Abstract
Background. During the treatment of unstable hips in developmental hip dysplasia (DDH), the position of the femoral head must be assessed in spica cast (SC) after reduction. A transinguinal sonographic technique (TIT) to the hip joint has been previously described in the literature. The aim of this study is to evaluate the agreement among TIT and MR to identify hip reduction. Methods. From 2016 to 2019, 14 consecutive newborns (10 female, 4 males) with a mean age of 2.97 ± 1.29 months were treated with closed reduction in SC. A total of 4/14 children had bilateral unstable DDH. Out of 18 hips, there were 8 hips type IV and 10 hips type IIIA, according to Graf. SC were changed monthly and hips were checked both with TIT and MR, looking for persistent dislocation. Results. Overall, a mean of 2.61 SC/hip (mode = 3) was accomplished, accounting for 47 procedures, with 46 reduced hips and 1 dislocated hip: TIT and MR always agreed on the same result (47/47; Cohen k = 1, CI95 1.00 to 1.00). Conclusions. The inguinal ultrasound technique described by van Douveren showed perfect agreement with MR and might be considered a reliable alternative to check the position of the femoral head during the conservative treatment of hip dysplasia in spica cast.
1. Introduction
In the conservative management of developmental dysplasia of the hip (DDH) in new-borns, unstable or dislocated hips need to first be reduced, then the femoral head is maintained in the socket with an harness or spica cast, allowing the maturation of the acetabulum [1]. Closed reduction and retention with a pelvi-podalic spica cast (SC) in a “human position”, as described by Fettweis [1,2,3,4], represents a possible treatment option.
Once SC has been applied, the position of the head must be evaluated, to check if the hip is reduced or not [5]. Different techniques are available to verify the position of the femoral head in SC: X-ray [6], computer tomography (CT) [7,8,9], magnetic resonance (MR) [5,6,10,11] and ultrasound (US) [10,12]. According to Graf’s technique, ultrasound examination should be performed in a frontal standard plane, approaching the hip laterally and avoiding tilting errors of the probe [13] (Figure 1); however, Graf’s method is not applicable in the presence of a SC. More recently, different sonographic techniques have been described, to overcome the problem of hips being covered by a cast [14,15,16]. Among those different US approaches, one of the most used is the transinguinal approach (TIT) described in 2003 by van Douveren et al. [12]. Over the following 20 years, more authors compared TIT with other available techniques as gold standard, such as radiographs or CT [10,17].
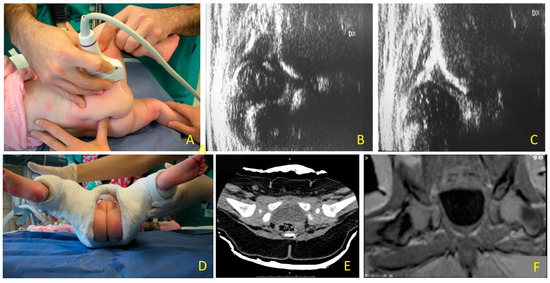
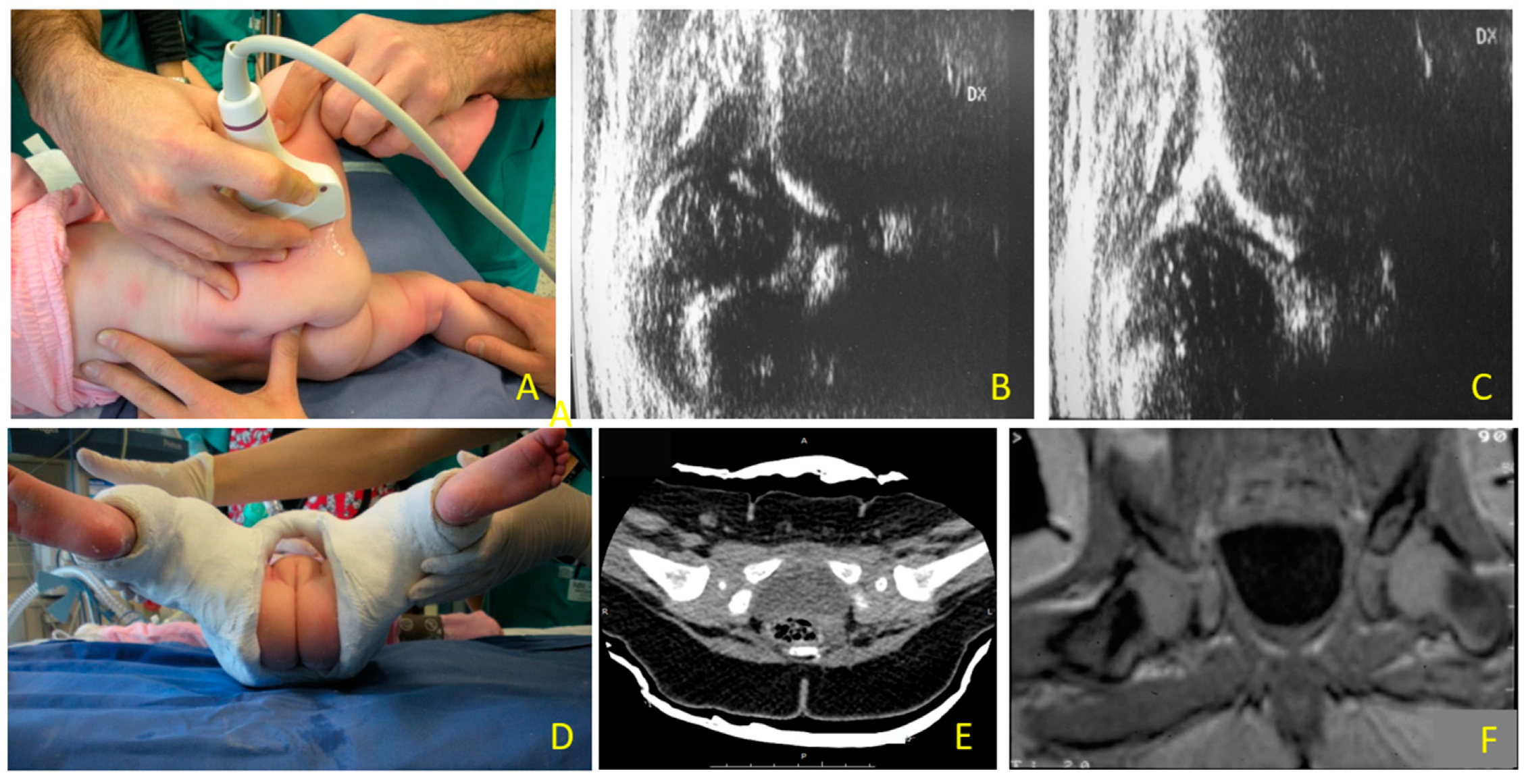
Figure 1.
Hip dislocation: (A) ultrasound evaluation with lateral approach to the hip joint according to Graf technique during reduction maneuver; (B) type IV hip; (C) femoral head in the acetabular fossa after closed reduction, before performing a pelvi-podalic spica cast (SC); (D) the SC has been applied. With SC, Graf’s technique cannot be applied anymore, to check if the hip is reduced or not, (E) to verify the position of the femoral head in SC, computer tomography (CT) or (F) magnetic resonance (MR) can be used.
The aim of this study is to evaluate the agreement between TIT and MR in identifying femoral head position in SC after closed reduction of unstable hips in DDH.
2. Materials and Methods
From 2016 to 2019, 14 consecutive patients (18 hips) with DDH and unstable hips were conservatively treated with closed reduction SC according to Fettweis.
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Ethics Committee of Bergamo (ITA), Nr 2021–0134. Informed consent was obtained from patients’ parents/guardians. Included patients were children with DDH and dislocated or unstable hip(s) (Graf type III or IV), treated conservatively with closed reduction in SC. Before every cast changing, each hip was classified according to Graf and a new cast was performed if at least one hip was still dislocated or unstable (Graf type D, III and IV) [10]. If the hip was still dysplastic but not unstable (Graf type IIb or IIc), no further SC was used, and the treatment followed with a brace until the maturation of the acetabulum (Graf type 1). Once maturation was reached, according to the ultrasound criteria described by Graf [1], a check with a single antero-posterior pelvic radiography without gonad shielding was performed [18,19], in order to measure the acetabular index according to Tönnis (AI). If AI showed normal values, then therapy with the brace was interrupted and the patient was scheduled for a long-term follow-up until skeletal maturity, according to Kubo et al. [20,21,22,23].
Each patient was first evaluated as an outpatient, clinically and with ultrasound (both Graf and TIT being performed); only if the hip resulted unstable or dislocated but reducible, a spica cast in narcosis was scheduled in the following days. Before each cast, the patient was re-evaluated in narcosis in the same fashion: clinically and with ultrasound (both Graf and TIT being performed). During the procedure, the position of the hip was checked with TIT and re-checked with TIT immediately after the cast dried, with the patient still in narcosis. This latter TIT after each cast is the one used for the comparison with MR in the present study. TIT was always performed by the same Author (GN).
Each cast was performed in narcosis and replaced every month; after every new cast the hips were checked both with TIT and MR in narcosis, looking for persistent dislocation (Figure 2). With TIT, a hip is defined as dislocated if the imaginary curved line tangent to the ramus superior of os pubis and the femur neck is interrupted [12] (Figure 3). MR was performed within 48 h of the positioning of the cast, with or without narcosis according to radiologist’s preferences and the condition of the child. Every patient was followed-up until hip maturation (according to both Graf classification and Tönnis’ acetabular index [13,20,24]).
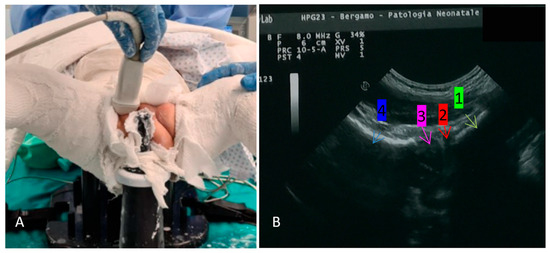
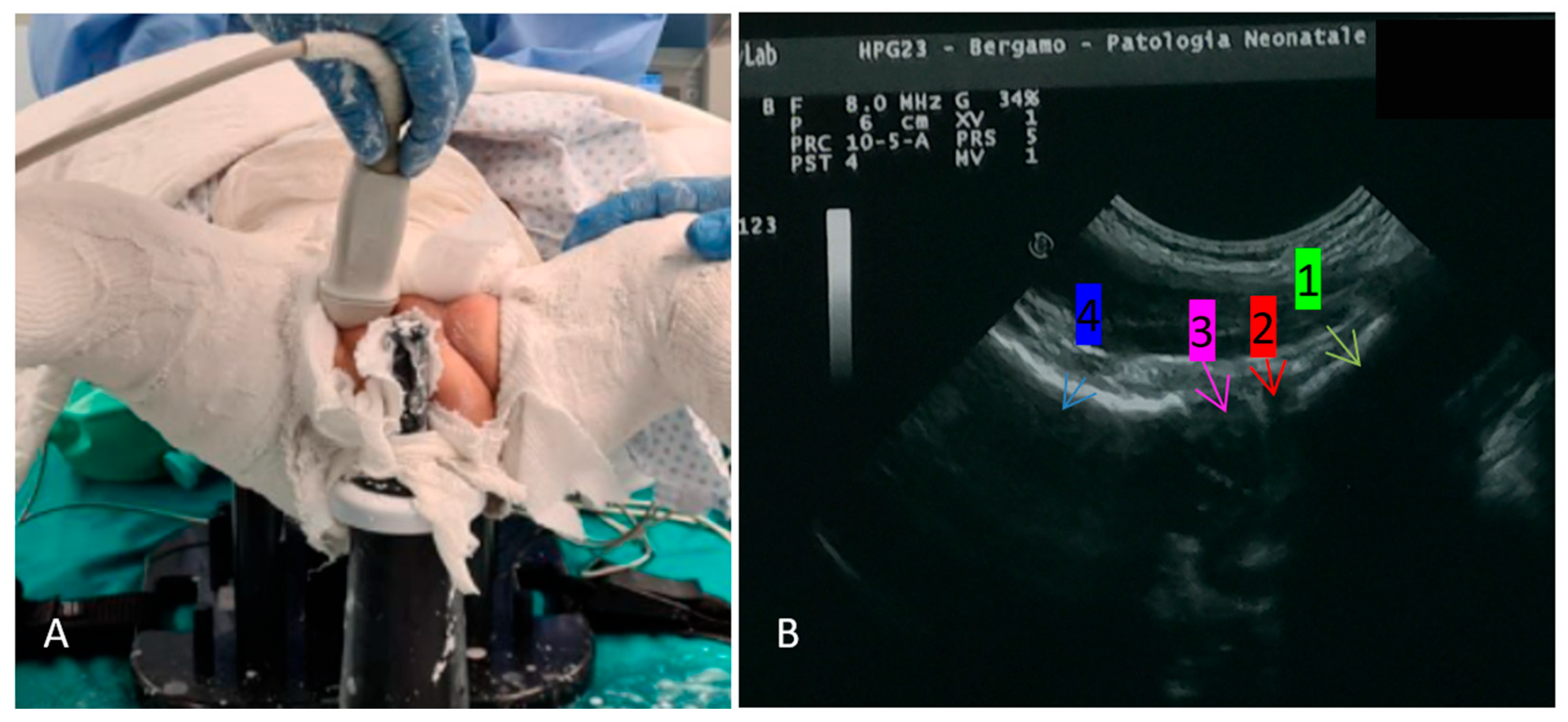
Figure 2.
(A) The patient is in narcosis on a pediatric table, the SC has already been performed (in human position, according to Fettweis); the right hip is checked with TIT, through the same perineal opening of the cast used for wipers; and (B) the sonographic image obtained in the same patient after reduction: 1 ramus superior os pubis, 2 labrum, 3 femoral head, 4 femoral neck.
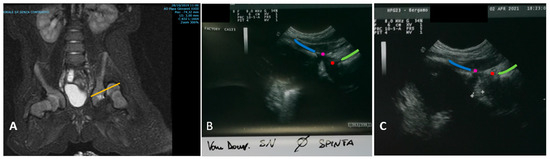
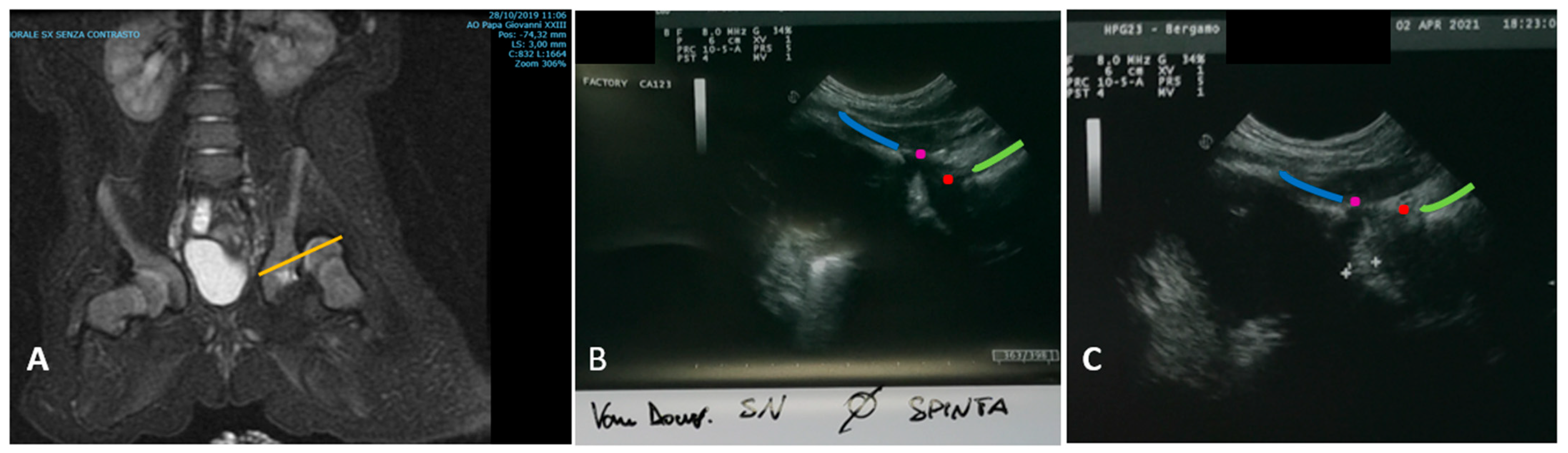
Figure 3.
(A) MR image (coronal plane) of a dislocated hip (patient Id Nr 4, Graf type IV, see text). The yellow line indicates the plane in which the hips are scanned with the miniconvex probe, using TIT technique. Looking at this image, it is easier to understand why the anatomical landmarks indicated in Figure 2 (ramus superior os pubis, labrum, femoral head and neck) must all be present in the ultrasound images obtained with TIT. Particularly, if the labrum is missing, the femoral head could be dislocated proximally and the iliac wing wrongly identified as os pubis, obtaining a false negative. (B) Another patient with a dislocated hip (Graf type IV) examined with TIT. The anatomical landmarks are indicated with the same colors as Figure 2B. The anterior contour of the ramus superior os pubis is marked with a blue line, the anterior border of the labrum is marked with a violet point. The anterior border of the head is marked with a red point and the anterior contour of the neck of the femur is marked with a green line. Here, the hip is dislocated, and the imaginary extension of the lines built by the anterior margin of pubis, labrum, femoral head and neck lies on different curves. (C) The same hip from (B), after reduction. The hip is now reduced, and the imaginary extension of the lines built by the anterior margin of pubis, labrum, femoral head and neck lies on the same curve.
The images obtained with TIT were contextually evaluated by the same orthopedic surgeon who also performed the examination (GN). With TIT, an Esaote MyLab™30 with a miniconvex (Esaote Convex probe 5-2, radius 13 mm, Genoa, Italy) was used, start settings 12 MHz and depth window of 4 cm. The MR was performed with a 1.5 T Siemens (Munich, Germany), using a fast protocol with T2 sequences with 3 mm thickness in 3 planes, evaluated by a radiologist with more than 5 years of experience with pediatric musculoskeletal imaging.
Statistical Methods
The hypothesis (H0) is that TIT performs like MR in detecting the position of the femoral head, whilst the alternative hypothesis (H1) is that TIT is less performing than MR [25]. In the present study, MR is considered the gold standard. To test this hypothesis, we compared the results of the TIT (intervention group) with MR (control group).
Sample size has been calculated according to Walter et al. for interclass correlation [26,27], with the following settings: minimum acceptable reliability: 0.95; expected reliability: 0.85; significance level (α): 0.05 (2-tailed); power (1–β): 90%; and expected dropout rate: 5%. This accounts for a sample size, n = 33 and sample size (with 5% dropout), ndrop = 35. Agreement has been computed according to Cohen’s kappa [25,27].
3. Results
In the present study 14 patients (18 hips) were included and according to Graf’s classification there were initially 8 hips type IV and 10 hips type IIIA [28]. Demographic data of the patients are summarized in Table 1.

Table 1.
Demographic data. All patients were treated conservatively with spica cast (SC) after closed reduction. F: female; M: male; worst and best hip in the same patient according to Graf classification 1. Nr cast = number of cast(s) performed for each patient during treatment. Nr hip MR = number of MR performed for each patient for each hip; it represents the number of events/patient (e.g., if a patient had 2 involved hips and underwent 3 spica casts, then the Nr Hip MR = 6).
There were 9/14 female and 5/14 male patients (F/M = 1.8). The mean age at the first procedure was 2.97 ± 1.29 months. A total of 4/14 children had bilateral unstable hip dysplasia. A mean of 2.61 casts/hip (mode = 3) have been performed. At the end of the therapy with cast(s), there were 1/18 still dislocated (Patient Id Nr = 4; initial Graf type IV), 9/18 IIc, 6/18 IIb and 3/18 Ib according to Graf. Patients with the worst hip classified D or worse followed a treatment with cast, whilst patients with the worst hip classified 2c or 2b followed a treatment with a static brace in a human position until maturation to Graf type I and normal acetabular index (Tönnis) according to age [29,30]. A total of 45/47 MR were performed in narcosis and 2/47 without (asleep patients).
In total, 47 procedures (SC in narcosis, TIT and MR) have been performed and in 100% (47/47 events) TIT and MR agreed on the same result (Cohen k = 1, CI95 1.00 to 1.00), (Table 2). There were 46/47 true negative and 1/47 true positive, no false positive or negative, referring to MR as gold standard.

Table 2.
Comparison between transinguinal ultrasound (TIT) and magnetic resonance (MR) images in spica cast (SC) after closed reduction. TIT and MR results are represented as follows: 1: hip reduced; 0: hip not reduced; * = in the best hip; ** = in the worst hip, according to Graf classification 1.
In 1/14 patient (Patient ID: Nr 4; 1/18 hip involved) the conservative treatment was interrupted after the first SC, due to irreducible persistent dislocation. This was the oldest patient (5.8 months at the beginning of the treatment with SC), for whom diagnosis and treatment were delayed because of a prolonged hospitalization for respiratory impairment in the neonatal intensive care unit. The preoperative evaluation occurred in the intensive care unit with the patient still in sedation for respiratory problems and it seemed reducible at that time. Later, the patient underwent an open reduction.
In 1/14 patient (Patient ID: Nr 1; 1/18 hip involved, male), after the first SC the TIT showed a still-dislocated hip, with the patient still in sedation in the operating room. Only in this event, we repeated the entire procedure (SC removal, reduction and TIT) before MR. After re-performing the reduction and SC, in TIT the hip was reduced, thereafter the patient underwent the MR. This broke the study protocol and was undertaken on an ethical basis, to exploit the same sedation and avoid additional procedures. Nevertheless, the Authors decided to include the data, as the concordance between TIT and MR is not biased.
With the exception of Patient Nr 4, all of the others (46/47, 98%) reached the hip maturity with conservative treatment and are still in long-term follow-up for residual acetabular dysplasia [20,21,22,23,31,32].
In total, 13/14 patients achieved the criteria of “mature hips” with an acetabular index (according to Tönnis) > 30° before the brace was removed. The remaining 1/14 (pt ref Nr 4) followed a surgical procedure after the first SC. According to study design and follow-up, we cannot comment on the evolution of the hip during the long-term follow-up, particularly regarding the acetabular index; up to now, no-one needed further treatment.
4. Discussion
After closed reduction of unstable or dislocated hips in DDH, the position of the femoral head in spica cast should always be checked [5]. The rate of persistent dislocation is consistent: in up to 10% of the cases, MRI revealed a persistent hip dislocation after application of Fettweis SC in children with unstable hip joint [5]. X-rays are an option that could be performed while performing the spica cast and are also widely available. However, the following problems are present, decreasing accuracy with X-rays: (1) direct visualization of the femoral head is usually not possible (according to patients age, there might be no ossification center of the femoral head), and (2) a persistent dislocation might be overseen with an antero-posterior view of the pelvis, as the dislocation occurs usually on an antero-posterior direction [10]. CT and MR can be considered gold standard, as both of them allow a direct 3-dimensional visualization of the hip [33,34]. MR has the obvious advantage of avoiding radiation and with dedicated simplified sequences it could be performed without sedation and in less than 3 min [35,36]. It is not only the post-reduction check that can be performed with MR, but the procedure itself can also be MR-guided [37]; however, the availability of an operating room with MR for closed reduction of the hip is still a rare option nowadays. In current practice, CT or MR are usually performed only after the spica cast has been performed and any detected failure requires a repeat of the whole procedure. In other words, with CT or MR, the surgeon usually has no way to check the situation of the hip during the reduction maneuver. In contrast, ultrasound techniques are a bed-side test, allow the visualization of the femoral head during the whole procedure and a post-procedural check in spica cast [10,12,17,38,39].
In the present study, TIT was performed comparing results with MR, examinations were performed in the same cohort within 48 h from the positioning of the cast, with or without narcosis. TIT and MR showed a 100% agreement (according to Cohen’s k [25]) in detecting the position in spica cast of the femoral head after closed reduction.
Our data showed a lower incidence of dislocated hips (true positives) in patients treated with SC in comparison to previous studies [10,12,17]. There are many reasons which might explain these data. First, the mean age of our patients was lower, and a younger hip has a higher probability of being reduced in a closed fashion [6,40,41,42,43]. Indeed the mean patient age was 3 months, whilst van Douveren et al. in their milestone work enrolled 13 patients with a mean age of 15 months [12]; also, Beek et al. retrospectively reviewed 33 patients with a mean age of 14 months [17]. On the contrary, Eberhardt et al. (2009) reported on a younger study population (Mean 6.4 weeks, range 1–30 weeks) and found similar results (2/68 dislocated hips). In the present study, there might be a bias drifting towards less difficult cases. The hips reducibility was tested (clinically and with TIT) before performing the procedure and irreducible hips were not included; moreover, TIT was performed during the execution of the SC and this could have influenced the rate of true positives, similarly as in case ID Nr 1. This feature is unique to TIT, in opposition to MR and CT, which are usually [37] used only after reduction and SC completion.
According to van Douveren et al. [12], a hip is defined as dislocated if the modified Shenton line between the ramus superior of os pubis and the femoral neck is interrupted [33]. To date, there are no data concerning the quantification of this interruption, as TIT has only a dichotomous binary outcome (the femoral head is reduced or not). However, the advantage of a simple binary outcome [35,36] could be confirmed in our study, with 100% agreement to the more accurate MR images.
Although TIT was developed as a technique to distinguish if a hip is dislocated or not, Eberhardt et al. already noticed how TIT might conceive further information. The thickness of the connective soft tissue occupying the fossa acetabuli can be visualized, together with the behavior of this soft tissue during the reduction maneuver (is this soft tissue moved apart from the femoral head? Is it still present in the fossa acetabuli after reduction?) [10,44]. These anatomical issues have not been considered nor analyzed in the present study.
The main advantages of the present study include the following: data from consecutive patients were collected prospectively; the control group was based on MR, which is a gold standard for the evaluation of the infant hip [5]; one surgeon used the same protocol and followed-up every single patient. The main limitations of this study must be acknowledged. First, it was designed to investigate the concordance between MR and TIT, not sensibility and specificity. Thus, their computation would not be trustworthy, according to study design and sample size. Second, this study was not blinded, and TIT possibly influenced surgeon’s decisions. In other words, even if this study is observational, TIT might have inferenced the results. Third, TIT was performed once for each procedure, by the same clinician who also evaluated the images: an intra-/interobserver assessment was not performed.
Concerning further clinical developments, the use of a static brace as an alternative to a Pavlik harness and SC to treat critical hips has already been described [10,20,45]. Utilizing bed-side ultrasound techniques to check the position of the femoral head could immediately provide the information that the clinician needs for the treatment [38] in the operating room and in an outpatient setting. Moreover, a preoperative outpatient evaluation with TIT might help to prepare families and clinicians when a reduction in narcosis is planned [4].
5. Conclusions
In the present study MR and ultrasound showed perfect agreement in detecting the position of the femoral head. The inguinal ultrasound technique according to van Douveren can be considered a reliable alternative to check the hip in spica cast for the conservative treatment of severe hip dysplasia in infants.
Author Contributions
Conceptualization, N.G.; Methodology, N.G. and M.D.P.; Software, N.G.; Validation, N.G., M.D.P. and F.C.; Formal analysis, M.D.P.; Investigation, N.G.; Resources, F.C.; Data curation, N.G.; Writing—original draft preparation, N.G.; Writing—review and editing, M.D.P. and F.C.; Visualization, F.C.; Supervision, F.C.; Project administration, F.C.; Funding acquisition, F.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Ethics Committee of Bergamo, ASST Papa Giovanni XXIII, approval code: 2021-0134; approval date: 15 June 2021.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Raw data are already contained within the study. All images presented in this study are not publicly available due to privacy and ethics, but anonymous copies are available on reasonable request from the corresponding author (N.G.).
Acknowledgments
The Authors acknowledge Carioli Greta, from the FROM foundation (Fondazione Ricerca Ospedale Maggiore di Bergamo) for her essential support in statistics.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Graf, R.; Scott, S.; Lercher, K.; Baumgartner, F.; Benaroya, A. Hip sonography: Diagnosis and management of infant hip dysplasia. In Hip Sonography: Diagnosis and Management of Infant Hip Dysplasia; Springer: Berlin/Heidelberg, Germany, 2006; pp. 1–114. [Google Scholar]
- De Pellegrin, M.; Moharamzadeh, D.; Fraschini, G. Early diagnosis and treatment of DDH: A sonographic approach. HIP Int. 2007, 17 (Suppl. 5), 15–21. [Google Scholar] [CrossRef]
- Tschauner, C.; Fürntrath, F.; Saba, Y.; Berghold, A.; Radl, R. Developmental dysplasia of the hip: Impact of sonographic newborn hip screening on the outcome of early treated decentered hip joints-a single center retrospective comparative cohort study based on Graf’s method of hip ultrasonography. J. Child. Orthop. 2011, 5, 415–424. [Google Scholar] [CrossRef]
- Fettweis, E. Sitz-Hock-Stellungsgips bei Hiiftgelenksdysplasien. Arch. Orthop. Trauma Surg. 1968, 51, 38–51. [Google Scholar]
- Kubo, H.; Pilge, H.; Holthoff, J.P.; Westhoff, B.; Krauspe, R. MRI reveals unrecognized treatment failures after application of Fettweis plaster in children with unstable hip joints. J. Pediatr. Orthop. Part B 2019, 28, 430–435. [Google Scholar] [CrossRef]
- Eberhardt, O.; Wirth, T. Hip dysplasia—New and proven methods. Orthopade 2019, 48, 508–514. [Google Scholar] [CrossRef] [PubMed]
- Mandel, D.M.; Loder, R.T.; Hensinger, R.N. The Predictive Value of Computed Tomography in the Treatment of Developmental Dysplasia of the Hip. J. Pediatr. Orthop. 1998, 18, 794–798. [Google Scholar] [CrossRef] [PubMed]
- Guyer, B.; Smith, D.S.; Cady, R.B.; Bassano, D.A.; Levinshn, E.M. Dosimetry of computerized tomography in the evaluation of hip dysplasia. Skelet. Radiol. 1984, 12, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Helms, C.A.; Goodman, P.C.; Brooke Jeffrey, R. Use of computed tomography in congenital dislocation of the hip. J. Comput. Tomogr. 1983, 7, 363–365. [Google Scholar] [CrossRef] [PubMed]
- Eberhardt, O.; Zieger, M.; Wirth, T.; Fernandez, F.F. Determination of femoral head position with transinguinal ultrasound in DDH treatment. Z. Orthop. Unfall. 2009, 147, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Bachy, M.; Thevenin-Lemoine, C.; Rogier, A.; Mary, P.; Le Pointe, H.D.; Vialle, R. Utility of magnetic resonance imaging (MRI) after closed reduction of developmental dysplasia of the hip. J. Child. Orthop. 2012, 6, 13–20. [Google Scholar] [CrossRef] [PubMed]
- van Douveren, F.Q.M.P.; Pruijs, H.E.H.; Sakkers, R.J.B.; Nievelstein, R.A.J.; Beek, F.J.A. Ultrasound in the management of the position of the femoral head during treatment in a spica cast after reduction of hip dislocation in developmental dysplasia of the hip. J. Bone Jt. Surg. Ser. B 2003, 85, 117–120. [Google Scholar] [CrossRef]
- Graf, R. Hip sonography: Background; technique and common mistakes; results; debate and politics; challenges. HIP Int. 2017, 27, 215–219. [Google Scholar] [CrossRef]
- Mehdizadeh, M.; Dehnavi, M.; Tahmasebi, A.; Mahlisha Kazemi Shishvan, S.A.; Babakhan Kondori, N.; Shahnazari, R. Transgluteal ultrasonography in spica cast in postreduction assessment of developmental dysplasia of the hip. J. Ultrasound 2020, 23, 509–514. [Google Scholar] [CrossRef]
- Limpaphayom, N. CORR Insights®: Is Hip Medial Ultrasound More Accurate Than Radiography for Determining the Status of Hip Reduction in Children Treated with a Spica Cast? A Retrospective Diagnostic Accuracy Study. Clin. Orthop. Relat. Res. 2023, 481, 606–607. [Google Scholar] [CrossRef]
- Yu, J.; Duan, F.; Guo, W.; Wang, D.; Qin, X.; Fu, G.; Chen, T. Consistency of Indices Obtained via Hip Medial Ultrasound and Magnetic Resonance Imaging in Reduction and Spica Cast Treatment for Developmental Dysplasia of the Hip. Ultrasound Med. Biol. 2021, 47, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Kubo, H.; Krauspe, R.; Pilge, H.; Westhoff, B. Radiological long-term follow-up up to 12 years of initially ultrasound unstable hip types D, III and IV after treatment with the Tübingen splint worn as a plaster. Arch. Orthop. Trauma Surg. 2023, 143, 4871–4878. [Google Scholar] [CrossRef] [PubMed]
- Terjesen, T. Residual hip dysplasia as a risk factor for osteoarthritis in 45 years follow-up of late-detected hip dislocation. J. Child. Orthop. 2011, 5, 425–431. [Google Scholar] [CrossRef]
- Haertlé, M.; Hawi, H.; Windhagen, H.; Becker, N.; Ahmad, S.S. Fifty percent of patients undergoing periacetabular osteotomy for hip dysplasia showed normal findings upon neonatal ultrasound screening: Symptomatic hip dysplasia in adulthood despite inconspicuous neonatal hip ultrasound. Orthopadie 2023, 52, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Baghdadi, S.; Sankar, W.N. Residual Acetabular Dysplasia in the Reduced Hip. Indian J. Orthop. 2020, 55, 1480–1489. [Google Scholar] [CrossRef] [PubMed]
- Kubo, H.; Pilge, H.; Nepp, K.; Westhoff, B.; Krauspe, R. Development of unstable hips after treatment with the Tübingen splint: Mid-term follow-up of 83 hip joints. Arch. Orthop. Trauma Surg. 2018, 138, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Riffenburgh, R.; Gillen, D. Statistics in Medicine, 4th ed.; Academic Press: Cambridge, UK; Elsevier: Amsterdam, The Netherlands, 2020. [Google Scholar]
- Walter, S.D.; Eliasziw, M.D.A. Sample size and optimal designs for reliability studies. Stat. Med. 1998, 17, 101–110. [Google Scholar] [CrossRef]
- Cantor, A.B. Sample-Size Calculations for Cohen’s Kappa. Psychol. Methods 1996, 1, 150–153. Available online: https://psycnet.apa.org/record/1996-04469-003 (accessed on 20 November 2023). [CrossRef]
- Graf, R.; Baumgartner, F.; Lercher, K. Ultraschalldiagnostik der Säuglingshüfte. Ein Atlas; Springer: Berlin/Heidelberg, Germany, 2006. [Google Scholar]
- Tönnis, D. Normal Values of the Hip Joint for the Evaluation of X-rays in Children and Adults. Clin. Orthop. Relat. Res. 1976, 119, 39–47. [Google Scholar]
- Novais, E.N.; Pan, Z.; Autruong, P.T.; Meyers, M.L.; Chang, F.M. Normal Percentile Reference Curves and Correlation of Acetabular Index and Acetabular Depth Ratio in Children. J. Pediatr. Orthop. 2018, 38, 163–169. [Google Scholar] [CrossRef]
- Pun, S. Hip dysplasia in the young adult caused by residual childhood and adolescent-onset dysplasia. Curr. Rev. Musculoskelet. Med. 2016, 9, 427–434. [Google Scholar] [CrossRef]
- De Pellegrin, M.; Montanari, L.; Moharamzadeh, D.; Eberhardt, O. The role of the labrum in early treatment of unstable developmental dysplasia of the hip. EFORT Open Rev. 2019, 4, 296–301. [Google Scholar] [CrossRef]
- Smith, B.G.; Kasser, J.R.; Hey, L.A.; Jaramillo, D.; Millis, M.B. Postreduction Computed Tomography in Developmental Dislocation of the Hip: Part I: Analysis of Measurement Reliability. J. Pediatr. Orthop. 1997, 17, 626–630. [Google Scholar] [CrossRef] [PubMed]
- Westhoff, B.; Wild, A.; Seller, K.; Krauspe, R. Magnetic resonance imaging after reduction for congenital dislocation of the hip. Arch. Orthop. Trauma Surg. 2003, 123, 289–292. [Google Scholar] [CrossRef] [PubMed]
- Gould, S.W.; Grissom, L.E.; Niedzielski, A.; Kecskemethy, H.H.; Bowen, J.R.; Harcke, H.T. Protocol for MRI of the hips after spica cast placement. J. Pediatr. Orthop. 2012, 32, 504–509. [Google Scholar] [CrossRef] [PubMed]
- Laor, T.; Jaramillo, D. MR imaging insights into skeletal maturation: What is normal? Radiology 2009, 250, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Vandevenne, J.E.; Lincoln, T.; Butts Pauly, K.; Rinsky, L.; Lang, P.K. Magnetic resonance imaging-guided closed reduction treatment for developmental dysplasia of the hip. Singap. Med. J. 2009, 50, 407–411. [Google Scholar]
- De Pellegrin, M.M.D. Immediate closed reduction of congenital dislocation of the hip. J. Child. Orthop. 2009, 3 (Suppl. 1), 22. [Google Scholar]
- De Pellegrin, M.; Fracassetti, D. Displasia dell’anca. Strategie a confronto per la diagnosi precoce. Il Pediatra 2014, 3, 46–53. [Google Scholar]
- De Pellegrin, M.; Bonifacini, C. Einfluss des Alters in der Frühbe hand—Lung einer schweren Hüftdysplasie auf die Pfannendachentwicklung. OUP 2016, 5, 408–412. [Google Scholar]
- Fawcett, S.L.; Barter, S.J. The use of gonad shielding in paediatric hip and pelvis radiographs. Br. J. Radiol. 2009, 82, 363–370. [Google Scholar] [CrossRef] [PubMed]
- O’Beirne, J.G.; Chlapoutakis, K.; Alshryda, S.; Aydingoz, U.; Baumann, T.; Casini, C.; de Pellegrin, M.; Domos, G.; Dubs, B.; Hemmadi, S.; et al. International Interdisciplinary Consensus Meeting on the Evaluation of Developmental Dysplasia of the Hip. Ultraschall Med. 2019, 40, 454–464. [Google Scholar]
- Farsetti, P.; Efremov, K.; Caterini, A.; Marsiolo, M.; De Maio, F.; Ippolito, E. The effectiveness of preliminary traction in the treatment of congenital dislocation of the hip. J. Orthop. Traumatol. 2021, 22, 26. [Google Scholar] [CrossRef] [PubMed]
- Eberhardt, O.; Fernandez, F.F.; Wirth, T. Arthroscopic reduction of the dislocated hip in infants. J. Bone Jt. Surg. Ser. B 2012, 94, 842–847. [Google Scholar] [CrossRef]
- Kubo, H.; Pilge, H.; Weimann-Stahlschmidt, K.; Stefanovska, K.; Westhoff, B.; Krauspe, R. Use of the Tübingen splint for the initial management of severely dysplastic and unstable hips in newborns with DDH: An alternative to Fettweis plaster and Pavlik harness. Arch. Orthop. Trauma Surg. 2018, 138, 149–153. [Google Scholar] [CrossRef]
- Suzuki, S.; Kasahara, Y.; Futami, T.; Ushikubo, S.; Tsuchiya, T. Ultrasonography in congenital dislocation of the hip. Simultaneous imaging of both hips from in front. J. Bone Jt. Surg. Br. 1991, 73, 879–883. [Google Scholar] [CrossRef]
- Beek, F.J.A.; Nievelstein, R.J.; Pruijs, H.E.; De Jong, P.A.; Sakkers, R.J.B. Transinguinal sonographic determination of the position of the femoral head after reposition and follow-up in a spica cast. Pediatr. Radiol. 2010, 40, 1794–1799. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.C.; Lloyd, J.; Solomito, M.J. Poor utility of gonadal shielding for pediatric pelvic radiographs. Orthopedics 2017, 40, e623–e627. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).