Attrition from Face-to-Face Pediatric Outpatient Chronic Pain Interventions: A Narrative Review and Theoretical Model
Abstract
1. Introduction
2. Prevalence of Attrition from Pediatric Chronic Pain Interventions
3. Evidence Regarding Factors Associated with Attrition from Pediatric Interventions and Adult Chronic Pain Interventions
3.1. Youth Factors
3.2. Caregiver and Family Factors
3.3. Health Service Factors
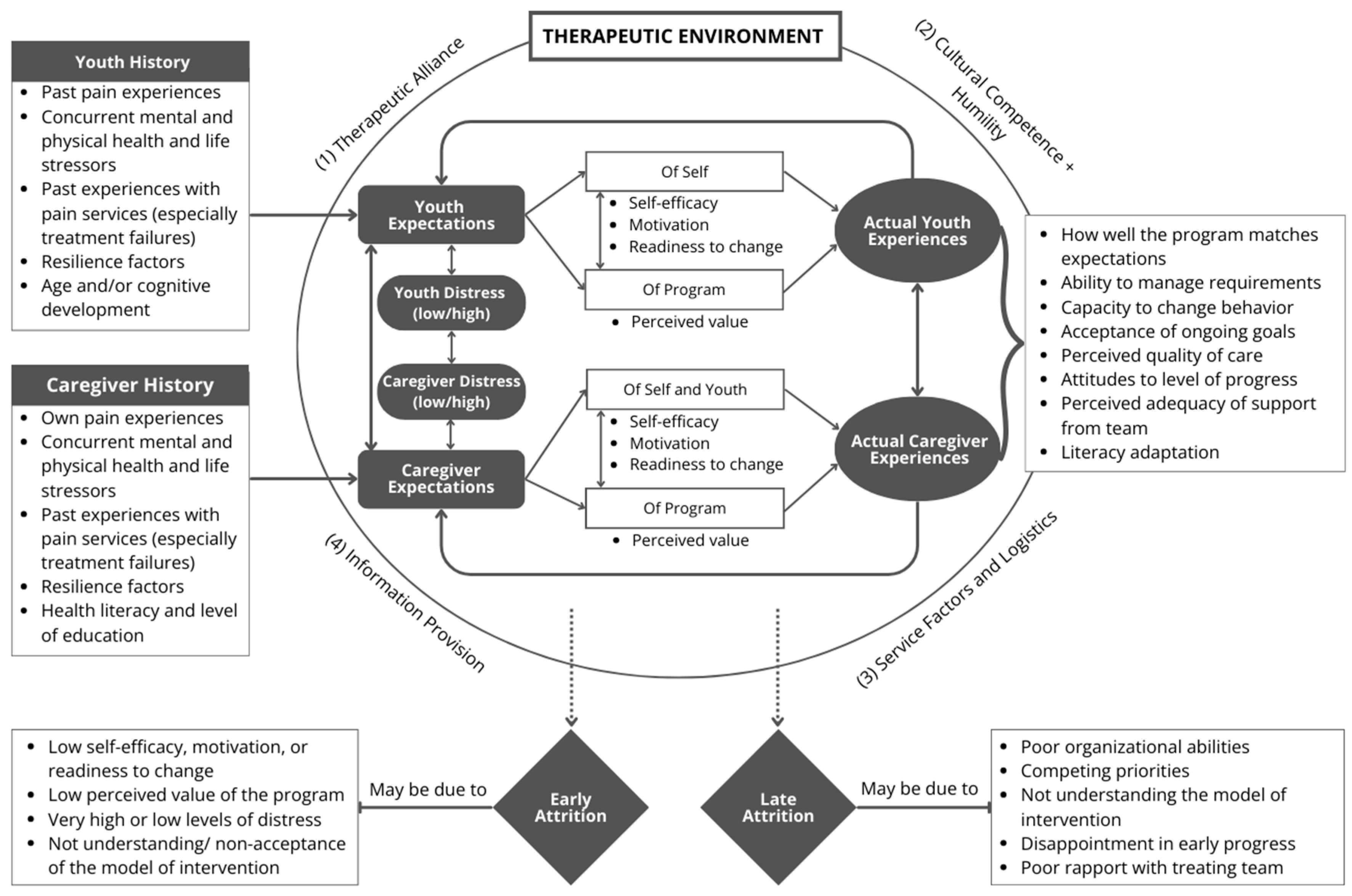
4. Developing a Theoretical Model for Understanding Patient Attrition
4.1. The Therapeutic Environment
4.2. Expectations and Distress Levels of the Youth and Caregiver
4.3. Actual Experiences of Youth and Caregivers of the Intervention
4.4. Background Youth/Caregiver Factors
5. Limitations and Future Research and Clinical Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mindlis, I.; Livert, D.; Federman, A.D.; Wisnivesky, J.P.; Revenson, T.A. Racial/ethnic concordance between patients and researchers as a predictor of study attrition. Soc. Sci. Med. 2020, 255, 113009. [Google Scholar] [CrossRef] [PubMed]
- Toolbox, E. Glossary. Available online: https://toolbox.eupati.eu/glossary (accessed on 23 February 2023).
- Meier, S.T. A model of the early therapeutic environment: Predicting client attrition. J. Psychother. Integr. 2023, 33, 235–247. [Google Scholar] [CrossRef]
- Oosterhaven, J.; Wittink, H.; Mollema, J.; Kruitwagen, C.L.; Deville, W. Predictors of dropout in interdisciplinary chronic pain management programmes: A systematic review. J. Rehabil. Med. 2019, 51, 2–10. [Google Scholar] [CrossRef]
- Suc, A.; Cayzac, D.; Iannuzzi, S.; Garnier, C.; Bonneau, B.; Sommet, A. Peacefull: A French mindfulness-based intervention for adolescents with chronic pain a feasibility study. Arch. Pediatr. 2022, 29, 581–587. [Google Scholar] [CrossRef] [PubMed]
- Ruskin, D.A.; Gagnon, M.M.; Kohut, S.A.; Stinson, J.N.; Walker, K.S. A mindfulness program adapted for adolescents with chronic pain. Clin. J. Pain 2017, 33, 1019–1029. [Google Scholar] [CrossRef] [PubMed]
- Macea, D.D.; Gajos, K.; Daglia Calil, Y.A.; Fregni, F. The Efficacy of Web-Based Cognitive Behavioral Interventions for Chronic Pain: A Systematic Review and Meta-Analysis. J. Pain 2010, 11, 917–929. [Google Scholar] [CrossRef]
- Spence, N.D.; Skelton, J.A.; Ball, G.D.C. A proposed standardized approach to studying attrition in pediatric weight management. Obes. Res. Clin. Pract. 2020, 14, 60–65. [Google Scholar] [CrossRef]
- Dumville, J.C.; Torgerson, D.J.; Hewitt, C.E. Reporting attrition in randomised controlled trials. BMJ 2006, 332, 969–971. [Google Scholar] [CrossRef]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. Available online: https://training.cochrane.org/handbook (accessed on 30 March 2019).
- Fergusson, D. Post-randomisation exclusions: The intention to treat principle and excluding patients from analysis. BMJ 2002, 325, 652–654. [Google Scholar] [CrossRef]
- Gilpin, H.R.; Keyes, A.; Stahl, D.R.; Greig, R.; McCracken, L.M. Predictors of treatment outcome in contextual cognitive and behavioral therapies for chronic pain: A systematic review. J. Pain 2017, 18, 1153–1164. [Google Scholar] [CrossRef]
- Hechler, T.; Kanstrup, M.; Holley, A.L.; Simons, L.E.; Wicksell, R.; Hirschfeld, G.; Zernikow, B. Systematic review on intensive interdisciplinary pain treatment of children with chronic pain. Pediatrics 2015, 136, 115–127. [Google Scholar] [CrossRef] [PubMed]
- Hechler, T.; Martin, A.; Blankenburg, M.; Schroeder, S.; Kosfelder, J.; Hölscher, L.; Denecke, H.; Zernikow, B. Specialized multimodal outpatient treatment for children with chronic pain: Treatment pathways and long-term outcome. Eur. J. Pain 2011, 15, 976–984. [Google Scholar] [CrossRef]
- Liossi, C.; Johnstone, L.; Lilley, S.; Caes, L.; Williams, G.; Schoth, D.E. Effectiveness of interdisciplinary interventions in paediatric chronic pain management: A systematic review and subset meta-analysis. Br. J. Anaesth. 2019, 123, e359–e371. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Lumbi, S.; Ruhe, A.K.; Pfenning, I.; Wager, J.; Zernikow, B. Economic long-term effects of intensive interdisciplinary pain treatment in paediatric patients with severe chronic pain: Analysis of claims data. Eur. J. Pain 2021, 25, 2129–2139. [Google Scholar] [CrossRef] [PubMed]
- Eccleston, C.; Palermo, T.M.; Williams, A.C.; Lewandowski Holley, A.; Morley, S.; Fisher, E.; Law, E. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst. Rev. 2014, 2014, Cd003968. [Google Scholar] [CrossRef]
- Harrison, L.E.; Pate, J.W.; Richardson, P.A.; Ickmans, K.; Wicksell, R.K.; Simons, L.E. Best-Evidence for the Rehabilitation of Chronic Pain Part 1: Pediatric Pain. J. Clin. Med. 2019, 8, 1267. [Google Scholar] [CrossRef]
- Palermo, T.M.; Valrie, C.R.; Karlson, C.W. Family and parent influences on pediatric chronic pain: A developmental perspective. Am. Psychol. 2014, 69, 142. [Google Scholar] [CrossRef]
- Russell, B.S.; Guite, J.W.; Homan, K.J.; Tepe, R.M.; Williams, S.E. Complementary Parent Components for Pediatric Pain Families: Innovations in Treatment. Children 2020, 7, 4. [Google Scholar] [CrossRef]
- Hechler, T.; Ruhe, A.-K.; Schmidt, P.; Hirsch, J.; Wager, J.; Dobe, M.; Krummenauer, F.; Zernikow, B. Inpatient-based intensive interdisciplinary pain treatment for highly impaired children with severe chronic pain: Randomized controlled trial of efficacy and economic effects. Pain 2014, 155, 118–128. [Google Scholar] [CrossRef]
- Palermo, T.M.; Slack, M.; Zhou, C.; Aaron, R.; Fisher, E.; Rodriguez, S. Waiting for a Pediatric Chronic Pain Clinic Evaluation: A Prospective Study Characterizing Waiting Times and Symptom Trajectories. J. Pain 2019, 20, 339–347. [Google Scholar] [CrossRef]
- Robinson, L.; Adair, P.; Coffey, M.; Harris, R.; Burnside, G. Identifying the participant characteristics that predict recruitment and retention of participants to randomised controlled trials involving children: A systematic review. Trials 2016, 17, 294. [Google Scholar] [CrossRef]
- Hilyard, A.; Kingsley, J.; Sommerfield, D.; Taylor, S.; Bear, N.; Gibson, N. Feasibility of a Randomized Controlled Trial of Paediatric Interdisciplinary Pain Management Using Home-Based Telehealth. J. Pain Res. 2020, 13, 897–908. [Google Scholar] [CrossRef]
- Ocay, D.D.; Ross, B.D.; Moscaritolo, L.; Ahmed, N.; Ouellet, J.A.; Ferland, C.E.; Ingelmo, P.M. The Psychosocial Characteristics and Somatosensory Function of Children and Adolescents Who Meet the Criteria for Chronic Nociplastic Pain. J. Pain Res. 2023, 16, 487–500. [Google Scholar] [CrossRef] [PubMed]
- Shear, D.; Harrison, L.E.; O’Brien, S.; Khazendar, Z.; Lyons, S.; Morgan, J.J.; Chan, S.K.; Feinstein, A.B.; Simons, L.E. Rapid Transition to Virtual Assessment and Treatment in an Interdisciplinary Randomized Clinical Trial for Youth with Chronic Pain: Adaptations and Implications for Future Trials. Clin. J. Pain 2022, 38, 459–469. [Google Scholar] [CrossRef] [PubMed]
- Tran, S.T.; Guite, J.W.; Pantaleao, A.; Pfeiffer, M.; Myer, G.D.; Sil, S.; Thomas, S.M.; Ting, T.V.; Williams, S.E.; Edelheit, B.; et al. Preliminary Outcomes of a Cross-Site Cognitive-Behavioral and Neuromuscular Integrative Training Intervention for Juvenile Fibromyalgia. Arthritis Care Res. 2017, 69, 413–420. [Google Scholar] [CrossRef]
- Hechler, T.; Wager, J.; Zernikow, B. Chronic pain treatment in children and adolescents: Less is good, more is sometimes better. BMC Pediatr. 2014, 14, 262. [Google Scholar] [CrossRef] [PubMed]
- Carter, B.; Kronenberger, W.; Cruce-Spurling, S.; Threlkeld, B.; Brady, C.; Jones, L.; Mizell, D. Factors associated with dropout versus completion of a manualized treatment for pediatric chronic pain. Clin. Pract. Pediatr. Psychol. 2015, 3, 327–339. [Google Scholar] [CrossRef]
- Cunningham, N.R.; Jagpal, A.; Tran, S.T.; Kashikar-Zuck, S.; Goldschneider, K.R.; Coghill, R.C.; Lynch-Jordan, A.M. Anxiety adversely impacts response to cognitive behavioral therapy in children with chronic pain. J. Pediatr. 2016, 171, 227–233. [Google Scholar] [CrossRef]
- Kashikar-Zuck, S.; Ting, T.V.; Arnold, L.M.; Bean, J.; Powers, S.W.; Graham, T.B.; Passo, M.H.; Schikler, K.N.; Hashkes, P.J.; Spalding, S. Cognitive behavioral therapy for the treatment of juvenile fibromyalgia: A multisite, single-blind, randomized, controlled clinical trial. Arthritis Rheum. 2012, 64, 297–305. [Google Scholar] [CrossRef]
- Lee, S.; Dick, B.D.; Jordan, A.; McMurtry, C.M. A Parent-Targeted Group Intervention for Pediatric Pain Delivered In-Person or Virtually: Feasibility, Acceptability, and Effectiveness. Clin. J. Pain 2023, 39, 127–137. [Google Scholar] [CrossRef]
- Ali, A.; Weiss, T.R.; Dutton, A.; McKee, D.; Jones, K.D.; Kashikar-Zuck, S.; Silverman, W.K.; Shapiro, E.D. Mindfulness-Based Stress Reduction for Adolescents with Functional Somatic Syndromes: A Pilot Cohort Study. J. Pediatr. 2017, 183, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Chadi, N.; McMahon, A.; Vadnais, M.; Malboeuf-Hurtubise, C.; Djemli, A.; Dobkin, P.L.; Lacroix, J.; Luu, T.M.; Haley, N. Mindfulness-based intervention for female adolescents with chronic pain: A pilot randomized trial. J. Can. Acad. Child Adolesc. Psychiatry 2016, 25, 159. [Google Scholar] [PubMed]
- Hesse, T.; Holmes, L.G.; Kennedy-Overfelt, V.; Kerr, L.M.; Giles, L.L. Mindfulness-based intervention for adolescents with recurrent headaches: A pilot feasibility study. Evid.-Based Complement. Altern. Med. 2015, 2015, 508958. [Google Scholar] [CrossRef] [PubMed]
- Jastrowski Mano, K.E.; Salamon, K.S.; Hainsworth, K.R.; Anderson Khan, K.J.; Ladwig, R.J.; Davies, W.; Weisman, S.J. A randomized, controlled pilot study of mindfulness-based stress reduction for pediatric chronic pain. Altern. Ther. Health Med. 2013, 19, 8–14. [Google Scholar] [PubMed]
- Lovas, D.A.; Pajer, K.; Chorney, J.M.; Vo, D.X.; Howlett, M.; Doyle, A.; Huber, A. Mindfulness for adolescent chronic pain: A pilot feasibility study. J. Child Adolesc. Ment. Health 2017, 29, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Bakshi, N.; Cooley, A.; Ross, D.; Hawkins, L.; Sullivan, M.; Astles, R.; Sinha, C.; Katoch, D.; Peddineni, M.; Gee, B.E. A pilot study of the acceptability, feasibility and safety of yoga for chronic pain in sickle cell disease. Complement. Ther. Med. 2021, 59, 102722. [Google Scholar] [CrossRef] [PubMed]
- Gmuca, S.; Weiss, P.F.; McGill, M.; Xiao, R.; Ward, M.; Nelson, M.; Sherry, D.D.; Cronholm, P.F.; Gerber, J.S.; Palermo, T.M. The Feasibility and Acceptability of Resilience Coaching for Adolescent Chronic Musculoskeletal Pain: A Single-Arm Pilot Trial. Children 2022, 9, 1432. [Google Scholar] [CrossRef] [PubMed]
- Bicego, A.; Monseur, J.; Rousseaux, F.; Faymonville, M.-E.; Malaise, N.; Salamun, I.; Collinet, A.; Nyssen, A.-S.; Vanhaudenhuyse, A. Drop-out from chronic pain treatment programmes: Is randomization justified in biopsychosocial approaches? J. Rehabil. Med. 2021, 53, jrm00185. [Google Scholar] [CrossRef]
- Fidelix, Y.L.; de Farias Júnior, J.C.; Lofrano-Prado, M.C.; Guerra, R.L.F.; Cardel, M.; de Prado, W.L. Multidisciplinary intervention in obese adolescents: Predictors of dropout. Einstein 2015, 13, 388–394. [Google Scholar] [CrossRef][Green Version]
- Zeller, M.; Kirk, S.; Claytor, R.; Khoury, P.; Grieme, J.; Santangelo, M.; Daniels, S. Predictors of attrition from a pediatric weight management program. J. Pediatr. 2004, 144, 466–470. [Google Scholar] [CrossRef]
- Schuiteman, S.; Chua, K.-P.; Plegue, M.A.; Ilyas, O.; Chang, T. Self-Management of Health Care Among Youth: Implications for Policies on Transitions of Care. J. Adolesc. Health 2020, 66, 616–622. [Google Scholar] [CrossRef] [PubMed]
- Carosella, A.M.; Lackner, J.M.; Feuerstein, M. Factors associated with early discharge from a multidisciplinary work rehabilitation program for chronic low back pain. Pain 1994, 57, 69–76. [Google Scholar] [CrossRef]
- Coughlan, G.; Ridout, K.; Williams, A.d.C.; Richardson, P. Attrition from a pain management programme. Br. J. Clin. Psychol. 1995, 34, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Hampl, S.; Demeule, M.; Eneli, I.; Frank, M.; Hawkins, M.J.; Kirk, S.; Morris, P.; Sallinen, B.J.; Santos, M.; Ward, W.L.; et al. Parent perspectives on attrition from tertiary care pediatric weight management programs. Clin. Pediatr. 2013, 52, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Sallinen, B.J.; Schaffer, S.; Woolford, S.J. In their own words: Learning from families attending a multidisciplinary pediatric weight management program at the YMCA. Child. Obes. 2013, 9, 2–207. [Google Scholar] [CrossRef] [PubMed]
- Simons, L.E.; Logan, D.E.; Chastain, L.; Cerullo, M. Engagement in multidisciplinary interventions for pediatric chronic pain: Parental expectations, barriers, and child outcomes. Clin. J. Pain 2010, 26, 291–299. [Google Scholar] [CrossRef] [PubMed]
- Oosterhaven, J.; Wittink, H.; Dekker, J.; Kruitwagen, C.; Devillé, W. Pain catastrophizing predicts dropout of patients from an interdisciplinary chronic pain management programme: A prospective cohort study. J. Rehabil. Med. 2019, 51, 761–769. [Google Scholar] [CrossRef]
- Hardman, R.; Lawn, S.; Tsourtos, G. Pain self-management: Easier said than done? Factors associated with early dropout from pain self-management in a rural primary care population. Pain Med. 2018, 20, 267–277. [Google Scholar] [CrossRef]
- Biller, N.; Arnstein, P.; Caudill, M.A.; Federman, C.W.; Guberman, C. Predicting completion of a cognitive-behavioral pain management program by initial measures of a chronic pain patient’s readiness for change. Clin. J. Pain 2000, 16, 352–359. [Google Scholar] [CrossRef]
- Berry, D.C.; Rhodes, E.T.; Hampl, S.; Young, C.B.; Cohen, G.; Eneli, I.; Fleischman, A.; Ip, E.; Sweeney, B.; Houle, T.T.; et al. Stay in treatment: Predicting dropout from pediatric weight management study protocol. Contemp. Clin. Trials Commun. 2021, 22, 100799. [Google Scholar] [CrossRef]
- Benjamin, J.Z.; Harbeck-Weber, C.; Sim, L. Pain is a family matter: Quality of life in mothers and fathers of youth with chronic pain. Child Care Health Dev. 2019, 45, 440–447. [Google Scholar] [CrossRef]
- Jastrowski Mano, K.E.; Khan, K.A.; Ladwig, R.J.; Weisman, S.J. The Impact of Pediatric Chronic Pain on Parents’ Health-Related Quality of Life and Family Functioning: Reliability and Validity of the PedsQL 4.0 Family Impact Module. J. Pediatr. Psychol. 2011, 36, 517–527. [Google Scholar] [CrossRef]
- Ngo, D.; Palmer, G.M.; Gorrie, A.; Kenmuir, T.; Crawford, M.; Jaaniste, T. Caregiver burden associated with pediatric chronic pain: A retrospective study using the Paediatric Electronic Persistent Pain Outcomes Collaboration (PaedePPOC) database. Clin. J. Pain 2023, in press. [CrossRef]
- Chong, J.L.; Meltzer, K.J.; Robinson, R.C.; Hynan, L.S.; Zafereo, J.A.; Noe, C.E.; Jarrett, R.B. Predictors of attrition in an interdisciplinary pain management program. Rehabil. Psychol. 2023, 68, 65–76. [Google Scholar] [CrossRef]
- Sørensen, K.; Pelikan, J.M.; Röthlin, F.; Ganahl, K.; Slonska, Z.; Doyle, G.; Fullam, J.; Kondilis, B.; Agrafiotis, D.; Uiters, E. Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Health Literacy Australia 2006. Available online: www.ausstats.abs.gov.au/ausstats/subscriber.nsf/0/73ED158C6B14BB5ECA2574720011AB83/$File/42330_2006.pdf (accessed on 17 January 2024).
- Morrison, A.K.; Glick, A.; Yin, H.S. Health literacy: Implications for child health. Pediatr. Rev. 2019, 40, 263–277. [Google Scholar] [CrossRef]
- Yin, H.S.; Johnson, M.; Mendelsohn, A.L.; Abrams, M.A.; Sanders, L.M.; Dreyer, B.P. The health literacy of parents in the United States: A nationally representative study. Pediatrics 2009, 124, S289–S298. [Google Scholar] [CrossRef]
- Morrison, A.K.; Chanmugathas, R.; Schapira, M.M.; Gorelick, M.H.; Hoffmann, R.G.; Brousseau, D.C. Caregiver low health literacy and nonurgent use of the pediatric emergency department for febrile illness. Acad. Pediatr. 2014, 14, 505–509. [Google Scholar] [CrossRef]
- Morrison, A.K.; Schapira, M.M.; Gorelick, M.H.; Hoffmann, R.G.; Brousseau, D.C. Low caregiver health literacy is associated with higher pediatric emergency department use and nonurgent visits. Acad. Pediatr. 2014, 14, 309–314. [Google Scholar] [CrossRef]
- Donnelly, T.J.; Palermo, T.M.; Newton-John, T.R.O. Parent cognitive, behavioural, and affective factors and their relation to child pain and functioning in pediatric chronic pain: A systematic review and meta-analysis. Pain 2020, 161, 1401–1419. [Google Scholar] [CrossRef]
- Caes, L.; Vervoort, T.; Eccleston, C.; Vandenhende, M.; Goubert, L. Parental catastrophizing about child’s pain and its relationship with activity restriction: The mediating role of parental distress. Pain 2011, 152, 212–222. [Google Scholar] [CrossRef]
- Barlow, S.E.; Ohlemeyer, C.L. Parent reasons for nonreturn to a pediatric weight management program. Clin. Pediatr. 2006, 45, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Morrissey-Kane, E.; Prinz, R.J. Engagement in child and adolescent treatment: The role of parental cognitions and attributions. Clin. Child Fam. Psychol. Rev. 1999, 2, 183–198. [Google Scholar] [CrossRef] [PubMed]
- Skelton, J.A.; Martin, S.; Irby, M.B. Satisfaction and attrition in paediatric weight management: Satisfaction in weight management. Clin. Obes. 2016, 6, 143–153. [Google Scholar] [CrossRef]
- Baier, A.L.; Kline, A.C.; Feeny, N.C. Therapeutic alliance as a mediator of change: A systematic review and evaluation of research. Clin. Psychol. Rev. 2020, 82, 101921. [Google Scholar] [CrossRef]
- Saatsi, S.; Hardy, G.E.; Cahill, J. Predictors of outcome and completion status in cognitive therapy for depression. Psychother. Res. 2007, 17, 185–195. [Google Scholar] [CrossRef]
- Samstag, L.W.; Batchelder, S.T.; Muran, J.C.; Safran, J.D.; Winston, A. Early identification of treatment failures in short-term psychotherapy. An assessment of therapeutic alliance and interpersonal behavior. J. Psychother. Pract. Res. 1998, 7, 126–143. [Google Scholar]
- Hall, A.M.; Ferreira, P.H.; Maher, C.G.; Latimer, J.; Ferreira, M.L. The influence of the therapist-patient relationship on treatment outcome in physical rehabilitation: A systematic review. Phys. Ther. 2010, 90, 1099–1110. [Google Scholar] [CrossRef]
- Taccolini Manzoni, A.C.; Bastos de Oliveira, N.T.; Nunes Cabral, C.M.; Aquaroni Ricci, N. The role of the therapeutic alliance on pain relief in musculoskeletal rehabilitation: A systematic review. Physiother. Theory Pract. 2018, 34, 901–915. [Google Scholar] [CrossRef]
- Dima, A.; Lewith, G.T.; Little, P.; Moss-Morris, R.; Foster, N.E.; Hankins, M.; Surtees, G.; Bishop, F.L. Patients’ treatment beliefs in low back pain: Development and validation of a questionnaire in primary care. Pain 2015, 156, 1489–1500. [Google Scholar] [CrossRef]
- Allegretti, A.; Borkan, J.; Reis, S.; Griffiths, F. Paired interviews of shared experiences around chronic low back pain: Classic mismatch between patients and their doctors. Fam. Pract. 2010, 27, 676–683. [Google Scholar] [CrossRef] [PubMed]
- Givler, A.; Bhatt, H.; Maani-Fogelman, P.A. The Importance of Cultural Competence in Pain and Palliative Care; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Nair, L.; Adetayo, O.A. Cultural competence and ethnic diversity in healthcare. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2219. [Google Scholar] [CrossRef]
- Purnell, L.D.; Fenkl, E.A. The Purnell Model for Cultural Competence; Springer International Publishing: Cham, Switzerland, 2019; pp. 7–18. [Google Scholar]
- Cochran, D.; Saleem, S.; Khowaja-Punjwani, S.; Lantos, J.D. Cross-Cultural Differences in Communication About a Dying Child. Pediatrics 2017, 140, e20170690. [Google Scholar] [CrossRef]
- Lekas, H.-M.; Pahl, K.; Fuller Lewis, C. Rethinking Cultural Competence: Shifting to Cultural Humility. Health Serv. Insights 2020, 13, 1178632920970580. [Google Scholar] [CrossRef]
- Anderson, K.N.; Bautista, C.L.; Hope, D.A. Therapeutic alliance, cultural competence and minority status in premature termination of psychotherapy. Am. J. Orthopsychiatry 2019, 89, 104. [Google Scholar] [CrossRef] [PubMed]
- Austin, A.; Wagner, E.F. Treatment Attrition Among Racial and Ethnic Minority Youth. J. Soc. Work Pract. Addict. 2010, 10, 63–80. [Google Scholar] [CrossRef]
- Jaaniste, T.; Hayes, B.; Baeyer, C. Providing Children with Information about Forthcoming Medical Procedures: A Review and Synthesis. Clin. Psychol. Sci. Pract. 2007, 14, 124–143. [Google Scholar] [CrossRef]
- Robins, H.; Perron, V.; Heathcote, L.C.; Simons, L.E. Pain Neuroscience Education: State of the Art and Application in Pediatrics. Children 2016, 3, 43. [Google Scholar] [CrossRef]
- Bandura, A. Human agency in social cognitive theory. Am. Psychol. 1989, 44, 1175–1184. [Google Scholar] [CrossRef]
- Guite, J.W.; Kim, S.; Chen, C.P.; Sherker, J.L.; Sherry, D.D.; Rose, J.B.; Hwang, W.T. Pain beliefs and readiness to change among adolescents with chronic musculoskeletal pain and their parents before an initial pain clinic evaluation. Clin. J. Pain 2014, 30, 27–35. [Google Scholar] [CrossRef]
- Csillik, A. Positive Motivational Interviewing: Activating Clients’ Strengths and Intrinsic Motivation to Change. J. Contemp. Psychother. 2015, 45, 119–128. [Google Scholar] [CrossRef]
- Glombiewski, J.A.; Hartwich-Tersek, J.; Rief, W. Attrition in cognitive-behavioral treatment of chronic back pain. Clin. J. Pain 2010, 26, 593–601. [Google Scholar] [CrossRef]
- Knox, S.; Miller, C.; Twidwell, R.E.; Knowlton, G. Client perspectives on psychotherapy failure. Psychother. Res. 2023, 33, 298–315. [Google Scholar] [CrossRef] [PubMed]
- Zunhammer, M.; Ploner, M.; Engelbrecht, C.; Bock, J.; Kessner, S.S.; Bingel, U. The effects of treatment failure generalize across different routes of drug administration. Sci. Transl. Med. 2017, 9, eaal2999. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, J.Z.; Harbeck-Weber, C.; Ale, C.; Sim, L. Becoming flexible: Increase in parent psychological flexibility uniquely predicts better well-being following participation in a pediatric interdisciplinary pain rehabilitation program. J. Context. Behav. Sci. 2020, 15, 181–188. [Google Scholar] [CrossRef]
- Cousins, L.A.; Kalapurakkel, S.; Cohen, L.L.; Simons, L.E. Topical Review: Resilience Resources and Mechanisms in Pediatric Chronic Pain. J. Pediatr. Psychol. 2015, 40, 840–845. [Google Scholar] [CrossRef] [PubMed]
- Wallace, D.P.; Woodford, B.; Connelly, M. Promoting psychological flexibility in parents of adolescents with chronic pain: Pilot study of an 8-week group intervention. Clin. Pract. Pediatr. Psychol. 2016, 4, 405–416. [Google Scholar] [CrossRef]
- Baltag, V.; Takeuchi, Y.; Guthold, R.; Ambresin, A.E. Assessing and Supporting Adolescents’ Capacity for Autonomous Decision-Making in Health-Care Settings: New Guidance From the World Health Organization. J. Adolesc. Health 2022, 71, 10–13. [Google Scholar] [CrossRef]
- Champion, D.; Bui, M.; Bott, A.; Donnelly, T.; Goh, S.; Chapman, C.; Lemberg, D.; Jaaniste, T.; Hopper, J. Familial and Genetic Influences on the Common Pediatric Primary Pain Disorders: A Twin Family Study. Children 2021, 8, 89. [Google Scholar] [CrossRef]
- Dario, A.B.; Kamper, S.J.; O’Keeffe, M.; Zadro, J.; Lee, H.; Wolfenden, L.; Williams, C.M. Family history of pain and risk of musculoskeletal pain in children and adolescents: A systematic review and meta-analysis. Pain 2019, 160, 2430–2439. [Google Scholar] [CrossRef]
- Danieles, P.K.; Ybarra, M.; Van Hulst, A.; Barnett, T.A.; Mathieu, M.-È.; Kakinami, L.; Drouin, O.; Bigras, J.-L.; Henderson, M. Determinants of attrition in a pediatric healthy lifestyle intervention: The CIRCUIT program experience. Obes. Res. Clin. Pract. 2021, 15, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Boppana, S.S.; Miller, R.; Wrona, A.; Tumin, D.; Wrona, S.; Smith, T.P.; Bhalla, T.; Kim, S.S.; Tobias, J.D. Barriers to Outpatient Pediatric Chronic Pain Clinic Participation Among Referred Patients. Clin. Pediatr. 2020, 59, 859–864. [Google Scholar] [CrossRef] [PubMed]
- Biele, G.; Gustavson, K.; Czajkowski, N.O.; Nilsen, R.M.; Reichborn-Kjennerud, T.; Magnus, P.M.; Stoltenberg, C.; Aase, H. Bias from self selection and loss to follow-up in prospective cohort studies. Eur. J. Epidemiol. 2019, 34, 927–938. [Google Scholar] [CrossRef]
- Elston, D.M. Participation bias, self-selection bias, and response bias. J. Am. Acad. Dermatol. 2021. Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Abdelazeem, B.; Abbas, K.S.; Amin, M.A.; El-Shahat, N.A.; Malik, B.; Kalantary, A.; Eltobgy, M. The effectiveness of incentives for research participation: A systematic review and meta-analysis of randomized controlled trials. PLoS ONE 2022, 17, e0267534. [Google Scholar] [CrossRef]
- Hsieh, G.; Kocielnik, R. You get who you pay for. In Proceedings of the 19th ACM Conference on Computer-Supported Cooperative Work & Social Computing, San Francisco, CA, USA, 27 February–2 March 2016; pp. 823–835. [Google Scholar]
- Fisher, E.; Law, E.; Dudeney, J.; Eccleston, C.; Palermo, T.M. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst. Rev. 2019, 4, CD011118. [Google Scholar] [CrossRef]
- Jiang, L.; Yang, J.; Huang, H.; Johnson, A.; Dill, E.J.; Beals, J.; Manson, S.M.; Roubideaux, Y. Derivation and evaluation of a risk-scoring tool to predict participant attrition in a lifestyle intervention project. Prev. Sci. 2016, 17, 461–471. [Google Scholar] [CrossRef]
- Guy, R.; Hocking, J.; Wand, H.; Stott, S.; Ali, H.; Kaldor, J. How effective are short message service reminders at increasing clinic attendance? A meta-analysis and systematic review. Health Serv. Res. 2012, 47, 614–632. [Google Scholar] [CrossRef]
- Robotham, D.; Satkunanathan, S.; Reynolds, J.; Stahl, D.; Wykes, T. Using digital notifications to improve attendance in clinic: Systematic review and meta-analysis. BMJ Open 2016, 6, e012116. [Google Scholar] [CrossRef]
- Frye, W.S.; Cucchiaro, G.; Nguyen, A.T.H.; Householder, K.; Kuhn, B. Preappointment Surveys and Reminder Calls to Improve Show Rate. Am. J. Manag. Care 2022, 28, e296–e300. [Google Scholar]
- Guite, J.W.; Logan, D.E.; Simons, L.E.; Blood, E.A.; Kerns, R.D. Readiness to change in pediatric chronic pain: Initial validation of adolescent and parent versions of the Pain Stages of Change Questionnaire. Pain 2011, 152, 2301–2311. [Google Scholar] [CrossRef] [PubMed]
- Katz, L.; Patterson, L.; Zacharias, R. Evaluation of an interdisciplinary chronic pain program and predictors of readiness for change. Can. J. Pain 2019, 3, 70–78. [Google Scholar] [CrossRef] [PubMed]
| First Author Year Country Study Type | Sample n | Age, Years (% Females [F]) | Chronic Pain Conditions | Intervention | Delivery | Intervention Duration | Attrition % of n * | Definition of Attrition and/or Non-Completion Used |
| Interdisciplinary with Physical Therapy [PT] component | ||||||||
| Hilyard et al., 2020 [24] Australia Pilot | (i) 6 families (ii) 5 families | 12–17 (91% F) | Chronic pain | (i) Hybrid (F2F and VC) ped. I-D pain program (clin. psychol., PT and OT) (ii) F2F sessions (standard care) | (i) Group F2F and VC, and Indiv. VC [Hybrid] (ii) Ind. F2F only [SC] | 7 weeks with 14.5 h total 11 h group; 3.5 h Indiv. | (i) 17% withdrew before starting drug trial (ii) 17% withdrew before starting SC 1/5, 20% loss to FU/declined questionnaires | Lost to FU OR declined questionnaires after starting intervention |
| Ocay et al., 2023 [25] Canada Cohort | 414 | 8–18 (83% F) | Chronic pain | Personalized I-D treatment (pharm., PT, psychol., nursing, SW and interventional) | Indiv. F2F | Variable (not specified) | 7.9% overall (i) loss to FU 3.1%; (ii) dropout 4.8% | Lost to FU OR dropout due to non-compliance with planned treatment. |
| Shear et al., 2022 [26] USA RCT | 68 | M = 14.2 (81% F) | Chronic pain | (i) I-D graded exposure treatment (ii) M-D pain management Joint delivery psychol. and PT | Mixture: F2F, VC and Hybrid. | 12 × 1 h (twice weekly) 6 weeks 12 h | 13% (3/9 withdrew related to COVID-19 reasons) | Withdrew from treatment before completion |
| Tran et al., 2017 [27] USA Pilot | 30 | 12–18 (100% F) | Juvenile fibromyalgia | CBT/exercise. Joint psychol. postdoctoral fellow/ped. pain psychol. and EP/PT | Group F2F | 2 × 1.5 h 8 weeks 24 h | Dropouts 20% | Dropout after starting program |
| Interdisciplinary without Physical Therapy component | ||||||||
| Hechler et al., 2011 [14] Germany Cohort | 275 | 4–18 (56% F) | Chronic Pain | Multimodal treatment with pharm. and psychol. components | Indiv. F2F | Variable | Dropouts 18%, 12%, 16% at 3, 6, 12 months Non-attendants (non-completers) 8%, 24%, 32% at 3, 6, 12 months | Study dropouts: withdrew entirely from study Non-attendants: discontinued multimodal treatment (non-completers) |
| Hechler et al., 2014 [28], Germany Cohort | 1520 | 1–19 (58% F) | Chronic pain | I-D outpatient medical, and psychological treatment recommendations | Indiv. F2F | Variable | 35% did not attend the required return visit | No return visit to treatment center within 12 months |
| Cognitive Behavioral Therapy [CBT] | ||||||||
| Carter et al., 2015 [29], USA Cohort | 62 | M = 14.6, SD = 1.6 (92.8% F) | Chronic painful and/or fatiguing conditions | Manualized psychosocial treatment: CBT, behavioral family systems therapy and interpersonal psychotherapy. Postdoctoral fellows, predoctoral interns, and ped. psychol. doctoral students | Indiv. F2F | 12 × 1 h sessions 12 weeks 12 h | Dropouts 32% | Completers attended 12/12 sessions |
| Cunningham et al., 2016 [30], USA Cohort | 175 | 8–18 (78% F) | Chronic pain and anxiety | Pain-focused CBT by clin. psychol. (specialized in ped. chronic pain or in advanced training) | Indiv. F2F | Variable (not specified) | Dropouts 44/84, 52% (52% non-starters) | Dropped out after intervention commenced |
| Kashikar-Zuck et al., 2012 [31], USA RCT | 114 | 11–18 (92% F) | Juvenile fibromyalgia | CBT. 5 postdoctoral ped. psychol. and CBT-trained therapists | Indiv. F2F | 8 × 45 min sessions 8 weeks 6 h | Dropouts 12/100, 12% (1.8% Non-starters) | Non-completion of treatment and follow-up |
| Lee et al., 2023 [32], USA Canada Pilot | 72 | Parents of 8–17 year olds (74% F) | Chronic Pain | Parent-targeted group CBT led by 2 facilitators (at least one clin. psychol. or clin. psychol. doctoral trainee) | Parents’ group F2F or VC | 5 × 2 h 5 weeks 10 h (USD 5 gift card per questionnaire $15 for 3—pre, post, f/u) | 5.6% overall F2F 1/27, 3.7% | Those who attended < 2 of the 5 sessions |
| Mindfulness-Based Interventions [MBI] | ||||||||
| Ali et al., 2017 [33], USA Cohort | 18 | 10–18 (73% F) | Functional somatic syndromes | Mindfulness-Based Stress Reduction (MBSR) led by an experienced instructor | Group F2F | 8 × 1.5 h, 8 weeks (plus 4 h retreat) 16 h ($200 USD for participation) | Dropouts 7% | Withdrew before completing all sessions |
| Chadi et al., 2016 [34], Canada Randomized pilot RCT | 20 | 13–17 (100% F) | Chronic pain | MBI by two psychiatry residents | Group F2F | 8 × 1.5 h sessions 8 weeks 12 h | Dropouts 5% (3 withdrew before randomization) | Non-completion of all 8 sessions |
| Hesse et al., 2015 [35], USA Pilot | 20 | 11–16 (100% F) | Recurrent headaches | MBI by three MBSR trained instructors; clin. psychol. and psychiatrist present during all sessions | Group F2F | 8 × 2 h evening sessions 8 weeks 16 h | Dropouts 25% | Of those enrolled, % that dropped out of intervention. |
| Jastrowski Mano et al., 2013 [36] USA Pilot | 6 | 12–17 (75% F) | Chronic pain | MBSR delivered by experienced MBSR practitioner | Group F2F | 6 × 1.5 h sessions 6 weeks 9 h | Psycho-education: lost to FU 2/2, 100% MBSR: lost to FU 2/4, 50% | Lost to FU at 4 weeks |
| Lovas et al., 2017 [37] Canada Pilot | 18 | 14–17 (86% F) | Chronic pain | MBI taught by a child and adolescent psychiatrist with formal training in MBSR and MBCT | Group F2F | 8 × 1.5 h sessions 8 weeks 12 h | Dropouts 0% of the 7 who commenced (61% Non-starters) | Completion of intervention by those who started |
| Ruskin et al., 2017 [6], Canada Pilot | 21 | 12–18 (95% F) | Chronic pain | MBI for adolescents led by two facilitators completing MBI training | Group F2F | 8 × 2 h (after school) 8 weeks 16 h | Non-completers 9.5% (0% Non-starters) | “Treatment completers” completed at least 6/8 sessions |
| Suc et al., 2022 [5], France Pilot | 27 | 12–17 (67% F) | Chronic pain | MBI led by at least two experienced MBSR instructors: focus on building skills and incorporating meditation, exercises, and activities adapted for teenagers | Group F2F | 8 × 1.5 h (after school) 8 weeks 12 h | Dropouts 11% | “Treatment completers” attended at least 6/8 sessions. |
| Other | ||||||||
| Bakshi et al., 2021 [38], USA Pilot | Part B: 9 | 15–18 (53% F) | Sickle-cell disease with chronic pain | Instructor-led yoga sessions | Group F2F | 8 × 1 h 8 weeks 8 h (USD 25 for surveys completed, USD 25 for interviews, USD 1/diary entry, USD 25/yoga session) | 89% did not complete any sessions One partial completer 11% 3/8 sessions | Not attending any of the 8 sessions despite enrollment |
| Gmuca et al., 2022 [39], USA Pilot | 27 | 12–17 (82% F) | Musculo-skeletal chronic illness | Promoting Resilience in Stress Management (PRISM) coaching. Delivered by trained, bachelor-level coaches | Indiv Choice of F2F or VC telephone. | 4 × 30–50 min over 3 months (1–2 weeks apart) | Dropouts 15% | Non-completion of each of the 4 required sessions by enrolled participants. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tiong, K.; Palmer, G.M.; Jaaniste, T. Attrition from Face-to-Face Pediatric Outpatient Chronic Pain Interventions: A Narrative Review and Theoretical Model. Children 2024, 11, 126. https://doi.org/10.3390/children11010126
Tiong K, Palmer GM, Jaaniste T. Attrition from Face-to-Face Pediatric Outpatient Chronic Pain Interventions: A Narrative Review and Theoretical Model. Children. 2024; 11(1):126. https://doi.org/10.3390/children11010126
Chicago/Turabian StyleTiong, Kristen, Greta M. Palmer, and Tiina Jaaniste. 2024. "Attrition from Face-to-Face Pediatric Outpatient Chronic Pain Interventions: A Narrative Review and Theoretical Model" Children 11, no. 1: 126. https://doi.org/10.3390/children11010126
APA StyleTiong, K., Palmer, G. M., & Jaaniste, T. (2024). Attrition from Face-to-Face Pediatric Outpatient Chronic Pain Interventions: A Narrative Review and Theoretical Model. Children, 11(1), 126. https://doi.org/10.3390/children11010126






