Screening of Developmental Dysplasia of the Hip in Europe: A Systematic Review
Abstract
1. Introduction
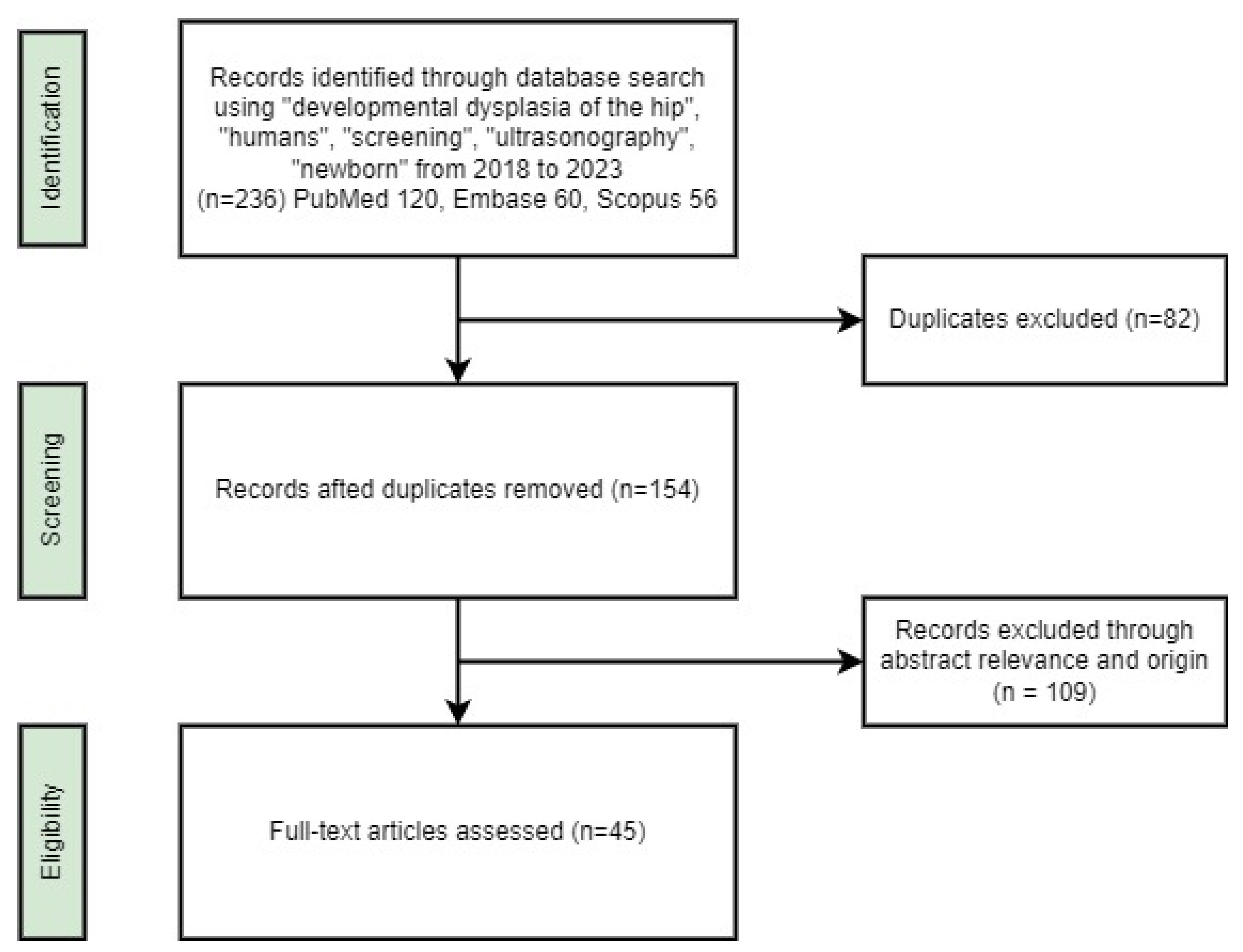
2. Materials and Methods
3. Results
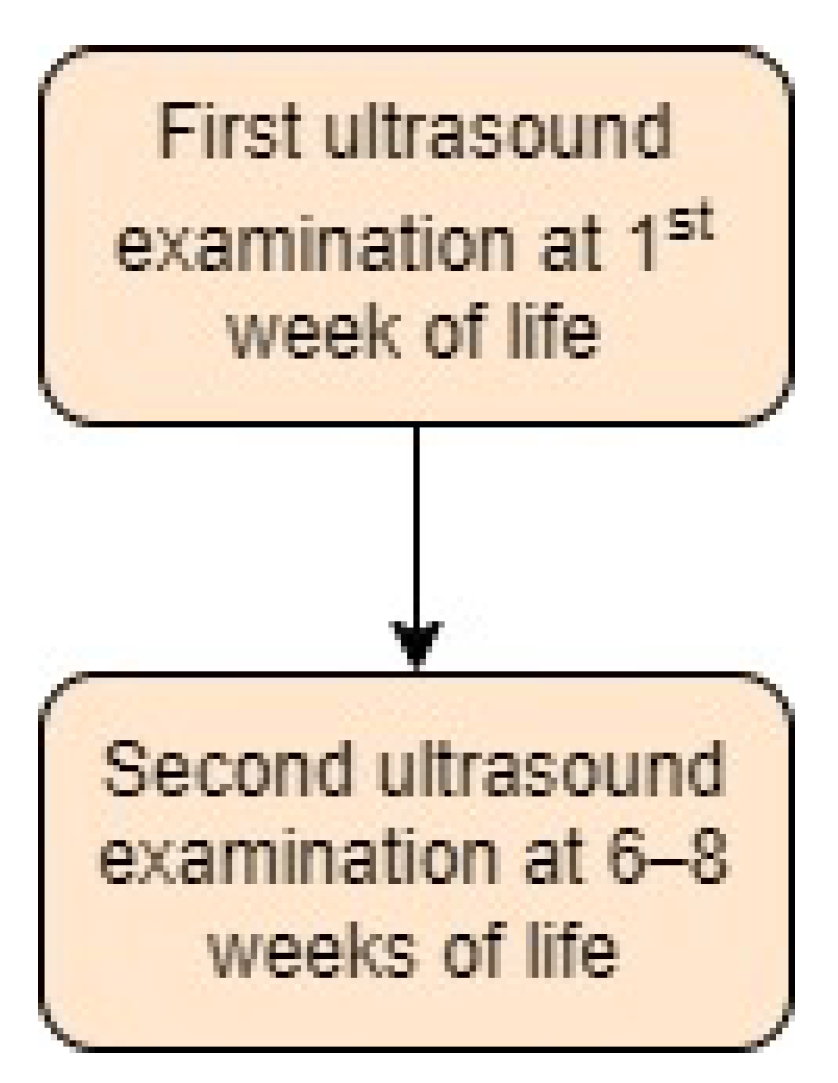
- Austria:
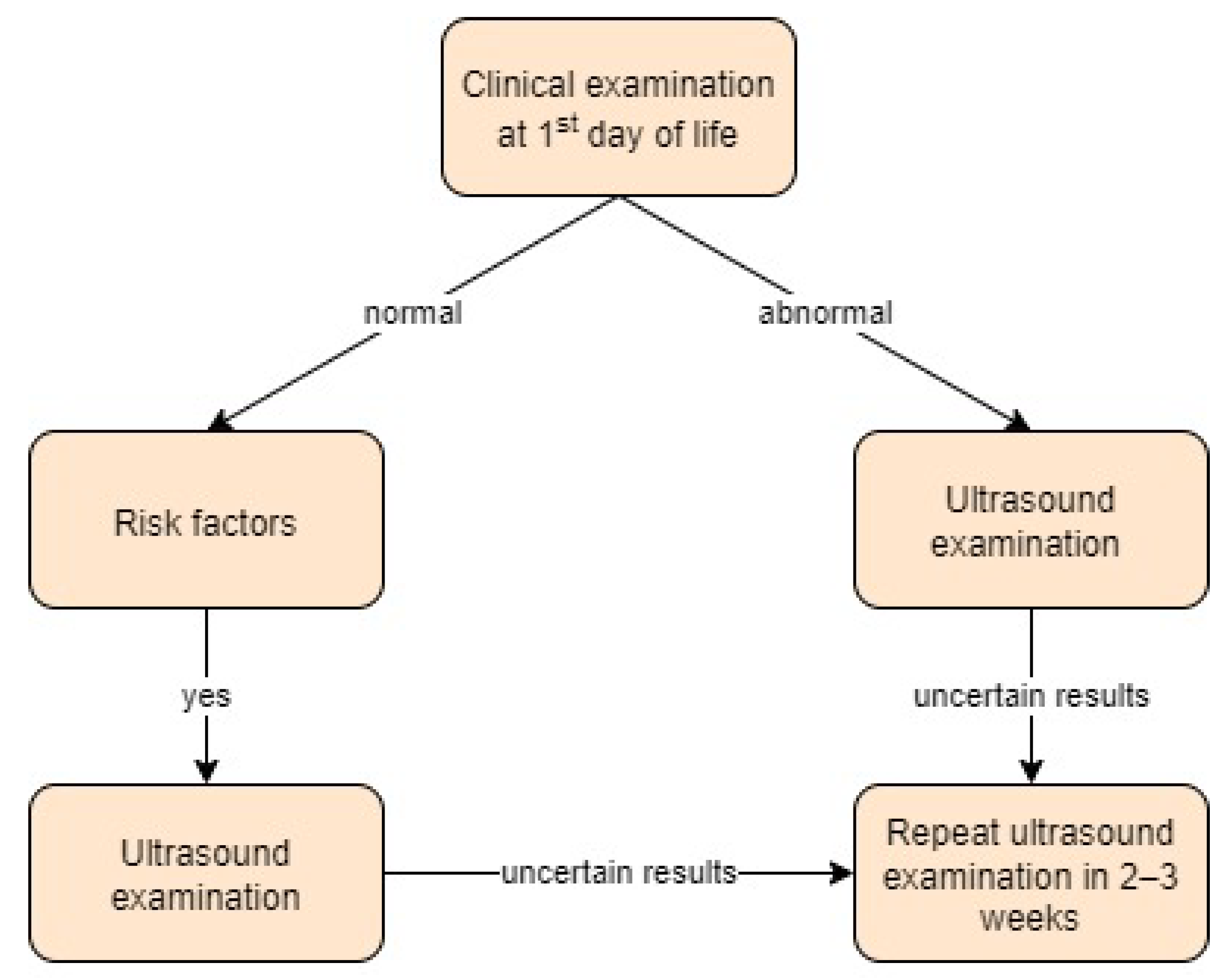
- Bosnia and Herzegovina:
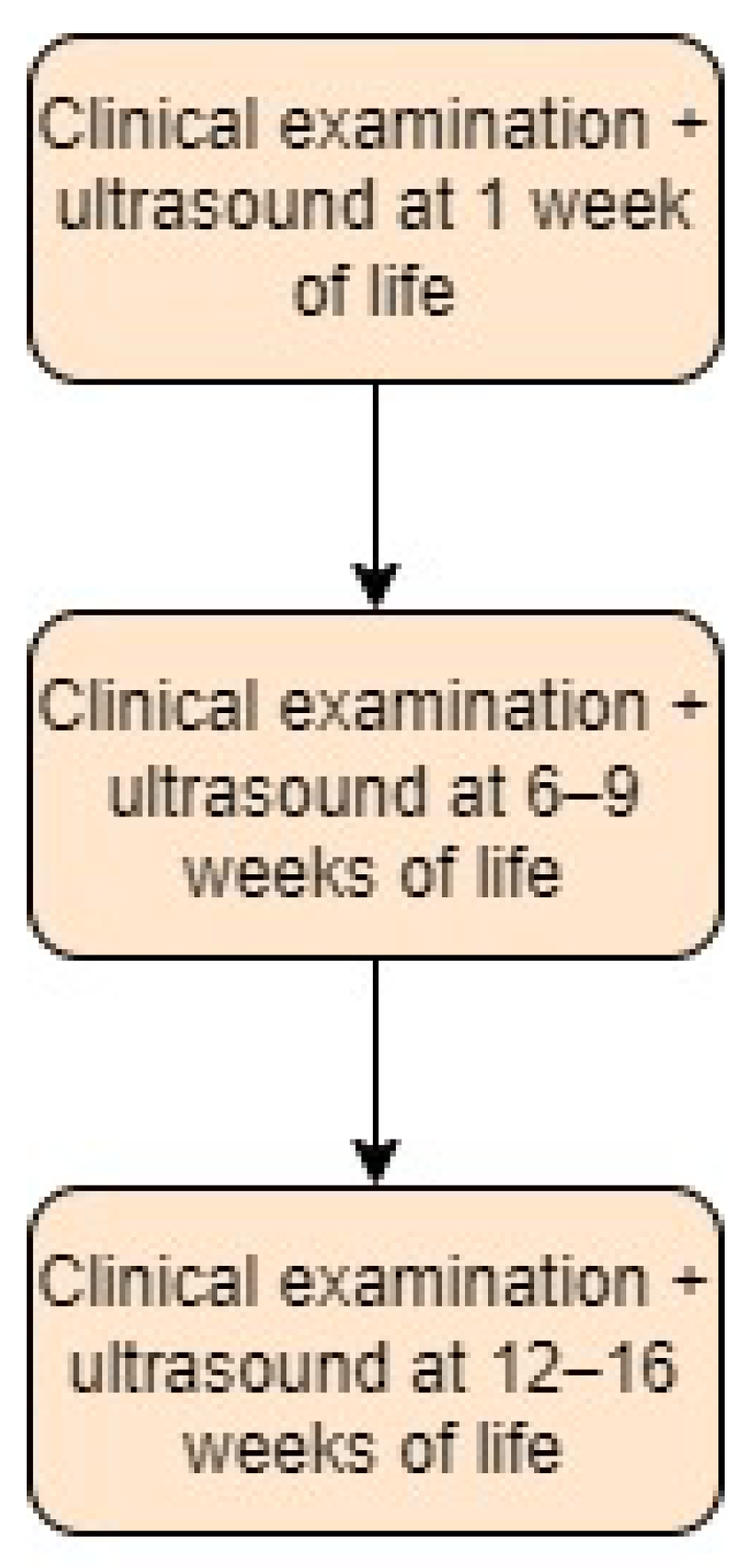
- Czech Republic:
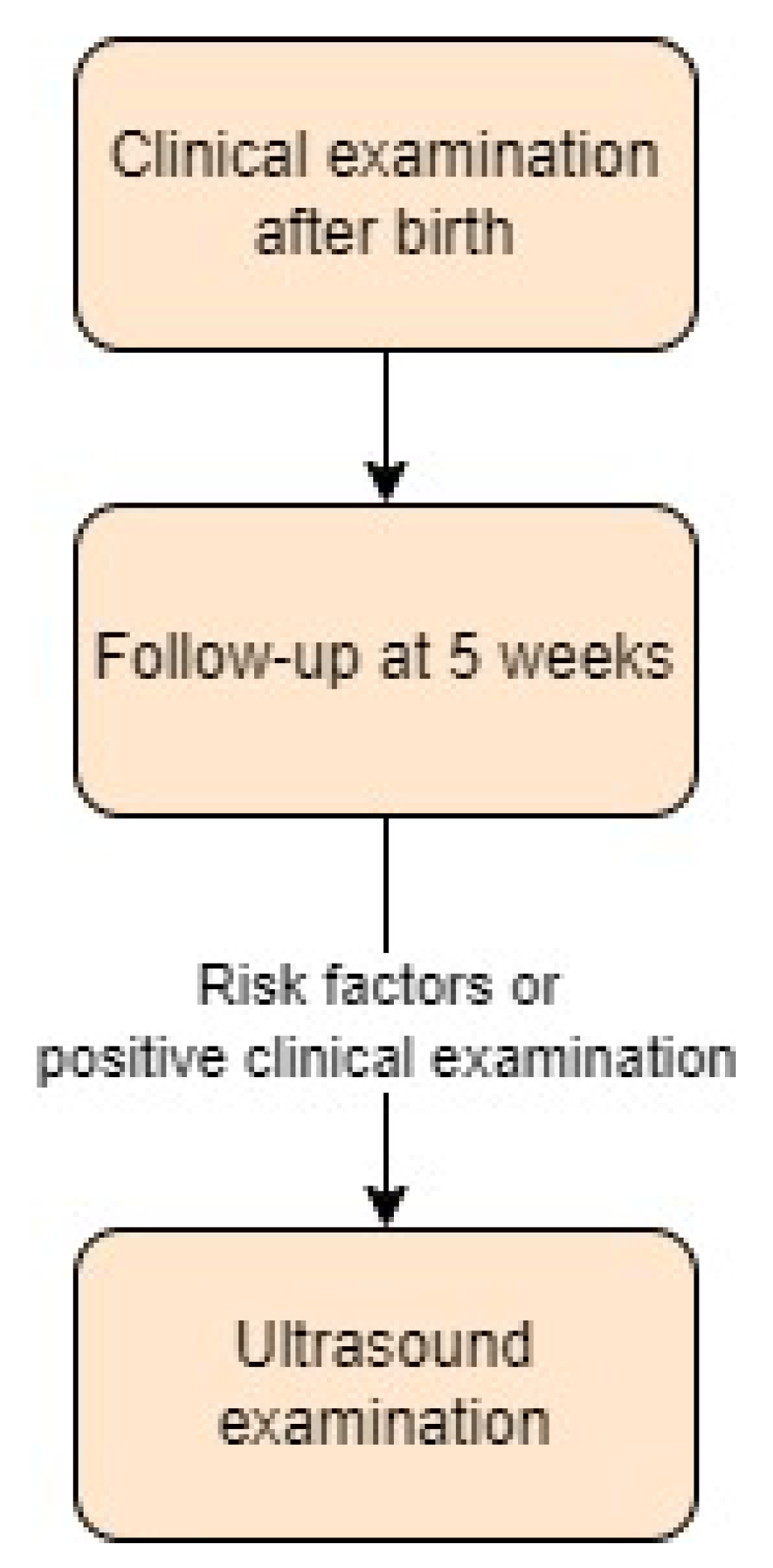
- Denmark:
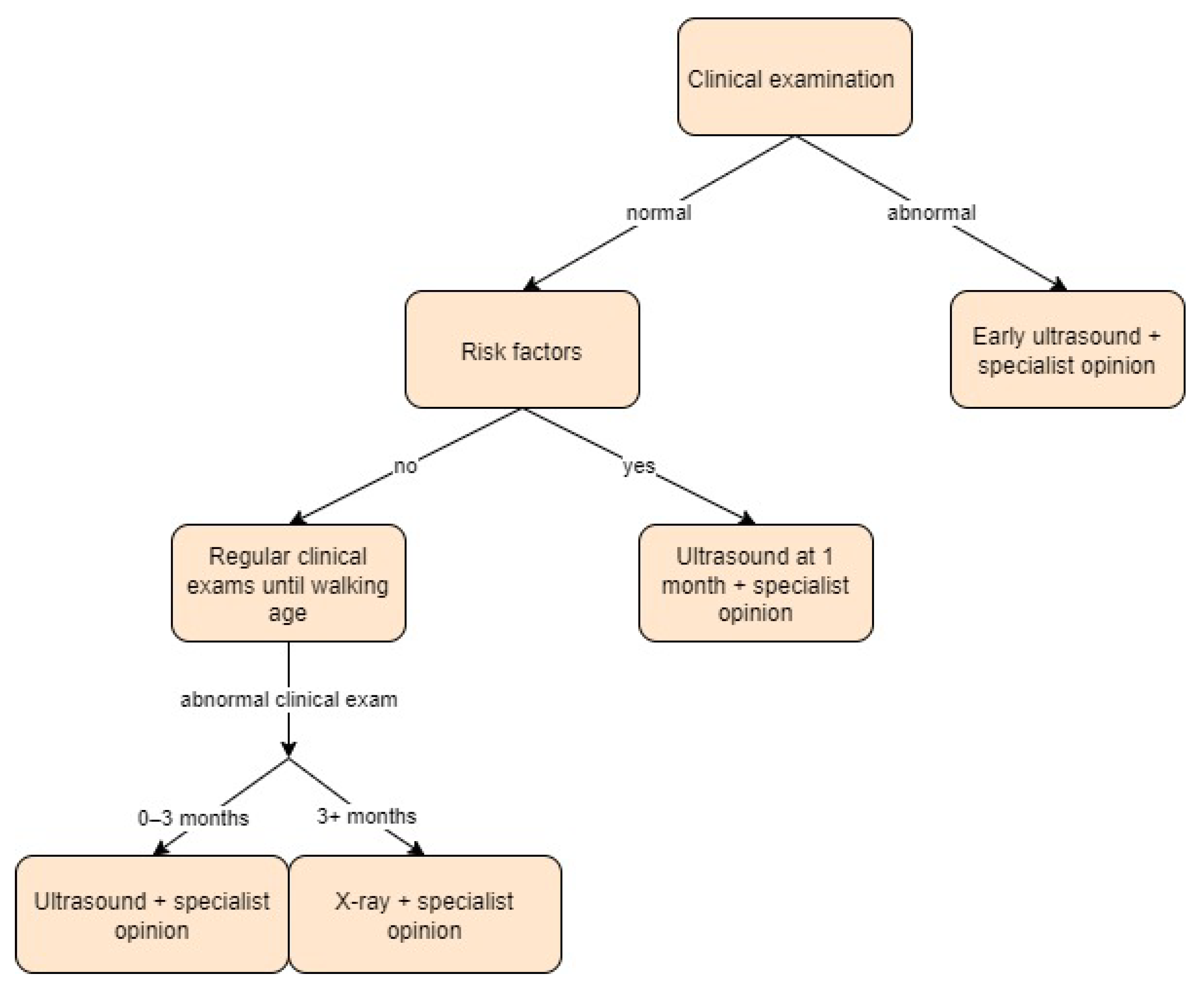
- France:
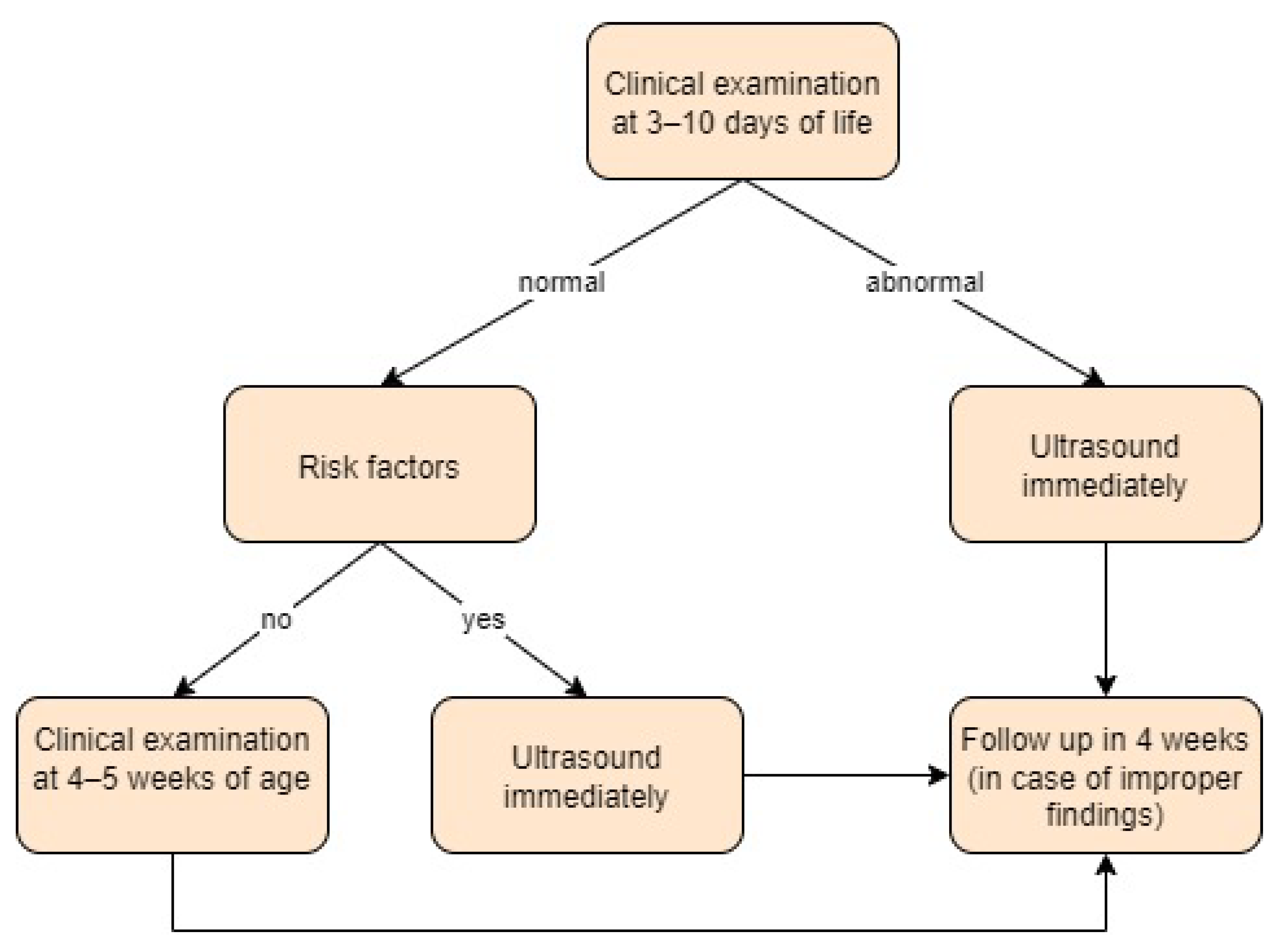
- Germany:
- Greece:
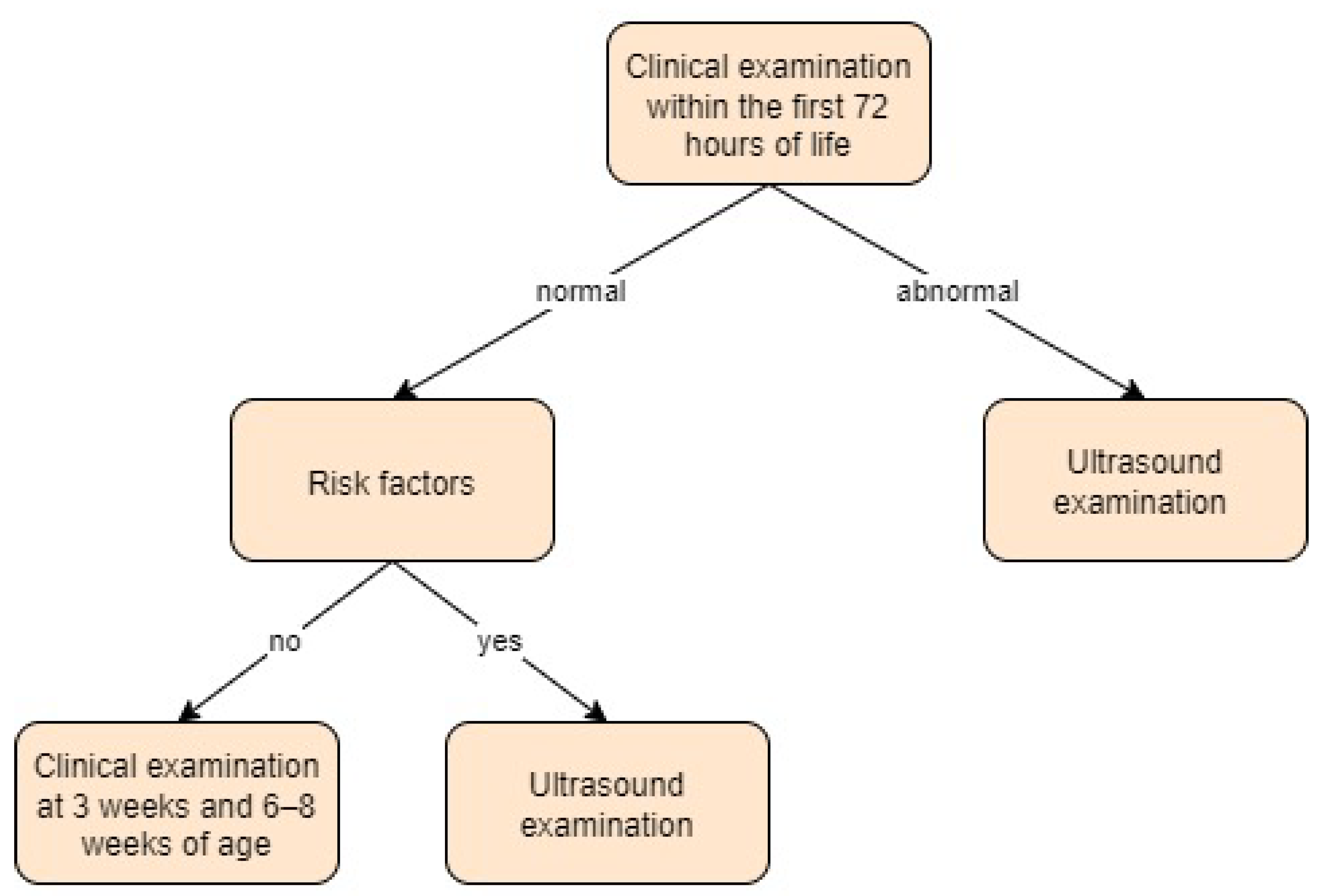
- Hungary:
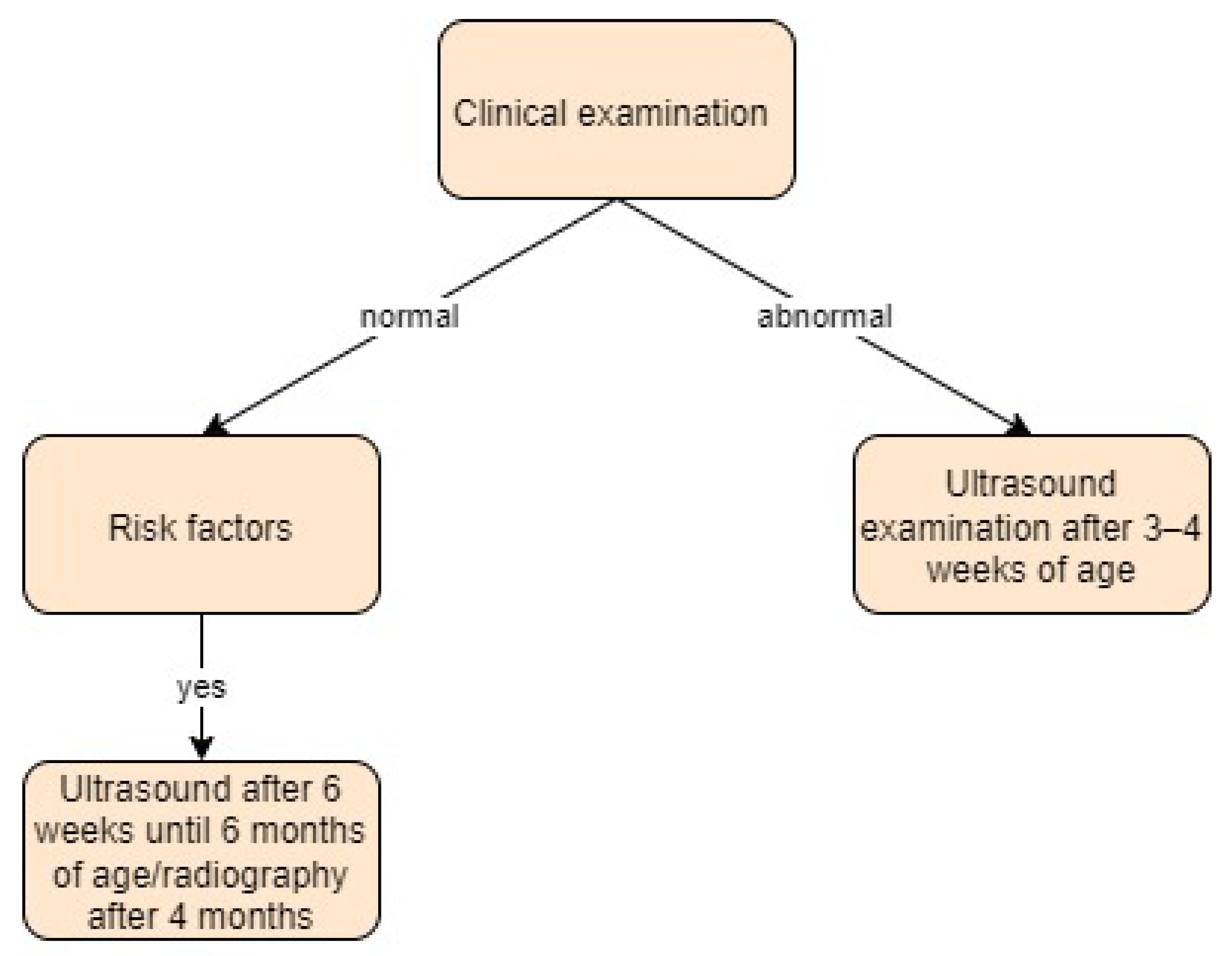
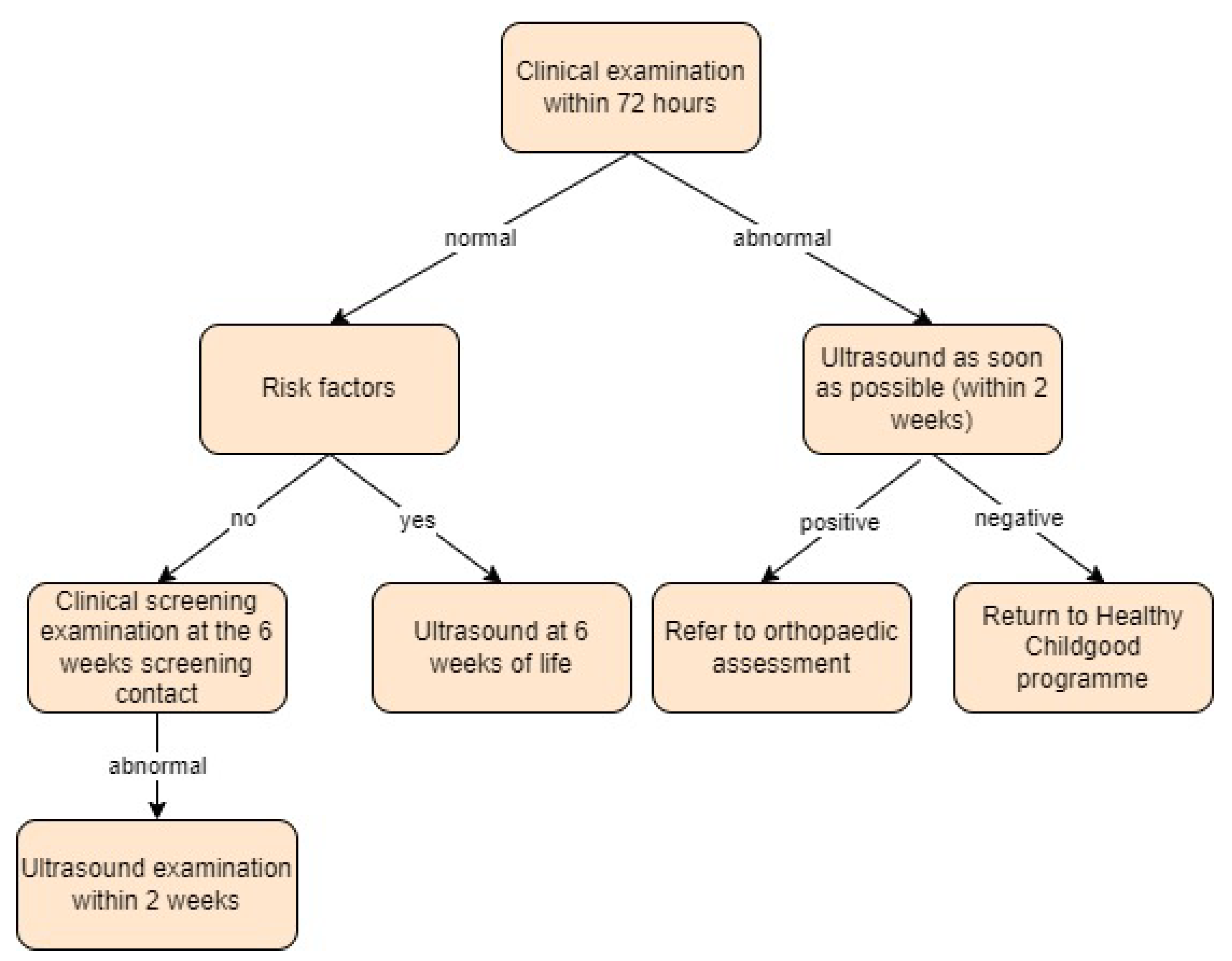
- Ireland:
- Italy:
- The Netherlands:
- Norway:
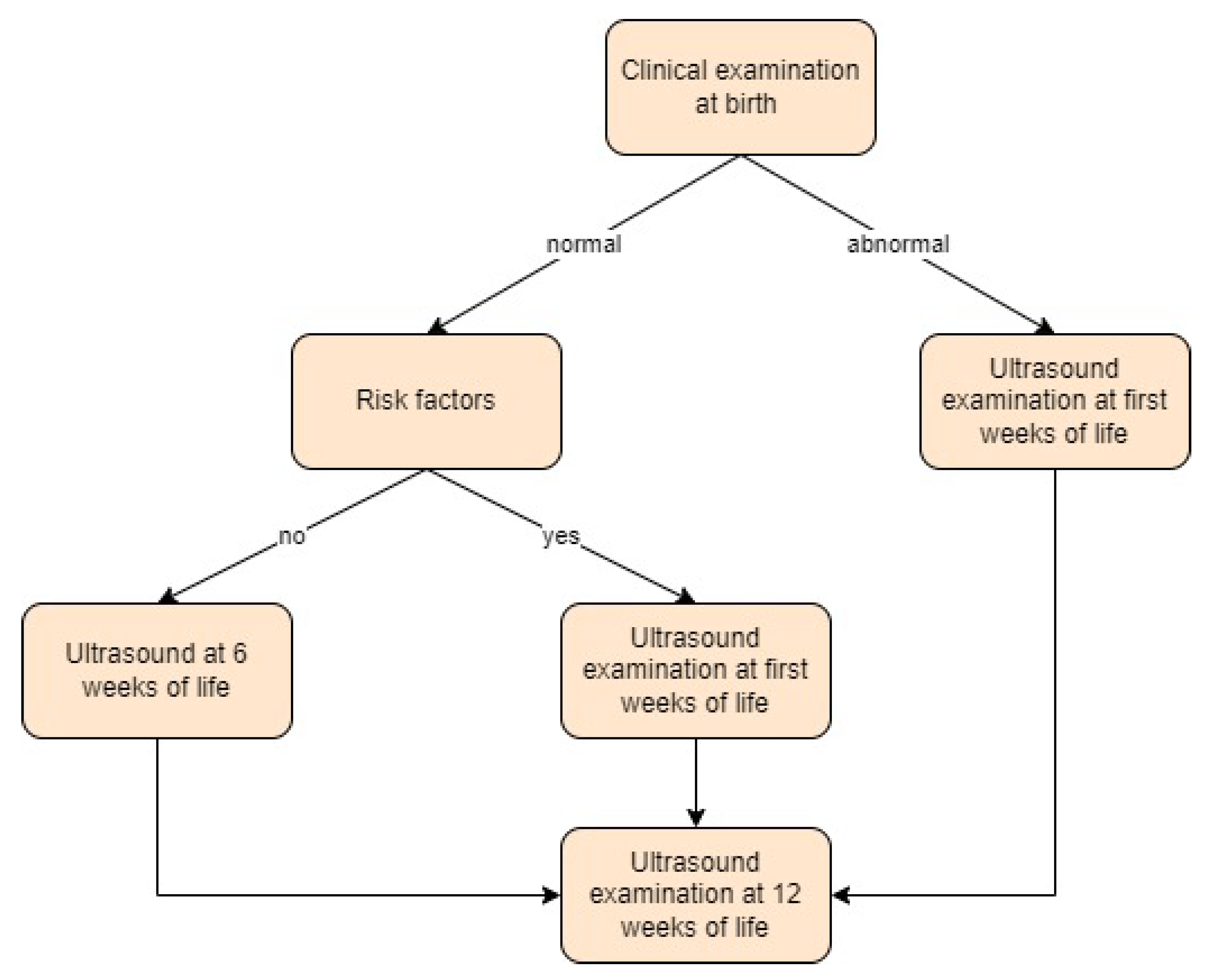
- Poland:
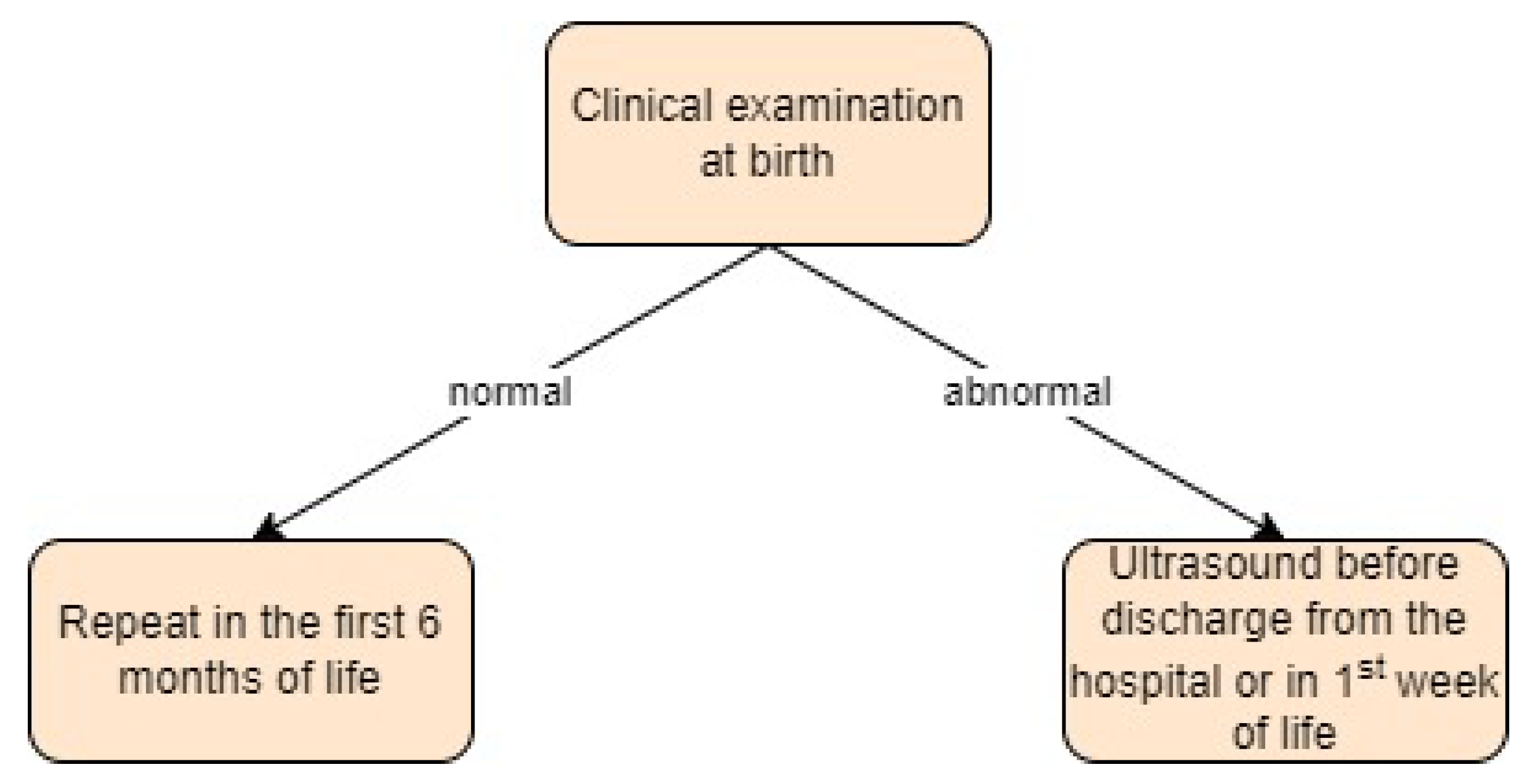
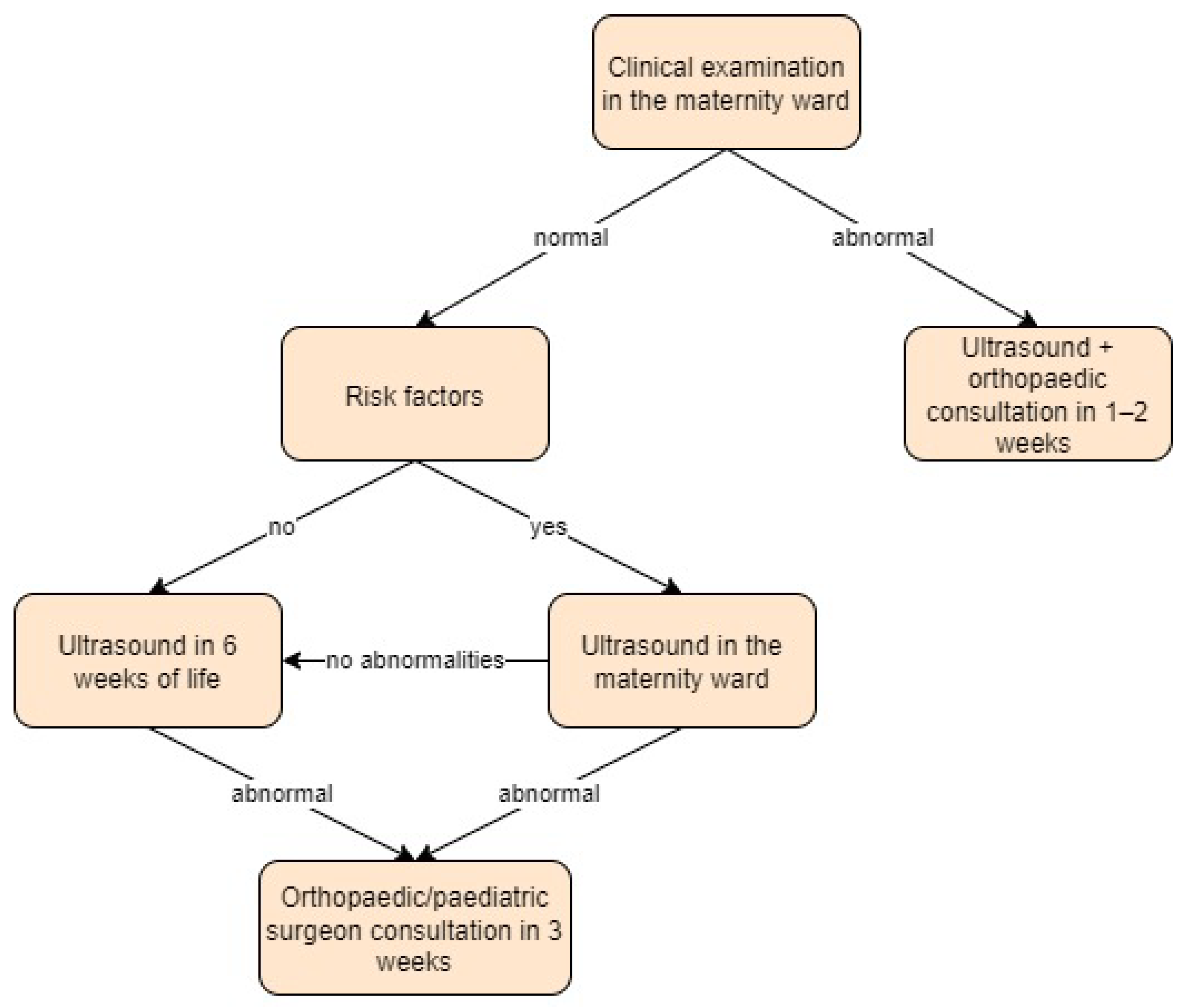
- Slovenia:
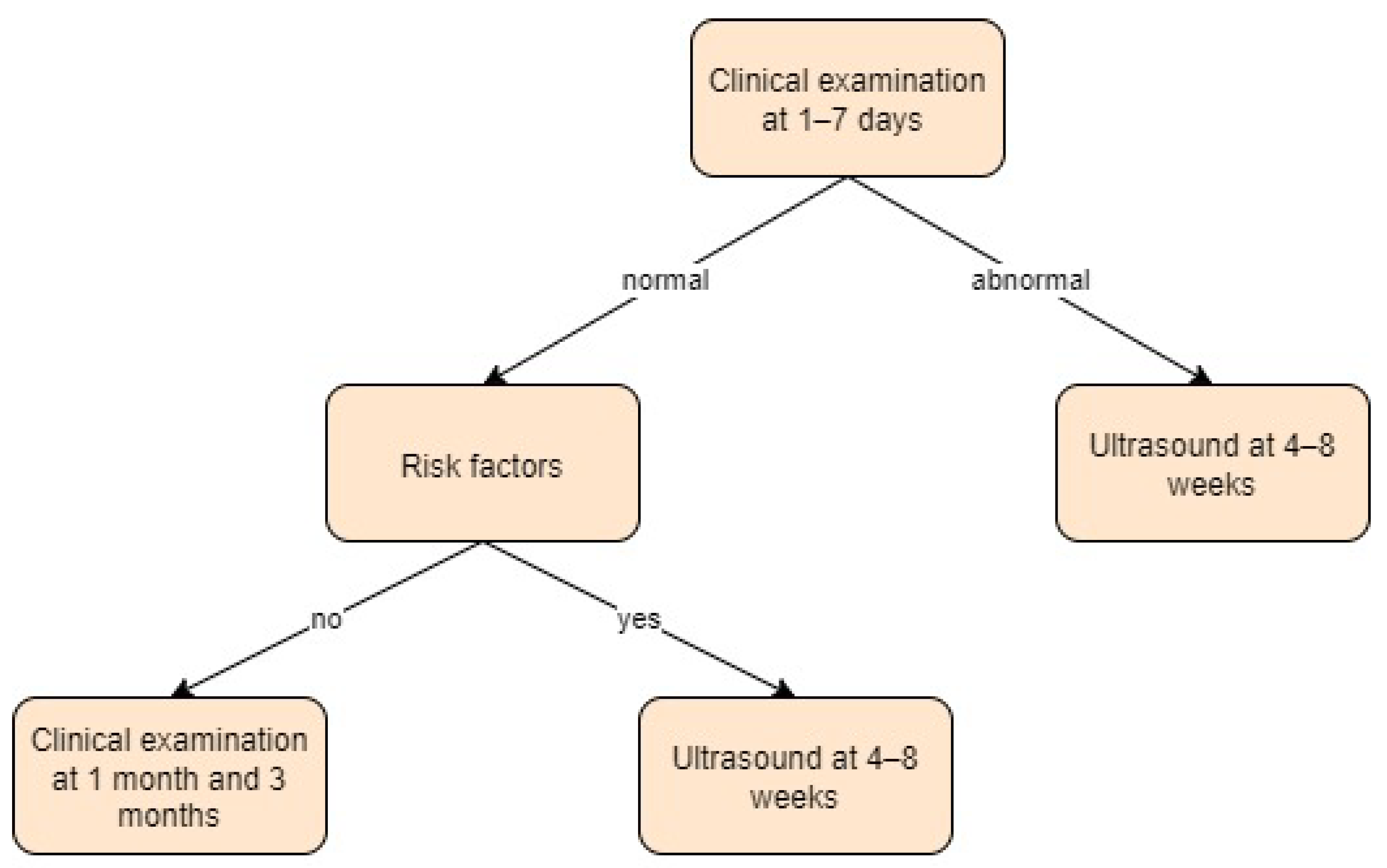
- Spain:
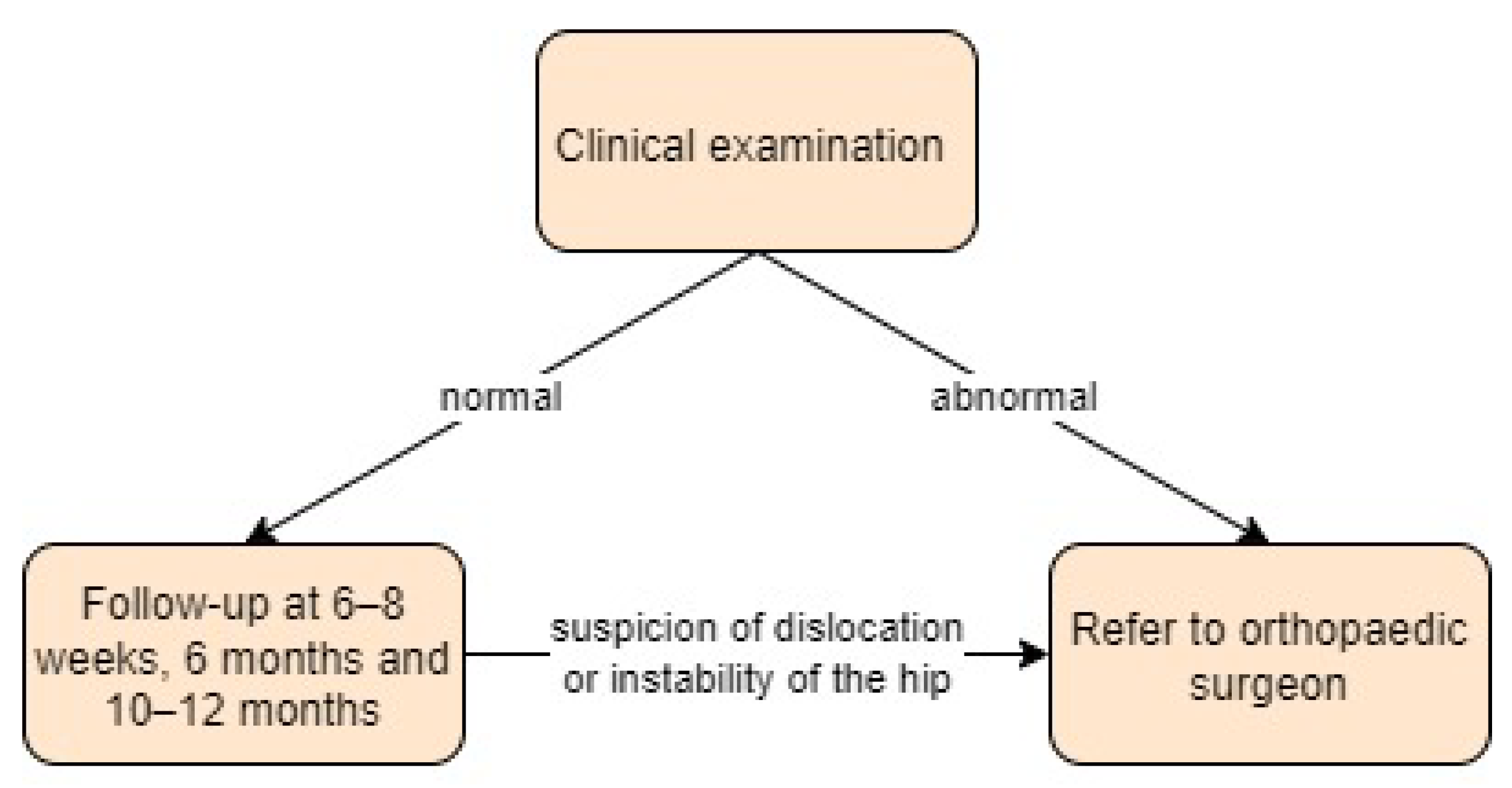
- Sweden:
- Ukraine:
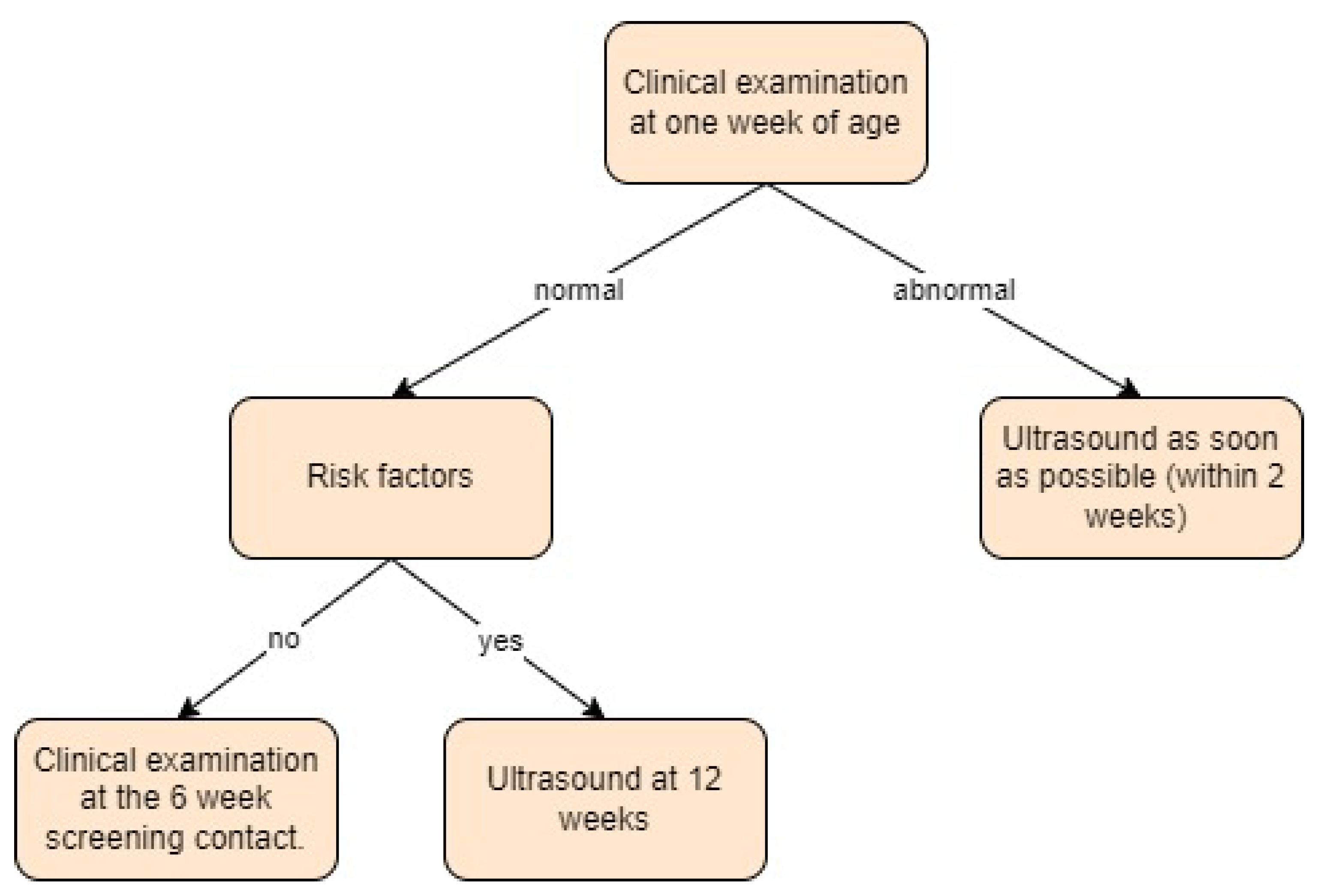
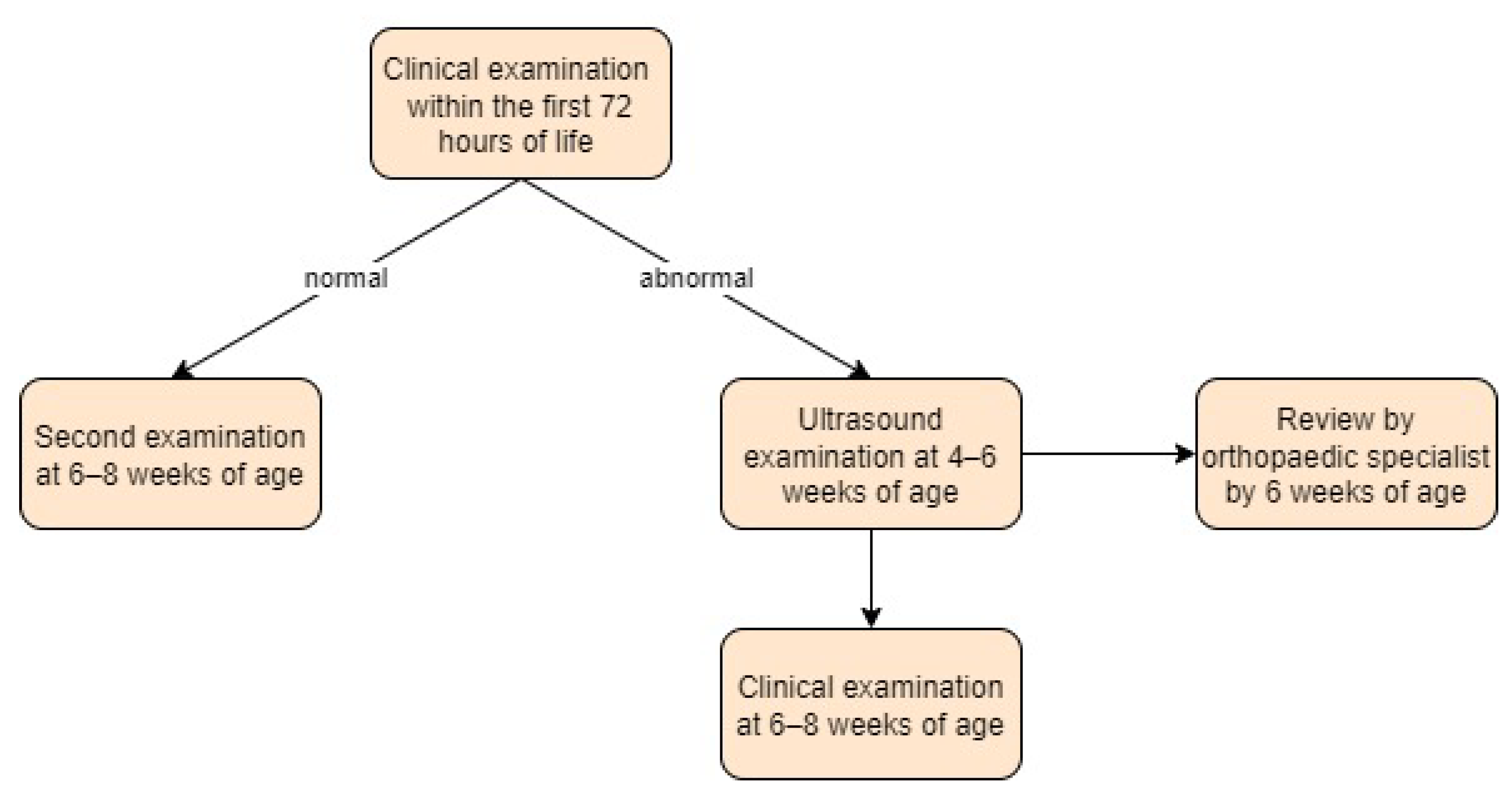
- United Kingdom:
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- O’Beirne, J.G.; Chlapoutakis, K.; Alshryda, S.; Aydingoz, U.; Baumann, T.; Casini, C.; de Pellegrin, M.; Domos, G.; Dubs, B.; Hemmadi, S.; et al. International Interdisciplinary Consensus Meeting on the Evaluation of Developmental Dysplasia of the Hip. Ultraschall Med. 2019, 40, 454–464. [Google Scholar] [CrossRef]
- Edmonds, E.W.; Hughes, J.L.; Bomar, J.D.; Brooks, J.T.; Upasani, V.V. Ultrasonography in the Diagnosis and Management of Developmental Dysplasia of the Hip. JBJS Rev. 2019, 7, e5. [Google Scholar] [CrossRef]
- Ortiz-Neira, C.L.; Paolucci, E.O.; Donnon, T. A meta-analysis of common risk factors associated with the diagnosis of developmental dysplasia of the hip in newborns. Eur. J. Radiol. 2012, 81, e344–e351. [Google Scholar] [CrossRef] [PubMed]
- De Hundt, M.; Vlemmix, F.; Bais, J.M.; Hutton, E.K.; de Groot, C.J.; Mol, B.W.; Kok, M. Risk factors for developmental dysplasia of the hip: A meta-analysis. Eur. J. Obs. Gynecol. Reprod. Biol. 2012, 165, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Loder, R.T.; Skopelja, E.N. The epidemiology and demographics of hip dysplasia. ISRN Orthop. 2011, 2011, 238607. [Google Scholar] [CrossRef] [PubMed]
- Ucar, D.H.; Isiklar, Z.U.; Kandemir, U.; Tumer, Y. Treatment of developmental dysplasia of the hip with Pavlik harness: Prospective study in Graf type IIc or more severe hips. J. Pediatr. Orthop. B 2004, 13, 70–74. [Google Scholar] [CrossRef]
- Baumann, T.; Munkhuu, B.; Chuluunbaatar, B.; Schmid, R.; Essig, S. 4-year follow-up of ultrasound-based diagnosis and non-surgical treatment of developmental dysplasia of the hip in mongolia: A prospective cohort study. Ultraschall Med.-Eur. J. Ultrasound 2016, 37, SL3_2. [Google Scholar] [CrossRef]
- Reijman, M.; Hazes, J.M.; Pols, H.A.; Koes, B.W.; Bierma-Zeinstra, S.M. Acetabular dysplasia predicts incident osteoarthritis of the hip: The Rotterdam study. Arthritis Rheum. 2005, 52, 787–793. [Google Scholar] [CrossRef]
- Dezateux, C.; Rosendahl, K. Developmental dysplasia of the hip. Lancet 2007, 369, 1541–1552. [Google Scholar] [CrossRef]
- Paton, R.W. Screening in Developmental Dysplasia of the Hip (DDH). Surgeon 2017, 15, 290–296. [Google Scholar] [CrossRef]
- Kilsdonk, I.; Witbreuk, M.; Van Der Woude, H.J. Ultrasound of the neonatal hip as a screening tool for ddh: How to screen and differences in screening programs between european countries. J. Ultrason. 2021, 21, e147–e153. [Google Scholar] [CrossRef] [PubMed]
- Graf, R. The use of ultrasonography in developmental dysplasia of the hip. Acta Orthop. Traumatol. Turc. 2007, 41 (Suppl. 1), 6–13. [Google Scholar] [PubMed]
- Von Kries, R.; Ihme, N.; Oberle, D.; Lorani, A.; Stark, R.; Altenhofen, L.; Niethard, F.U. Effect of ultrasound screening on the rate of first operative procedures for developmental hip dysplasia in Germany. Lancet 2003, 362, 1883–1887. [Google Scholar] [CrossRef] [PubMed]
- Developmental Dysplasia of the Hip—Guidelines for Evaluation and Referral in Newborns and Infants in Slovenia. Available online: http://www.slovenskapediatrija.si/sl-si/pdf_datoteka?revija=44&clanek=1263 (accessed on 1 April 2023).
- Zídka, M.; Džupa, V. National Register of Joint Replacement Reflecting the Treatment of Developmental Dysplasia of the Hip in Newborns. Acta Chir. Orthop. Traumatol. Cech. 2019, 86, 324–329. [Google Scholar] [CrossRef] [PubMed]
- DDH (Dysplastische Heupontwikkeling) bij Kinderen Onder Één Jaar. Available online: https://richtlijnendatabase.nl/richtlijn/ddh_dysplastische_heupontwikkeling_bij_kinderen_onder_n_jaar/diagnostiek_ddh.html (accessed on 6 April 2023).
- Irvine, I.; Hayden, R.; McDonald, H.; O’Beirne, J.; O’Driscoll, D. Developmental Dysplasia of the Hip: An Audit of the Ultrasound Screening Programme. Ir. Med. J. 2022, 115, 598. [Google Scholar]
- Developmental Dysplasia of the Hip: Screening. Available online: https://www.has-sante.fr/upload/docs/application/pdf/2016-11/luxation_hanche_v3_dtp_apr_16_hi_res_no_marks.pdf (accessed on 15 April 2023).
- Olsen, S.F.; Blom, H.C.; Rosendahl, K. Introducing universal ultrasound screening for developmental dysplasia of the hip doubled the treatment rate. Acta Paediatr. 2018, 107, 255–261. [Google Scholar] [CrossRef]
- Wenger, D.; Düppe, H.; Nilsson, J.A.; Tiderius, C.J. Incidence of Late-Diagnosed Hip Dislocation after Universal Clinical Screening in Sweden. JAMA Netw. Open 2019, 2, e1914779. [Google Scholar] [CrossRef]
- Newborn and Infant Physical Examination (NIPE) Screening Programme Handbook. Available online: https://www.gov.uk/government/publications/newborn-and-infant-physical-examination-programme-handbook/newborn-and-infant-physical-examination-screening-programme-handbook#screening-examination-of-the-hips (accessed on 15 April 2023).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Hüftgelenksdysplasie. Available online: https://www.gesundheit.gv.at/krankheiten/kinderkrankheiten/hueftgelenksdysplasie.html (accessed on 21 April 2023).
- Voitl, P.; Sebelefsky, C.; Hosner, S.; Woditschka, A.; Diesner, S.; Böck, A. Ultrasound of the infant hip: Manual fixation is equivalent to Graf’s technique regarding image quality-a randomized trial. BMC Pediatr. 2019, 19, 14. [Google Scholar] [CrossRef]
- Biedermann, R.; Riccabona, J.; Giesinger, J.M.; Brunner, A.; Liebensteiner, M.; Wansch, J.; Dammerer, D.; Nogler, M. Results of universal ultrasound screening for developmental dysplasia of the hip: A prospective follow-up of 28 092 consecutive infants. Bone Jt. J. 2018, 100-b, 1399–1404. [Google Scholar] [CrossRef]
- Čustović, S.; Šadić, S.; Vujadinović, A.; Hrustić, A.; Jašarević, M.; Čustović, A.; Krupić, F. The predictive value of the clinical sign of limited hip abduction for developmental dysplasia of the hip (DDH). Med. Glas. 2018, 15, 174–178. [Google Scholar] [CrossRef]
- Vývojová Dysplazie Kyčelního Kloubu. Available online: https://www.nzip.cz/clanek/638-vyvojova-dysplazie-kycelniho-kloubu (accessed on 25 April 2023).
- Effectiveness of the DDH Screening in Czech Republic. Available online: https://www.researchgate.net/publication/235004160_Effectiveness_of_the_DDH_Screening_in_Czech_Republic (accessed on 25 April 2023).
- Agostiniani, R.; Atti, G.; Bonforte, S.; Casini, C.; Cirillo, M.; De Pellegrin, M.; Di Bello, D.; Esposito, F.; Galla, A.; Marrè Brunenghi, G.; et al. Recommendations for early diagnosis of Developmental Dysplasia of the Hip (DDH): Working group intersociety consensus document. Ital. J. Pediatr. 2020, 46, 150. [Google Scholar] [CrossRef] [PubMed]
- Vejledning om Forebyggende Sundhedsydelser Til Børn og Unge. Available online: https://www.sst.dk/da/udgivelser/2019/vejledning-om-forebyggende-sundhedsydelser-til-boern-og-unge (accessed on 26 April 2023).
- Husum, H.C.; Møller-Madsen, B.; Thomsen, J.L.; Maimburg, R.D.; Rahbek, O. Screening of dysplasia of the hip in Denmark. Ugeskr. Laeger 2021, 183, V05200371. [Google Scholar]
- Husum, H.C.; Ghaffari, A.; Rytoft, L.A.; Svendsson, J.; Harving, S.; Kold, S.; Rahbek, O. Positive predictive values in clinical screening for developmental dysplasia of the hip. Acta Paediatr. 2021, 110, 2430–2434. [Google Scholar] [CrossRef]
- Printemps, C.; Cousin, I.; Le Lez Soquet, S.; Saliou, P.; Josse, A.; De Vries, P.; Mesureur, S.; Pons, C.; Thepaut, M. Pulvinar and pubic cartilage measurements to refine universal ultrasound screening for developmental dysplasia of the hip: Data from 1896 infant hips. Eur. J. Radiol. 2021, 139, 109727. [Google Scholar] [CrossRef] [PubMed]
- Leitlinie für das Hüftsonographische Screening–Konsensusstatement? Available online: https://www.aerzteblatt.de/archiv/53/Leitlinie-fuer-das-hueftsonographische-Screening-Konsensusstatement (accessed on 29 April 2023).
- Health Checks for Children & Adolescents. Available online: https://handbookgermany.de/en/health-checks-children-adolescent (accessed on 1 May 2023).
- Struwe, C.; Bornemann, R.; Walter, S.G.; Koob, S.; Placzek, R. The Phenomenon of the Apparent (Double) Femoral Head in Infant Hip Sonography According to Graf-Description, Incidence and Clinical Relevance. Z. Orthop. Unf. 2020, 158, 462–465. [Google Scholar] [CrossRef]
- Koob, S.; Garbe, W.; Bornemann, R.; Ploeger, M.M.; Scheidt, S.; Gathen, M.; Placzek, R. Is Prematurity a Protective Factor Against Developmental Dysplasia of the Hip? A Retrospective Analysis of 660 Newborns. Ultraschall Med. 2022, 43, 177–180. [Google Scholar] [CrossRef]
- Touzopoulos, P.; Markeas, N.G. Asymmetrical thigh creases or isolated thigh crease may be a false positive sign with low predictive value in the diagnosis of developmental dysplasia of the hip in infants: A prospective cohort study of 117 patients. Eur. J. Orthop. Surg. Traumatol. 2020, 30, 133–138. [Google Scholar] [CrossRef]
- Shaw, B.A.; Segal, L.S.; Section On, O. Evaluation and Referral for Developmental Dysplasia of the Hip in Infants. Pediatrics 2016, 138, e20163107. [Google Scholar] [CrossRef]
- Gyurkovits, Z.; Sohár, G.; Baricsa, A.; Németh, G.; Orvos, H.; Dubs, B. Early detection of developmental dysplasia of hip by ultrasound. Hip Int. 2021, 31, 424–429. [Google Scholar] [CrossRef]
- National Selective Ultrasound Screening Programme for Developmental Dysplasia of the Hip in Infants. Available online: https://www.hse.ie/eng/services/publications/clinical-strategy-and-programmes/radiologyddhimplementaionpack.pdf (accessed on 3 May 2023).
- Mulrain, J.; Hennebry, J.; Dicker, P.; Condren, J.; O’Driscoll, D.; O’Beirne, J. A normal screening ultrasound does not provide complete reassurance in infants at risk of hip dysplasia; further follow-up is required. Ir. J. Med. Sci. 2021, 190, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Buonsenso, D.; Curatola, A.; Lazzareschi, I.; Panza, G.; Morello, R.; Marrocco, R.; Valentini, P.; Cota, F.; Rendeli, C. Developmental dysplasia of the hip: Real world data from a retrospective analysis to evaluate the effectiveness of universal screening. J. Ultrasound 2021, 24, 403–410. [Google Scholar] [CrossRef] [PubMed]
- Pedrotti, L.; Crivellari, I.; Degrate, A.; De Rosa, F.; Ruggiero, F.; Mosconi, M. Interpreting neonatal hip sonography: Intraobserver and interobserver variability. J. Pediatr. Orthop. B 2020, 29, 214–218. [Google Scholar] [CrossRef]
- Geertsema, D.; Meinardi, J.E.; Kempink, D.R.J.; Fiocco, M.; van de Sande, M.A.J. Screening program for neonates at risk for developmental dysplasia of the hip: Comparing first radiographic evaluation at five months with the standard twelve week ultrasound. A prospective cross-sectional cohort study. Int. Orthop. 2019, 43, 1933–1938. [Google Scholar] [CrossRef]
- Håberg, Ø.; Foss, O.A.; Lian, Ø.B.; Holen, K.J. Is foot deformity associated with developmental dysplasia of the hip? Bone Jt. J. 2020, 102-b, 1582–1586. [Google Scholar] [CrossRef]
- Pulik, Ł.; Płoszka, K.; Romaniuk, K.; Sibilska, A.; Jedynak, A.; Tołwiński, I.; Kumięga, P.; Wojtyński, P.; Łęgosz, P. Impact of Multiple Factors on the Incidence of Developmental Dysplasia of the Hip: Risk Assessment Tool. Medicina 2022, 58, 1158. [Google Scholar] [CrossRef]
- Treiber, M.; Korpar, B.; Sirše, M.; Merc, M. Early neonatal universal ultrasound screening for developmental dysplasia of the hip: A single institution observational study. Int. Orthop. 2021, 45, 991–995. [Google Scholar] [CrossRef]
- Recomendaciones para el Diagnóstico Precoz de la Displasia Evolutiva de Cadera. Available online: https://fapap.es/articulo/410/recomendaciones-para-el-diagnostico-precoz-de-la-displasia-evolutiva-de-cadera (accessed on 4 May 2023).
- Escribano García, C.; Bachiller Carnicero, L.; Marín Urueña, S.I.; Del Mar Montejo Vicente, M.; Izquierdo Caballero, R.; Morales Luengo, F.; Caserío Carbonero, S. Developmental dysplasia of the hip: Beyond the screening. Physical exam is our pending subject. An. Pediatr. Engl. Ed. 2021, 95, 240–245. [Google Scholar] [CrossRef]
- Zinchenko, V.; Kabatsii, M.; Hertsen, I. Clinical diagnostics of ddh and peculiarities of hip joint development in children throughout the first year of life. Georgian Med. News 2021, 316–317, 114–118. [Google Scholar]
- Humphry, S.; Price, N.; Williams, P.R.; Thompson, D. The ‘clicky hip’: To refer or not to refer? Bone Jt. J. 2018, 100B, 1249–1252. [Google Scholar] [CrossRef]
- Anderton, M.J.; Hastie, G.R.; Paton, R.W. The positive predictive value of asymmetrical skin creases in the diagnosis of pathological developmental dysplasia of the hip. Bone Jt. J. 2018, 100-b, 675–679. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, A.G.; Wilkinson, S.; Elton, R.A. Values for bony acetabular roof angle and percentage femoral head cover in a selective ultrasound neonatal hip-screening programme: Effect of age, sex and side. J. Pediatr. Orthop. B 2018, 27, 236–243. [Google Scholar] [CrossRef] [PubMed]
- Marson, B.A.; Hunter, J.B.; Price, K.R. Value of the ‘clicky hip’ in selective screening for developmental dysplasia of the hip. Bone Jt. J. 2019, 101-b, 635–638. [Google Scholar] [CrossRef] [PubMed]
- Choudry, Q.A.; Paton, R.W. Neonatal screening and selective sonographic imaging in the diagnosis of developmental dysplasia of the hip. Bone Jt. J. 2018, 100-b, 806–810. [Google Scholar] [CrossRef] [PubMed]
- Morris, A.R.; Thomas, J.M.C.; Reading, I.C.; Clarke, N.M.P. Does Late Hip Dysplasia Occur After Normal Ultrasound Screening in Breech Babies? J. Pediatr. Orthop. 2019, 39, 187–192. [Google Scholar] [CrossRef]
- Poacher, A.T.; Hathaway, I.; Crook, D.L.; Froud, J.L.J.; Scourfield, L.; James, C.; Horner, M.; Carpenter, E.C. The impact of the introduction of selective screening in the UK on the epidemiology, presentation, and treatment outcomes of developmental dysplasia of the hip. Bone Jt. Open 2023, 4, 635–642. [Google Scholar] [CrossRef]
- Shorter, D.; Hong, T.; Osborn, D.A. Cochrane Review: Screening programmes for developmental dysplasia of the hip in newborn infants. Evid. Based Child. Health 2013, 8, 11–54. [Google Scholar] [CrossRef]
- Roposch, A.; Liu, L.Q.; Hefti, F.; Clarke, N.M.; Wedge, J.H. Standardized diagnostic criteria for developmental dysplasia of the hip in early infancy. Clin. Orthop. Relat. Res. 2011, 469, 3451–3461. [Google Scholar] [CrossRef]
- Roposch, A.; Liu, L.Q.; Protopapa, E. Variations in the use of diagnostic criteria for developmental dysplasia of the hip. Clin. Orthop. Relat. Res. 2013, 471, 1946–1954. [Google Scholar] [CrossRef]
- Rusjan, B.; Kiauta, M. Improving healthcare through process standardization: A general hospital case study. Int. J. Health Care Qual. Assur. 2019, 32, 459–469. [Google Scholar] [CrossRef]
- Roovers, E.A.; Boere-Boonekamp, M.M.; Castelein, R.M.; Zielhuis, G.A.; Kerkhoff, T.H. Effectiveness of ultrasound screening for developmental dysplasia of the hip. Arch. Dis. Child. Fetal Neonatal Ed. 2005, 90, F25–F30. [Google Scholar] [CrossRef] [PubMed]
- Zídka, M.; Džupa, V. Pavlik harness and Frejka pillow: Compliance affects results of outpatient treatment. Arch. Orthop. Trauma. Surg. 2019, 139, 1519–1524. [Google Scholar] [CrossRef] [PubMed]
| Study | Type of Ultrasound Screening | Time of Clinical Examination | Time of Ultrasound Examination | Ultrasound Technique |
|---|---|---|---|---|
| Austria | ||||
| [23] | Universal | 1st: 1st week of life 2nd: 6–8 weeks | 1st: 1st week of life 2nd: 6–8 weeks | Graf |
| [24] | Universal | 1st: 1st week of life 2nd: 6–8 weeks | 1st: 1st week of life 2nd: 6–8 weeks | Graf, manual fixation |
| [25] | Universal | 1st: 2 days after birth 2nd: 6–8 weeks | 1st: 2 days after birth 2nd: 6–8 weeks | Graf |
| [1] | Universal | - | 1st: 1st week of life 2nd: 4–7 weeks | Graf |
| Bosnia and Herzegovina | ||||
| [26] | Universal | 1st day of life | 1st day of life | Graf |
| Czech Republic | ||||
| [27] | Universal | 1st: 1st week 2nd: 6–9 weeks 3rd: 12–16 weeks | 1st: 1st week 2nd: 6–9 weeks 3rd: 12–16 weeks | Graf |
| [28] | Universal | 1st: 1 week 2nd: 6 weeks 3rd: 4 months | 2–3 times | Graf |
| [64] | Universal | No timeframes | No timeframes | Graf |
| Denmark | ||||
| [30,31] | Selective | 1st: 1st day of life 2nd: 5 weeks | - | - |
| [32] | Selective | 1st: 1st day of life 2nd: 5 weeks routinely/40.7 days if +examination | 13.7 days | Graf |
| France | ||||
| [18] | Selective | At each routine examination until walking age | 1st: 1 month | Graf |
| [33] | Universal | 1st: At birth | 1st: 4–12 weeks | Couture and Tréguier |
| Germany | ||||
| [34,35] | Universal | 1st: 3–10 days 2nd: 4–5 weeks | 1st: 3–10 days if +examination/+risk factors 2nd: 4–5 weeks | Graf |
| [36] | Universal | 1st: 1st week of life | 1st: 1st week of life if +risk factors | Graf |
| [37] | Universal | 1st: 1st week of life | 1st: 1st week of life | Graf |
| Greece | ||||
| [38] | Selective | 1st: shortly after birth | No timeframes | Graf and Harcke |
| Hungary | ||||
| [40] | Universal | 1st: <72 h 2nd: 3 weeks 3rd: 6–8 weeks | 1st: <72 h IIc and worse: 2nd: 3 weeks 3rd: 6 weeks | Graf |
| Ireland | ||||
| [41] | Selective | 1st: <72 h 2nd: 6 weeks | 1st: by 2 weeks (only if +examination) 2nd: by 6 weeks (if + risk factors/follow-up for +examination group) After 3–4 months -radiograph | Graf |
| [17] | Selective | - | 1st: 6 weeks + additional radiograph at 6 months | Graf |
| [42] | Selective | - | 1st: 6 weeks 2nd: Graf IIa—3 months +additional radiograph at 6 months | Graf |
| Italy | ||||
| [29] | Selective | 1st: at birth and until 6 months | 1st week of life | Graf |
| [43] | Universal | 1st: 1st day of life 2nd: 3rd day of life | As soon as possible if clinical findings present or at 6 weeks of age | Graf |
| [44] | Universal | - | About 3 months | Graf |
| The Netherlands | ||||
| [11] | Selective | 1st: 1 week 2nd: 1 month 3rd: 3 months | 1st: 3 months/earlier if +examination | Graf |
| [45] | Selective | 1st: 2–3 weeks | 1st: 3 months/6 weeks if +examination Other group radiograph—5 months of age | Graf |
| Norway | ||||
| [19] | Universal | 1st: <3 days | 1st: <3days | Graf |
| [46] | Selective | 1st: 1 day | - | Terjesen |
| Poland | ||||
| [47] | Universal | 1st: at birth 2nd: 6 weeks 3rd: 12 weeks | 1st: first weeks of life if +examination/+risk factors 2nd: 6 weeks 3rd: 12 weeks | Graf |
| Slovenia | ||||
| [14] | Universal | 1st: first few days 2nd: 6 weeks | 1st: on maternity ward if +examination/+risk factors 2nd: 6 weeks | Graf |
| [48] | Universal | - | 1st: 1st week of life 2nd: 12 weeks (normal hips), 6 weeks (immature hips), 2 weeks (IIc/D) | Graf |
| Spain | ||||
| [49] | Selective | 1st: 1–7 days | 1st: 4–8 weeks Radiograph—4–6 months | Graf |
| [50] | Selective | 1st: 48–72 h post-birth | 4–8 weeks | - |
| Sweden | ||||
| [20] | Selective | 1st: before discharge from a maternity ward 2nd: 6–8 weeks 3rd: 6 months 4th: 10–12 months | No timeframes | Graf Dahlström |
| Ukraine | ||||
| [51] | Universal | - | - | Graf |
| United Kingdom | ||||
| [21,52,53,54,55,56,57] | Selective | 1st: <72 h 2nd: 6–8 weeks | 4–6 weeks | Graf, Harcke |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krysta, W.; Dudek, P.; Pulik, Ł.; Łęgosz, P. Screening of Developmental Dysplasia of the Hip in Europe: A Systematic Review. Children 2024, 11, 97. https://doi.org/10.3390/children11010097
Krysta W, Dudek P, Pulik Ł, Łęgosz P. Screening of Developmental Dysplasia of the Hip in Europe: A Systematic Review. Children. 2024; 11(1):97. https://doi.org/10.3390/children11010097
Chicago/Turabian StyleKrysta, Wojciech, Patryk Dudek, Łukasz Pulik, and Paweł Łęgosz. 2024. "Screening of Developmental Dysplasia of the Hip in Europe: A Systematic Review" Children 11, no. 1: 97. https://doi.org/10.3390/children11010097
APA StyleKrysta, W., Dudek, P., Pulik, Ł., & Łęgosz, P. (2024). Screening of Developmental Dysplasia of the Hip in Europe: A Systematic Review. Children, 11(1), 97. https://doi.org/10.3390/children11010097