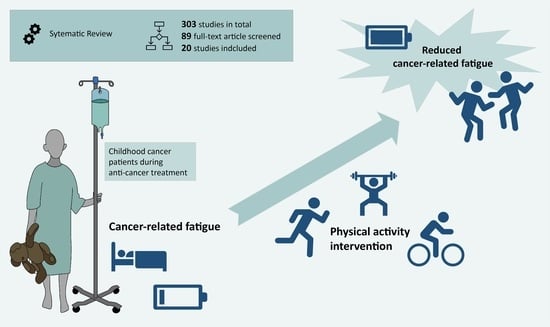
Physical Activity as a Treatment for Cancer-Related Fatigue in Children, Adolescents and Young Adults: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Search Strategy
2.3. Study Selection
- a study population consisting of cancer patients,
- a study population in which at least 75 percent of the subjects were children, adolescents or young adults under 21 years of age,
- the conduct of the studies during cancer treatment (intensive and maintenance therapy),
- the recording of the outcome CRF,
- the implementation of a physical activity intervention, and
- the examination of the association between the physical activity intervention and CRF.
2.4. Methodological Quality
2.5. Data Extraction and Analysis
- -
- Reference (author, year)
- -
- Country
- -
- Study design
- -
- Type of physical activity intervention
- -
- Study population (intervention and control group (number, age))
- -
- Entity
- -
- Therapy
- -
- Description of the intervention (duration, frequency, duration of a session, intensity)
- -
- Organisation and setting
- -
- Measurement of CRF and measurement time points
- -
- Results of the interventions on CRF (scores) and other outcomes (e.g., health-related quality of life)
- -
- Methodological quality.
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.2.1. Study Participants and Control Group
3.2.2. Physical Activity Interventions
3.2.3. Implementation of the Physical Activity Interventions
3.3. Methodological Quality
3.4. Effect of Physical Activity Interventions on CRF
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chang, C.-W.; Mu, P.-F.; Jou, S.-T.; Wong, T.-T.; Chen, Y.-C. Systematic review and meta-analysis of nonpharmacological interventions for fatigue in children and adolescents with cancer. Worldviews Evid.-Based Nurs. 2013, 10, 208–217. [Google Scholar] [CrossRef] [PubMed]
- Erickson, J.M. Fatigue in adolescents with cancer: A review of the literature. Clin. J. Oncol. Nurs. 2004, 8, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Ekti Genc, R.; Conk, Z. Impact of effective nursing interventions to the fatigue syndrome in children who receive chemotherapy. Cancer Nurs. 2008, 31, 312–317. [Google Scholar] [CrossRef]
- Hockenberry-Eaton, M.; Hinds, P.S.; Alcoser, P.; O’Neill, J.B.; Euell, K.; Howard, V.; Gattuso, J.; Taylor, J. Fatigue in children and adolescents with cancer. J. Pediatr. Oncol. Nurs. 1998, 15, 172–182. [Google Scholar] [CrossRef] [PubMed]
- Hofman, M.; Ryan, J.L.; Figueroa-Moseley, C.D.; Jean-Pierre, P.; Morrow, G.R. Cancer-related fatigue: The scale of the problem. Oncologist 2007, 12 (Suppl. 1), 4–10. [Google Scholar] [CrossRef]
- Nowe, E.; Stöbel-Richter, Y.; Sender, A.; Leuteritz, K.; Friedrich, M.; Geue, K. Cancer-related fatigue in adolescents and young adults: A systematic review of the literature. Crit. Rev. Oncol./Hematol. 2017, 118, 63–69. [Google Scholar] [CrossRef]
- Spathis, A.; Booth, S.; Grove, S.; Hatcher, H.; Kuhn, I.; Barclay, S. Teenage and Young Adult Cancer-Related Fatigue Is Prevalent, Distressing, and Neglected: It Is Time to Intervene. A Systematic Literature Review and Narrative Synthesis. J. Adolesc. Young Adult Oncol. 2015, 4, 3–17. [Google Scholar] [CrossRef]
- Walter, L.M.; Nixon, G.M.; Davey, M.J.; Downie, P.A.; Horne, R.S.C. Sleep and fatigue in pediatric oncology: A review of the literature. Sleep Med. Rev. 2015, 24, 71–82. [Google Scholar] [CrossRef]
- Goedendorp, M.M.; Gielissen, M.F.M.; Verhagen, C.A.H.; Peters, M.E.J.W.; Bleijenberg, G. Severe fatigue and related factors in cancer patients before the initiation of treatment. Br. J. Cancer 2008, 99, 1408–1414. [Google Scholar] [CrossRef]
- Horneber, M.; Fischer, I.; Dimeo, F.; Rüffer, J.U.; Weis, J. Cancer-related fatigue: Epidemiology, pathogenesis, diagnosis, and treatment. Dtsch. Arztebl. Int. 2012, 109, 161–171. [Google Scholar] [CrossRef]
- Langeveld, N.E.; Grootenhuis, M.A.; Voûte, P.A.; Haan, R.J.; van den Bos, C. No excess fatigue in young adult survivors of childhood cancer. Eur. J. Cancer 2003, 39, 204–214. [Google Scholar] [CrossRef] [PubMed]
- Thong, M.S.Y.; van Noorden, C.J.F.; Steindorf, K.; Arndt, V. Cancer-Related Fatigue: Causes and Current Treatment Options. Curr. Treat. Options Oncol. 2020, 21, 17. [Google Scholar] [CrossRef] [PubMed]
- Ullrich, C.K.; Dussel, V.; Hilden, J.M.; Sheaffer, J.W.; Moore, C.L.; Berde, C.B.; Wolfe, J. Fatigue in children with cancer at the end of life. J. Pain Symptom Manag. 2010, 40, 483–494. [Google Scholar] [CrossRef] [PubMed]
- Berger, A.M.; Mitchell, S.A.; Jacobsen, P.B.; Pirl, W.F. Screening, evaluation, and management of cancer-related fatigue: Ready for implementation to practice? CA A Cancer J. Clin. 2015, 65, 190–211. [Google Scholar] [CrossRef]
- Wagner, L.I.; Cella, D. Fatigue and cancer: Causes, prevalence and treatment approaches. Br. J. Cancer 2004, 91, 822–828. [Google Scholar] [CrossRef]
- Barsevick, A.M.; Irwin, M.R.; Hinds, P.; Miller, A.; Berger, A.; Jacobsen, P.; Ancoli-Israel, S.; Reeve, B.B.; Mustian, K.; O’Mara, A.; et al. Recommendations for High-Priority Research on Cancer-Related Fatigue in Children and Adults. JNCI J. Natl. Cancer Inst. 2013, 105, 1432–1440. [Google Scholar] [CrossRef]
- Morrow, G.R. Cancer-related fatigue: Causes, consequences, and management. Oncologist 2007, 12 (Suppl. 1), 1–3. [Google Scholar] [CrossRef]
- Daniel, L.C.; Brumley, L.D.; Schwartz, L.A. Fatigue in adolescents with cancer compared to healthy adolescents. Pediatr. Blood Cancer 2013, 60, 1902–1907. [Google Scholar] [CrossRef]
- Eddy, L.; Cruz, M. The relationship between fatigue and quality of life in children with chronic health problems: A systematic review. J. Spec. Pediatr. Nurs. JSPN 2007, 12, 105–114. [Google Scholar] [CrossRef]
- Hooke, M.C.; Linder, L.A. Symptoms in Children Receiving Treatment for Cancer-Part I: Fatigue, Sleep Disturbance, and Nausea/Vomiting. J. Pediatr. Oncol. Nurs. Off. J. Assoc. Pediatr. Oncol. Nurses 2019, 36, 244–261. [Google Scholar] [CrossRef]
- Tomlinson, D.; Zupanec, S.; Jones, H.; O’Sullivan, C.; Hesser, T.; Sung, L. The lived experience of fatigue in children and adolescents with cancer: A systematic review. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2016, 24, 3623–3631. [Google Scholar] [CrossRef]
- Bower, J.E. Cancer-related fatigue--mechanisms, risk factors, and treatments. Nat. Rev. Clin. Oncol. 2014, 11, 597–609. [Google Scholar] [CrossRef]
- Meneses-Echávez, J.F.; González-Jiménez, E.; Ramírez-Vélez, R. Effects of Supervised Multimodal Exercise Interventions on Cancer-Related Fatigue: Systematic Review and Meta-Analysis of Randomized Controlled Trials. BioMed Res. Int. 2015, 2015, 328636. [Google Scholar] [CrossRef] [PubMed]
- Mustian, K.M.; Alfano, C.M.; Heckler, C.; Kleckner, A.S.; Kleckner, I.R.; Leach, C.R.; Mohr, D.; Palesh, O.G.; Peppone, L.J.; Piper, B.F.; et al. Comparison of Pharmaceutical, Psychological, and Exercise Treatments for Cancer-Related Fatigue: A Meta-analysis. JAMA Oncol. 2017, 3, 961–968. [Google Scholar] [CrossRef] [PubMed]
- Braam, K.I.; van der Torre, P.; Takken, T.; Veening, M.A.; van Dulmen-den Broeder, E.; Kaspers, G.J.L. Physical exercise training interventions for children and young adults during and after treatment for childhood cancer. Cochrane Database Syst. Rev. 2016, 3, CD008796. [Google Scholar] [CrossRef]
- Robinson, P.D.; Oberoi, S.; Tomlinson, D.; Duong, N.; Davis, H.; Cataudella, D.; Culos-Reed, N.; Gibson, F.; Götte, M.; Hinds, P.; et al. Management of fatigue in children and adolescents with cancer and in paediatric recipients of haemopoietic stem-cell transplants: A clinical practice guideline. Lancet Child Adolesc. Health 2018, 2, 371–378. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- WHO Guidelines Approved by the Guidelines Review Committee. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Tufanaru, C.; Munn, Z.; Aromataris, E.; Campbell, J.; Hopp, L. Chapter 3: Systematic Reviews of Effectiveness. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: North Adelaide, SA, Australia, 2020. [Google Scholar]
- Pescatello, L.S. ACSM’s Guidelines for Exercise Testing and Prescription, 9th ed.; Wolters Kluwer/Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2014; p. 456. [Google Scholar]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; DeBeer, H.; et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, M.; Murnane, A.; Goddard, T.; Pendergrast, C.; Rogers, P.; Manudhane, R.; Osborn, M. A randomized controlled trial of a structured exercise intervention after the completion of acute cancer treatment in adolescents and young adults. Pediatr. Blood Cancer 2021, 68, e28751. [Google Scholar] [CrossRef]
- Bhatt, K.D.; Dhoriyani, N.B.; Smitha, D. A Comparative Study between Relaxation Technique and Aerobic Exercise in Fatigue During Chemotherapy in Acute Lymphoblastic Leukemia in Children. Indian J. Physiother. Occup. Ther.-Int. J. 2013, 7, 140. [Google Scholar] [CrossRef]
- Hamari, L.; Järvelä, L.S.; Lähteenmäki, P.M.; Arola, M.; Axelin, A.; Vahlberg, T.; Salanterä, S. The effect of an active video game intervention on physical activity, motor performance, and fatigue in children with cancer: A randomized controlled trial. BMC Res. Notes 2019, 12, 784. [Google Scholar] [CrossRef]
- Hinds, P.S.; Hockenberry, M.; Rai, S.N.; Zhang, L.; Razzouk, B.I.; Cremer, L.; McCarthy, K.; Rodriguez-Galindo, C. Clinical field testing of an enhanced-activity intervention in hospitalized children with cancer. J. Pain Symptom Manag. 2007, 33, 686–697. [Google Scholar] [CrossRef]
- Lam, K.K.W.; Li, W.H.C.; Chung, O.K.; Ho, K.Y.; Chiu, S.Y.; Lam, H.S.; Chan, G.C.F. An integrated experiential training programme with coaching to promote physical activity, and reduce fatigue among children with cancer: A randomised controlled trial. Patient Educ. Couns. 2018, 101, 1947–1956. [Google Scholar] [CrossRef] [PubMed]
- Stössel, S.; Neu, M.A.; Wingerter, A.; Bloch, W.; Zimmer, P.; Paret, C.; Malki, K.E.; Baumann, F.T.; Russo, A.; Henninger, N.; et al. Benefits of Exercise Training for Children and Adolescents Undergoing Cancer Treatment: Results From the Randomized Controlled MUCKI Trial. Front. Pediatr. 2020, 8, 243. [Google Scholar] [CrossRef] [PubMed]
- Van Dijk-Lokkart, E.M.; Braam, K.I.; van Dulmen-den Broeder, E.; Kaspers, G.J.L.; Takken, T.; Grootenhuis, M.A.; Streng, I.C.; Bierings, M.; Merks, J.H.; van den Heuvel-Eibrink, M.M.; et al. Effects of a combined physical and psychosocial intervention program for childhood cancer patients on quality of life and psychosocial functioning: Results of the QLIM randomized clinical trial. Psycho-Oncol. 2016, 25, 815–822. [Google Scholar] [CrossRef]
- Däggelmann, J.; Krauth, K.A.; Mailand, P.; Nopper, S.; Renniger, M.; Bündgen, L.; Rustler, V.; Bloch, W.; Baumann, F.T. Einfluss einer vierwöchigen familienorientierten Rehabilitation auf die motorische Leistungsfähigkeit, Lebensqualität und Fatigue bei krebskranken Kindern und gesunden Geschwistern. Die Rehabil. 2017, 56, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Hooke, M.C.; Hoelscher, A.; Tanner, L.R.; Langevin, M.; Bronas, U.G.; Maciej, A.; Mathiason, M.A. Kids Are Moving: A Physical Activity Program for Children with Cancer. J. Pediatr. Oncol. Nurs. Off. J. Assoc. Pediatr. Oncol. Nurses 2019, 36, 379–389. [Google Scholar] [CrossRef]
- Khoirunnisa; Hayati, H.; Afiyanti, Y.; Allenidekania. “AeRop exercise” can improve the sleep quality of Indonesian pediatric cancer patients. Enfermería Clínica 2019, 29, 342–345. [Google Scholar] [CrossRef]
- Rosenhagen, A.; Bernhörster, M.; Vogt, L.; Weiss, B.; Senn, A.; Arndt, S.; Siegler, K.; Jung, M.; Bader, P.; Banzer, W. Implementation of structured physical activity in the pediatric stem cell transplantation. Klin. Padiatr. 2011, 223, 147–151. [Google Scholar] [CrossRef]
- Spreafico, F.; Barretta, F.; Murelli, M.; Chisari, M.; Gattuso, G.; Terenziani, M.; Ferrari, A.; Veneroni, L.; Meazza, C.; Massimino, M. Positive Impact of Organized Physical Exercise on Quality of Life and Fatigue in Children and Adolescents with Cancer. Front. Pediatr. 2021, 9, 627876. [Google Scholar] [CrossRef] [PubMed]
- Yeh, C.H.; Man Wai, J.P.; Lin, U.-S.; Chiang, Y.-C. A pilot study to examine the feasibility and effects of a home-based aerobic program on reducing fatigue in children with acute lymphoblastic leukemia. Cancer Nurs. 2011, 34, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Bogg, T.F.T.; Broderick, C.; Shaw, P.; Cohn, R.; Naumann, F.L. Feasibility of an inpatient exercise intervention for children undergoing hematopoietic stem cell transplant. Pediatr. Transplant. 2015, 19, 925–931. [Google Scholar] [CrossRef]
- Diorio, C.; Schechter, T.; Lee, M.; O’Sullivan, C.; Hesser, T.; Tomlinson, D.; Piscione, J.; Armstrong, C.; Tomlinson, G.; Sung, L. A pilot study to evaluate the feasibility of individualized yoga for inpatient children receiving intensive chemotherapy. BMC Complement. Altern. Med. 2015, 15, 2. [Google Scholar] [CrossRef]
- Hooke, M.C.; Gilchrist, L.; Tanner, L.; Hart, N.; Withycombe, J.S. Use of a Fitness Tracker to Promote Physical Activity in Children with Acute Lymphoblastic Leukemia. Pediatr. Blood Cancer 2016, 63, 684–689. [Google Scholar] [CrossRef] [PubMed]
- Keats, M.R.; Culos-Reed, S.N. A community-based physical activity program for adolescents with cancer (project TREK): Program feasibility and preliminary findings. J. Pediatr. Hematol./Oncol. 2008, 30, 272–280. [Google Scholar] [CrossRef]
- Ovans, J.A.; Hooke, M.C.; Bendel, A.E.; Tanner, L.R. Physical Therapist Coaching to Improve Physical Activity in Children with Brain Tumors: A Pilot Study. Pediatr. Phys. Ther. Off. Publ. Sect. Pediatr. Am. Phys. Ther. Assoc. 2018, 30, 310–317. [Google Scholar] [CrossRef]
- Platschek, A.-M.; Kehe, L.; Abeln, V.; Berthold, F.; Simon, T.; Strüder, H. Computer-Based Exercise Program: Effects of a 12-Week Intervention on Mood and Fatigue in Pediatric Patients with Cancer. Clin. J. Oncol. Nurs. 2017, 21, E280–E286. [Google Scholar] [CrossRef]
- Su, H.-L.; Wu, L.-M.; Chiou, S.-S.; Lin, P.-C.; Liao, Y.-M. Assessment of the effects of walking as an exercise intervention for children and adolescents with cancer: A feasibility study. Eur. J. Oncol. Nurs. Off. J. Eur. Oncol. Nurs. Soc. 2018, 37, 29–34. [Google Scholar] [CrossRef]
- Oberoi, S.; Robinson, P.D.; Cataudella, D.; Culos-Reed, S.N.; Davis, H.; Duong, N.; Gibson, F.; Götte, M.; Hinds, P.; Nijhof, S.L.; et al. Physical activity reduces fatigue in patients with cancer and hematopoietic stem cell transplant recipients: A systematic review and meta-analysis of randomized trials. Crit. Rev. Oncol./Hematol. 2018, 122, 52–59. [Google Scholar] [CrossRef]
- Tomlinson, D.; Diorio, C.; Beyene, J.; Sung, L. Effect of exercise on cancer-related fatigue: A meta-analysis. Am. J. Phys. Med. Rehabil. 2014, 93, 675–686. [Google Scholar] [CrossRef] [PubMed]
- Zimmer, P.; Rüffer, J.U. Fatigue-Syndrom. In Sport Und Körperliche Aktivität in der Onkologie; Springer: Berlin/Heidelberg, Germany, 2012. [Google Scholar]
- Hilfiker, R.; Meichtry, A.; Eicher, M.; Nilsson Balfe, L.; Knols, R.H.; Verra, M.L.; Taeymans, J. Exercise and other non-pharmaceutical interventions for cancer-related fatigue in patients during or after cancer treatment: A systematic review incorporating an indirect-comparisons meta-analysis. Br. J. Sport. Med. 2018, 52, 651–658. [Google Scholar] [CrossRef] [PubMed]
- Patel, J.G.; Bhise, A.R. Effect of Aerobic Exercise on Cancer-related Fatigue. Indian J. Palliat. Care 2017, 23, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Tian, L.; Lu, H.J.; Lin, L.; Hu, Y. Effects of aerobic exercise on cancer-related fatigue: A meta-analysis of randomized controlled trials. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2016, 24, 969–983. [Google Scholar] [CrossRef]
- Van Vulpen, J.K.; Sweegers, M.G.; Peeters, P.H.M.; Courneya, K.S.; Newton, R.U.; Aaronson, N.K.; Jacobsen, P.B.; Galvão, D.A.; Chinapaw, M.J.; Steindorf, K.; et al. Moderators of Exercise Effects on Cancer-related Fatigue: A Meta-analysis of Individual Patient Data. Med. Sci. Sport. Exerc. 2020, 52, 303–314. [Google Scholar] [CrossRef]
- Campbell, K.L.; Winters-Stone, K.M.; Wiskemann, J.; May, A.M.; Schwartz, A.L.; Courneya, K.S.; Zucker, D.S.; Matthews, C.E.; Ligibel, J.A.; Gerber, L.H.; et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med. Sci. Sport. Exerc. 2019, 51, 2375–2390. [Google Scholar] [CrossRef]
- Stout, N.L.; Baima, J.; Swisher, A.K.; Winters-Stone, K.M.; Welsh, J. A Systematic Review of Exercise Systematic Reviews in the Cancer Literature (2005–2017). PM R J. Inj. Funct. Rehabil. 2017, 9, S347–S384. [Google Scholar] [CrossRef]
- LaVoy, E.C.P.; Fagundes, C.P.; Dantzer, R. Exercise, inflammation, and fatigue in cancer survivors. Exerc. Immunol. Rev. 2016, 22, 82–93. [Google Scholar]
- Phillips, S.M.; McAuley, E. Social cognitive influences on physical activity participation in long-term breast cancer survivors. Psycho-Oncol. 2013, 22, 783–791. [Google Scholar] [CrossRef]
- Medysky, M.E.; Temesi, J.; Culos-Reed, S.N.; Millet, G.Y. Exercise, sleep and cancer-related fatigue: Are they related? Neurophysiol. Clin. Clin. Neurophysiol. 2017, 47, 111–122. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]



| Author (Year) | Study Design | Population | Cancer Entity | Physical Activity Intervention | Control Group |
|---|---|---|---|---|---|
| Atkinson et al. (2021) [33] | RCT | N = 43 Maintenance therapy After care IG (n = 22): age (mean): 20.59 ± 3.2 y CG (n = 21): age (mean): 20.9 ± 2.6 y | Lymphomas 58.1% Germ cell tumours 18.6% Leukaemia 9.3% Bone tumours 7.0% Soft tissue sarcomas 4.7% CNS tumours 2.3% | Endurance and strength training (supervised) Duration of intervention: 10 Weeks Frequency: 2×/Week Duration of a session: 15–30 min Intensity: moderate–vigorous | Usual care |
| Bhatt et al. (2013) [34] | RCT | N = 36 age (range): 8–16 y Intensive cancer treatment | Leukaemia | Endurance training (supervised) Duration of intervention: 3 Weeks Frequency: 5×/Week Duration of a session: 20 min Intensity: n.a. | Relaxation technique |
| Bogg et al. (2015) [46] | SGI | N = 14 age (mean): 11.0 y Intensive cancer treatment | Leukaemia 36.4% Haematol. disorders 14.3% Lymphomas 7.1% | Multimodal training (supervised) Duration of intervention: Isolation phase during SCT Frequency: 5×/Week Duration of a session: 10–60 min Intensity: low–moderate | No CG |
| Däggelmann et al. (2017) [40] | QET | N = 42 Maintenance therapy After care IG (n = 22): age (mean): 10.36 ± 4.04 y CG (n = 20): age (mean): 9.10 ± 5.83 y | Leukaemia 36.3% CNS tumours 22.6% Lymphomas 13.5% Neuroblastomas 4.6% Retinoblastomas 4.6% Bone tumours 4.6% Soft tissue sarcomas 4.6% Germ cell tumours 4.6% Other solid tumours 4.6% | Rehabilitation program (multimodal; supervised) Duration of intervention: 4 Weeks Frequency: n.a. Duration of a session: n.a. Intensity: n.a. | Healthy siblings receive the same intervention as the IG |
| Diorio et al. (2015) [47] | SGI | N = 11 age (Median): 14.0 y Intensive cancer treatment | Leukaemia and lymphomas 72.7% Solid tumours 9.1% CNS tumours 9.1% Haematol. disorders 9.1% | Yoga (supervised) Duration of intervention: 3 Weeks Frequency: 3×/Week Duration of a session: n.a. Intensity: low–vigorous | No CG |
| Hamari et al. (2019) [35] | RCT | N = 36 IG (n = 17): age (mean): 7.8 y CG (n = 19): age (mean): 7.9 y | Leukaemia 47.2% Lymphomas 30.6% Nephroblastomas 5.6% Other solid tumours 16.7% | Technology-based physical activity intervention (partly supervised) Duration of intervention: 8 Weeks Frequency: daily Duration of a session: mind. 30 min Intensity: n.a. | Written advice for PA of 30 min/ day |
| Hinds et al. (2007) [36] | RCT | N = 29 IG (n = 14): age (mean): 13.08 ± 2.55 y CG (n = 15): age (mean): 11.92 ± 3.24 y. | Solid tumours 86.0% Leukaemia 14.0% | Endurance training (supervised) Duration of intervention: 2–4 Days Frequency: 2×/Tag Duration of a session: 30 min Intensity: n.a. | Usual care |
| Hooke et al. (2016) [48] | SGI | N = 16 age (mean): 8.69 ± 3.09 y | Leukaemia | Walking intervention with fitness tracker (non-supervised) Duration of intervention: 2 Weeks Frequency: n.a. Duration of a session: n.a. Intensity: n.a. | No CG |
| Hooke et al. (2019) [41] | QET | N = 57 IG (n = 30): age (mean): 12.0 ± 3.6 y CG (n = 27): age (mean): 12.8 ± 3.3 y | Leukaemia 33.3% Lymphomas 28.1% Solid tumours 38.6% | Education and coaching (non-supervised) Duration of intervention: n.a. Frequency: n.a. Duration of a session: n.a. Intensity: n.a. | Historical control group (usual care) |
| Keats and Culos-Read et al. (2008) [49] | SGI | N = 10 age (mean): 16.2 ± 1.6 y Intensive cancer treatment Maintenance therapy After care | Leukaemia 40.0% Lymphomas 40.0% CNS tumours 10.0% Germ cell tumours 10.0% | Multimodal training (supervised) Duration of intervention: 16 Weeks Frequency: 1×/Week Duration of a session: 90 min Intensity: individually adapted | No CG |
| Khoirunnisa et al. (2019) [42] | QET | N = 64 Intensive cancer treatment Maintenance therapy IG (n = 32): age (mean): 11.69 ± 2.58 y CG (n = 32): age (mean): 12.97 ± 3.20 y | Leukaemia and lymphomas 57.8% Solid tumours 42.2% | AeRop (endurance training and PMR) (partly supervised) Duration of intervention: 5 Days Frequency: daily Duration of a session: 30 min Intensity: n.a. | Usual care |
| Lam et al. (2018) [37] | RCT | N = 70 Intensive cancer treatment IG (n = 37): age (mean): 12.8 ± 2.5 y CG (n = 33): age (mean): 12.97 ± 3.20 y | Leukaemia 42.9% Lymphomas 21.4% CNS tumours 15.7% Germ cell tumours 8.6% Bone tumours 5.7% Other solid tumours 5.7% | Multimodal training (supervised) Duration of intervention: 6 months Frequency: 1–2×/Week Duration of a session: 60 min Intensity: low–moderate | Placebo intervention (home visits with leisure activities) |
| Ovans et al. (2018) [50] | SGI | N = 15 age (mean): 11.47 ± 3.33 y Intensive cancer treatment Maintenance therapy After care | CNS tumours | Walking interventions withfitness tracker and coaching(non-supervised) Duration of intervention: 2 Weeks Frequency: daily Duration of a session: n.a. Intensity: n.a. | No CG |
| Platschek et al. (2017) [51] | SGI | N = 9 age (mean): 11.33 ± 2.24 y Intensive cancer treatment Maintenance therapy | Leukaemia 33.3% Lymphomas 33.3% Sarcomas 22.2% Neuroblastomas 11.1% | Technology-based exercise intervention (supervised) Duration of intervention: 12 Weeks Frequency: n.a. Duration of a session: 45 min Intensity: individually adapted | No CG |
| Rosenhagen et al. (2011) [43] | QET | N = 23 age (mean): 15.3 ± 3.7 y Intensive cancer treatment IG (n = 13): age: n.a. CG (n = 10): age (mean): 13.6 ± 4.0 y | Leukaemia 79.0% Lymphomas 4.2% Neuroblastomas 4.2% Soft tissue sarcomas 4.2% Germ cell tumours 4.2% Haematol. disorders 4.2% | Multimodal training (supervised) Duration of intervention: 34.1 ± 9.4 days Frequency: 3×/Week Duration of a session: 50 min Intensity: moderate | Retrospective CG (usual care) |
| Spreafico et al. (2021) [44] | QET | N = 44 age (median): 15.5 y Intensive cancer treatment Maintenance therapy After care IG (n = 21): age: n.a. CG (n = 23): age: n.a. | Bone tumours 31.8% CNS tumours 18.2% Soft tissue sarcomas 18.2% Lymphomas 11.4% Neuroblastomas 11.4% Nephroblastomas 4.6% Other solid tumours 4.6% | Multimodal training (supervised) Duration of intervention: 6 Weeks Frequency: 3×/Week Duration of a session: 60 min Intensity: moderate | Usual care |
| Stössel et al. (2020) [38] | RCT | N = 33 Intensive cancer treatment IG (n = 16): age (mean): 10.6 ± 5.19 y CG (n = 17): age (mean): 11.4 ± 4.25 y | Leukaemia and lymphomas 45.5% CNS tumours 12.1% Other solid tumours 42.4% | Multimodal training (partly supervised) Duration of intervention: 6–8 Weeks Frequency: 3×/Week Duration of a session: 45–60 min Intensity: moderate | Usual care |
| Su et al. (2018) [52] | SGI | N = 18 age (mean): 11.89 ± 4.63 y Intensive cancer treatment Maintenance therapy After care | Leukaemia 66.7% Solid tumours 33.3% | Walking intervention with fitness tracker and education (partly supervised) Duration of intervention: 6 Weeks Frequency: 5×/Week Duration of a session: 15–30 min Intensity: n.a. | No CG |
| van Dijk-Lokkart et al. (2016) [39] | RCT | N = 68 Intensive cancer treatment Maintenance therapy After care IG (n = 30): age (mean): 13.0 ± 3.0 y CG (n = 10): age (mean): 12.6 ± 3.1 y | Leukaemia and lymphomas 67.7% Solid tumours 22.1% CNS tumours 10.3% | Endurance and strength training and psychosocial training (supervised) Duration of intervention: 12 Weeks Frequency: 2×/Week Duration of a session: 45 min Intensity: vigorous | Usual care |
| Yeh et al. (2011) [45] | QET | N = 22 Intensive cancer treatment Maintenance therapy IG (n = 12): age (mean): 11.01 ± 3.56 y CG (n = 10): age (mean): 12.48 ± 3.86 y | Leukaemia | Technology-based physical activity intervention (non-supervised) Duration of intervention: 6 Weeks Frequency: 3×/Week Duration of a session: 30 min Intensity: low–moderate | Usual care |
| Characteristics | Number of Studies |
|---|---|
| Diagnosis | |
| Leukaemias | 3 |
| CNS tumours | 1 |
| Heterogenous entitities | 16 |
| Treatment | |
| CTx | 9 |
| CTx and RT | 4 |
| SCT | 2 |
| CTx, RT and surgery | 1 |
| CTX, RT and SCT | 1 |
| CTx and SCT | 1 |
| CTx and surgery | 1 |
| Unclear | 1 |
| Treatment phase | |
| Intensive cancer treatment | 8 |
| Maintenance therapy | 1 |
| Intensive cancer treatment and maintenance therapy | 4 |
| Maintenance therapy and after care | 2 |
| During all treatment phases | 5 |
| Criteria | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author (Year) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | Score | % |
| Atkinson et al. (2021) [33] | y | y | Y | u | u | y | u | n | u | y | y | n | y | 7 | 53.85 |
| Bhatt et al. (2013) [34] | y | y | U | u | u | u | n | u | u | y | y | u | y | 5 | 38.46 |
| Hamari et al. (2019) [35] | y | u | Y | y | y | n | y | y | n | y | u | y | y | 9 | 69.23 |
| Hinds et al. (2007) [36] | y | u | Y | n | n | n | u | u | y | y | y | n | y | 6 | 46.15 |
| Lam et al. (2018) [37] | y | y | Y | n | n | y | n | y | y | y | u | y | y | 9 | 69.23 |
| Stössel et al. (2020) [38] | y | y | Y | n | n | n | y | y | y | y | y | u | y | 9 | 69.23 |
| van Dijk-Lokkart et al. (2016) [39] | y | u | Y | u | u | u | y | y | u | y | y | y | y | 8 | 61.54 |
| Criteria | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Author (Year) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Score | % |
| Bogg et al. (2015) [46] | y | Y | u | n | n | y | na | u | u | 3 | 33.33 |
| Däggelmann et al. (2017) [40] | y | N | n | y | y | u | y | y | u | 5 | 55.56 |
| Diorio et al. (2015) [47] | y | Y | n | n | y | u | na | y | n | 4 | 44.44 |
| Hooke et al. (2016) [48] | y | Y | y | n | y | u | na | y | u | 5 | 55.56 |
| Hooke et al. (2019) [41] | y | Y | u | y | n | n | n | y | u | 4 | 44.44 |
| Keats and Culos-Reed (2008) [49] | y | Y | n | n | y | y | na | u | n | 4 | 44.44 |
| Khoirunnisa et al. (2019) [42] | y | Y | y | y | y | u | y | y | u | 7 | 77.78 |
| Ovans et al. (2018) [50] | y | Y | n | n | y | y | na | y | u | 5 | 55.56 |
| Platschek et al. (2017) [51] | y | Y | y | n | y | y | na | y | u | 6 | 66.67 |
| Rosenhagen et al. (2011) [43] | y | N | n | n | y | u | y | y | u | 4 | 44.44 |
| Spreafico et al. (2021) [44] | y | N | y | y | n | na | n | y | u | 4 | 44.44 |
| Su et al. (2018) [52] | y | Y | n | n | y | y | na | u | u | 4 | 44.44 |
| Yeh et al. (2011) [45] | y | Y | y | y | y | y | y | u | u | 7 | 77.78 |
| Author (Year) | Measurement of CRF | ADH | Within-Group Differences (IG) | Between-Group Differences | ||
|---|---|---|---|---|---|---|
| Post-Test | Follow-Up Test | Post-Test | Follow-Up Test | |||
| Atkinson et al. (2021) [33] | FS-C FS-A | 90% | Post-test (after 10 weeks): CRF ↓ Endurance (VO2peak) ↑ Strength ↑ Flexibility ↑ QoL ↑ PA ↑ BMI ∼ | Follow-up (after 6 months): CRF ↓ Endurance (VO2peak) ∼ Strength ↑ Flexibility ↑ QoL ↑ PA ↑ BMI ↑↑ | Post-test (after 10 weeks): CRF ∼ Endurance (VO2peak) ++ Strength ∼ Flexibility ∼ QoL ∼ PA ∼ BMI ∼ | Follow-up (after 6 months): CRF ∼ Endurance (VO2peak) ∼ Strength ∼ Flexibility ∼ QoL ∼ PA ∼ BMI ++ |
| Bhatt et al. (2013) [34] | PFS | n.a. | Post-test (after 3 weeks): CRF ↓↓ | Post-test (after 3 weeks): CRF- - | ||
| Bogg et al. (2015) [46] | PedsQL MFS | 63% | Post-test (6 weeks after Tx): CRF ∼ QoL ∼ Endurance (6MWT) ↓↓ Strength ∼ Balance ↓↓ | |||
| Däggelmann et al. (2017) [40] | PedsQL MFS | n.a. | Post-test (after 4 weeks): Total CRF ↓↓ General fatigue ↓↓ Cognitive fatigue ↓ Sleep/rest fatigue ↓↓ HrQoL ↑ Motor performance ↑ | Follow-up (after 7 months): Total CRF ↓↓ General fatigue ↓↓ Cognitive fatigue ↓ Sleep/rest fatigue ↓↓ HrQoL ↑↑ Motor performance ↑↑ | ||
| Diorio et al. (2015) [47] | PedsQL MFS FS-C FS-A FS-P | n.a. | Post-test (after 3 weeks): General fatigue ∼ Sleep/rest fatigue ↑ CRF (parent-report) ↓ QoL ↑ | |||
| Hamari et al. (2019) [35] | PedsQL MFS | 77% | Post-test (after 8 weeks): CRF ∼ PA ↓ Motor performance ↓ | Post-test (after 8 weeks): CRF ∼ Step count + PA ∼ Motor performance ∼ | Follow-up (after 1 year): Step count - - | |
| Hinds et al. (2007) [36] | FS-Child FS-A FS-P FS-S | 85% | Post-test (daily for 3 days): CRF (self-report) ∼ CRF (parent-report) ∼ CRF (staff-report) ∼ Sleep duration ∼ | Post-test (daily for 3 days): CRF (self-report)- CRF (parent-report) + CRF (staff-report) + Sleep efficacy + Sleep duration + | ||
| Significant negative correlation between CRF and sleep quality | ||||||
| Hooke et al. (2016) [48] | FS-C FS-A | 92% | Post-test (after 2 weeks): CRF ∼ Step count ↑ | |||
| Significant negative correlation between step count and fatigue | ||||||
| Hooke et al. (2019) [41] | FS-C FS-A | n.a. | Post-test (after 6 months): All diagnosis groups: CRF↓ PA (self-report) ∼ Step count ∼ Sedentary time ∼ Solid tumours: CRF ↑↑ PA (self-report) ↓ Step count ∼ Sedentary time ∼ | ALL: CRF↓ PA (self-report) ↑ Step count↓ Sedentary time ∼ Lymphomas: CRF↓ PA (self-report)↓ Step count ↑↑ Sedentary time ∼ | Post-test (after 6 months): Differences between solid tumours and ALL/ lymphomas: CRF: significantly higher in solid tumours PA (self-report): non-significantly lower in solid tumours | |
| No correlation between PA and CRF | ||||||
| Keats and Culos-Read et al. (2008) [49] | PedsQL MFS | 82% | Post-test (after 16 weeks): Total CRF ↓ General fatigue ↓↓ Cognitive fatigue ∼ Sleep/rest fatigue ↓ QoL ↑↑ PA ↑ Upper body strength ↑↑ Flexibility ↑↑ BMI ∼ | Follow-up (after 7 months): Total CRF ↓↓ General fatigue ↓↓ Cognitive fatigue ↓ Sleep/rest fatigue ↓↓ QoL ↑↑ PA ↑↑ Upper body strength ↑↑ Flexibility ↑ BMI ↑ | ||
| Khoirunnisa et al. (2019) [42] | CFS | n.a. | Post-test (at day 5): CRF ++ Sleep quality ++ | |||
| Lam et al. (2018) [37] | FS-C FS-A | n.a. | Follow-up (after 9 months): CRF ↓↓ QoL ↑↑ PA ↑↑ Self-efficacy ↑↑ Hand-grip strength ↑↑ | Post-test (after 6 months): CRF ++ QoL + Self-efficacy ++ Hand-grip strength ++ | Follow-up (after 9 months): CRF ++ QoL ++ PA ++ Self-efficacy + Hand-grip strength + | |
| Ovans et al. (2018) [50] | PedsQL MFS | n.a. | Post-test (after 12 weeks): Total CRF ↓↓ General fatigue ↓↓ Cognitive fatigue ↓ Sleep/rest fatigue ↓↓ QoL ↑ Step count ↑ Endurance (6MWT) ↑↑ PA ↑ | Follow-up (after 24 weeks): Total CRF ↓↓ General fatigue ↓↓ Cognitive fatigue ↓ Sleep/rest fatigue ↓ QoL ↑ Step count ↑ Endurance (6MWT) ↑ PA ↑ | ||
| Significant negative correlation between CRF and step count | ||||||
| Platschek et al. (2017) [51] | PedsQL MFS | n.a. | Post-test (after 12 weeks): Total CRF ↓↓ General fatigue ↓ Cognitive fatigue ↓ Sleep/rest fatigue ↓↓ Physical condition ↑↑ Mental resilience ↑↑ Motivation ↑↑ | |||
| Rosenhagen et al. (2011) [43] | PedsQL MFS | n.a. | Post-test (at discharge after Tx): CRF ↓ QoL ↑ Hand-grip strength ↑ Endurance ∼ | |||
| Spreafico et al. (2021) [44] | PedsQL MFS | n.a. | Post-test (after 6 weeks): Total CRF- General fatigue + Cognitive fatigue - Sleep/rest fatigue - QoL + | |||
| Stössel et al. (2020) [38] | PedsQL MFS | n.a. | Post-test (after 6–8 weeks): CRF (self report) ↓↓ CRF (parent report) ↓↓ QoL (self report) ↑ QoL (parent report) ∼ Leg strength ↑↑ Arm strength ↑ Endurance (6MWT) ↑↑ Phase angle ∼ BMI ∼ PA ↑↑ | Post-test (after 6–8 weeks): CRF (self report) + CRF (parent report) ++ QoL (self report) + QoL (parent report) ∼ Leg strength ++ Arm strength ∼ Endurance (6MWT) ++ Phase angle ∼ BMI ∼ PA ++ | ||
| Significant correlation between PA and better physical and mental well-being, higher self-confidence and lower CRF values | ||||||
| Su et al. (2018) [52] | PedsQL MFS | 72–89% | Post-test (after 6 weeks): Total CRF ↓↓ General fatigue ↓↓ Cognitive fatigue ↓↓ Sleep/rest fatigue ↓ QoL ↑ Endurance (6MWT) ↑↑ Sleep quality ∼ PA ↑↑ | |||
| van Dijk- Lokkart et al. (2016) [39] | PedsQL MFS | n.a. | Post-test (after 4 months): CRF (self report) ↓ CRF (parent report) ↓ | Follow-up (after 12 months): CRF (self report) ↓ CRF (parent report) ↓ | Post-test (after 4 months): CRF (self report) ∼ CRF (parent report) ∼ QoL ∼ Behav. disorders ∼ Depression ∼ Self-perception ∼ | Follow-up (after 12 months): CRF (self report) ∼ CRF (parent report) ∼ QoL ∼ Behav. disorders ∼ Depression ∼ Self-perception ∼ |
| Yeh et al. (2011) [45] | PedsQL MFS | ITT: 76% PP: 90% | Post-test (after 6 weeks): ITT: General fatigue ↓ Cognitive fatigue ↓ Sleep/rest fatigue ↓ PP: General fatigue ↓ Cognitive fatigue ↓ Sleep/rest fatigue ↓ | Follow-up (after 10 weeks): ITT: General fatigue ↓ Cognitive fatigue ↓ Sleep/rest fatigue ↓ PP: General fatigue ↓ Cognitive fatigue ↓ Sleep/rest fatigue ↓ | Post-test (after 6 weeks): ITT: General fatigue ∼ Cognitive fatigue + Sleep/rest fatigue + PP: General fatigue ∼ Cognitive fatigue + Sleep/rest fatigue + | Follow-up (after 10 weeks): ITT: General fatigue + Cognitive fatigue + Sleep/rest fatigue + PP: General fatigue ++ Cognitive fatigue + Sleep/rest fatigue + |
| No correlation between haemoglobin level and fatigue | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuehn, M.; Wypyrsczyk, L.; Stoessel, S.; Neu, M.A.; Ploch, L.; Dreismickenbecker, E.; Simon, P.; Faber, J. Physical Activity as a Treatment for Cancer-Related Fatigue in Children, Adolescents and Young Adults: A Systematic Review. Children 2023, 10, 572. https://doi.org/10.3390/children10030572
Kuehn M, Wypyrsczyk L, Stoessel S, Neu MA, Ploch L, Dreismickenbecker E, Simon P, Faber J. Physical Activity as a Treatment for Cancer-Related Fatigue in Children, Adolescents and Young Adults: A Systematic Review. Children. 2023; 10(3):572. https://doi.org/10.3390/children10030572
Chicago/Turabian StyleKuehn, Mareike, Lena Wypyrsczyk, Sandra Stoessel, Marie A. Neu, Lisa Ploch, Elias Dreismickenbecker, Perikles Simon, and Joerg Faber. 2023. "Physical Activity as a Treatment for Cancer-Related Fatigue in Children, Adolescents and Young Adults: A Systematic Review" Children 10, no. 3: 572. https://doi.org/10.3390/children10030572
APA StyleKuehn, M., Wypyrsczyk, L., Stoessel, S., Neu, M. A., Ploch, L., Dreismickenbecker, E., Simon, P., & Faber, J. (2023). Physical Activity as a Treatment for Cancer-Related Fatigue in Children, Adolescents and Young Adults: A Systematic Review. Children, 10(3), 572. https://doi.org/10.3390/children10030572