Abstract
Language disorders are characterized by impairments in verbal expression/understanding, including difficulties with one or more language components. The Virtual Reality Rehabilitation System (VRRS) is a bioelectromedical device equipped with exercise sections aimed at improving cognitive and language deficits. It also increases patient motivation and engagement. The aim of our study was to test the feasibility and efficacy of VRRS intervention to improve speech therapy treatment for children with speech disorders. Thirty-two patients were enrolled in this study and randomly assigned to the experimental (EG) or control group (CG). The CG underwent conventional speech therapy, while EG underwent VRRS-implemented speech therapy. Both groups were evaluated before (T0) and after (T1) the intervention using the Language Assessment Test. The results showed improvements in both groups. However, the EG group showed greater improvement in various areas, including comprehension of total words, repetition, naming of body parts, naming of everyday objects, total naming, morphosyntactic accuracy, sentence construction, average length of utterance, and spontaneous word production. This study demonstrated that VRRS can be a valuable tool for implementing effective speech rehabilitation. Further studies are needed, as the use of VRRS is still in its early stages, requiring larger samples sizes and long-term follow-up.
1. Introduction
Developmental language disorder (DLD) is a neurodevelopmental condition characterized by persistent difficulty in the acquisition and use of language in all its modalities (spoken, written, sign language, or other). Children may present deficits in both comprehension and production, with a reduced number of words known and a persistent difficulty in their correct usage, limited ability to connect sentences to explain or describe a topic or series of events, or difficulty sustaining a conversation [1].
According to the literature, DLD is one of the most common disorders, and affects about 3–7% of preschoolers [2,3,4]. Language abilities in these children appear significantly below what is expected from subjects of the same age: children’s expressive language should be 50% intelligible by age 36 months and about 75% intelligible by age 48 months [5]. The onset of symptoms occurs in the early developmental period: sufficient receptive language seems to be positively correlated with better expressive language outcomes, such as toddlerhood vocabulary size [6]. Conversely, about 15–16% of toddlers with delays in both expression and comprehension of language presented a high risk of developing a persistent DLD [7]. DLD is described as a heterogeneous disorder because it may impair different aspects of language; often phonologic development is involved, and semantics or syntax difficulties are usually present [8]. Moreover, it is often associated with other neurodevelopmental disorders such as attention deficit hyperactivity disorder, specific learning disorder, autism spectrum disorder, and coordination development disorder [9,10,11]. These dysfunctions can lead to long-term disadvantages for the child, such as isolation, regression, and poor school performance [12]. Compared to other students, children and adolescents with a previous language disorder had a higher risk of reading or writing difficulties and are three times more likely to experience clinical levels of anxiety [13,14]. Overall, the outcome of an untreated DLD can result in functional limitations in effective communication, impaired peer interaction, reduction in academic achievement, and poor job retention [15]. To prevent comorbidity and improve outcome, specialist intervention is essential [12,16]. The best available evidence confirms the positive effect of speech and language therapy for children with DLD [17,18]. Speech therapy often involves exercises that can be boring, so it is necessary to motivate children to practice them through new techniques and innovative tools [19].
Over the past decade, virtual reality (VR) has played an increasing role in the treatment of several neurological disorders [20,21]. VR is a new methodology that involves the use of computer technologies that create various artificial environments (in 2D or 3D) similar to real ones that the patient will have to interact with through sight, sound, and touch [22,23,24]. The central nervous system, thanks to virtual scenarios, receives more sensory feedback (auditory, visual, tactile), which can create changes in synaptic plasticity and reinforce learning [25]. In this context, among the various tools involved in using virtual reality, the Virtual Reality Rehabilitation System (VRRS) developed by Khymeia (Padua, Italy) is a promising tool for rehabilitation [22,26,27]. It is a medical device with cognitive and linguistic modules that aim to improve the cognitive and linguistic abilities of patients with neurological disorders [22]. The application of VRRS could be beneficial for children with DLD as it increases motivation, reduces anxiety, and causes less attractive activities to be perceived as play. These latter elements are prerequisites for more effective recovery [28]. In this field, few studies have reported the usefulness of VR in communication disorders, mainly using it to mediate caregiver–child interaction [29] or to improve communication ability in patients with autism spectrum disorder. However, several clinical trials have been published that have shown the benefits of virtual reality in communication disorders, with results such as improvements in fluency disorders, pragmatic abilities, and interaction areas [30]. To our knowledge, this is the first prospective pilot study to verify the feasibility and clinical effectiveness of speech therapy implemented by the VRRS device in children with a developmental language disorder.
The purpose of this study is to test the feasibility and clinical effectiveness of speech therapy with the VRRS device in children with speech disorders, comparing the results with conventional treatment.
2. Materials and Methods
2.1. Population and Study Design
This pilot randomized control trial was developed in order to evaluate the feasibility and compare the efficacy of speech intervention implemented with a virtual reality system with treatment as usual (TAU) delivered to children affected by DLD. This study has been reviewed and approved by the Local Ethics Committee (approval number n. 15/2019) and completed in accordance with the CONSORT guidelines [31] (Figure 1). Written informed consent was obtained from both parents, or from a legal representative of the patient. Children were recruited at the IRCCS Bonino Pulejo Neurolesi Center in Messina, Italy, between February 2021 and December 2022. Recruited participants had a primary diagnosis of DLD as defined by the DSM-5 which was not attributable to sensory impairment or another medical or neurological condition. Other eligibility requirements were: age between 36 months and 84 months and a written informed consent provided by parents or guardians. Patients were excluded if they were receiving other behavioral therapy or medical treatments, and if they were diagnosed with other significant medical conditions such as epilepsy, visual and auditory sensory deficits, traumatic brain injury, or other significant genetic disorders. Patients included were randomly assigned to either the experimental group (EG) or the control group (CG) using a computer-generated list of random numbers.
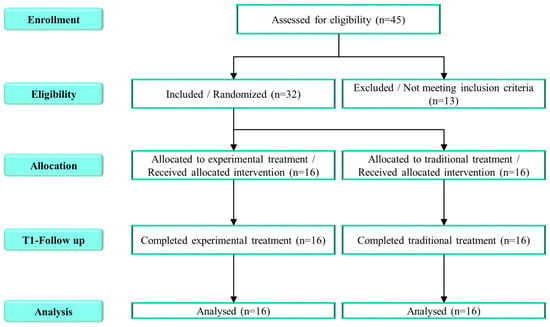
Figure 1.
The CONSORT flowchart with detailed information on participants in the study.
2.2. Neuropsychological Assessment
All patients underwent a complete and exhaustive assessment performed by expert clinicians. Diagnoses were made by a medical team comprised of pediatric neuropsychiatrists, psychologists, and speech therapists based on direct observation, a play session, a medical examination, a neuropsychological evaluation, and an interview with the parents. Children were assessed at baseline (T0) and at the end of the protocol (T1) with the Test of Language Assessment (TVL) [32] by an independent evaluator, blinded to treatment conditions. The TVL is an Italian standardized test that investigates language development in preschool children [33,34,35]. It is divided into four components: (1) receptive language, assessed through images representing body parts, common objects, colors, actions, objects, and spatiotemporal concepts; (2) sentence repetition ability, investigated by asking for repetition of 15 sentences of increasing length; (3) naming ability, examined by using pictures representing body parts and common objects and asking the child to name them; (4) spontaneous language production, assessed by asking the child to describe pictures representing actions, scenes, stories, and to narrate actions in sequence [36,37]. In addition, intellectual quotient (IQ) was assessed using a cognitive test (Leiter-3 [38], Wippsi-IV [39], Wisc-IV [40]). The tests administered were selected by child neuropsychiatrists based on the clinical characteristics of each patient.
2.3. Intervention
Each child participating in both groups received two 1-h sessions per week of treatment for a period of six months. The CG underwent conventional speech therapy, while the EG underwent speech therapy implemented by VRRS sessions. This virtual reality device is recognized as one of the most advanced, comprehensive, and clinically proven systems for rehabilitation [41,42]. It is a technological innovation tool to provide assistance with motor [43], cognitive, and linguistic performance [44,45]. VRRS allows the child to simulate daily activities in a non-immersive virtual environment, adapting task parameters according to the patient’s performance. This increases engagement and avoids boredom and frustration via a more sophisticated and holistic approach [42,46]. In our study, the speech therapy with the VRRS was planned by the speech therapist based on the neuropsychological assessment performed at T0. The tasks were the same for all children, but the difficulty and duration varied according to the needs and goals to be achieved. The exercises were 2D and the patient interacted with the scenarios through the touch screen. Table 1 shows the exercises proposed by speech therapists broken down by individual areas of focus.

Table 1.
Description of the main exercises used during session with VRRS and language domain involved in each activity.
2.4. Statistical Analysis
Data were analyzed using R version 4.2.3, considering a p < 0.05 as statistically significant. A nonparametric analysis was performed. A Wilcoxon signed-rank test was used to compare scores between baseline and follow-up.
3. Results
A total of 45 children with DLD were screened for eligibility. Thirty-two children (mean age ± SD: 4.8 ± 1.1 years; M:F = 4.3:1) met the inclusion criteria and were randomly assigned to either the experimental group (EG: n = 16) or the control group (CG: n = 16). A more detailed description of the two groups is given in Table 2.

Table 2.
Demographic data of the sample.
All patients involved in the study predominantly manifested DLD. Comorbid neurodevelopmental disorders were attention deficit hyperactivity disorder (n.6, 18.7%) and developmental coordination disorder (n.2, 6.3%).
The feasibility appears to be well supported, as all patients accepted the procedures, attended regularly, and actively participated in the therapy, indicating that the DLD children were able to tolerate the virtual reality and the protocol. The retention rate of patients completing six months of treatment was 100%. Speech therapy led to improvement in both groups. In the EG group there were greater improvements in: comprehension—total words (p = 0.011), naming body parts (p = 0.033), naming everyday objects (p = 0.011), total naming (p = 0.029), morphosyntactic accuracy (p = 0.012), sentence construction (p = 0.030), average utterance length (p = 0.013), and spontaneous word production (p = 0.031). Significant improvements were not registered in comprehension—total sentences, construction—style, and construction—spontaneous production for the control group. For more details, see Table 3.

Table 3.
Statistical comparisons of clinical scores between baseline (T0) and follow-up (T1), for both experimental and control groups.
4. Discussion
In our study, we compared traditional speech therapy treatment with a treatment aided by virtual technology by examining language at T0 and T1 through an assessment test of individual areas of language. The areas assessed were receptive language, sentence repetition ability, naming ability, and spontaneous language production. The treatment aimed to improve the same areas. Our study showed that speech therapy intervention with VRRS compared with conventional intervention made further improvements. In particular, an increase was observed in word comprehension, naming (of body parts, everyday objects, and totals), morphosyntactic accuracy, period construction, average utterance length, and spontaneous word production.
It was not possible to compare all the areas of language investigated through TVL, as in the literature studies were not found that implement virtual reality and evaluate the improvement of language in children in all the components of TVL. This shortage is likely attributable to the lack of high-tech rehabilitation tools in hospitals due to high costs, accessibility issues, and lack of highly trained therapists [47]. Current studies are uneven and mainly concern adults and autism spectrum disorders. Recent studies of children with autism spectrum syndrome [48,49,50,51,52,53] show that VR made improvements in naming consonants [48], vowels [48], words, and sentences [49]. These results are in agreement with those of our study. In addition, VR improved progress in pragmatic skills by improving communication skills and social interaction [50,51,52,53]. Many authors have examined speech therapy treatment with VR in adults. It has been shown [54,55] that the authentic, safe, and controlled environments provided by VR can be useful for the assessment and treatment of stuttering [54] and that naming difficulties have been reduced with spontaneous reading and voice tests [55]. Again, our results are in line with these studies in terms of improved naming [54,55]. VR has also been applied to speech disorders following brain injury. In aphasia studies, general improvements were found in all areas analyzed, except writing [45] and learning, showing these improvements 2.3 times faster than in patients treated with conventional therapy [56].
Virtual reality is applicable in many areas of rehabilitation [50,57]. Such a tool is conducive to the treatment of communication disorders, particularly language disorders in children, as it promotes enjoyment, increases perception of self-efficacy, and facilitates engagement [58,59]. These elements allow for a longer duration of speech intervention and greater adherence to treatment [60]. The rehabilitative activities conducted with virtual reality in our research project resulted in improved speech. Some studies attribute the improvement predominantly to the simulation of reality [61,62]. Our research group believes that improvement is also related to the variety of stimuli selected and individualized for each child, mediation by therapists, and the experience of VR as a highly motivating playful situation [28,63,64].
Children also improve language skills through social and experiential games to which, however, they are increasingly less exposed, such as outdoor activities with animals and exposure to different stimuli [65]. Virtual reality, unlike experiential activities, encourages exposure to more stimuli and motivating activities, such as farm exercise, that reduce learning time and break down logistical barriers [66]. Digital stimuli induce greater frustration tolerance because even error is experienced as a game, and this facilitates improvement through repetition and trial-and-error procedures [66,67]. This technique can be useful because it allows therapists to present in a real-world-like setting [68] safe, controllable, and repeatable modes of intervention that enhance the development of children’s social, cognitive, and language skills [48]. Communication also becomes crucial, not only in relation to verbalization but also to socialization [69]. Another advantage of technological treatment is the reduction of rehabilitation time [70,71].
Overall, these results are in line with several studies conducted on DLD using VR, although our study is the first to provide a detailed picture of all the components of language that can improve in children through a speech intervention associated with VR investigated with TVL.
5. Conclusions
In conclusion, this study demonstrates that VRRS can be a valuable innovative tool for implementing feasible and effective speech rehabilitation, as it allowed greater recovery of abilities in different areas of language than usual treatment alone, thus promoting psychological well-being.
The VRRS is equipped with a large screen and contains many virtual exercises divided into specific categories in order to perform speech disorder training tailored to the specific needs of children.
It can therefore be considered a useful complementary treatment to reduce symptoms by providing fun and actively engaging children, increasing motivation and adherence to treatment. This is why VRRS should be widely implemented in clinical practice.
This is a preliminary study, as we are conducting further research to highlight what we found in our sample. However, our study has limitations in that it examines a very small sample with heterogeneous issues. The children also had possible comorbidities with other disorders. These factors might make the reader uncertain with respect to the methodology, however, we have positive results regarding the rapid recovery of language skills. The innovative element of our project concerns the rehabilitation of language components through high-tech tools. The technological aspects are appealing because they are immediate, allow for the breaking down of logistical barriers, and promote learning motivation through sounds, colors, and setting. To improve clinical practice in the future, more studies are needed as the use of VRRS is still in its early stages, so larger samples and long-term follow-ups are essential.
Author Contributions
M.T., M.L.F. and I.C. participated in the study design and coordination, provided clinical oversight for data collection and interpretation, and drafted the manuscript; C.D.D., M.D.C. and F.C. (Francesca Cucinotta) conceptualized the study and supervised the manuscript; C.S., R.M. and M.D.C. participated in data collection and processing, contributed to the literature review, and helped draft the manuscript; A.I. and M.C.D.C. performed statistical analysis of the data; E.T., C.I. and F.C. (Francesco Corallo) contributed to the literature review and helped draft the manuscript; A.Q. and F.C. (Francesca Cucinotta) supervised the coordination of the study. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by Current Research Funds 2023, Ministry of Health, Italy.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethical Committee IRCCS Sicilia Centro Neurolesi “Bonino Pulejo” (protocol code 15/2019 and date of approval 5 June 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
The authors gratefully acknowledge all the families who participated in this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Diagnostic and Statistical Manual of Mental Disorders: DSM-5; American Psychiatric Publishing: Washington, DC, USA, 2013.
- Chilosi, A.M.; Brovedani, P.; Cipriani, P.; Casalini, C. Sex differences in early language delay and in developmental language disorder. J. Neurosci. Res. 2023, 101, 654–667. [Google Scholar] [CrossRef]
- Norbury, C.F.; Gooch, D.; Baird, G.; Charman, T.; Simonoff, E.; Pickles, A. Younger children experience lower levels of language competence and academic progress in the first year of school: Evidence from a population study. J. Child Psychol. Psychiatry 2016, 57, 65–73. [Google Scholar] [CrossRef]
- Tomblin, J.B.; Smith, E.; Zhang, X. Epidemiology of specific language impairment: Prenatal and perinatal risk factors. J. Commun. Disord. 1997, 30, 325–343. [Google Scholar] [CrossRef]
- Sharp, H.M.; Hillenbrand, K. Speech and language development and disorders in children. Pediatr. Clin. N. Am. 2008, 55, 1159–1173. [Google Scholar] [CrossRef] [PubMed]
- Fisher, E.L. A Systematic Review and Meta-Analysis of Predictors of Expressive-Language Outcomes Among Late Talkers. J. Speech Lang. Hear. Res. 2017, 60, 2935–2948. [Google Scholar] [CrossRef]
- Friend, M.; Schmitt, S.A.; Simpson, A.M. Evaluating the predictive validity of the computerized comprehension task: Comprehension predicts production. Dev. Psychol. 2012, 48, 136–148. [Google Scholar] [CrossRef] [PubMed]
- Feldman, H.M. How young children learn language and speech. Pediatr. Rev. 2019, 40, 398–411. [Google Scholar] [CrossRef] [PubMed]
- Redmond, S.M. Clinical intersections among idiopathic language disorder, social (pragmatic) communication disorder, and attention-deficit/hyperactivity disorder. J. Speech Lang. Hear. Res. 2020, 63, 3263–3276. [Google Scholar] [CrossRef]
- Yew, S.G.K.; O’Kearney, R. Emotional and behavioural outcomes later in childhood and adolescence for children with specific language impairments: Meta-analyses of controlled prospective studies. J. Child. Psychol. Psychiatry 2013, 54, 516–524. [Google Scholar] [CrossRef] [PubMed]
- O’Hare, A. Wayward words and watchful waiting: Should clinicians be more proactive for the preschooler with ‘uncomplicated’ expressive language delay? Arch Dis. Child 2009, 94, 80–82. [Google Scholar] [CrossRef]
- Desmarais, C.; Sylvestre, A.; Meyer, F.; Bairati, I.; Rouleau, N. Three profiles of language abilities in toddlers with an expressive vocabulary delay: Variations on a theme. J. Speech Lang. Hear. Res. 2010, 53, 699–709. [Google Scholar] [CrossRef]
- Young, A.R.; Beitchman, J.H.; Johnson, C.; Douglas, L.; Atkinson, L.; Escobar, M.; Wilson, B. Young adult academic outcomes in a longitudinal sample of early identified language impaired and control children. J. Child Psychol. Psychiatry 2002, 43, 635–645. [Google Scholar] [CrossRef]
- Conti-Ramsden, G.; Botting, N. Emotional health in adolescents with and without a history of specific language impairment (SLI). J. Child Psychol. Psychiatry 2008, 49, 516–525. [Google Scholar] [CrossRef]
- Law, J.; Rush, R.; Schoon, I.; Parsons, S. Modeling developmental language difficulties from school entry into adulthood: Literacy, mental health, and employment outcomes. J. Speech Lang. Hear. Res. 2009, 52, 1401–1416. [Google Scholar] [CrossRef]
- O’Hare, A.; Bremner, L. Management of developmental speech and language disorders: Part 1. Arch. Dis. Child. 2016, 101, 272–277. [Google Scholar] [CrossRef]
- Ebbels, S.H.; McCartney, E.; Slonims, V.; Dockrell, J.E.; Norbury, C.F. Evidence-based pathways to intervention for children with language disorders. International. J. Lang. Commun. Disord. 2019, 54, 3–19. [Google Scholar] [CrossRef]
- Lowe, H.; Henry, L.; Joffe, V.L. The Effectiveness of Classroom Vocabulary Intervention for Adolescents with Language Disorder. J. Speech Lang. Hear. Res. 2019, 62, 2829–2846. [Google Scholar] [CrossRef] [PubMed]
- Martins, S.; Cavaco, S. Customizable Serious Speech Therapy Games with Dynamic Difficulty Adjustment for Children with Sigmatism. MEDINFO 2022, 2021, 924–928. [Google Scholar]
- De Luca, R.; Calabrò, R.S.; Bramanti, P. Cognitive rehabilitation after severe acquired brain injury: Current evidence and future directions. Neuropsychol. Rehabil. 2018, 28, 879–898. [Google Scholar] [CrossRef]
- Moreno, J.M.M.; Sánchez, J.S.; Carrion, R.S.; Palmero, S.G.; González, P.S.; Pérez, C.G.; Aguilera, E.J.G. Monitoring visual attention on a neurorehabilitation environment based on Interactive Video. In Proceedings of the International Conference on Recent Advances on Neurorehabilitation (ICRAN 2013), Valencia, Spain, 7–8 March 2013. [Google Scholar]
- Martini, G.; Beani, E.; Filogna, S.; Menici, V.; Cioni, G.; Battini, R.; Sgandurra, G. New Technological Approach for the Evaluation of Postural Control Abilities in Children with Developmental Coordination Disorder. Children 2022, 9, 957. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, S.; Maggio, M.G.; Russo, M.; Bramanti, A.; Arcadi, F.A.; Naro, A.; Calabrò, R.S.; De Luca, R. Cognitive recovery in people with relapsing/remitting multiple sclerosis: A randomized clinical trial on virtual reality-based neurorehabilitation. Clin. Neurol. Neurosurg. 2021, 208, 106828. [Google Scholar] [CrossRef]
- Ravi, D.K.; Kumar, N.; Singhi, P. Effectiveness of virtual reality rehabilitation for children and adolescents with cerebral palsy: An updated evidence-based systematic review. Physiotherapy 2017, 103, 245–258. [Google Scholar]
- Alemanno, F.; Houdayer, E.; Emedoli, D.; Locatelli, M.; Mortini, P.; Mandelli, C.; Raggi, A.; Iannaccone, S. Efficacy of virtual reality to reduce chronic low back pain: Proof-of-concept of a non-pharmacological approach on pain, quality of life, neuropsychological and functional outcome. PLoS ONE 2019, 14, e0216858. [Google Scholar] [CrossRef]
- Maresca, G.; Maggio, M.G.; Buda, A.; La Rosa, G.; Manuli, A.; Bramanti, P.; Luca, R.D.; Calabrò, R.S. A novel use of virtual reality in the treatment of cognitive and motor deficit in spinal cord injury: A case report. Medicine 2018, 97, e13559. [Google Scholar] [CrossRef] [PubMed]
- Laver, K.; George, S.; Thomas, S.; Deutsch, J.E.; e Crotty, M. Realtà virtuale per la riabilitazione dell’ictus: Una versione ridotta di una revisione Cochrane. Riv. Eur. Di Med. Fis. E Riabil. 2015, 51, 497–506. [Google Scholar]
- Maresca, G.; Leonardi, S.; De Cola, M.C.; Giliberto, S.; Di Cara, M.; Corallo, F.; Quartarone, A.; Pidalà, A. Use of Virtual Reality in Children with Dyslexia. Children 2022, 9, 1621. [Google Scholar] [CrossRef] [PubMed]
- Patel, R.; Salata, A. Using computer games to mediate caregiver–child communication for children with severe dysarthria. J. Med. Speech Lang. Pathol. 2006, 14, 279–284. [Google Scholar]
- Bryant, L.; Brunner, M.; Hemsley, B. A review of virtual reality technologies in the field of communication disability: Implications for practice and research. Disabil. Rehabil. Assist. Technol. 2020, 15, 365–372. [Google Scholar] [CrossRef]
- Eldridge, S.M.; Chan, C.L.; Campbell, M.J.; Bond, C.M.; Hopewell, S.; Thabane, L.; Lancaster, G.A. PAFS consensus group. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. BMJ 2016, 355, i5239. [Google Scholar] [CrossRef]
- Cianchetti, C.; Fancello, G.S. Test TVL. Test di valutazione del linguaggio. In Livello Prescolare; Edizioni Erickson: Trento, Italy, 1997; Volume 16. [Google Scholar]
- Majorano, M.; Lavelli, M. The use of sophisticated words with children with specific language impairment during shared book reading. J. Commun. Disord. 2015, 53, 1–16. [Google Scholar] [CrossRef]
- Panesi, S.; Morra, S. The relation between drawing and language in preschoolers: The role of working Memory and executive functions. Cogn. Dev. 2022, 61, 101142. [Google Scholar] [CrossRef]
- Nicastri, M.; Giallini, I.; Amicucci, M.; Mariani, L.; de Vincentiis, M.; Greco, A.; Guerzoni, L.; Cuda, D.; Ruoppolo, G.; Mancini, P. Variables influencing executive functioning in preschool hearing-impaired children implanted within 24 months of age: An observational cohort study. Eur. Arch. Oto-Rhino-Laryngol. 2021, 278, 2733–2743. [Google Scholar]
- Angelillo, N.; Di Costanzo, B.; Barillari, U. Speech-language evaluation and rehabilitation treatment in Floating-Harbor syndrome: A case study. J. Commun. Disord. 2010, 43, 252–260. [Google Scholar] [CrossRef]
- Montirosso, R.; Giusti, L.; Del Prete, A.; Zanini, R.; Bellù, R.; Borgatti, R. Language outcomes at 36 months in prematurely born children is associated with the quality of developmental care in NICUs. J. Perinatol. 2016, 36, 768–774. [Google Scholar] [CrossRef]
- Roid, G.H.; Pomplun, M.; Martin, J. Nonverbal intellectual assessment with the Leiter-R. In A Practitioner’s Guide to Assessment of Intelligence Achievement; Naglieri, J., Goldstein, S., Eds.; Wiley: New York, NY, USA, 2013; pp. 265–290. [Google Scholar]
- Wechsel, D. Wechsler Preschool and Primary Scale of Intelligence-Fourth Edition (WPPSI-IV) dt. Bearbeitung von F.Petermann M. Daseking; Pearson Assessment: Frankfurt, Germany, 2018. [Google Scholar]
- Wechsler, D. Wechsler Intelligence Scale for Children, 4th Edition (WISC-IV); Psychological Corporation: San Antonio, TX, USA, 2003. [Google Scholar]
- Contrada, M.; Arcuri, F.; Tonin, P.; Pignolo, L.; Mazza, T.; Nudo, G.; Pignataro, M.L.; Quintieri, M.; Iozzi, A.; Cerasa, A. Stroke Telerehabilitation in Calabria: A Health Technology Assessment. Front. Neurol. 2022, 12, 2333. [Google Scholar] [CrossRef]
- De Luca, R.; Bonanno, M.; Rifici, C.; Pollicino, P.; Caminiti, A.; Morone, G.; Calabrò, R.S. Does Non-Immersive Virtual Reality Improve Attention Processes in Severe Traumatic Brain Injury? Encouraging Data from a Pilot Study. Brain Sci. 2022, 12, 1211. [Google Scholar] [CrossRef] [PubMed]
- Turolla, A.; Dam, M.; Ventura, L.; Tonin, P.; Agostini, M.; Zucconi, C.; Kiper, P.; Cagnin, A.; Piron, L. Virtual reality for the rehabilitation of the upper limb motor function after stroke: A prospective controlled trial. J. Neuroeng. Rehabil. 2013, 10, 1–9. [Google Scholar] [CrossRef]
- Agostini, M.; Garzon, M.; Benavides-Varela, S.; De Pellegrin, S.; Bencini, G.; Rossi, G.; Rosadoni, S.; Mancuso, M.; Turolla, A.; Meneghello, F.; et al. Telerehabilitation in poststroke anomia. BioMed Res. Int. 2014, 2014, 706909. [Google Scholar] [CrossRef]
- Maresca, G.; Maggio, M.G.; Latella, D.; Cannavò, A.; De Cola, M.C.; Portaro, S.; Stagnitti, M.C.; Silvestri, G.; Torrisi, M.; Bramanti, A.; et al. Toward improving poststroke aphasia: A pilot study on the growing use of telerehabilitation for the continuity of care. J. Stroke Cerebrovasc. Dis. 2019, 28, 104303. [Google Scholar] [CrossRef] [PubMed]
- Menici, V.; Barzacchi, V.; Filogna, S.; Beani, E.; Tinelli, F.; Cioni, G.; Sgandurra, G. Tele-Rehabilitation for Postural Control by Means of Virtual Reality Rehabilitation System in an Adolescent with Motor Disorder: A Case Study. Front. Psychol. 2021, 12, 720677. [Google Scholar] [PubMed]
- Stanica, I.C.; Moldoveanu, F.; Portelli, G.P.; Dascalu, M.I.; Moldoveanu, A.; Ristea, M.G. Flexible virtual reality system for neurorehabilitation and quality of life improvement. Sensors 2020, 20, 6045. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Wang, L.; Peng, G.; Yan, N.; Pan, X. Development and evaluation of a 3-D virtual pronunciation tutor for children with autism spectrum disorders. PLoS ONE 2019, 14, e0210858. [Google Scholar] [CrossRef]
- Halabi, O.; El-Seoud, S.A.; Alja’am, J.M.; Alpona, H.; Al-Hemadi, M.; Al-Hassan, D. Design of immersive virtual reality system to improve communication skills in individuals with autism. Int. J. Emerg. Technol. Learn. 2017, 12, 50–64. [Google Scholar] [CrossRef]
- Zhao, J.; Zhang, X.; Lu, Y.; Wu, X.; Zhou, F.; Yang, S.; Wang, L.; Wu, X.; Fei, F. Virtual reality technology enhances the cognitive and social communication of children with autism spectrum disorder. In Frontiers in Public Health. Frontiers Media SA. 2022, 10, 1029392. [Google Scholar] [CrossRef]
- Zhao, H.; Swanson, A.R.; Weitlauf, A.S.; Warren, Z.E.; Sarkar, N. Hand-in-hand: A communication-enhancement collaborative virtual reality system for promoting social interaction in children with autism spectrum disorders. IEEE Trans. Hum. Mach. Syst. 2018, 48, 136–148. [Google Scholar]
- Lorenzo, G.; Pomares, J.; Lledó, A. Inclusion of immersive virtual learning environments and visual control systems to support the learning of students with Asperger syndrome. Comput. Educ. 2013, 62, 88–101. [Google Scholar] [CrossRef]
- Frolli, A.; Savarese, G.; Di Carmine, F.; Bosco, A.; Saviano, E.; Rega, A.; Carotenuto, M.; Ricci, M.C. Children on the autism spectrum and the use of virtual reality for supporting social skills. Children 2022, 9, 181. [Google Scholar] [CrossRef]
- Brundage, S.B.; Hancock, A.B. Real enough: Using virtual public speaking environments to evoke feelings and behaviors targeted in stuttering assessment and treatment. Am. J. Speech-Lang. Pathol. 2015, 24, 139–149. [Google Scholar] [CrossRef]
- Almudhi, A. Evaluating adaptation effect in real versus virtual reality environments with people who stutter. Expert Rev. Med. Devices 2022, 19, 75–81. [Google Scholar] [CrossRef]
- Van Vuuren, S.; Cherney, L.R. A virtual therapist for speech and language therapy. In Proceedings of the Intelligent Virtual Agents: 14th International Conference, IVA 2014, Boston, MA, USA, 27–29 August 2014; Springer International Publishing: Berlin/Heidelberg, Germany, 2014; pp. 438–448. [Google Scholar]
- O’Connor, S. Virtual reality and avatars in health care. Clin. Nurs. Res. 2019, 28, 523–528. [Google Scholar] [CrossRef]
- Moro, C.; Štromberga, Z.; Raikos, A.; Stirling, A. The effectiveness of virtual and augmented reality in health sciences and medical anatomy. Anat. Sci. Educ. 2017, 10, 549–559. [Google Scholar] [CrossRef]
- Karamians, R.; Proffitt, R.; Kline, D.; Gauthier, L.V. Effectiveness of virtual reality-and gaming-based interventions for upper extremity rehabilitation poststroke: A meta-analysis. Arch. Phys. Med. Rehabil. 2020, 101, 885–896. [Google Scholar] [CrossRef]
- Giachero, A.; Calati, M.; Pia, L.; La Vista, L.; Molo, M.; Rugiero, C.; Fornaro, C.; Marangolo, P. Conversational therapy through semi-immersive virtual reality environments for language recovery and psychological well-being in post stroke aphasia. Behav. Neurol. 2020, 2020, 15. [Google Scholar] [CrossRef]
- Sultan, N.; Khushnood, K.; Qureshi, S.; Altaf, S.; Khan, M.K.; Malik, A.N.; Mehmood, R.; Awan, M.M.A. Effects of Virtual Reality Training Using Xbox Kinect on Balance, Postural Control, and Functional Independence in Subjects with Stroke. In Games for Health Journal; Mary Ann Liebert Inc.: Larchmont, NY, USA, 2023. [Google Scholar] [CrossRef]
- Manjari, K.; Verma, M.; Singal, G. A survey on assistive technology for visually impaired. Internet Things 2020, 11, 100188. [Google Scholar] [CrossRef]
- Feng, H.; Li, C.; Liu, J.; Wang, L.; Ma, J.; Li, G.; Gan, L.; Shang, X.; Wu, Z. Virtual reality rehabilitation versus conventional physical therapy for improving balance and gait in Parkinson’s disease patients: A randomized controlled trial. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2019, 25, 4186. [Google Scholar]
- Arane, K.; Behboudi, A.; Goldman, R.D. Virtual reality for pain and anxiety management in children. Can. Fam. Physician 2017, 63, 932–934. [Google Scholar] [PubMed]
- Coad, J.; Harding, S.; Hambly, H.; Parker, N.; Morgan, L.; Marshall, J.; Roulstone, S. Perspectives of preschool children in England with speech and language needs in the development of evidence-based activities. Child Care Health Dev. 2020, 46, 283–293. [Google Scholar] [CrossRef]
- Parsons, T.D.; Riva, G.; Parsons, S.; Mantovani, F.; Newbutt, N.; Lin, L.; Venturini, E.; Hall, T. Virtual reality in pediatric psychology. Pediatrics 2017, 140 (Suppl. S2), S86–S91. [Google Scholar] [CrossRef]
- Cavalcante Neto, J.L.; Steenbergen, B.; Tudella, E. Motor intervention with and without Nintendo® Wii for children with developmental coordination disorder: Protocol for a randomized clinical trial. Trials 2019, 20, 1–12. [Google Scholar]
- Bellani, M.; Fornasari, L.; Chittaro, L.; Brambilla, P. Virtual reality in autism: State of the art. Epidemiol. Psychiatr. Sci. 2011, 20, 235–238. [Google Scholar] [CrossRef]
- Shorey, S.; Ang, E.; Ng, E.D.; Yap, J.; Lau, L.S.T.; Chui, C.K. Communication skills training using virtual reality: A descriptive qualitative study. Nurse Educ. Today 2020, 94, 104592. [Google Scholar] [CrossRef] [PubMed]
- Salem, Y.; Elokda, A. Use of virtual reality gaming systems for children who are critically ill. J. Pediatr. Rehabil. Med. 2014, 7, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Voinescu, A.; Sui, J.; Fraser, D.S. Virtual reality in neurorehabilitation: An umbrella review of meta-analyses. J. Clin. Med. 2021, 10, 1478. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).