italian and American adolescents. Pediatrics 2005, 115, 257–265. [Google Scholar] [CrossRef]
- Aschoff, J.; Pohl, H. Phase relations between a circadian rhythm and its zeitgeber within the range of entrainment. Naturwissenschaften 1978, 65, 80–84. [Google Scholar] [CrossRef]
- Roenneberg, T.; Pilz, L.K.; Zerbini, G.; Winnebeck, E.C. Chronotype and Social Jetlag: A (Self-) Critical Review. Biology 2019, 8, 54. [Google Scholar] [CrossRef]
- Lewandowski, A.S.; Ward, T.M.; Palermo, T.M. Sleep problems in children and adolescents with common medical conditions. Pediatr. Clin. N. Am. 2011, 58, 699–713. [Google Scholar] [CrossRef]
- Spruyt, K.; Gozal, D. Sleep disturbances in children with attention-deficit/hyperactivity disorder. Expert Rev. Neurother. 2011, 11, 565–577. [Google Scholar] [CrossRef] [PubMed]
- Pallesen, S.; Hetland, J.; Sivertsen, B.; Samdal, O.; Torsheim, T.; Nordhus, I.H. Time trends in sleep-onset difficulties among Norwegian adolescents: 1983–2005. Scand. J. Public Health 2008, 36, 889–895. [Google Scholar] [CrossRef] [PubMed]
- Kronholm, E.; Puusniekka, R.; Jokela, J.; Villberg, J.; Urrila, A.S.; Paunio, T.; Välimaa, R.; Tynjälä, J. Trends in self-reported sleep problems, tiredness and related school performance among Finnish adolescents from 1984 to 2011. J. Sleep Res. 2015, 24, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Touitou, Y.; Reinberg, A.; Touitou, D. Association between light at night, melatonin secretion, sleep deprivation, and the internal clock: Health impacts and mechanisms of circadian disruption. Life Sci. 2017, 173, 94–106. [Google Scholar] [CrossRef]
- Touitou, Y. The double face of light effects: Circadian adjustment or disruption. J. Basic Clin. Physiol. Pharmacol. 2017, 28, 293–294. [Google Scholar] [CrossRef]
- Gubin, D.; Weinert, D. Melatonin, circadian rhythms and glaucoma: Current perspective. Neural Regen. Res. 2022, 17, 1759–1760. [Google Scholar] [CrossRef] [PubMed]
- Gubin, D.G.; Weinert, D.; Rybina, S.V.; Danilova, L.A.; Solovieva, S.V.; Durov, A.M.; Prokopiev, N.Y.; Ushakov, P.A. Activity, sleep and ambient light have a different impact on circadian blood pressure, heart rate and body temperature rhythms. Chronobiol. Int. 2017, 34, 632–649. [Google Scholar] [CrossRef] [PubMed]
- Maury, E.; Brichard, S.M.; Pataky, Z.; Carpentier, A.; Golay, A.; Bobbioni-Harsch, E. Effect of obesity on growth-related oncogene factor-alpha, thrombopoietin, and tissue inhibitor metalloproteinase-1 serum levels. Obesity 2010, 18, 1503–1509. [Google Scholar] [CrossRef]
- Fonken, L.K.; Workman, J.L.; Walton, J.C.; Weil, Z.M.; Morris, J.S.; Haim, A.; Nelson, R.J. Light at night increases body mass by shifting the time of food intake. Proc. Natl. Acad. Sci. USA 2010, 107, 18664–18669. [Google Scholar] [CrossRef] [PubMed]
- Kooijman, S.; van den Berg, R.; Ramkisoensing, A.; Boon, M.R.; Kuipers, E.N.; Loef, M.; Zonneveld, T.C.; Lucassen, E.A.; Sips, H.C.; Chatzispyrou, I.A.; et al. Prolonged daily light exposure increases body fat mass through attenuation of brown adipose tissue activity. Proc. Natl. Acad. Sci. USA 2015, 112, 6748–6753. [Google Scholar] [CrossRef]
- Casiraghi, L.P.; Alzamendi, A.; Giovambattista, A.; Chiesa, J.J.; Golombek, D.A. Effects of chronic forced circadian desynchronization on body weight and metabolism in male mice. Physiol. Rep. 2016, 4, e12743. [Google Scholar] [CrossRef]
- Gale, J.T.; Martinez-Rubio, C.; Sheth, S.A.; Eskandar, E.N. Intra-operative behavioral tasks in awake humans undergoing deep brain stimulation surgery. J. Vis. Exp. 2011, 6, 2156. [Google Scholar]
- Simko, F.; Paulis, L. Antifibrotic effect of melatonin-perspective protection in hypertensive heart disease. Int. J. Cardiol. 2013, 168, 2876–2877. [Google Scholar] [CrossRef]
- Merikanto, I.; Lahti, T.; Puolijoki, H.; Vanhala, M.; Peltonen, M.; Laatikainen, T.; Vartiainen, E.; Salomaa, V.; Kronholm, E.; Partonen, T. Associations of chronotype and sleep with cardiovascular diseases and type 2 diabetes. Chronobiol. Int. 2013, 30, 470–477. [Google Scholar] [CrossRef] [PubMed]
- Gupta, P.; Sagar, R.; Mehta, M. Subjective sleep problems and sleep hygiene among adolescents having depression: A case-control study. Asian J. Psychiatr. 2019, 44, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Kolomeichuk, S.N.; Randler, C.; Morozov, A.V.; Gubin, D.G.; Drake, C.L. Social Jetlag and Excessive Daytime Sleepiness from a Sample of Russian Children and Adolescents. Nat. Sci. Sleep 2021, 13, 729–737. [Google Scholar] [CrossRef]
- Kolomeichuk, S.N.; Morozov, A.V.; Petrashova, D.A.; Pozharskaya, V.V.; Stafeeva, E.B.; Vinogradova, I.A.; Bochkarev, M.V.; Tarasov, B.A. Daytime sleepiness and sleep parameters in children living in the European north of Russia. Yakut Med. J. 2019, 3, 88–90. [Google Scholar] [CrossRef]
- Maganti, R.; Hausman, N.; Koehn, M.; Sandok, E.; Glurich, I.; Mukesh, B.N. Excessive daytime sleepiness and sleep complaints among children with epilepsy. Epilepsy Behav. 2006, 8, 272–277. [Google Scholar] [CrossRef]
- Rhie, S.; Lee, S.; Chae, K.Y. Sleep patterns and school performance of Korean adolescents assessed using a Korean version of the pediatric daytime sleepiness scale. Korean J. Pediatr. 2011, 54, 29–35. [Google Scholar] [CrossRef]
- Yang, C.M.; Huang, Y.S.; Song, Y.C. Clinical utility of the Chinese version of the Pediatric Daytime Sleepiness Scale in children with obstructive sleep apnea syndrome and narcolepsy. Psychiatry Clin. Neurosci. 2010, 64, 134–140. [Google Scholar] [CrossRef]
- Komada, Y.; Breugelmans, R.; Drake, C.L.; Nakajima, S.; Tamura, N.; Tanaka, H.; Inoue, S.; Inoue, Y. Social jetlag affects subjective daytime sleepiness in school-aged children and adolescents: A study using the Japanese version of the Pediatric Daytime Sleepiness Scale (PDSS-J). Chronobiol. Int. 2016, 33, 1311–1319. [Google Scholar] [CrossRef]
- Li, S.; Arguelles, L.; Jiang, F.; Chen, W.; Jin, X.; Yan, C.; Tian, Y.; Hong, X.; Qian, C.; Zhang, J.; et al. Sleep, school performance, and a school-based intervention among school-aged children: A sleep series study in China. PLoS ONE 2013, 8, e67928. [Google Scholar] [CrossRef]
- Perez-Chada, D.; Perez-Lloret, S.; Videla, A.J.; Cardinali, D.; Bergna, M.A.; Fernández-Acquier, M.; Larrateguy, L.; Zabert, G.E.; Drake, C. Sleep disordered breathing and daytime sleepiness are associated with poor academic performance in teenagers. A study using the Pediatric Daytime Sleepiness Scale (PDSS). Sleep 2007, 30, 1698–1703. [Google Scholar] [CrossRef]
- Wheaton, A.G.; Chapma, D.P.; Croft, J.B. School Start Times, Sleep, Behavioral, Health, and Academic Outcomes: A Review of the Literature. J. Sch. Health 2016, 86, 363–381. [Google Scholar] [CrossRef] [PubMed]
- Zakharov, I.M.; Ismatullina, V.I.; Kolyasnikov, P.V.; Marakshina, J.A.; Malykh, A.S.; Tabueva, A.O.; Adamovich, T.V.; Lobaskova, M.M.; Malykh, S.B. An Independent Evaluation of the Psychometric Properties of the Russian Version of the Pediatric Daytime Sleepiness Scale (PDSS). Psychol. Russ. 2023, 16, 206–221. [Google Scholar] [CrossRef] [PubMed]


| No | Settlements | Geographic Coordinates | Population, Persons * | N, Persons | Girls | Boys |
|---|---|---|---|---|---|---|
| 1 | Kem’ (Northern Karelia) | 64°57′ N 34°34′ E | 11,000 | 38 | 24 | 14 |
| 2 | Apatity (Murmansk Region) | 67°34′ N 33°23′ E | 55,000 | 56 | 32 | 24 |
| Total | 94 | 56 | 38 |
| Variable | N | Total Sample | Kem’, N = 38 | Apatity, N = 56 | p-Level/X2/Degrees of Freedom |
|---|---|---|---|---|---|
| Age, years | 94 | 14.34 (13; 15) | 14.26 (13; 15) | 14.39 (13; 15) | p = 0.154 |
| Sex, males/females, %males a | 94 | 38/56 (40.4%) | 14/24 (36.8%) | 24/32 (42.86%) | p = 0.34; X2 = 0.56 df = 1 |
| Height, cm | 76 | 165 (130; 190) | 165 (130; 182) | 165 (152; 190) | p = 0.39 |
| Weight, kg | 75 | 55 (26; 110) | 52 (26; 87) | 56.5 (35; 110) | p = 0.16 |
| BMI, kg/m2 | 75 | 19.8 (13.2; 40.4) | 20.1 (13.2; 29.1) | 19.8 (14.4; 40.4) | p = 0.35 |
| Physical activity, yes/no a | 93 | 73 (78%) | 35 (92%) | 38 (67.9%) | p = 0.008 **; X2 = 7.051 df = 1 |
| Alcohol consumption c Never Rarely Once a week Every day | 94 | 81 (87.1%) 8 (8.6%) 5 (4.3%) 0 | 35 (92.1%) 1 (2.6%) 2 (5.3%) 0 | 46 (82.14%) 7 (12.5%) 3 (5.36%) 0 | p < 0.001 ** X2 = 11.91 df = 1 |
| Smoking, yes/no | 93 | 8 (8.5%) | 5 (13.2%) | 3 (5.4%) | p = 0.19 |
| Number of study days per week, 5 or 6 b | 94 | 5 (40.4%) 6 (59.6%) | 5 | 6 | p < 0.001 ** |
| Academic success, average score (1–5) | 94 | 4.4 (3; 5) | 4.4 (3; 5) | 3.6 (3; 5) | p = 0.20 |
| Variable | N | Total Sample | Kem’ | Apatity | p-Value |
|---|---|---|---|---|---|
| Sleep latency on schooldays, min | 89 | 15 (0; 300) | 20 (2; 300) | 15 (0; 90) | 0.19 |
| Sleep latency on the weekend, min | 88 | 15 (0; 300) | 15 (2; 300) | 15 (0; 60) | 0.20 |
| Bedtime on weekend Before 10:00 p.m. After 10:00 p.m. | 89 | 7 (7.9%) 82 (92.1%) | 5 (13.2%) 33 (86.8%) | 2 (3.9%) 49 (96.1%) | 0.13 |
| Bedtime on schooldays Before 10:00 p.m. 10:00–11:59 p.m. After 00:00 a.m. | 89 | 16 (18.0%) 59 (66.2%) 14 (15.8%) | 10 (26.3) 25 (65.8%) 3 (7.9%) | 6 (11.8%) 34 (66.7%) 11 (21.6%) | 0.024 * Χ2 = 4.11 |
| Sleep duration on schooldays, h | 85 | 7.58 ± 1.27 | 7.47 ± 1.38 | 7.66 ± 1.17 | 0.52 |
| Sleep duration on the weekend, h | 84 | 9.20 ± 1.97 | 9.08 ± 2.36 | 9.30 ± 1.61 | 0.96 |
| Daylight exposure on schooldays, min | 94 | 285 (0; 600) | 300 (60; 600) | 270 (0; 630) | 0.070 |
| Daylight exposure on the weekend, min | 94 | 150 (5; 570) | 120 (20; 360) | 180 (5; 570) | 0.49 |
| Alarm on schooldays | 94 | 61 (64.9%) | 20 (52.6%) | 41 (80.4%) | 0.005 **; Χ2 = 7.782 |
| Alarm on the weekend | 94 | 6 (6.4%) | 3 (7.9%) | 3 (5.9%) | 0.71; |
| Wake-up on schooldays Before 7:00 a.m. After 7:00 a.m. | 85 | 18 (21.2%) 67 (78.8%) | 12 (31.6%) 26 (68.4%) | 6 (12.8%) 41 (87.2%) | 0.035 * Χ2 = 4.45 |
| Wake-up on weekends Before 7:00 a.m. After 7:00 a.m. | 84 | 3 (3.6%) 81 (96.4%) | 3 (7.9%) 35 (92.1%) | 0 46 (100%) | 0.089 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kolomeichuk, S.N.; Korostovtseva, L.S.; Morozov, A.V.; Bochkarev, M.V.; Sviryaev, Y.V.; Petrashova, D.A.; Pozharskaya, V.V.; Markov, A.A.; Poluektov, M.G.; Gubin, D.G. Comparative Analysis of Sleep Hygiene and Patterns among Adolescents in Two Russian Arctic Regions: A Pilot Study. Children 2024, 11, 279. https://doi.org/10.3390/children11030279
Kolomeichuk SN, Korostovtseva LS, Morozov AV, Bochkarev MV, Sviryaev YV, Petrashova DA, Pozharskaya VV, Markov AA, Poluektov MG, Gubin DG. Comparative Analysis of Sleep Hygiene and Patterns among Adolescents in Two Russian Arctic Regions: A Pilot Study. Children. 2024; 11(3):279. https://doi.org/10.3390/children11030279
Chicago/Turabian StyleKolomeichuk, Sergey N., Lyudmila S. Korostovtseva, Artem V. Morozov, Michail V. Bochkarev, Yury V. Sviryaev, Dina A. Petrashova, Victoria V. Pozharskaya, Alexander A. Markov, Michail G. Poluektov, and Denis G. Gubin. 2024. "Comparative Analysis of Sleep Hygiene and Patterns among Adolescents in Two Russian Arctic Regions: A Pilot Study" Children 11, no. 3: 279. https://doi.org/10.3390/children11030279
APA StyleKolomeichuk, S. N., Korostovtseva, L. S., Morozov, A. V., Bochkarev, M. V., Sviryaev, Y. V., Petrashova, D. A., Pozharskaya, V. V., Markov, A. A., Poluektov, M. G., & Gubin, D. G. (2024). Comparative Analysis of Sleep Hygiene and Patterns among Adolescents in Two Russian Arctic Regions: A Pilot Study. Children, 11(3), 279. https://doi.org/10.3390/children11030279