Intrainstitutional Changes of the Treatment of Supracondylar Humerus Fracture in Children over a Period of 9 Years
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Acquisition
2.2. Questionnaire Study
2.3. Data Analysis and Ethics Committee Approval
3. Results
3.1. Patient Characteristics
3.2. Fracture Types
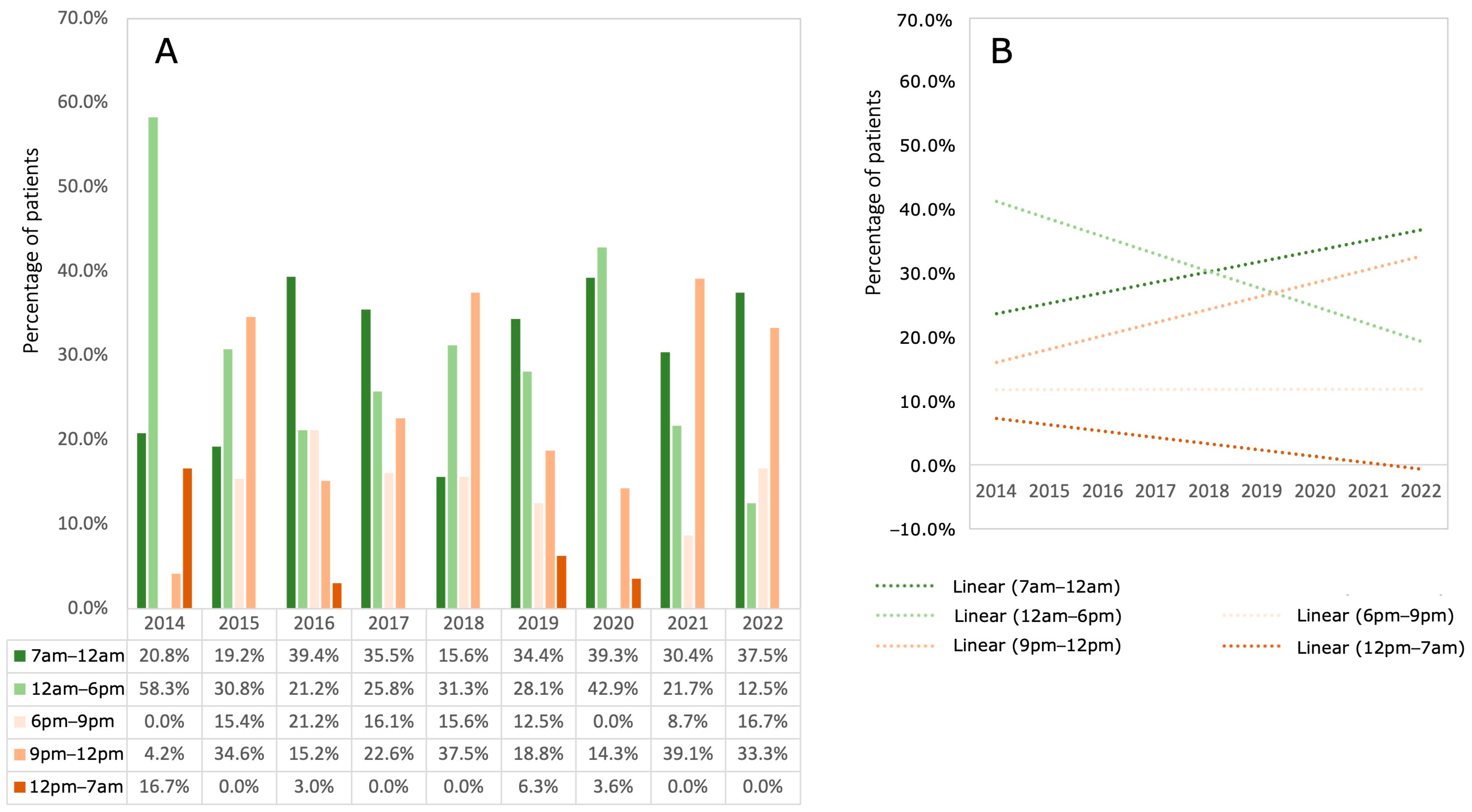
3.3. Time of Day (TD) the Surgery Started
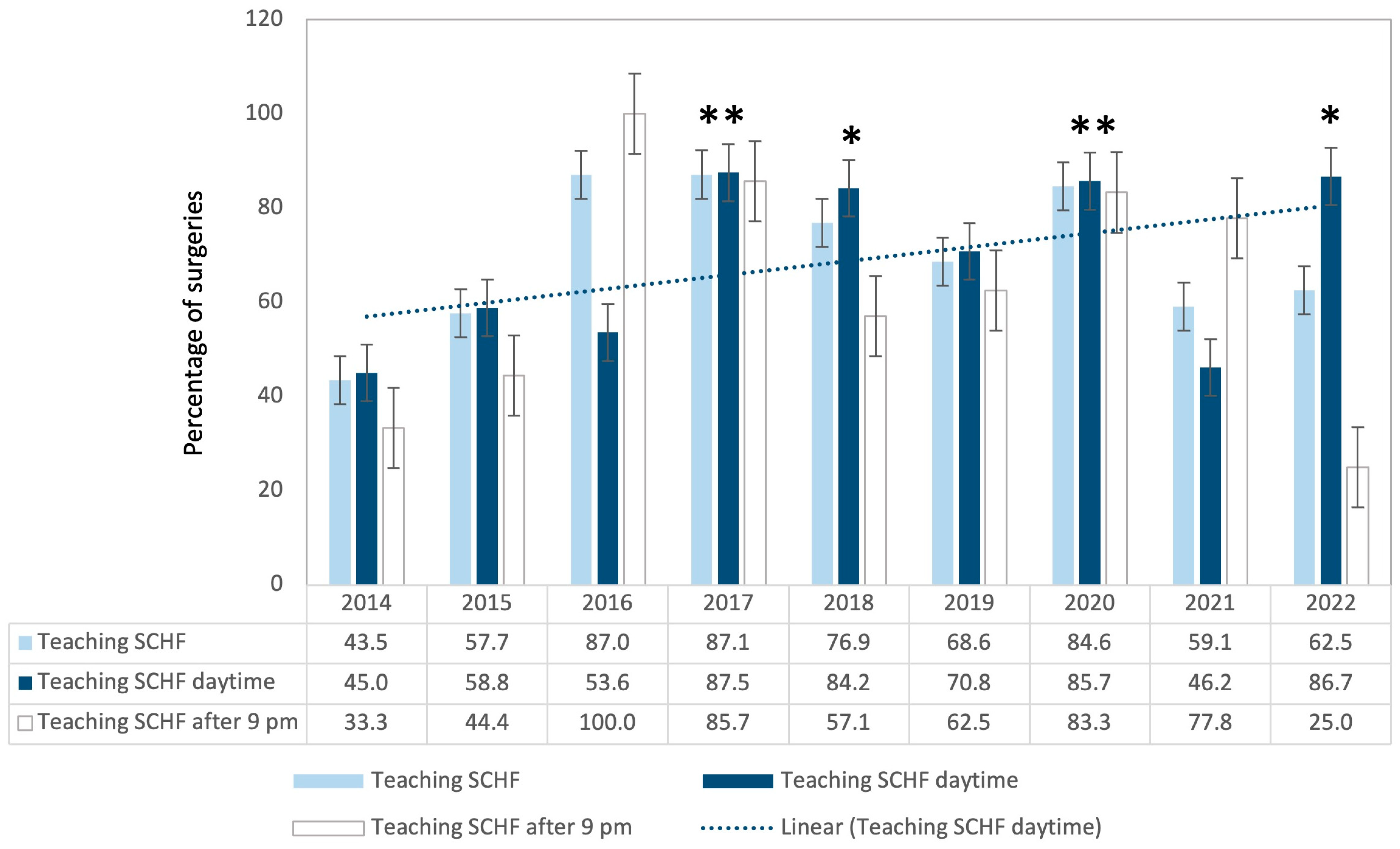
3.4. Teaching Interventions
3.5. Operative Time (OT)
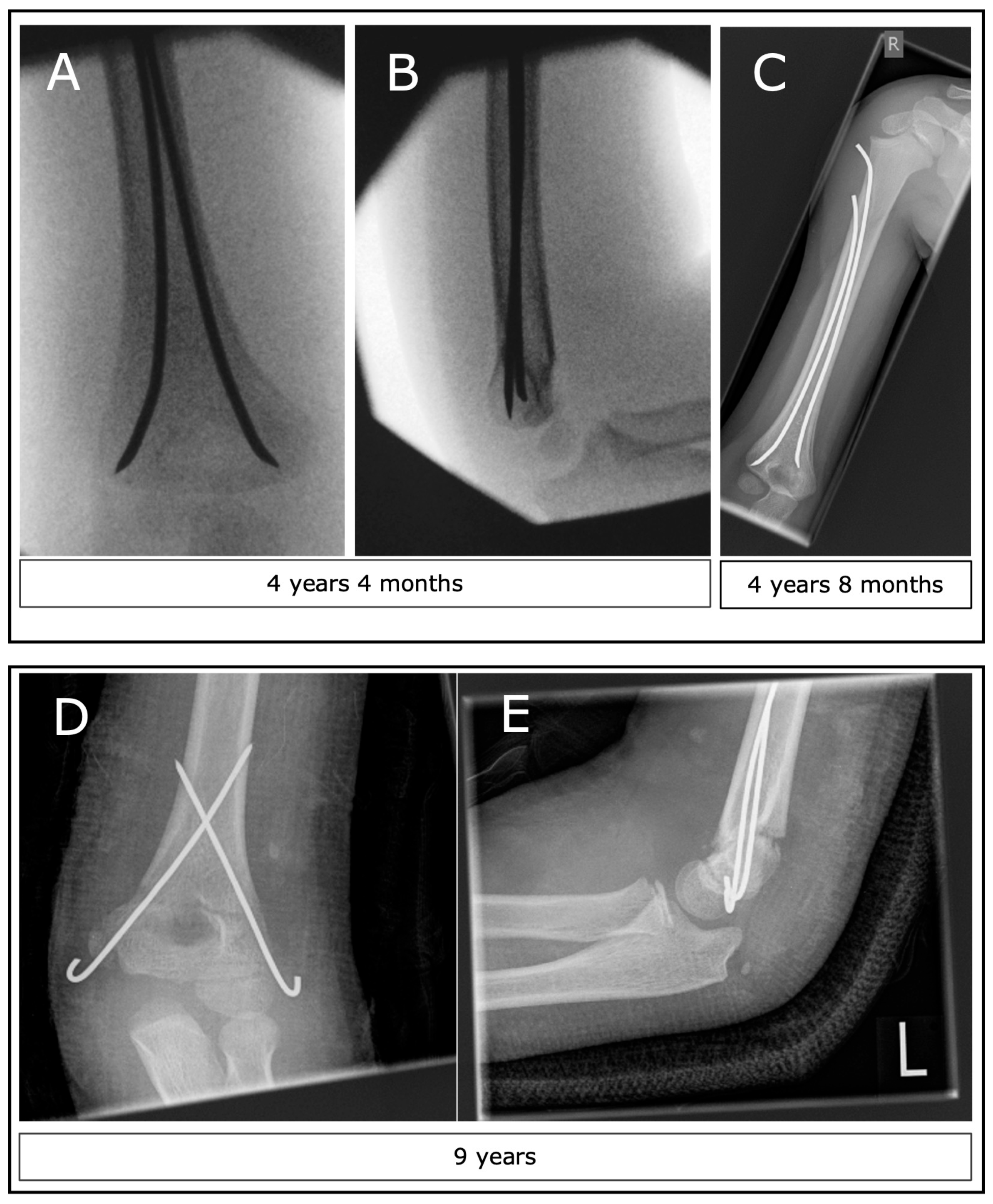
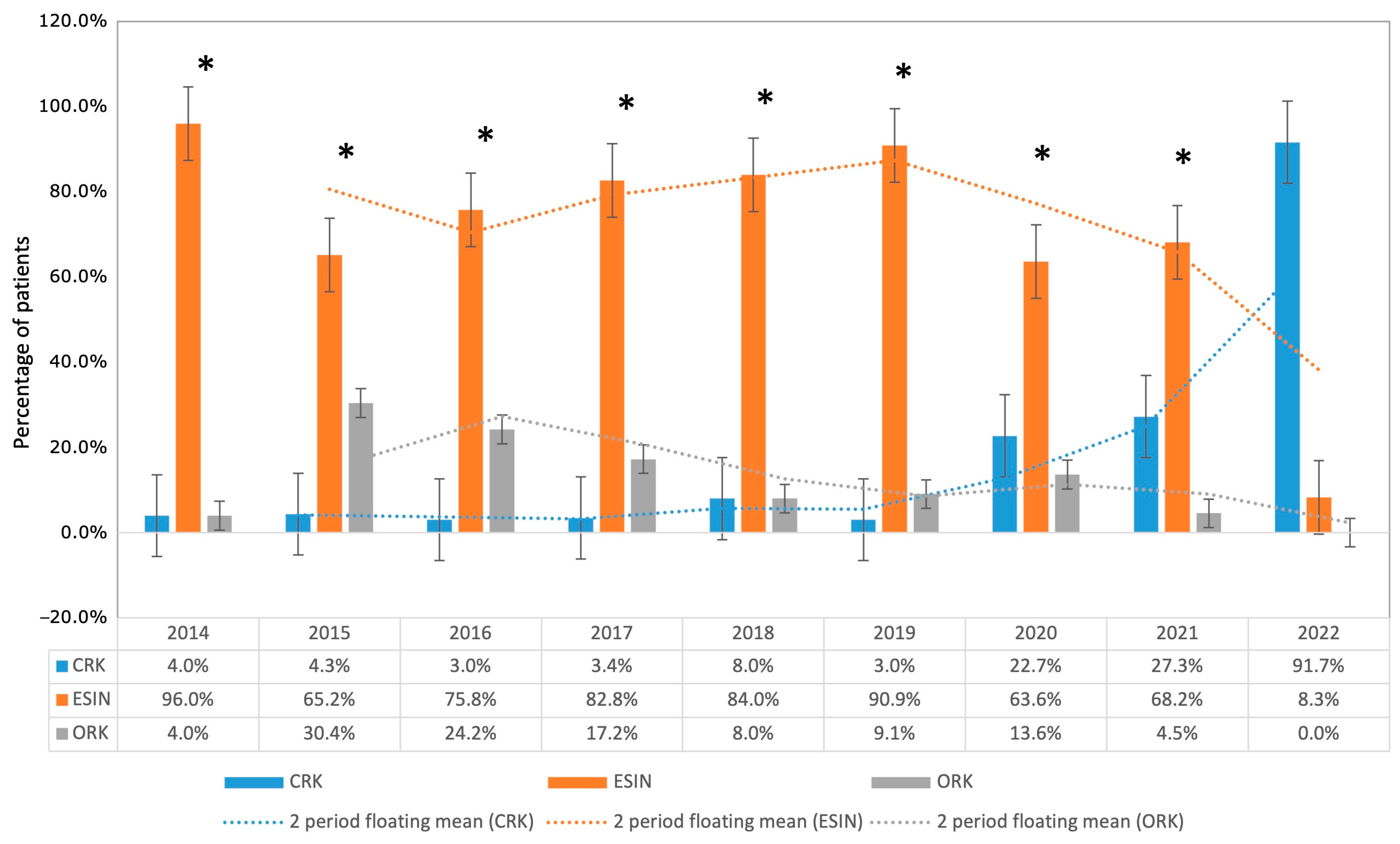
3.6. Operative Technique (CRK, ESIN, ORK)
3.7. Questionnaires
4. Discussion
4.1. General Discussion
4.2. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Minkowitz, B.; Busch, M.T. Supracondylar humerus fractures. Current trends and controversies. Orthop. Clin. N. Am. 1994, 25, 581–594. [Google Scholar] [CrossRef]
- Cheng, J.C.; Lam, T.P.; Maffulli, N. Epidemiological features of supracondylar fractures of the humerus in Chinese children. J. Pediatr. Orthop. B 2001, 10, 63–67. [Google Scholar] [PubMed]
- Otsuka, N.Y.; Kasser, J.R. Supracondylar Fractures of the Humerus in Children. J. Am. Acad. Orthop. Surg. 1997, 5, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Omid, R.; Choi, P.D.; Skaggs, D.L. Supracondylar humeral fractures in children. J. Bone Jt. Surg. Am. 2008, 90, 1121–1132. [Google Scholar] [CrossRef] [PubMed]
- Farnsworth, C.L.; Silva, P.D.; Mubarak, S.J. Etiology of supracondylar humerus fractures. J. Pediatr. Orthop. 1998, 18, 38–42. [Google Scholar] [CrossRef]
- Abzug, J.M.; Herman, M.J. Management of supracondylar humerus fractures in children: Current concepts. J. Am. Acad. Orthop. Surg. 2012, 20, 69–77. [Google Scholar] [CrossRef]
- Lacher, M.; Schaeffer, K.; Boehm, R.; Dietz, H.G. The treatment of supracondylar humeral fractures with elastic stable intramedullary nailing (ESIN) in children. J. Pediatr. Orthop. 2011, 31, 33–38. [Google Scholar] [CrossRef]
- Wendling-Keim, D.S.; Binder, M.; Dietz, H.G.; Lehner, M. Prognostic Factors for the Outcome of Supracondylar Humeral Fractures in Children. Orthop. Surg. 2019, 11, 690–697. [Google Scholar] [CrossRef]
- Dietz, H.G.; Illing, P.; Schmittenbecher, P.P.; Slongo, T.; Sommerfeldt, D.W. Praxis der Kinder- und Jugendtraumatologie; Springer: Berlin/Heidelberg, Germany, 2011. [Google Scholar]
- Hering, J.A.; Ho, C. Upper Extremity Injuries. Tachdjian’s Pediatric Orthopaedics, 5th ed.; Saunders: Philadelphia, PA, USA, 2014. [Google Scholar]
- Marzi, I. Kindertraumatologie; Springer: Berlin/Heidelberg, Germany, 2016. [Google Scholar]
- Franca, U.L.; McManus, M.L. An Approach to Consolidating Pediatric Hospital Beds During the COVID-19 Surge. Pediatrics 2020, 146, e20201464. [Google Scholar] [CrossRef]
- Hoffmann, F.; Landeg, M.; Rittberg, W.; Hinzmann, D.; Steinbrunner, D.; Bocker, W.; Heinen, F.; Kanz, K.G.; Bogner-Flatz, V. Pediatric Emergencies-Worsening Care Bottlenecks as Exemplified in a Major German City. Dtsch. Arztebl. Int. 2021, 118, 373–374. [Google Scholar] [CrossRef]
- Bowyer, M.W.; Andreatta, P.B.; Armstrong, J.H.; Remick, K.N.; Elster, E.A. A Novel Paradigm for Surgical Skills Training and Assessment of Competency. JAMA Surg. 2021, 156, 1103–1109. [Google Scholar] [CrossRef] [PubMed]
- Liebs, T.R.; Burgard, M.; Kaiser, N.; Slongo, T.; Berger, S.; Ryser, B.; Ziebarth, K. Health-related quality of life after paediatric supracondylar humeral fractures. Bone Jt. J. 2020, 102-B, 755–765. [Google Scholar] [CrossRef] [PubMed]
- Lutz, N.; Audige, L.; Schmittenbecher, P.; Clavert, J.M.; Frick, S.; Slongo, T. Diagnostic algorithm for a validated displacement grading of pediatric supracondylar fractures. J. Pediatr. Orthop. 2011, 31, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Hudak, P.L.; Amadio, P.C.; Bombardier, C. Development of an upper extremity outcome measure: The DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am. J. Ind. Med. 1996, 29, 602–608. [Google Scholar] [CrossRef]
- Kreimeier, S.; Astrom, M.; Burstrom, K.; Egmar, A.C.; Gusi, N.; Herdman, M.; Kind, P.; Perez-Sousa, M.A.; Greiner, W. EQ-5D-Y-5L: Developing a revised EQ-5D-Y with increased response categories. Qual. Life Res. 2019, 28, 1951–1961. [Google Scholar] [CrossRef] [PubMed]
- Kreimeier, S.; Greiner, W. Development of the German version of EQ-5D-Y-5L to measure health-related quality of life in children and adolescents: Identification of response labels and pilot testing. Z. Evid. Fortbild Qual. Gesundheitswesen 2019, 144–145, 24–34. [Google Scholar] [CrossRef]
- Kreimeier, S.; Greiner, W. EQ-5D-Y as a Health-Related Quality of Life Instrument for Children and Adolescents: The Instrument’s Characteristics, Development, Current Use, and Challenges of Developing Its Value Set. Value Health 2019, 22, 31–37. [Google Scholar] [CrossRef]
- Musters, L.; Diederix, L.W.; Roth, K.C.; Edomskis, P.P.; Kraan, G.A.; Allema, J.H.; Reijman, M.; Colaris, J.W. Below-elbow cast sufficient for treatment of minimally displaced metaphyseal both-bone fractures of the distal forearm in children: Long-term results of a randomized controlled multicenter trial. Acta Orthop. 2021, 92, 468–471. [Google Scholar] [CrossRef]
- Verstraete, J.; Lloyd, A.; Scott, D.; Jelsma, J. How does the EQ-5D-Y Proxy version 1 perform in 3, 4 and 5-year-old children? Health Qual. Life Outcomes 2020, 18, 149. [Google Scholar] [CrossRef]
- Chen, C.; Zhang, X.; Gu, C.; Wang, Y.; Liu, K.; Pan, X.; Fu, S.; Fan, L.; Wang, R. Surgery performed at night by continuously working surgeons contributes to a higher incidence of intraoperative complications in video-assisted thoracoscopic pulmonary resection: A large monocentric retrospective study. Eur. J. Cardiothorac. Surg. 2020, 57, 447–454. [Google Scholar] [CrossRef]
- De Simone, B.; Kluger, Y.; Moore, E.E.; Sartelli, M.; Abu-Zidan, F.M.; Coccolini, F.; Ansaloni, L.; Tebala, G.D.; Di Saverio, S.; Di Carlo, I.; et al. The new timing in acute care surgery (new TACS) classification: A WSES Delphi consensus study. World J. Emerg. Surg 2023, 18, 32. [Google Scholar] [CrossRef] [PubMed]
- Bales, J.G.; Spencer, H.T.; Wong, M.A.; Fong, Y.J.; Zionts, L.E.; Silva, M. The effects of surgical delay on the outcome of pediatric supracondylar humeral fractures. J. Pediatr. Orthop. 2010, 30, 785–791. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.; Kay, R.M.; Leitch, K.; Femino, J.D.; Tolo, V.T.; Skaggs, D.L. Effect of surgical delay on perioperative complications and need for open reduction in supracondylar humerus fractures in children. J. Pediatr. Orthop. 2004, 24, 245–248. [Google Scholar] [CrossRef] [PubMed]
- Mehlman, C.T.; Strub, W.M.; Roy, D.R.; Wall, E.J.; Crawford, A.H. The effect of surgical timing on the perioperative complications of treatment of supracondylar humeral fractures in children. J. Bone Jt. Surg. Am. 2001, 83, 323–327. [Google Scholar] [CrossRef]
- Sullivan, M.H.; Wahlig, B.D.; Broida, S.E.; Larson, A.N.; Shaughnessy, W.J.; Stans, A.A.; Milbrandt, T.A. Does Shorter Time to Treatment of Pediatric Supracondylar Humerus Fractures Impact Clinical Outcomes? J. Pediatr. Orthop. 2023, 43, 350–354. [Google Scholar] [CrossRef]
- Holme, T.J.; Crate, G.; Trompeter, A.J.; Monsell, F.P.; Bridgens, A.; Gelfer, Y. Preoperative vascular assessment of patients with a supracondylar humeral fracture and a perfused, pulseless limb. Bone Jt. J. 2023, 105-B, 231–238. [Google Scholar] [CrossRef]
- Louahem, D.; Cottalorda, J. Acute ischemia and pink pulseless hand in 68 of 404 gartland type III supracondylar humeral fractures in children: Urgent management and therapeutic consensus. Injury 2016, 47, 848–852. [Google Scholar] [CrossRef]
- Delniotis, I.; Delniotis, A.; Saloupis, P.; Gavriilidou, A.; Galanis, N.; Kyriakou, A.; Potoupnis, M.; Tsiridis, E.; Ktenidis, K. Management of the Pediatric Pulseless Supracondylar Humeral Fracture: A Systematic Review and Comparison Study of "Watchful Expectancy Strategy" Versus Surgical Exploration of the Brachial Artery. Ann. Vasc. Surg. 2019, 55, 260–271. [Google Scholar] [CrossRef]
- Stichhauer, R.; Preis, J.; Planka, L.; Turek, J.; Urban, J.; Horak, Z.; Zeman, J.; Konecny, M.; Kopacek, I.; Hanak, F.; et al. Strategy of pulseless pink supracondylar humerus fracture treatment in children: A comparison of two approaches. Eur. J. Trauma Emerg. Surg. 2022, 48, 3785–3791. [Google Scholar] [CrossRef]
- Wilks, D.J.; Ye, X.; Biggins, R.; Wang, K.K.; Wade, R.G.; McCombe, D. Median Nerve Palsy in Pediatric Supracondylar Humerus Fractures Recovers Faster with Open Than Closed Reduction. J. Pediatr. Orthop. 2023, 43, 407–413. [Google Scholar] [CrossRef]
- Weber, M.; Worlicek, M.; Voellner, F.; Woerner, M.; Benditz, A.; Weber, D.; Grifka, J.; Renkawitz, T. Surgical training does not affect operative time and outcome in total knee arthroplasty. PLoS ONE 2018, 13, e0197850. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, S.E.; Crawford, L.; Holmes, S.; Kadado, A.A.; Memon, R.; Souder, C.D.; Swarup, I.; Halsey, M. Return to the Operating Room for Unplanned Pin Removal After Percutaneous Pinning of Supracondylar Humerus Fractures: A Retrospective Review. J. Pediatr. Orthop. 2023, 43, e508–e512. [Google Scholar] [CrossRef] [PubMed]
- Schneidmueller, D.; Eijkenboom, A.; Brand, A.; Langenhan, R.; Kertai, M.; Voth, M.; Adrian, M.; Loose, O.; Bohn, B.; Wagner, F.; et al. To Bury or Not to Bury-Kirschner Wire Fixation in Children and Adolescents. Dtsch. Arztebl. Int. 2022, 119, 818–819. [Google Scholar] [CrossRef] [PubMed]
- Canavese, F.; Marengo, L.; Samba, A.; Rousset, M.; Mansour, M.; Andreacchio, A.; Dimeglio, A. Evaluation of upper extremity function of displaced diaphyseal humeral fractures in children treated by elastic stable intramedullary nailing: Preliminary results. J. Pediatr. Orthop. B 2016, 25, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Sapienza, M.; Testa, G.; Vescio, A.; Panvini, F.M.C.; Caldaci, A.; Parisi, S.C.; Pavone, V.; Canavese, F. The Role of Patient Position in the Surgical Treatment of Supracondylar Fractures of the Humerus: Comparison of Prone and Supine Position. Medicina 2023, 59, 374. [Google Scholar] [CrossRef] [PubMed]
- Eberl, R.; Eder, C.; Smolle, E.; Weinberg, A.M.; Hoellwarth, M.E.; Singer, G. Iatrogenic ulnar nerve injury after pin fixation and after antegrade nailing of supracondylar humeral fractures in children. Acta Orthop. 2011, 82, 606–609. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Kamara, A.; Liu, T.; Yan, Y.; Wang, E. Mechanical stability study of three techniques used in the fixation of transverse and oblique metaphyseal-diaphyseal junction fractures of the distal humerus in children: A finite element analysis. J. Orthop. Surg. Res. 2020, 15, 34. [Google Scholar] [CrossRef]
- Greve, F.; Biberthaler, P.; Castellani, C.; Singer, G.; Till, H.; Wegmann, H. Beneficial Perioperative Aspects Favor the Use of Percutaneous Crossed Pinning over Antegrade Nailing in Pediatric Supracondylar Fractures—A Retrospective Comparative Study. Children 2023, 10, 830. [Google Scholar] [CrossRef]
- Green, D.W.; Widmann, R.F.; Frank, J.S.; Gardner, M.J. Low incidence of ulnar nerve injury with crossed pin placement for pediatric supracondylar humerus fractures using a mini-open technique. J. Orthop. Trauma 2005, 19, 158–163. [Google Scholar] [CrossRef]
- Haddad, A.; Janda, A.; Renk, H.; Stich, M.; Frieh, P.; Kaier, K.; Lohrmann, F.; Nieters, A.; Willems, A.; Huzly, D.; et al. Long COVID symptoms in exposed and infected children, adolescents and their parents one year after SARS-CoV-2 infection: A prospective observational cohort study. EBioMedicine 2022, 84, 104245. [Google Scholar] [CrossRef]
- Long, D.; Bonsel, G.J.; Lubetkin, E.I.; Yfantopoulos, J.N.; Janssen, M.F.; Haagsma, J.A. Health-Related Quality of Life and Mental Well-Being during the COVID-19 Pandemic in Five Countries: A One-Year Longitudinal Study. J. Clin. Med. 2022, 11, 6467. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wagner, F.; Boeriu, A.; Eberz, P.; Weigert, A.; Holzapfel, B.M.; Böcker, W.; Hubertus, J.; Muensterer, O.; Bergmann, F.; Ziegler, C.M. Intrainstitutional Changes of the Treatment of Supracondylar Humerus Fracture in Children over a Period of 9 Years. Children 2024, 11, 27. https://doi.org/10.3390/children11010027
Wagner F, Boeriu A, Eberz P, Weigert A, Holzapfel BM, Böcker W, Hubertus J, Muensterer O, Bergmann F, Ziegler CM. Intrainstitutional Changes of the Treatment of Supracondylar Humerus Fracture in Children over a Period of 9 Years. Children. 2024; 11(1):27. https://doi.org/10.3390/children11010027
Chicago/Turabian StyleWagner, Ferdinand, Amalia Boeriu, Pascal Eberz, Annabelle Weigert, Boris Michael Holzapfel, Wolfgang Böcker, Jochen Hubertus, Oliver Muensterer, Florian Bergmann, and Christian Max Ziegler. 2024. "Intrainstitutional Changes of the Treatment of Supracondylar Humerus Fracture in Children over a Period of 9 Years" Children 11, no. 1: 27. https://doi.org/10.3390/children11010027
APA StyleWagner, F., Boeriu, A., Eberz, P., Weigert, A., Holzapfel, B. M., Böcker, W., Hubertus, J., Muensterer, O., Bergmann, F., & Ziegler, C. M. (2024). Intrainstitutional Changes of the Treatment of Supracondylar Humerus Fracture in Children over a Period of 9 Years. Children, 11(1), 27. https://doi.org/10.3390/children11010027








