Strategies to Aid Successful Transition of Adolescents with Congenital Heart Disease: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Data Extraction
3. Results
3.1. Proportion of Loss of Follow-Up around the World
3.2. Regional Fluctuations in Loss of Follow-Up
3.3. Relationship between Disease Complexity and Discontinuation of Care
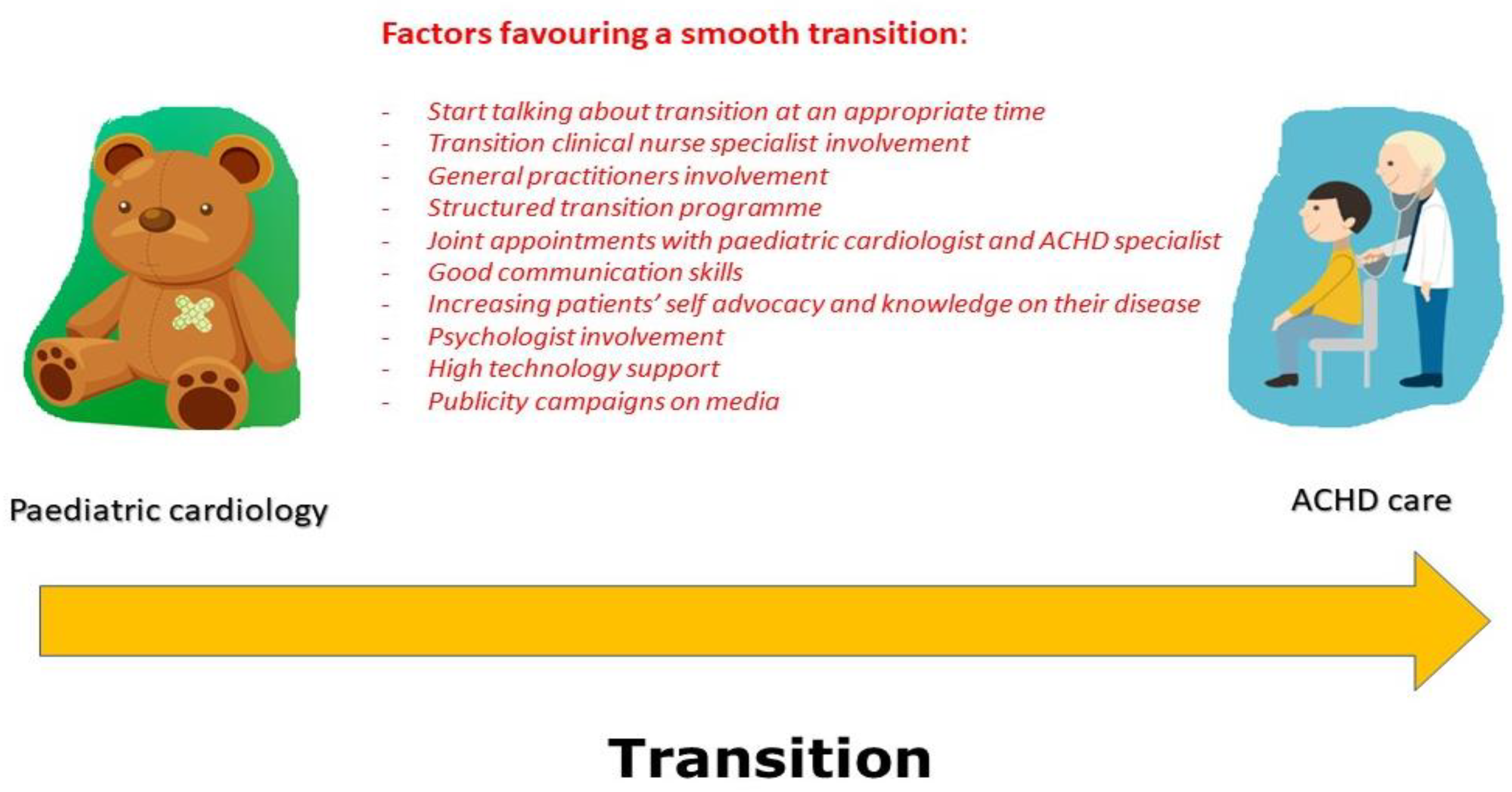
3.4. Strategies to Lower the Loss to Follow-Up
- Creating a tailored app with a few things such as a specific diagram for each patient, a transition checklist, a way to monitor progress throughout the list, a past medical history background, notifications of appointments, and therapeutic changes;
- Establishing education for patients with video clips for each specific disease with links to learning topics such as the way to recognise an emergency;
- Promoting mentorship from peers and ACHD patients suffering from the same condition and enabling connection with each other by means of chats;
- Creating blog spaces and forums for patients to share their experience, ask medical questions, and make comments about the other patients’ observations [63].
- Features that are specific to ACHD populations including the influence of social factors determining health, well-being, and neurological status;
- The additional costs for the health care system and potential health complications that are related to inadequate transition to ACHD care including the increased access to the Emergency Department;
- The need to set up tailored transition programmes addressing and implementing the participation of CHD adolescents in face-to-face and online appointments with care givers, adopting a family-centred approach [69].
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mandalenakis, Z.; Rosengren, A.; Skoglund, K.; Lappas, G.; Eriksson, P.; Dellborg, M. Survivorship in children and young adults with congenital heart disease in Sweden. JAMA Intern. Med. 2017, 177, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Moons, P.; Bovijn, L.; Budts, W.; Belmans, A.; Gewillig, M. Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation 2010, 122, 2264–2272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campbell, F.; Biggs, K.; Aldiss, S.K.; O’Neill, P.M.; Clowes, M.; McDonagh, J.; While, A.; Gibson, F. Transition of care for adolescents from paediatric services to adult health services. Cochrane Database Syst. Rev. 2016, 4, CD009794. [Google Scholar] [CrossRef] [Green Version]
- Bassareo, P.P.; Saba, L.; Solla, P.; Barbanti, C.; Marras, A.R.; Mercuro, G. Factors influencing adaptation and performance at physical exercise in complex congenital heart diseases after surgical repair. Biomed. Res. Int. 2014, 2014, 862372. [Google Scholar] [CrossRef]
- Webb, G.; Mulder, B.J.; Aboulhosn, J.; Daniels, C.J.; Elizari, M.A.; Hong, G.; Horlick, E.; Landzberg, M.J.; Marelli, A.J.; O’Donnell, C.P.; et al. The care of adults with congenital heart disease across the globe: Current assessment and future perspective: A position statement from the International Society for Adult Congenital Heart Disease (ISACHD). Int. J. Cardiol. 2015, 195, 326–333. [Google Scholar] [CrossRef] [PubMed]
- Moons, P.; Meijboom, F.J.; Baumgartner, H.; Trindade, P.T.; Huyghe, E.; Kaemmerer, H.; ESC Working Group on Grown-up Congenital Heart Disease. Structure and activities of adult congenital heart disease programmes in Europe. Eur. Heart J. 2010, 31, 1305–1310. [Google Scholar] [CrossRef] [Green Version]
- Baumgartner, H.; De Backer, J.; Babu-Narayan, S.V.; Budts, W.; Chessa, M.; Diller, G.P.; Lung, B.; Kluin, J.; Lang, I.M.; Meijboom, F.; et al. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur. Heart J. 2021, 42, 563–645. [Google Scholar] [CrossRef]
- Stout, K.K.; Daniels, C.J.; Aboulhosn, J.A.; Bozkurt, B.; Broberg, C.S.; Colman, J.M.; Crumb, S.R.; Dearani, J.A.; Fuller, S.; Gurvitz, M.; et al. 2018 AHA/ACC guideline for the management of adults with congenital heart disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2019, 73, e81–e192. [Google Scholar] [CrossRef]
- Yu, C.; Moore, B.M.; Kotchetkova, I.; Cordina, R.L.; Celermajer, D.S. Causes of death in a contemporary adult congenital heart disease cohort. Heart 2018, 104, 1678–1682. [Google Scholar] [CrossRef]
- Neidenbach, R.; Achenbach, S.; Andonian, C.; Beckmann, J.; Biber, S.; Dittrich, S.; Ewert, P.; Freilinger, S.; Huntgeburth, M.; Nagdyman, N.; et al. Medizinische Versorgung von Erwachsenen mit angeborenen Herzfehlern: Gegenwart und Zukunft [Medical care of adults with congenital heart diseases: Present and future]. Herz 2019, 44, 553–572. [Google Scholar] [CrossRef]
- Deutsche Herzstiftung e., V. (Hrsg.): 30. Deutscher Herzbericht 2018; Deutsche Herzstiftung e. V.: Frankfurt, Germany, 2018; 252p, ISBN 978-3-9817032-7-6. [Google Scholar]
- Seidel, L.; Nebel, K.; Achenbach, S.; Bauer, U.; Ewert, P.; Freilinger, S.; Gundlach, U.; Kaemmerer, H.; Nagdyman, N.; Oberhoffer, R.; et al. Facts about the General Medical Care of Adults with Congenital Heart Defects: Experience of a Tertiary Care Center. J. Clin. Med. 2020, 9, 1943. [Google Scholar] [CrossRef]
- Wray, J.; Frigiola, A.; Bull, C.; Adult Congenital Heart Disease Research Network (ACoRN). Loss to specialist follow-up in congenital heart disease; out of sight, out of mind. Heart 2013, 99, 485–490. [Google Scholar] [CrossRef] [Green Version]
- Sable, C.; Foster, E.; Uzark, K.; Bjornsen, K.; Canobbio, M.M.; Connolly, H.M.; Graham, T.P.; Gurvitz, M.Z.; Kovacs, A.; Meadows, A.K.; et al. Best practices in managing transition to adulthood for adolescents with congenital heart disease: The transition process and medical and psychosocial issues: A scientific statement from the American Heart Association. Circulation 2011, 123, 1454–1485. [Google Scholar] [CrossRef] [Green Version]
- Goossens, E.; Bovijn, L.; Gewillig, M.; Budts, W.; Moons, P. Predictors of care gaps in adolescents with complex chronic condition transitioning to adulthood. Pediatrics 2016, 137, e20152413. [Google Scholar] [CrossRef] [Green Version]
- Kollengode, M.S.; Daniels, C.J.; Zaidi, A.N. Loss of follow-up in transition to adult CHD: A single-centre experience. Cardiol. Young 2018, 28, 1001–1008. [Google Scholar] [CrossRef]
- Iversen, K.; Vejlstrup, N.G.; Sondergaard, L.; Nielsen, O.W. Screening of adults with congenital cardiac disease lost for follow-up. Cardiol. Young 2007, 17, 601–608. [Google Scholar] [CrossRef]
- Yeung, E.; Kay, J.; Roosevelt, G.E.; Brandon, M.; Yetman, A.T. Lapse of care as a predictor for morbidity in adults with congenital heart disease. Int. J. Cardiol. 2008, 125, 62–65. [Google Scholar] [CrossRef]
- Baumgartner, H.; Budts, W.; Chessa, M.; Deanfield, J.; Eicken, A.; Holm, J.; Iserin, L.; Meijboom, F.; Stein, J.; Szatmari, A.; et al. Recommendations for organization of care for adults with congenital heart disease and for training in the subspecialty of ‘Grown-up Congenital Heart Disease’ in Europe: A position paper of the Working Group on Grown-up Congenital Heart Disease of the European Society of Cardiology. Eur. Heart J. 2014, 35, 686–690. [Google Scholar] [PubMed] [Green Version]
- Moons, P.; Hilderson, D.; Van Deyk, K. Implementation of transition programs can prevent another lost generation of patients with congenital heart disease. Eur. J. Cardiovasc. Nurs. 2008, 7, 259–263. [Google Scholar] [CrossRef] [PubMed]
- Acuña Mora, M.; Sparud-Lundin, C.; Bratt., E.-L.; Moons, P. Person centred transition programme to empower adolescents with congenital heart disease in the transition to adulthood: A study protocol for a hybrid randomised controlled trial (stepstones project). BMJ Open 2017, 7, e014593. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernandes, S.M.; Verstappen, A.; Clair, M.; Rummell, M.; Barber, D.; Ackerman, K.; Dummer, K.; Mares, J.C.; Cannobio, M.M.; Reardon, L.C.; et al. Knowledge of life-long cardiac care by adolescents and young adults with congenital heart disease. Pediatr. Cardiol. 2019, 40, 1439–1444. [Google Scholar] [CrossRef] [PubMed]
- Van Deyk, K.; Pelgrims, E.; Troost, E.; Goossens, E.; Budts, W.; Gewillig, M.; Moons, P. Adolescents’ understanding of their congenital heart disease on transfer to adult-focused care. Am. J. Cardiol. 2010, 106, 1803–1807. [Google Scholar] [CrossRef] [PubMed]
- Flocco, S.F.; Dellafore, F.; Caruso, R.; Giamberti, A.; Micheletti, A.; Negura, D.G.; Piazza, L.; Carminati, M.; Chessa, M. Improving health perception through a transition care model for adolescents with congenital heart disease. J. Cardiovasc. Med. 2019, 20, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Acuna Mora, M.; Saarijarvi, M.; Moons, P.; Sparud-Lundin, C.; Bratt, E.L.; Goossens, E. The scope of research on transfer and transition in young persons with chronic conditions. J. Adolesc. Health 2019, 65, 581–589. [Google Scholar] [CrossRef] [PubMed]
- Moons, P.; Skogby, S.; Bratt, E.L.; Zühlke, L.; Marelli, A.; Goossens, E. Discontinuity of Cardiac Follow-Up in Young People With Congenital Heart Disease Transitioning to Adulthood: A Systematic Review and Meta-Analysis. J. Am. Heart Assoc. 2021, 10, e019552. [Google Scholar] [CrossRef]
- Bassareo, P.P.; Melis, M.R.; Marras, S.; Calcaterra, G. Learning from the past in the COVID-19 era: Rediscovery of quarantine, previous pandemics, origin of hospitals and national healthcare systems, and ethics in medicine. Postgrad Med. J. 2020, 96, 633–638. [Google Scholar] [CrossRef]
- Salciccioli, K.B.; Oluyomi, A.; Lupo, P.J.; Ermis, P.R.; Lopez, K.N. A model for geographic and sociodemographic access to care disparities for adults with congenital heart disease. Congenit. Heart Dis. 2019, 14, 752–759. [Google Scholar] [CrossRef]
- Caruana, M.; Aquilina, O.; Grech, V. Can the inevitable be prevented?—An analysis of loss to follow-up among grown-ups with congenital heart disease in Malta. Malta Med. J. 2018, 30, 13–21. [Google Scholar]
- Goossens, E.; Stephani, I.; Hilderson, D.; Gewillig, M.; Budts, W.; Van Deyk, K.; Moons, P.; SWITCH(2) Investigators. Transfer of adolescents with congenital heart disease from pediatric cardiology to adult health care: An analysis of transfer destinations. J. Am. Coll. Cardiol. 2011, 57, 2368–2374. [Google Scholar] [CrossRef] [Green Version]
- Mackie, A.S.; Ionescu-Ittu, R.; Therrien, J.; Pilote, L.; Abrahamowicz, M.; Marelli, A.J. Children and adults with congenital heart disease lost to follow-up: Who and when? Circulation 2009, 120, 302–309. [Google Scholar] [CrossRef] [Green Version]
- Winter, M.M.; Mulder, B.J.; van der Velde, E.T. Children and adults with congenital heart disease lost to follow-up: Who and when? Circulation 2010, 121, e252. [Google Scholar] [CrossRef] [Green Version]
- Mercuro, G.; Bassareo, P.P.; Mariucci, E.; Deidda, M.; Zedda, A.M.; Bonvicini, M. Sex differences in congenital heart defects and genetically induced arrhythmias. J. Cardiovasc. Med. 2014, 15, 855–863. [Google Scholar] [CrossRef] [PubMed]
- Skogby, S.; Moons, P.; Johansson, B.; Sunnegårdh, J.; Christersson, C.; Nagy, E.; Winberg, P.; Hanséus, K.; Trzebiatowska-Krzynska, A.; Fadl, S.; et al. Outpatient volumes and medical staffing resources as predictors for continuity of follow-up care during transfer of adolescents with congenital heart disease. Int. J. Cardiol. 2020, 310, 51–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coats, L.; Chaudhry, B. Ambulatory Care in Adult Congenital Heart Disease-Time for Change? J. Clin. Med. 2022, 11, 2058. [Google Scholar] [CrossRef] [PubMed]
- Vaikunth, S.S.; Williams, R.G.; Uzunyan, M.Y.; Tun, H.; Barton, C.; Chang, P.M. Short-term outcomes following implementation of a dedicated young adult congenital heart disease transition program. Congenit. Heart Dis. 2018, 13, 85–91. [Google Scholar] [CrossRef]
- Goossens, E.; Fernandes, S.M.; Landzberg, M.J.; Moons, P. Implementation of the American College of Cardiology/American Heart Association 2008 guidelines for the management of adults with congenital heart disease. Am. J. Cardiol. 2015, 116, 452–457. [Google Scholar] [CrossRef]
- Reid, G.J.; Irvine, M.J.; McCrindle, B.W.; Sananes, R.; Ritvo, P.G.; Siu, S.C.; Webb, G.D. Prevalence and correlates of successful transfer from pediatric to adult health care among a cohort of young adults with complex congenital heart defects. Pediatrics 2004, 113, e197–e205. [Google Scholar] [CrossRef] [Green Version]
- Mackie, A.S.; Rempel, G.R.; Kovacs, A.H.; Kaufman, M.; Rankin, K.N.; Jelen, A.; Yaskina, M.; Sananes, R.; Oechslin, E.; Dragieva, D.; et al. Transition intervention for adolescents with congenital heart disease. J. Am. Coll. Cardiol. 2018, 71, 1768–1777. [Google Scholar] [CrossRef]
- Mondal, T.K.; Muddaluru, V.; Jaafar, A.; Gupta-Bhatnagar, S.; Greville, L.J.; Gorter, J.W. Transition of adolescents with congenital heart disease from pediatric to adult congenital cardiac care: Lessons from a retrospective cohort study. J. Trans. Med. 2020, 2, 20190003. [Google Scholar] [CrossRef]
- Dickinson, C.; Kotchetkova, I.; Nicholson, C.; Osborne, D.; Chard, R.; Celermajer, D.; Cordina, R. Loss to specialised cardiology follow-up in adults living with congenital heart disease. Heart Lung Circ. 2020, 29 (Suppl. 2), S57–S58. [Google Scholar] [CrossRef]
- Bassareo, P.P.; Tumbarello, R.; Piras, A.; Mercuro, G. Evaluation of regional myocardial function by Doppler tissue imaging in univentricular heart after successful Fontan repair. Echocardiography 2010, 27, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Serfas, J.D.; Spates, T.; D’Ottavio, A.; Spears, T.; Ciociola, E.; Chiswell, K.; Davidson-Ray, L.; Ryan, G.; Forestieri, N.; Krasuski, R.A.; et al. Disparities in Loss to Follow-Up Among Adults with Congenital Heart Disease in North Carolina. World J. Pediatr. Congenit. Heart Surg. 2022, 13, 707–715. [Google Scholar] [CrossRef] [PubMed]
- Kaemmerer, H.; Fratz, S.; Bauer, U.; Oechslin, E.; Brodherr-Heberlein, S.; Zrenner, B.; Turina, J.; Jenni, R.; Lange, P.E.; Hess, J. Emergency hospital admissions and three-year survival of adults with and without cardiovascular surgery for congenital cardiac disease. J. Thorac. Cardiovasc. Surg. 2003, 126, 1048–1052. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mylotte, D.; Pilote, L.; Ionescu-Ittu, R.; Abrahamowicz, M.; Khairy, P.; Therrien, J.; Mackie, A.S.; Marelli, A. Specialized adult congenital heart disease care: The impact of policy on mortality. Circulation 2014, 129, 1804–1812. [Google Scholar] [CrossRef] [Green Version]
- Davey, B.; Sinha, R.; Lee, J.H.; Gauthier, M.; Flores, G. Social determinants of health and outcomes for children and adults with congenital heart disease: A systematic review. Pediatr. Res. 2021, 89, 275–294. [Google Scholar] [CrossRef]
- Calcaterra, G.; Bassareo, P.P.; Barilla, F.; Romeo, F.; de Gregorio, C.; Mehta, P.; Mehta, J.L. Syndemic: A Synergistic Anthropological Approach to the COVID-19 Pandemic. Encyclopedia 2022, 2, 90. [Google Scholar] [CrossRef]
- Clarizia, N.A.; Chahal, N.; Manlhiot, C.; Kilburn, J.; Redington, A.N.; McCrindle, B.W. Transition to adult health care for adolescents and young adults with congenital heart disease: Perspectives of the patient, parent and health care provider. Can. J. Cardiol. 2009, 25, e317–e322. [Google Scholar] [CrossRef] [Green Version]
- Habibi, H.; Emmanuel, Y.; Chung, N. Process of Transition for Congenital Heart Patients: Preventing Loss to Follow-up. Clin. Nurse Spec. 2017, 31, 329–334. [Google Scholar] [CrossRef]
- Strijbosch, A.M.; Zwart, R.; Blom, N.A.; Bouma, B.J.; Groenink, M.; Boekholdt, S.M.; de Winter, R.; Mulder, B.J.; Backx, A.P. Transition from paediatric to adult care of adolescent patients with congenital heart disease: A pathway to optimal care. Neth. Heart J. 2016, 24, 682–690. [Google Scholar] [CrossRef] [Green Version]
- Heery, E.; Sheehan, A.M.; While, A.E.; Coyne, I. Experiences and Outcomes of Transition from Pediatric to Adult Health Care Services for Young People with Congenital Heart Disease: A Systematic Review. Congenit. Heart Dis. 2015, 10, 413–427. [Google Scholar] [CrossRef]
- Knauth Meadows, A.; Bosco, V.; Tong, E.; Fernandes, S.; Saidi, A. Transition and transfer from pediatric to adult care of young adults with complex congenital heart disease. Curr. Cardiol. Rep. 2009, 11, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Moons, P.; Meijboom, F.J. Healthcare provision for adults with congenital heart disease in Europe: A review. Curr. Opin. Pediatr. 2010, 22, 573–578. [Google Scholar] [CrossRef] [PubMed]
- Bassareo, P.P.; Mcmahon, C.J.; Prendiville, T.; James, A.; Roberts, P.; Oslizlok, P.; Walsh, M.A.; Kenny, D.; Walsh, K.P. Planning Transition of Care for Adolescents Affected by Congenital Heart Disease: The Irish National Pathway. Pediatr. Cardiol. 2023, 44, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Blum, R.W.; Garell, D.; Hodgman, C.H.; Jorissen, T.W.; Okinow, N.A.; Orr, D.P.; Slap, G.P. Transition from child-centered to adult healthcare systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. J. Adolesc. Health 1993, 14, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Chessa, M.; Tutarel, O. Adults with congenital heart disease—We need more Europe for a better care. Eur. J. Heart Fail. 2021, 23, 454–455. [Google Scholar] [CrossRef]
- King, B.J.; Gilmore-Bykovskyi, A.L.; Roiland, R.A.; Polnaszek, B.E.; Bowers, B.J.; Kind, A.J. The consequences of poor communication during transitions from hospital to skilled nursing facility: A qualitative study. J. Am. Geriatr. Soc. 2013, 61, 1095–1102. [Google Scholar] [CrossRef] [Green Version]
- Harrison, D.J.; Uzark, K.; Gauvreau, K.; Yu, S.; Lowery, R.; Yetman, A.T.; Cramer, J.; Rudd, N.; Cohen, S.; Gurvitz, M. Transition readiness in congenital heart disease: Are teens and young adults getting the recommended information? Int. J. Cardiol. Congenit. Heart Dis. 2022, 7, 100311. [Google Scholar] [CrossRef]
- Uzark, K.; Yu, S.; Lowery, R.; Afton, K.; Yetman, A.T.; Cramer, J.; Rudd, N.; Cohen, S.; Gongwer, R.; Gurvitz, M. Transition Readiness in Teens and Young Adults with Congenital Heart Disease: Can We Make a Difference? J. Pediatr. 2020, 221, 201–206.e1. [Google Scholar] [CrossRef]
- Schoormans, D.; Sprangers, M.A.; Mulder, B.J. Future challenges in providing appropriate care for adults with congenital heart disease. Int. J. Cardiol. 2013, 168, 3115–3116. [Google Scholar] [CrossRef]
- Amin, K.; Patel, K. Role of Psychologists in Pediatric Congenital Heart Disease. Pediatr. Clin. N. Am. 2022, 69, 865–878. [Google Scholar] [CrossRef]
- Lopez, K.N.; O’Connor, M.; King, J.; Alexander, J.; Challman, M.; Lovick, D.K.; Goodly, N.; Smith, A.; Fawcett, E.; Mulligan, C.; et al. Improving Transitions of Care for Young Adults with Congenital Heart Disease: Mobile App Development Using Formative Research. JMIR Form. Res. 2018, 2, e16. [Google Scholar] [CrossRef] [PubMed]
- Applebaum, M.A.; Lawson, E.F.; von Scheven, E. Perception of transition readiness and preferences for use of technology in transition programs: Teens’ ideas for the future. Int. J. Adolesc. Med. Health 2013, 25, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Lopez, M.H.; Gonzales-Barrera, A.; Patten, E. Closing the Digital Divide: Latinos and Technology Adoption; Pew Internet and American Life Project: Washington, DC, USA, 2013; Available online: http://assets.pewresearch.org/wpcontent/uploads/sites/7/2013/03/Latinos_Social_Media_and_Mobile_Tech_03-2013_final.pdf (accessed on 27 December 2022).
- Smith, A. African Americans and Technology Use; Pew Internet and American Life Project: Washington, DC, USA. Available online: http://assets.pewresearch.org/wp-content/uploads/sites/14/2014/01/African-Americans-and-Technology-Use.pdf (accessed on 27 December 2022).
- NORC at the University of Chicago. New Survey: Snapchat and Instagram Are Most Popular Social Media Platforms among American Teens: Black Teens Are the Most Active on Social Media and Messaging Apps. 2017. Available online: https://www.sciencedaily.com/releases/2017/04/170421113306.htm (accessed on 27 December 2022).
- Pai, A.; Ostendorf, H/M. Treatment adherence in adolescents and young adults affected by chronic illness during the health care transition from pediatric to adult health care: A literature review. Child Health Care 2011, 40, 16–33. [Google Scholar] [CrossRef]
- Diallo, A.O.; Krishnaswamy, A.; Shapira, S.K.; Oster, M.E.; George, M.G.; Adams, J.C.; Walker, E.R.; Weiss, P.; Ali, M.K.; Book, W. Detecting moderate or complex congenital heart defects in adults from an electronic health records system. J. Am. Med. Inform. Assoc. 2018, 25, 1634–1642. [Google Scholar] [CrossRef] [PubMed]
- John, A.S.; Jackson, J.L.; Moons, P.; Uzark, K.; Mackie, A.S.; Timmins, S.; Lopez, K.N.; Kovacs, A.H.; Gurvitz, M.; American Heart Association Adults with congenital Heart Disease Committee of the Council on Lifelong congenital Heart Disease and Heart Health in the Young and the Council on Clinical Cardiology; et al. Advances in Managing Transition to Adulthood for Adolescents with Congenital Heart Disease: A Practical Approach to Transition Program Design: A Scientific Statement from the American Heart Association. J. Am. Heart Assoc. 2022, 11, e025278. [Google Scholar] [CrossRef] [PubMed]
- Saarijarvi, M.; Wallin, L.; Moons, P.; Gyllensten, H.; Bratt, E.L. Transition program for adolescents with congenital heart disease in transition to adulthood: Protocol for a mixed-method process evaluation study (the STEPSTONES project). BMJ Open 2019, 9, e028229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Acuna Mora, M.; Saarijarvi, M.; Sparud-Lundin, C.; Moons, P.; Bratt, E.L. Empowering young persons with congenital heart disease: Using intervention mapping to develop a transition program—The STEPSTONES project. J. Pediatr. Nurs. 2020, 50, e8–e17. [Google Scholar] [CrossRef] [PubMed]
- Werner, O.; Abassi, H.; Lavastre, K.; Guillaumont, S.; Picot, M.C.; Serrand, C.; Dulac, Y.; Souletie, N.; Acar, P.; Bredy, C.; et al. Factors influencing the participation of adolescents and young adults with a congenital heart disease in a transition education program: A prospective multicentre controlled study. Patient Educ. Couns. 2019, 102, 2223–2230. [Google Scholar] [CrossRef]
- Bal, M.I.; Sattoe, J.N.; Roelofs, P.D.; Bal, R.; van Staa, A.; Miedema, H.S. Exploring effectiveness and effective components of self-management interventions for young people with chronic physical conditions: A systematic review. Patient Educ. Couns. 2016, 99, 1293–1309. [Google Scholar] [CrossRef] [Green Version]
- Report of the British Cardiac Society Working Party. Grown-up congenital heart (GUCH) disease: Current need and provision of service for adolescents and adults with congenital heart disease in the UK. Chairman Jane Somerville. Heart 2002, 88 (Suppl. 1), i1–i14. [Google Scholar] [CrossRef]
- White, P.H.; Cooley, W.C.; American Academy of Pediatrics; American Academy of Family Physicians; American College of Physicians; Transitions Clinical Report Authoring Group. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics 2018, 142, e20182587. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ravens, E.; Becker, J.; Pape, L.; Ernst, G. Psychosocial benefits and adherence of adolescents with chronic disease participating in transition programs: A systematic review. J. Transit. Med. 2020, 2, 1–10. [Google Scholar] [CrossRef]
- Zhang, L.F.; Ho, J.S.; Kennedy, S.E. A systematic review of the psychometric properties of transition readiness assessment tools in adolescents with chronic disease. BMC Pediatr 2014, 14, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mackie, A.S.; Rempel, G.R.; Kovacs, A.H.; Kaufman, M.; Rankin, K.N.; Jelen, A.; Manlhiot, C.; Anthony, S.J.; Magill-Evans, J.; Nicholas, D.; et al. A cluster randomized trial of a transition intervention for adolescents with congenital heart disease: Rationale and design of the CHAPTER 2 study. BMC Cardiovasc. Disord. 2016, 16, 127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mackie, A.S.; Rempel, G.R.; Islam, S.; Rankin, K.; McCurdy, C.; Vonder Muhll, I.; Magill-Evans, J.; Nicholas, D.; Kovacs, A.H. Psychosocial maturity, autonomy, and transition readiness among young adults with congenital heart disease or a heart transplant. Congenit. Heart Dis. 2016, 11, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Klassen, A.F.; Grant, C.; Barr, R.; Brill, H.; Kraus de Camargo, O.; Ronen, G.M.; Samaan, M.C.; Mondal, T.; Cano, S.J.; Schlatman, A.; et al. Development and validation of a generic scale for use in transition programmes to measure self-management skills in adolescents with chronic health conditions: The TRANSITION-Q. Child Care Health Dev. 2015, 41, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Mackie, A.S.; Rankin, K.; Yaskina, M.; Gingrich, M.; Schuh, M.; Williams, E.; Nicholas, D.; Rempel, G.R. Randomized controlled trial of a transition intervention program for young adolescents with congenital heart disease. Circulation 2019, 140, A12604. [Google Scholar]
- Lesch, W.; Specht, K.; Lux, A.; Frey, M.; Utens, E.; Bauer, U. Disease-specific knowledge and information preferences of young patients with congenital heart disease. Cardiol. Young 2014, 24, 321–330. [Google Scholar] [CrossRef]
- Yang, H.L.; Chen, Y.C.; Wang, J.K.; Gau, B.S.; Chen, C.W.; Moons, P. Measuring knowledge of patients with congenital heart disease and their parents: Validity of the ‘Leuven Knowledge Questionnaire for congenital Heart Disease’. Eur. J. Cardiovasc. Nurs. 2012, 11, 77–84. [Google Scholar] [CrossRef] [Green Version]
- Arozullah, A.M.; Yarnold, P.R.; Bennett, C.L.; Soltysik, R.C.; Wolf, M.S.; Ferreira, R.M.; Lee, S.Y.; Costello, S.; Shakir, A.; Denwood, C.; et al. Development and validation of a short-form, rapid estimate of adult literacy in medicine. Med. Care 2007, 45, 1026–1033. [Google Scholar] [CrossRef]
- Dimopoulos, K.; Opotowsky, A.R.; Constantine, A.; D’Alto, M. Often transferred, rarely transitioned: The current state of transition for young people with congenital heart disease. Int. J. Cardiol. 2021, 329, 89–90. [Google Scholar] [CrossRef] [PubMed]
- Culen, C.; Herle, M.; Ertl, D.A.; Fröhlich-Reiterer, E.; Blümel, P.; Wagner, G.; Häusler, G. Less ready for adulthood?-Turner syndrome has an impact on transition readiness. Clin. Endocrinol. 2020, 93, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]


| Disease Complexity | |
|---|---|
| Simple |
|
| Moderate complexity |
|
| High complexity |
|
| |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bassareo, P.P.; Chessa, M.; Di Salvo, G.; Walsh, K.P.; Mcmahon, C.J. Strategies to Aid Successful Transition of Adolescents with Congenital Heart Disease: A Systematic Review. Children 2023, 10, 423. https://doi.org/10.3390/children10030423
Bassareo PP, Chessa M, Di Salvo G, Walsh KP, Mcmahon CJ. Strategies to Aid Successful Transition of Adolescents with Congenital Heart Disease: A Systematic Review. Children. 2023; 10(3):423. https://doi.org/10.3390/children10030423
Chicago/Turabian StyleBassareo, Pier Paolo, Massimo Chessa, Giovanni Di Salvo, Kevin Patrick Walsh, and Colin Joseph Mcmahon. 2023. "Strategies to Aid Successful Transition of Adolescents with Congenital Heart Disease: A Systematic Review" Children 10, no. 3: 423. https://doi.org/10.3390/children10030423
APA StyleBassareo, P. P., Chessa, M., Di Salvo, G., Walsh, K. P., & Mcmahon, C. J. (2023). Strategies to Aid Successful Transition of Adolescents with Congenital Heart Disease: A Systematic Review. Children, 10(3), 423. https://doi.org/10.3390/children10030423