The Future for the Children of Tomorrow: Avoiding Salt in the First 1000 Days
Abstract
1. Introduction
1.1. Why Are the First 1000 Days of Life Important?
1.2. Salt Consumption: Neither Depletion nor Excess
1.3. Recommendations for Salt Intake during Childhood
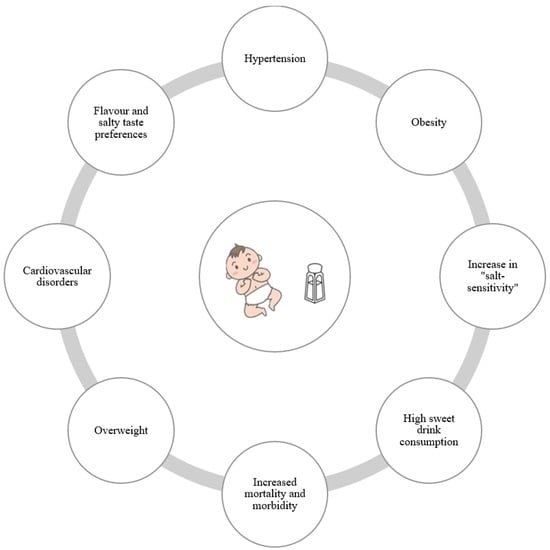
1.4. Main Consequences of High Salt Consumption
2. Physiology of Sodium Chloride
3. Salt Intake: Benefits and Consequences
3.1. Benefits
3.1.1. The Role of Sodium in Newborns and Infants’ Growth
3.1.2. The Importance of Iodized Salt
3.2. Short-Term Consequences
3.2.1. The Development of Flavor and Taste
3.2.2. How to Regulate Predisposition to Salty Taste
3.3. Long-Term Consequences
3.3.1. Hypertension
Pathophysiology of Hypertension
Hypertension and Nutritional Intervention
Sodium Sensitivity
3.3.2. Obesity
Epidemiology
The Relationship between Obesity and Salt Intake
Obesity Prevention Strategies
4. Effects of Low-Sodium Diet
5. Salty and Sweet: Two Health Enemies
6. Discussion
6.1. Factors Influencing Neurobehavioral Development
6.2. The Role of a Low-Salt Diet for Public and Individual Health
6.3. Strengths and Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Scott, J.A. The first 1000 days: A critical period of nutritional opportunity and vulnerability. Nutr. Diet. 2020, 77, 295–297. [Google Scholar] [CrossRef]
- Pietrobelli, A.; Agosti, M.; Palmer, C.; Pereira-Da-Silva, L.; Rego, C.; Rolland-Cacherà, M.F.; Zuccotti, G. Nutrition in the First 1000 Days: Ten Practices to Minimize Obesity Emerging from Published Science. Int. J. Environ. Res. Public Health 2017, 14, 1491. [Google Scholar] [CrossRef] [PubMed]
- Schwarzenberg, S.J.; Georgieff, M.K.; Daniels, S.; Corkins, M.; Golden, N.H.; Kim, J.H.; Wesley Lindsey, C.; Magge, S.N. Advocacy for Improving Nutrition in the First 1000 Days to Support Childhood Development and Adult Health. Pediatrics 2018, 141, e20173716. [Google Scholar] [CrossRef] [PubMed]
- Lutter, C.K.; Grummer-Strawn, L.; Rogers, L. Complementary feeding of infants and young children 6 to 23 months of age. Nutr. Rev. 2021, 79, 825–846. [Google Scholar] [CrossRef] [PubMed]
- Rust, P.; Ekmekcioglu, C. Impact of Salt Intake on the Pathogenesis and Treatment of Hypertension. Adv. Exp. Med. Biol. 2017, 956, 61–84. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Xu, Y. Nutrition and Metabolism in the First 1000 Days of Life. Nutrients 2023, 15, 2554. [Google Scholar] [CrossRef]
- Aburto, N.J.; Ziolkovska, A.; Hooper, L.; Elliott, P.; Cappuccio, F.P.; Meerpohl, J.J. Effect of lower sodium intake on health: Systematic review and meta-analyses. BMJ 2013, 346, f1326. [Google Scholar] [CrossRef]
- Farebrother, J.; Zimmermann, M.B.; Andersson, M. Excess iodine intake: Sources, assessment, and effects on thyroid function. Ann. N. Y. Acad. Sci. 2019, 1446, 44–65. [Google Scholar] [CrossRef]
- Iacone, R.; Iaccarino Idelson, P.; Campanozzi, A.; Rutigliano, I.; Russo, O.; Formisano, P.; Galeone, D.; Macchia, P.E.; Strazzullo, P.; The MINISAL-GIRCSI Study Group. Relationship between salt consumption and iodine intake in a pediatric population. Eur. J. Nutr. 2021, 60, 2193–2202. [Google Scholar] [CrossRef]
- Gowrishankar, M.; Blair, B.; Rieder, M.J. Dietary intake of sodium by children: Why it matters. Paediatr. Child. Health 2020, 25, 47–61. [Google Scholar] [CrossRef]
- Fewtrell, M.; Bronsky, J.; Campoy, C.; Domellöf, M.; Embleton, N.; Fidler Mis, N.; Hosjak, I.; Hulst, J.M.; Indrio, F.; Lapillonne, A.; et al. Complementary Feeding: A Position Paper by the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 119–132. [Google Scholar] [CrossRef] [PubMed]
- WHO. Guideline: Sodium Intake for Adults and Children; WHO Guidelines Approved by the Guidelines Review Committee; World Health Organization: Geneva, Switzerland, 2012. Available online: http://www.ncbi.nlm.nih.gov/books/NBK133309/ (accessed on 11 December 2023).
- Noce, A.; Romani, A.; Bernini, R. Dietary Intake and Chronic Disease Prevention. Nutrients 2021, 13, 1358. [Google Scholar] [CrossRef] [PubMed]
- Società Italiana di Nutrizione Umana. LARN: Livelli di Assunzione di Riferimento di Nutrienti ed Energia per la Popolazione Italiana, 4th ed.; SICS Editore: Milan, Italy, 2014. [Google Scholar]
- Puma, A.; Pecoraro, L.; Salvottini, C.; Carbonare, L.D.; Piacentini, G.; Pietrobelli, A. Parental Perceptions and Concerns Related to the Consequences of Pediatric Obesity: Feeling or Real Problem? Endocr. Metab. Immune Disord. Drug Targets 2023, 23, 1380–1391. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; He, F.J.; MacGregor, G.A. High salt intake: Independent risk factor for obesity? Hypertension 2015, 66, 843–849. [Google Scholar] [CrossRef] [PubMed]
- Genovesi, S.; Giussani, M.; Orlando, A.; Orgiu, F.; Parati, G. Salt and Sugar: Two Enemies of Healthy Blood Pressure in Children. Nutrients 2021, 13, 697. [Google Scholar] [CrossRef]
- Cogswell, M.E.; Gunn, J.P.; Yuan, K.; Park, S.; Merritt, R. Sodium and sugar in complementary infant and toddler foods sold in the United States. Pediatrics 2015, 135, 416–423. [Google Scholar] [CrossRef]
- Lava, S.A.; Bianchetti, M.G.; Simonetti, G.D. Salt intake in children and its consequences on blood pressure. Pediatr. Nephrol. 2015, 30, 1389–1396. [Google Scholar] [CrossRef]
- Hatch-McChesney, A.; Lieberman, H.R. Iodine and Iodine Deficiency: A Comprehensive Review of a Re-Emerging Issue. Nutrients 2022, 14, 3474. [Google Scholar] [CrossRef]
- Zimmermann, M.B.; Jooste, P.L.; Pandav, C.S. Iodine-deficiency disorders. Lancet 2008, 372, 1251–1262. [Google Scholar] [CrossRef]
- Mennella, J.A. Ontogeny of taste preferences: Basic biology and implications for health. Am. J. Clin. Nutr. 2014, 99, 704S–711S. [Google Scholar] [CrossRef]
- Strazzullo, P.; Campanozzi, A.; Avallone, S. Does salt intake in the first two years of life affect the development of cardiovascular disorders in adulthood? Nutr. Metab. Cardiovasc. Dis. 2012, 22, 787–792. [Google Scholar] [CrossRef] [PubMed]
- Mennella, J.A.; Reiter, A.R.; Daniels, L.M. Vegetable and Fruit Acceptance during Infancy: Impact of Ontogeny, Genetics, and Early Experiences. Adv. Nutr. 2016, 7, 211S–219S. [Google Scholar] [CrossRef] [PubMed]
- Rosenstein, D.; Oster, H. Differential facial responses to four basic tastes in newborns. Child. Dev. 1988, 59, 1555–1568. [Google Scholar] [CrossRef] [PubMed]
- Beauchamp, G.K.; Cowart, B.J.; Moran, M. Developmental changes in salt acceptability in human infants. Dev. Psychobiol. 1986, 19, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Leyvraz, M.; Chatelan, A.; da Costa, B.R.; Taffe, P.; Paradis, G.; Bovet, P.; Bochu, M.; Chiolero, A. Sodium intake and blood pressure in children and adolescents: A systematic review and meta-analysis of experimental and observational studies. Int. J. Epidemiol. 2018, 47, 1796–1810. [Google Scholar] [CrossRef] [PubMed]
- Ha, S.K. Dietary Salt Intake and Hypertension. Electrolytes Blood Press. 2014, 12, 7–18. [Google Scholar] [CrossRef]
- Suckling, R.J.; He, F.J.; Markandu, N.D.; MacGregor, G.A. Dietary salt influences postprandial plasma sodium concentration and systolic blood pressure. Kidney Int. 2012, 81, 407–411. [Google Scholar] [CrossRef]
- Newberry, S.J.; Chung, M.; Anderson, C.A.; Chen, C.; Fu, Z.; Tang, A.; Zhao, N.; Booth, M.; Marks, J.; Hollands, S.; et al. Sodium and Potassium Intake: Effects on Chronic Disease Outcomes and Risks. In AHRQ Comparative Effectiveness Reviews; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2018. Available online: http://www.ncbi.nlm.nih.gov/books/NBK519328/ (accessed on 5 December 2023).
- Haseler, E.; Sinha, M.D. Hypertension in Children and Young Adults. Pediatr. Clin. N. Am. 2022, 69, 1165–1180. [Google Scholar] [CrossRef]
- Kos, M.; Nađ, T.; Stanojević, L.; Lukić, M.; Stupin, A.; Drenjančević, I.; Pušeljić, S.; Davidović Cvetko, E.; Mihaljević, Z.; Dumančić, D.; et al. Estimation of Salt Intake in Normotensive and Hypertensive Children: The Role of Body Weight. Nutrients 2023, 15, 736. [Google Scholar] [CrossRef]
- Friedemann, C.; Heneghan, C.; Mahtani, K.; Thompson, M.; Perera, R.; Ward, A.M. Cardiovascular disease risk in healthy children and its association with body mass index: Systematic review and meta-analysis. BMJ 2012, 345, e4759. [Google Scholar] [CrossRef]
- Brand, A.; Visser, M.E.; Schoonees, A.; Naude, C.E. Replacing salt with low-sodium salt substitutes (LSSS) for cardiovascular health in adults, children and pregnant women. Cochrane Database Syst. Rev. 2022, 8, CD015207. [Google Scholar] [CrossRef]
- Jachimowicz-Rogowska, K.; Winiarska-Mieczan, A. Initiatives to Reduce the Content of Sodium in Food Products and Meals and Improve the Population’s Health. Nutrients 2023, 15, 2393. [Google Scholar] [CrossRef] [PubMed]
- McLean, R.M. Salt Substitutes—An Important Tool to Increase Potassium and Reduce Sodium Intakes? Nutrients 2023, 15, 2647. [Google Scholar] [CrossRef] [PubMed]
- Bernabe-Ortiz, A.; Sal y Rosas, V.G.; Ponce-Lucero, V.; Cárdenas, M.K.; Carrillo-Larco, R.M.; Diez-Canseco, F.; Pesantes, M.A.; Sacksteder, K.A.; Gilman, R.H.; Miranda, J.J. Effect of salt substitution on community-wide blood pressure and hypertension incidence. Nat. Med. 2020, 26, 374–378. [Google Scholar] [CrossRef] [PubMed]
- Marklund, M.; Singh, G.; Greer, R.; Cudhea, F.; Matsushita, K.; Micha, R.; Brady, T.; Zhao, D.; Huang, L.; Tian, M.; et al. Estimated population wide benefits and risks in China of lowering sodium through potassium enriched salt substitution: Modelling study. BMJ 2020, 369, m824. [Google Scholar] [CrossRef]
- Ajenikoko, A.; Ide, N.; Shivashankar, R.; Ge, Z.; Marklund, M.; Anderson, C.; Atun, A.; Thomson, A.; Henry, M.E.; Cobb, L.K. Core Strategies to Increase the Uptake and Use of Potassium-Enriched Low-Sodium Salt. Nutrients 2021, 13, 3203. [Google Scholar] [CrossRef]
- He, F.J.; Marrero, N.M.; MacGregor, G.A. Salt intake is related to soft drink consumption in children and adolescents: A link to obesity? Hypertension 2008, 51, 629–634. [Google Scholar] [CrossRef]
- Aparicio, A.; Rodríguez-Rodríguez, E.; Cuadrado-Soto, E.; Navia, B.; López-Sobaler, A.M.; Ortega, R.M. Estimation of salt intake assessed by urinary excretion of sodium over 24 h in Spanish subjects aged 7–11 years. Eur. J. Nutr. 2017, 56, 171–178. [Google Scholar] [CrossRef]
- Švigelj, M.; Jančić, G.; Močnik, M.; Marčun Varda, N. Body composition obtained by bioelectrical impedance with a nutritional questionnaire in children with chronic kidney disease, obesity, or hypertension. Clin. Nephrol. 2021, 96, 36–42. [Google Scholar] [CrossRef]
- Drozdz, D.; Kwinta, P.; Korohoda, P.; Pietrzyk, J.A.; Drozdz, M.; Sancewicz-Pach, K. Correlation between fat mass and blood pressure in healthy children. Pediatr. Nephrol. 2009, 24, 1735–1740. [Google Scholar] [CrossRef]
- Spagnolo, A.; Giussani, M.; Ambruzzi, A.M.; Bianchetti, M.; Maringhini, S.; Matteucci, M.C.; Menghetti, E.; Salice, P.; Simionato, L.; Strambi, M.; et al. Focus on prevention, diagnosis and treatment of hypertension in children and adolescents. Ital. J. Pediatr. 2013, 39, 20. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.B. Iodine deficiency. Endocr. Rev. 2009, 30, 376–408. [Google Scholar] [CrossRef] [PubMed]
- Leggio, M.; Lombardi, M.; Caldarone, E.; Severi, P.; D’emidio, S.; Armeni, M.; Bravi, V.; Grazia Bendini, M.; Mazza, A. The relationship between obesity and hypertension: An updated comprehensive overview on vicious twins. Hypertens. Res. 2017, 40, 947–963. [Google Scholar] [CrossRef] [PubMed]
- Trieu, K.; Neal, B.; Hawkes, C.; Dunford, E.; Campbell, N.; Rodriguez-Fernandez, R.; Legetic, B.; McLaren, L.; Barberio, A.; Webster, J. Salt Reduction Initiatives around the World—A Systematic Review of Progress towards the Global Target. PLoS ONE 2015, 10, e0130247. [Google Scholar] [CrossRef]
| Food Product Category | Sodium Density (mg/1000 Kcal)—Mean | Sodium Concentration (mg/100 g)—Mean |
|---|---|---|
| Vegetables | 501 (302–700) | 20 (12–28) |
| Fruit | 77 (59–96) | 5 (4–5) |
| Cereals | 31 (12–51) | 12 (5–20) |
| Mixed grains and fruit | 103 (61–146) | 9 (5–13) |
| Savory snacks | 1382 (1114–1649) | 486 (367–604) |
| Juices/drinks | 184 (150–218) | 9 (7–10) |
| Dairy-based desserts | 421 (357–484) | 42 (31–53) |
| Dry grain-based dessert | 399 (301–496) | 169 (125–214) |
| Dry fruit-based snacks | 383 (302–463) | 138 (108–167) |
| Cereal bars and breakfast pastries | 744 (558–930) | 248 (199–298) |
| Dinners, soups, and vegetables | 503 (428–578) | 28 (25–31) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mazzuca, G.; Artusa, S.; Pietrobelli, A.; Di Cara, G.; Piacentini, G.; Pecoraro, L. The Future for the Children of Tomorrow: Avoiding Salt in the First 1000 Days. Children 2024, 11, 98. https://doi.org/10.3390/children11010098
Mazzuca G, Artusa S, Pietrobelli A, Di Cara G, Piacentini G, Pecoraro L. The Future for the Children of Tomorrow: Avoiding Salt in the First 1000 Days. Children. 2024; 11(1):98. https://doi.org/10.3390/children11010098
Chicago/Turabian StyleMazzuca, Giorgia, Silvia Artusa, Angelo Pietrobelli, Giuseppe Di Cara, Giorgio Piacentini, and Luca Pecoraro. 2024. "The Future for the Children of Tomorrow: Avoiding Salt in the First 1000 Days" Children 11, no. 1: 98. https://doi.org/10.3390/children11010098
APA StyleMazzuca, G., Artusa, S., Pietrobelli, A., Di Cara, G., Piacentini, G., & Pecoraro, L. (2024). The Future for the Children of Tomorrow: Avoiding Salt in the First 1000 Days. Children, 11(1), 98. https://doi.org/10.3390/children11010098