Extra Lateral Pin or Less Radiation? A Comparison of Two Different Pin Configurations in the Treatment of Supracondylar Humerus Fracture
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Anjum, R.; Sharma, V.; Jindal, R.; Singh, T.P.; Rathee, N. Epidemiologic pattern of paediatric supracondylar fractures of humerus in a teaching hospital of rural India: A prospective study of 263 cases. Chin. J. Traumatol. 2017, 20, 158–160. [Google Scholar] [CrossRef] [PubMed]
- Mehlman, C.T.; Denning, J.R.; McCarthy, J.J.; Fisher, M.L. Infantile supracondylar humeral fractures (patients less than two years of age): Twice as common in females and a high rate of malunion with lateral column-only fixation. J. Bone Jt. Surg. Am. 2019, 101, 25–34. [Google Scholar] [CrossRef]
- Wilkins, K.E. Supracondylar Fractures. In Fractures in Children, 3rd ed.; Rockwood, C.A., Wilkins, K.E., King, R.E., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 1991; pp. 526–617. [Google Scholar]
- Kocher, M.S.; Kasser, J.R.; Waters, P.M.; Bae, D.; Snyder, B.D.; Hresko, M.T.; Daniel, H.; Lawrence, K.; Kim, Y.J.; Murray, M.M.; et al. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children. A randomized clinical trial. J. Bone Jt. Surg. Am. 2007, 89, 706–712. [Google Scholar] [CrossRef]
- Otsuka, N.Y.; Kasser, J.R. Supracondylar Fractures of the Humerus in Children. J. Am. Acad. Orthop. Surg. 1997, 5, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Gartland, J.J. Management of supracondylar fractures of the humerus in children. Surg. Gynecol. Obstet. 1959, 109, 145–154. [Google Scholar] [PubMed]
- Leitch, K.K.; Kay, R.M.; Femino, J.D.; Tolo, V.T.; Storer, S.K.; Skaggs, D.L. Treatment of multidirectionally unstable supracondylar humeral fractures in children. A modified Gartland type-IV fracture. J. Bone Jt. Surg. Am. 2006, 88, 980–985. [Google Scholar] [CrossRef] [PubMed]
- Keskin, D.; Sen, H. The comparative evaluation of treatment outcomes in pediatric displaced supracondylar humerus fractures managed with either open or closed reduction and percutaneous pinning. Acta Chir. Orthop. Traumatol. Cech. 2014, 81, 380–386. [Google Scholar]
- Rakha, A.; Khan, R.D.A.; Arshad, A.; Khan, Z.A.; Ahmad, S.; Mahmood, S. Comparison of efficacy between open and close reduction in supracondylar fracture of humerus in children using Flynn’s criteria. Ann. Punjab Med. Coll. 2020, 14, 32–36. [Google Scholar]
- Maity, A.; Saha, D.; Roy, D.S. A prospective randomised, controlled clinical trial comparing medial and lateral entry pinning with lateral entry pinning for percutaneous fixation of displaced extension type supracondylar fractures of the humerus in children. J. Orthop. Surg. Res. 2012, 7, 6. [Google Scholar] [CrossRef]
- Gordon, J.E.; Patton, C.M.; Luhmann, S.J.; Bassett, G.S.; Schoenecker, P.L. Fracture stability after pinning of displaced supracondylar distal humerus fractures in children. J. Pediatr. Orthop. 2001, 21, 313–318. [Google Scholar] [CrossRef]
- Skaggs, D.L.; Hale, J.M.; Bassett, J.; Kaminsky, C.; Kay, R.M.; Tolo, V.T. Operative treatment of supracondylar fractures of the humerus in children. The consequences of pin placement. J. Bone Jt. Surg. Am. 2001, 83, 735–740. [Google Scholar] [CrossRef]
- Rasool, M.N. Ulnar nerve injury after K-wire fixation of supracondylar humerus fractures in children. J. Pediatr. Orthop. 1998, 18, 686–690. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.S.; Mahar, A.T.; Miesen, D.; Newton, P.O. Displaced pediatric supracondylar humerus fractures: Biomechanical analysis of percutaneous pinning techniques. J. Pediatr. Orthop. 2002, 22, 440–443. [Google Scholar] [CrossRef] [PubMed]
- Feng, C.; Guo, Y.; Zhu, Z.; Zhang, J.; Wang, Y. Biomechanical analysis of supracondylar humerus fracture pinning for fractures with coronal lateral obliquity. J. Pediatr. Orthop. 2012, 32, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Wallace, M.; Johnson, D.B.; Pierce, W.; Iobst, C.; Riccio, A.; Wimberly, R.L. Biomechanical Assessment of Torsional Stiffness in a Supracondylar Humerus Fracture Model. J. Pediatr. Orthop. 2019, 39, e210–e215. [Google Scholar] [CrossRef]
- Larson, L.; Firoozbakhsh, K.; Passarelli, R.; Bosch, P. Biomechanical analysis of pinning techniques for pediatric supracondylar humerus fractures. J. Pediatr. Orthop. 2006, 26, 573–578. [Google Scholar] [CrossRef] [PubMed]
- Richter, P.; Dehner, C.; Scheiderer, B.; Gebhard, F.; Kraus, M. Emission of radiation in the orthopaedic operation room: A comprehensive review. OA Musculoskelet. Med. 2013, 1, 11. [Google Scholar] [CrossRef]
- Ron, E. Ionizing radiation and cancer risk: Evidence from epidemiology. Pediatr. Radiol. 2002, 32, 232–244. [Google Scholar] [CrossRef]
- Sapienza, M.; Testa, G.; Vescio, A.; Panvini, F.M.C.; Caldaci, A.; Parisi, S.C.; Pavone, V.; Canavese, F. The Role of Patient Position in the Surgical Treatment of Supracondylar Fractures of the Humerus: Comparison of Prone and Supine Position. Medicina 2023, 59, 374. [Google Scholar] [CrossRef]
- Flynn, J.C.; Matthews, J.G.; Benoit, R.L. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years’ experience with long-term follow-up. J. Bone Jt. Surg. Am. 1974, 56, 263–272. [Google Scholar] [CrossRef]
- Topping, R.E.; Blanco, J.S.; Davis, T.J. Clinical evaluation of crossed-pin versus lateral-pin fixation in displaced supracondylar humerus fractures. J. Pediatr. Orthop. 1995, 15, 435–439. [Google Scholar] [CrossRef] [PubMed]
- Sankar, W.N.; Hebela, N.M.; Skaggs, D.L.; Flynn, J.M. Loss of pin fixation in displaced supracondylar humeral fractures in children: Causes and prevention. J. Bone Jt. Surg. Am. 2007, 89, 713–717. [Google Scholar]
- Lyons, J.P.; Ashley, E.; Hoffer, M.M. Ulnar nerve palsies after percutaneous cross-pinning of supracondylar fractures in children’s elbows. J. Pediatr. Orthop. 1998, 18, 43–45. [Google Scholar] [CrossRef]
- Özçelik, A.; Tekcan, A.; Ömeroglu, H. Correlation between iatrogenic ulnar nerve injury and angular insertion of the medial pin in supracondylar humerus fractures. J. Pediatr. Orthop. 2006, 15, 58–61. [Google Scholar] [CrossRef] [PubMed]
- Royce, R.O.; Dutkowsky, J.P.; Kasser, J.R.; Rand, F.R. Neurologic complications after K-wire fixation of supracondylar humerus fractures in children. J. Pediatr. Orthop. 1991, 11, 191–194. [Google Scholar] [CrossRef] [PubMed]
- Prashant, K.; Lakhotia, D.; Bhattacharyya, T.D.; Mahanta, A.K.; Ravoof, A. A comparative study of two percutaneous pinning techniques (lateral vs medial-lateral) for Gartland type III pediatric supracondylar fracture of the humerus. J. Orthop. Traumatol. 2016, 17, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Dekker, A.E.; Krijnen, P.; Schipper, I.B. Results of crossed versus lateral entry K-wire fixation of displaced pediatric supracondylar humeral fractures: A systematic review and meta-analysis. Injury 2016, 47, 2391–2398. [Google Scholar] [CrossRef]
- Appelboam, A.; Reuben, A.D.; Benger, J.R.; Beech, F.; Dutson, J.; Haig, S.; Higginson, I.; Klein, J.A.; Le Roux, S.; Saranga, S.S.; et al. Elbow extension test to rule out elbow fracture: Multicentre, prospective validation and observational study of diagnostic accuracy in adults and children. BMJ 2008, 337, a2428. [Google Scholar] [CrossRef]
- Lennon, R.I.; Riyat, M.S.; Hilliam, R.; Anathkrishnan, G.; Alderson, G. Can a normal range of elbow movement predict a normal elbow X-ray? Emerg. Med. J. EMJ 2007, 24, 86–88. [Google Scholar] [CrossRef]
- Darracq, M.A.; Vinson, D.R.; Panacek, E.A. Preservation of active range of motion after acute elbow trauma predicts absence of elbow fracture. Am. J. Emerg. Med. 2008, 26, 779–782. [Google Scholar] [CrossRef]
- Kraus, R.; Dresing, K. Rational Usage of Fracture Imaging in Children and Adolescents. Diagnostics 2023, 13, 538. [Google Scholar] [CrossRef] [PubMed]
- Kocaoğlu, H.; Kalem, M.; Kavak, M.; Şahin, E.; Başarır, K.; Kınık, H. Comparison of operating time, fluoroscopy exposure time, and functional and radiological results of two surgical methods for distal forearm fractures of both-bones in pediatric patients: Is it necessary to fix both bones? Acta Orthop. Traumatol. Turc. 2020, 54, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Martus, J.E.; Hilmes, M.A.; Grice, J.V.; Stutz, C.M.; Schoenecker, J.G.; Lovejoy, S.A.; Mencio, G.A. Radiation Exposure During Operative Fixation of Pediatric Supracondylar Humerus Fractures: Is Lead Shielding Necessary? J. Pediatr. Orthop. 2018, 38, 249–253. [Google Scholar] [CrossRef]
- Schmucker, A.; Chen, R.; Vachhrajani, S.; Martinek, M.; Albert, M. Radiation exposure in the treatment of pediatric supracondylar humerus fractures. Arch. Orthop. Trauma Surg. 2020, 140, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Tzatzairis, T.; Firth, G.; Bijlsma, P.; Manoukian, D.; Maizen, C.; Ramachandran, M. Radiation Exposure in The Treatment of Pediatric Supracondylar Humerus Fractures: Comparison of Two Fixation Methods. Open Orthop. J. 2021, 15, 22–26. [Google Scholar] [CrossRef]



| 2L1M | 1L1M | p Value | |
|---|---|---|---|
| No. of patients | 26 | 22 | |
| Age | 6.57 ± 2.01 | 6.51 ± 2.08 | 0.925 |
| Sex | 0.141 | ||
| male | 15 | 8 | |
| female | 11 | 14 | |
| Type of Fracture | 0.105 | ||
| Gartland 2 | 6 | 6 | |
| Gartland 3 | 11 | 14 | |
| Gartland 4 | 9 | 2 | |
| Flynn Criteria | 0.330 | ||
| excellent | 24 | 17 | |
| good | 2 | 7 | |
| fair | 0 | 0 | |
| poor | 0 | 0 |
| Pin Configuration | N | Mean Rank | p Value | |
|---|---|---|---|---|
| Surgical duration in min | 2L1M | 26 | 40.61 ± 8.25 | |
| 1L1M | 22 | 30.59 ± 8.72 | ||
| Total | 48 | 0.001 | ||
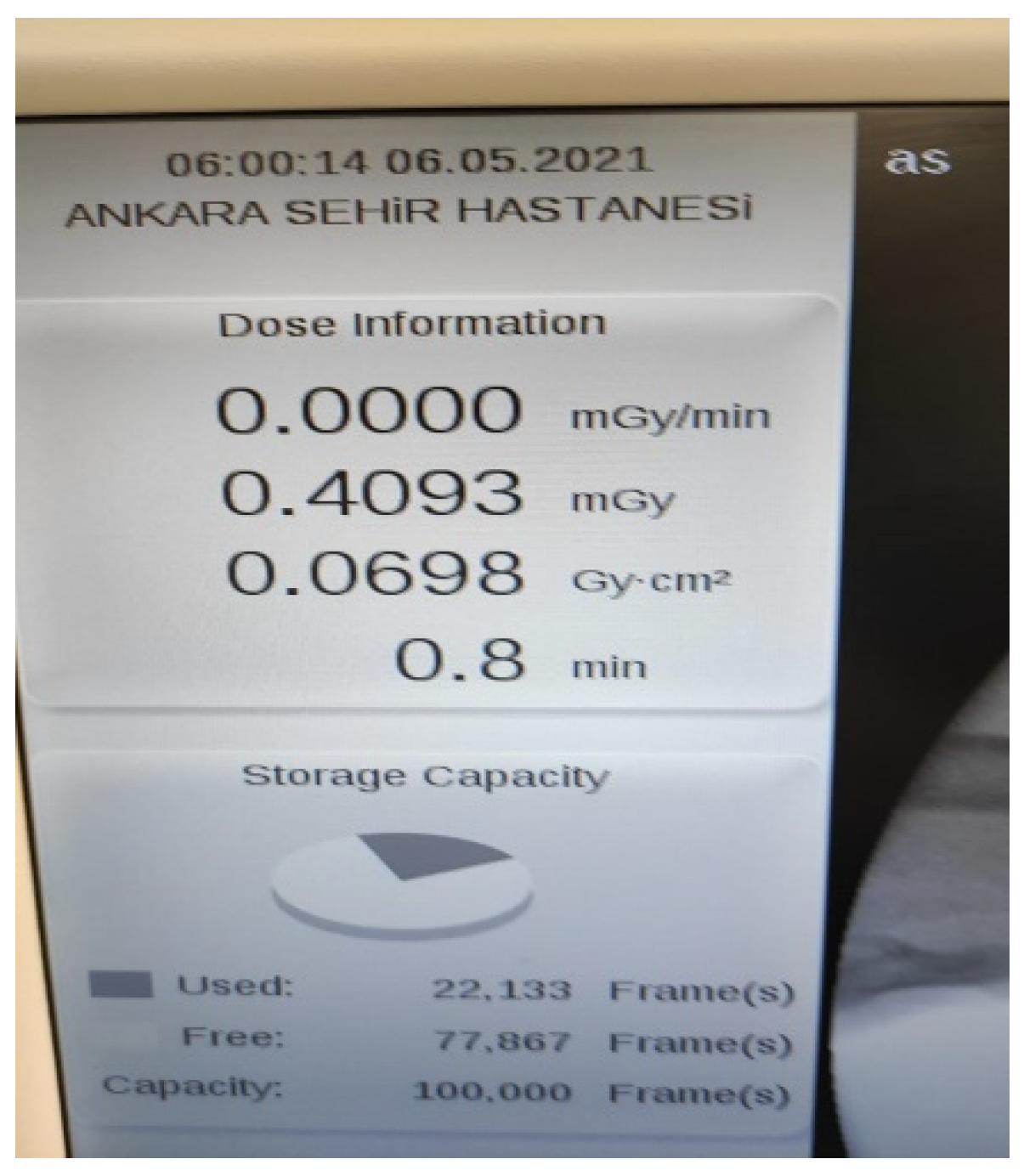
| Radiation duration in min | 2L1M | 26 | 1.68 ± 0.55 | |
| 1L1M | 22 | 0.76 ± 0.33 | ||
| Total | 48 | <0.001 | ||
| Radiaton dose in mGy | 2L1M | 26 | 2.45 ± 1.15 | |
| 1L1M | 22 | 0.55 ± 0.43 | ||
| Total | 48 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaya, Ö.; Gencer, B.; Çulcu, A.; Doğan, Ö. Extra Lateral Pin or Less Radiation? A Comparison of Two Different Pin Configurations in the Treatment of Supracondylar Humerus Fracture. Children 2023, 10, 550. https://doi.org/10.3390/children10030550
Kaya Ö, Gencer B, Çulcu A, Doğan Ö. Extra Lateral Pin or Less Radiation? A Comparison of Two Different Pin Configurations in the Treatment of Supracondylar Humerus Fracture. Children. 2023; 10(3):550. https://doi.org/10.3390/children10030550
Chicago/Turabian StyleKaya, Özgür, Batuhan Gencer, Ahmet Çulcu, and Özgür Doğan. 2023. "Extra Lateral Pin or Less Radiation? A Comparison of Two Different Pin Configurations in the Treatment of Supracondylar Humerus Fracture" Children 10, no. 3: 550. https://doi.org/10.3390/children10030550
APA StyleKaya, Ö., Gencer, B., Çulcu, A., & Doğan, Ö. (2023). Extra Lateral Pin or Less Radiation? A Comparison of Two Different Pin Configurations in the Treatment of Supracondylar Humerus Fracture. Children, 10(3), 550. https://doi.org/10.3390/children10030550







