The Efficacy of a Posterior Approach to Surgical Correction for Neglected Idiopathic Scoliosis: A Comparative Analysis According to Health-Related Quality of Life, Pulmonary Function, Back Pain and Sexual Function
Abstract
1. Introduction
2. Patients and Methods
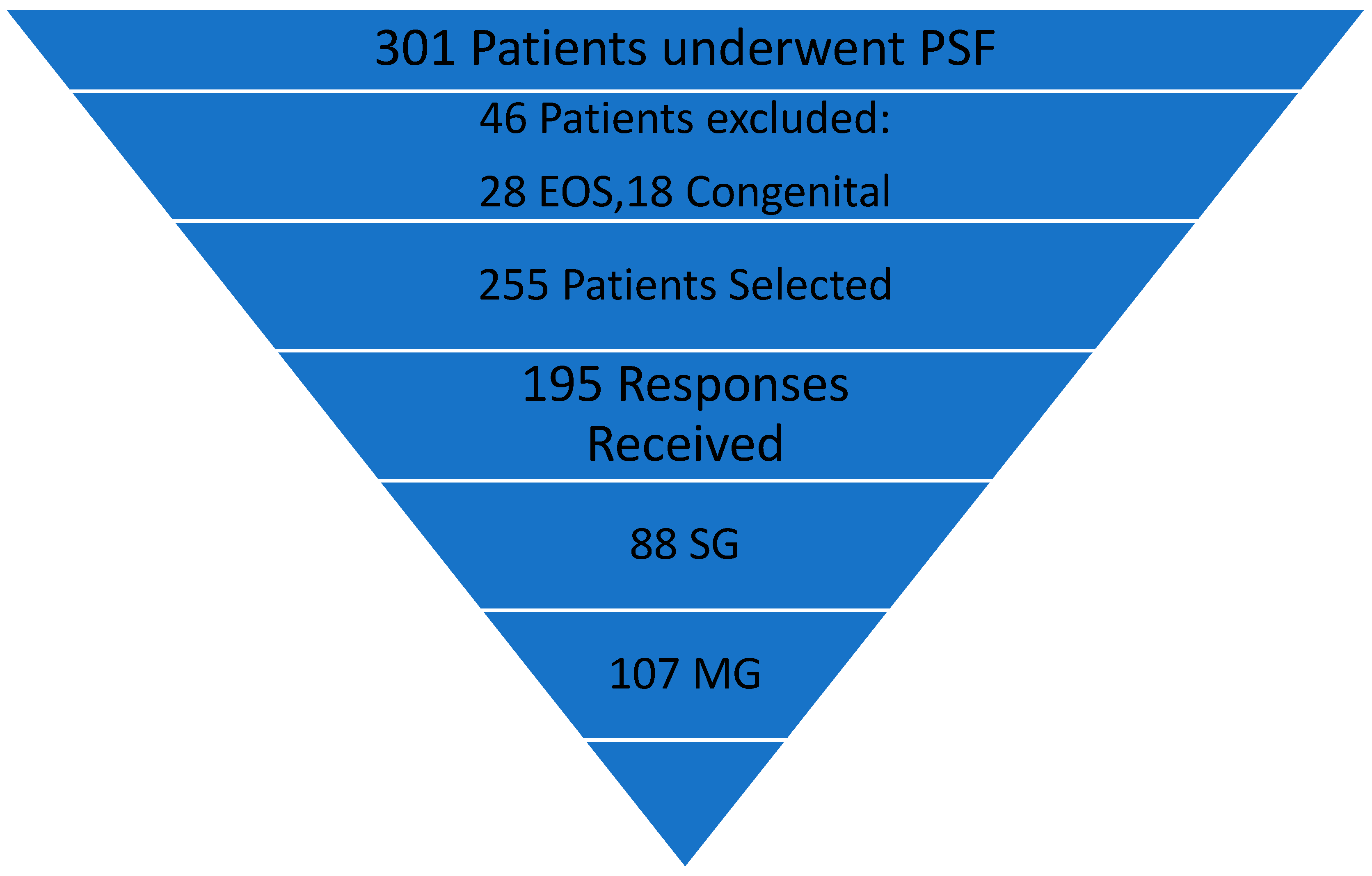
2.1. Setting and Patients
2.2. Outcome Parameters
2.3. Radiographic Parameters
2.4. Statistical Analysis
3. Results
3.1. Clinical Characteristics, Radiographic and PF Outcomes
3.2. HRQoL
3.3. Complications
4. Discussion
4.1. Correction of Spinal Deformity
4.2. Back Pain
4.3. HRQoL, PF, and SF
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hresko, M.T. Clinical practice. Idiopathic scoliosis in adolescents. N. Engl. J. Med. 2013, 368, 834–841. [Google Scholar] [CrossRef] [PubMed]
- Teixeira da Silva, L.E.; de Barros, A.G.; de Azevedo, G.B. Management of severe and rigid idiopathic scoliosis. Eur. J. Orthop. Surg. Traumatol. 2015, 25, S7–S12. [Google Scholar] [CrossRef]
- Suk, S.-I.; Chung, E.-R.; Kim, J.-H.; Kim, S.-S.; Lee, J.-S.; Choi, W.-K. Posterior Vertebral Column Resection for Severe Rigid Scoliosis. Spine 2005, 30, 1682–1687. [Google Scholar] [CrossRef]
- Wang, Y.; Li, C.; Liu, L.; Li, H.; Yi, X. Presurgical Short-Term Halo-Pelvic Traction for Severe Rigid Scoliosis (Cobb Angle > 120°): A 2-Year Follow-up Review of 62 Patients. Spine 2021, 46, E95–E104. [Google Scholar] [CrossRef] [PubMed]
- Garabekyan, T.; Hosseinzadeh, P.; Iwinski, H.J.; Muchow, R.D.; Talwalkar, V.R.; Walker, J.; Milbrandt, T.A. The results of preoperative halo-gravity traction in children with severe spinal deformity. J. Pediatr. Orthop. B 2014, 23, 1–5. [Google Scholar] [CrossRef]
- Boachie-Adjei, O.; Duah, H.O.; Yankey, K.P.; Lenke, L.G.; Sponseller, P.D.; Sucato, D.J.; Samdani, A.F.; Newton, P.O.; Shah, S.A.; Erickson, M.A.; et al. New neurologic deficit and recovery rates in the treatment of complex pediatric spine deformities exceeding 100 degrees or treated by vertebral column resection (VCR). Spine Deform. 2021, 9, 427–433. [Google Scholar] [CrossRef]
- Sponseller, P.D.; Jain, A.; Lenke, L.G.; Shah, S.A.; Sucato, D.J.; Emans, J.B.; Newton, P.O. Vertebral Column Resection in Children with Neuromuscular Spine Deformity. Spine 2012, 37, E655–E661. [Google Scholar] [CrossRef]
- Liu, D.; Yang, J.; Sui, W.; Deng, Y.; Li, F.; Yang, J.; Huang, Z. Efficacy of halo-gravity traction in the perioperative treatment of severe scoliosis and kyphosis: A comparison of adolescent and adult patients. World Neurosurg. 2022, 166, e70–e76. [Google Scholar] [CrossRef]
- Buchowski, J.M.; Bhatnagar, R.; Skaggs, D.L.; Sponseller, P.D. Temporary Internal Distraction as An Aid to Correction of Severe Scoliosis. J. Bone Jt. Surg. 2006, 88, 2035–2041. [Google Scholar] [CrossRef]
- Skaggs, D.L.; Lee, C.; Myung, K.S. Neuromonitoring Changes Are Common and Reversible with Temporary Internal Distraction for Severe Scoliosis. Spine Deform. 2014, 2, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.-M.; Hui, H.; Zhang, H.-P.; Huang, D.-G.; Liu, Z.-K.; Zhao, Y.-T.; He, S.-M.; Zhang, X.-F.; He, B.-R.; Hao, D.-J. The impact of posterior temporary internal distraction on stepwise corrective surgery for extremely severe and rigid scoliosis greater than 130°. Eur. Spine J. 2016, 25, 557–568. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Tao, L.; Hai, Y.; Yang, J.; Zhou, L.; Yin, P.; Pan, A.; Liu, C. One-stage posterior multiple-level asymmetrical ponte osteotomies versus single-level posterior vertebral column resection for severe and rigid adult idiopathic scoliosis: A minimum 2-year follow-up comparative study. Spine 2019, 44, E1196–E1205. [Google Scholar] [CrossRef] [PubMed]
- Koller, H.; Mayer, M.; Koller, J.; Ferraris, L.; Wiedenhöfer, B.; Hitzl, W.; Hempfing, A. Temporary treatment with magnetically controlled growing rod for surgical correction of severe adolescent idiopathic thoracic scoliosis greater than 100°. Eur. Spine J. 2021, 30, 788–796. [Google Scholar] [CrossRef]
- Yang, J.H.; Kim, H.J.; Chang, D.-G.; Suh, S.W.; Nam, Y.; Hong, J.-Y. The Efficacy of Single-Stage Correction by Posterior Approach for Neglected Congenital Scoliosis: Comparative Analysis According to the Age of Surgical Intervention. J. Clin. Med. 2022, 11, 2278. [Google Scholar] [CrossRef]
- Kinel, E.; Korbel, K.; Kozinoga, M.; Czaprowski, D.; Stępniak, Ł.; Kotwicki, T. The Measurement of Health-Related Quality of Life of Girls with Mild to Moderate Idiopathic Scoliosis—Comparison of ISYQOL versus SRS-22 Questionnaire. J. Clin. Med. 2021, 10, 4806. [Google Scholar] [CrossRef] [PubMed]
- Erwin, J.; Carlson, B.B.; Bunch, J.; Jackson, R.S.; Burton, D. Impact of unoperated adolescent idiopathic scoliosis in adulthood: A 10-year analysis. Spine Deform. 2020, 8, 1009–1016. [Google Scholar] [CrossRef]
- Osuka, S.; Sudo, H.; Yamada, K.; Tachi, H.; Watanabe, K.; Sentoku, F.; Chiba, T.; Iwasaki, N.; Mukaino, M.; Tohyama, H. Effects of Posterior Spinal Correction and Fusion on Postural Stability in Patients with Adolescent Idiopathic Scoliosis. J. Clin. Med. 2023, 12, 270. [Google Scholar] [CrossRef] [PubMed]
- Swany, L.; Larson, A.N.; Shah, S.A.; Grabala, P.; Milbrandt, T.; Yaszemski, M.J. Outcomes of pregnancy in operative vs. nonoperative adolescent idiopathic scoliosis patients at mean 30-year follow-up. Spine Deform. 2020, 8, 1169–1174. [Google Scholar] [CrossRef]
- Grabala, P.; Helenius, I.; Shah, S.A.; Larson, A.N.; Buchowski, J.M.; Latalski, M.; Grabala, M.; Guszczyn, T. Impact of Pregnancy on Loss of Deformity Correction After Pedicle Screw Instrumentation for Adolescent Idiopathic Scoliosis. World Neurosurg. 2020, 139, e121–e126. [Google Scholar] [CrossRef] [PubMed]
- Helenius, I.; Lamberg, T.; Österman, K.; Schlenzka, D.; Yrjönen, T.; Tervahartiala, P.; Seitsalo, S.; Poussa, M.; Remes, V. Posterolateral, Anterior, or Circumferential Fusion In Situ for High-Grade Spondylolisthesis in Young Patients: A Long-Term Evaluation Using The Scoliosis Research Society Questionnaire. Spine 2006, 31, 190–196. [Google Scholar] [CrossRef] [PubMed]
- Torén, S.; Diarbakerli, E. Health-related quality of life in adolescents with idiopathic scoliosis: A cross-sectional study including healthy controls. Eur. Spine J. 2022, 31, 3512–3518. [Google Scholar] [CrossRef]
- Soliman, H.A.G. Health-related Quality of Life and Body Image Disturbance of Adolescents with Severe Untreated Idiopathic Early-onset Scoliosis in a Developing Country. Spine 2018, 43, 1566–1571. [Google Scholar] [CrossRef] [PubMed]
- Théroux, J.; Le May, S.; Hebert, J.J.; Labelle, H. Back Pain Prevalence Is Associated with Curve-type and Severity in Adolescents with Idiopathic Scoliosis: A Cross-sectional Study. Spine 2017, 42, E914–E919. [Google Scholar] [CrossRef] [PubMed]
- Helenius, L.; Diarbakerli, E.; Grauers, A.; Lastikka, M.; Oksanen, H.; Pajulo, O.; Löyttyniemi, E.; Manner, T.; Gerdhem, P.; Helenius, I. Back Pain and Quality of Life After Surgical Treatment for Adolescent Idiopathic Scoliosis at 5-Year Follow-up: Comparison with Healthy Controls and Patients with Untreated Idiopathic Scoliosis. J. Bone Jt. Surg. Am. 2019, 101, 1460–1466. [Google Scholar] [CrossRef] [PubMed]
- Suk, S.I.; Lee, C.K.; Kim, W.J.; Chung, Y.J.; Park, Y.B. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine 1995, 20, 1399–1405. [Google Scholar] [CrossRef]
- Lenke, L.G. Lenke classification system of adolescent idiopathic scoliosis: Treatment recommendations. Instr. Course Lect. 2005, 54, 537–542. [Google Scholar] [PubMed]
- Rinella, A.; Lenke, L.; Whitaker, C.; Kim, Y.; Park, S.-S.; Peelle, M.; Edwards, C.; Bridwell, K. Perioperative Halo-Gravity Traction in the Treatment of Severe Scoliosis and Kyphosis. Spine 2005, 30, 475–482. [Google Scholar] [CrossRef]
- Nemani, V.M.; Kim, H.J.; Bjerke-Kroll, B.T.; Yagi, M.; Sacramento-Dominguez, C.; Akoto, H.; Papadopoulos, E.C.; Sanchez-Perez-Grueso, F.; Pellise, F.; Nguyen, J.T.; et al. Preoperative Halo-Gravity Traction for Severe Spinal Deformities at an SRS-GOP Site in West Africa: Protocols, complications, and results. Spine 2015, 40, 153–161. [Google Scholar] [CrossRef]
- Wulff, I.; Duah, H.O.; Tutu, H.O.; Ofori-Amankwah, G.; Yankey, K.P.; Owiredu, M.A.; Yahaya, H.B.; Akoto, H.; Oteng-Yeboah, A.; Boachie-Adjei, O.; et al. Postoperative Pulmonary Complications in Complex Pediatric and Adult Spine Deformity: A Retrospective Review of Consecutive Patients Treated at a Single Site in West Africa. Glob. Spine J. 2020, 11, 1208–1214. [Google Scholar] [CrossRef]
- Hwang, C.J.; Kim, D.G.; Lee, C.S.; Lee, D.-H.; Cho, J.H.; Park, J.-W.; Baik, J.M.; Lee, K.B. Preoperative Halo Traction for Severe Scoliosis. Spine 2020, 45, E1158–E1165. [Google Scholar] [CrossRef] [PubMed]
- Boachie-Adjei, O.; FOCOS Spine Research Group; Sacramento-Dominguez, C.; Ayamga, J.; Sackeyfio, A.; Duah, H.O.; Yankey, K.P.; Akoto, H.; Hodes, R.; Wulff, I.; et al. Characterization of complex vertebral transposition (gamma deformity) > 180 degrees: Clinical and radiographic outcomes of halo gravity traction and vertebral column resection (VCR). Spine Deform. 2021, 9, 411–425. [Google Scholar] [CrossRef]
- Grabala, P.; Helenius, I.J. Clinical and Radiological Outcomes of Less Invasive Temporary Internal Distraction Followed by Staged Pedicle Screw Instrumentation in Adolescents with Severe Idiopathic Scoliosis at 2-Year Minimum Follow-Up. World Neurosurg. 2020, 143, e464–e473. [Google Scholar] [CrossRef]
- Hamzaoglu, A.; Ozturk, C.; Aydogan, M.; Tezer, M.; Aksu, N.; Bruno, M.B. Posterior Only Pedicle Screw Instrumentation with Intraoperative Halo-Femoral Traction in the Surgical Treatment of Severe Scoliosis (>100°). Spine 2008, 33, 979–983. [Google Scholar] [CrossRef]
- Glowacki, M.; Misterska, E.; Laurentowska, M.; Mankowski, P. Polish Adaptation of Scoliosis Research Society-22 Questionnaire. Spine 2009, 34, 1060–1065. [Google Scholar] [CrossRef] [PubMed]
- Nowosielski, K.; Wróbel, B.; Sioma-Markowska, U.; Poręba, R. Sexual Dysfunction and Distress—Development of a Polish Version of the Female Sexual Distress Scale-Revised. J. Sex. Med. 2013, 10, 1304–1312. [Google Scholar] [CrossRef]
- Miekisiak, G.; Kollataj, M.; Dobrogowski, J.; Kloc, W.; Libionka, W.; Banach, M.; Łątka, D.; Sobolewski, T.; Sulewski, A.; Nowakowski, A.; et al. Validation and Cross-Cultural Adaptation of the Polish Version of the Oswestry Disability Index. Spine 2013, 38, E237–E243. [Google Scholar] [CrossRef] [PubMed]
- Golicki, D.; Jakubczyk, M.; Niewada, M.; Wrona, W.; Busschbach, J.J. Valuation of EQ-5D Health States in Poland: First TTO-Based Social Value Set in Central and Eastern Europe. Value Health 2010, 13, 289–297. [Google Scholar] [CrossRef]
- Lao, L.; Weng, X.; Qiu, G.; Shen, J. The role of preoperative pulmonary function tests in the surgical treatment of extremely severe scoliosis. J. Orthop. Surg. Res. 2013, 8, 32. [Google Scholar] [CrossRef]
- Lenke, L.G.; Newton, P.O.; Sucato, D.J.; Shufflebarger, H.L.; Emans, J.B.; Sponseller, P.D.; Shah, S.A.; Sides, B.A.; Blanke, K.M. Complications after 147 consecutive vertebral column resections for severe pediatric spinal deformity: A multicenter analysis. Spine 2013, 38, 119–132. [Google Scholar] [CrossRef] [PubMed]
- Jasiewicz, B.; Potaczek, T.; Szcześniak, A.; Tesiorowski, M. Retrospective study of two-stage surgery in the treatment of scoliosis exceeding 100 degrees—Assessment including spinal balance evaluation. Ortop. Traumatol. Rehabil. 2009, 11, 495–500. [Google Scholar] [PubMed]
- Potaczek, T.; Jasiewicz, B.; Tesiorowski, M.; Zarzycki, D.; Szcześniak, A. Treatment of idiopathic scoliosis exceeding 100 degrees—Comparison of different surgical techniques. Ortop. Traumatol. Rehabil. 2009, 11, 485–494. [Google Scholar]
- Lenke, L.G.; Sides, B.A.; Koester, L.A.; Hensley, M.; Blanke, K.M. Vertebral Column Resection for the Treatment of Severe Spinal Deformity. Clin. Orthop. Relat. Res. 2010, 468, 687–699. [Google Scholar] [CrossRef]
- Di Silvestre, M.; Zanirato, A.; Greggi, T.; Scarale, A.; Formica, M.; Vallerga, D.; Legrenzi, S.; Felli, L. Severe adolescent idiopathic scoliosis: Posterior staged correction using a temporary magnetically-controlled growing rod. Eur. Spine J. 2020, 29, 2046–2053. [Google Scholar] [CrossRef]
- Ding, R.; Liang, J.; Qiu, G.; Shen, J.; Li, Z. Evaluation of quality of life in adolescent idiopathic scoliosis with different distal fusion level: A comparison of L3 versus L4. Clin. Spine Surg. 2014, 27, E155–E161. [Google Scholar] [CrossRef] [PubMed]
- Enercan, M.; Kahraman, S.; Yilar, S.; Cobanoglu, M.; Gokcen, B.H.; Karadereler, S.; Mutlu, A.; Ulusoy, L.O.; Ozturk, C.; Erturer, E.; et al. Does It Make a Difference to Stop Fusion at L3 Versus L4 in Terms of Disc and Facet Joint Degeneration: An MRI Study with Minimum 5 Years Follow-up. Spine Deform. 2016, 4, 237–244. [Google Scholar] [CrossRef]
- Akazawa, T.; Kotani, T.; Sakuma, T.; Minami, S.; Orita, S.; Fujimoto, K.; Shiga, Y.; Takaso, M.; Inoue, G.; Miyagi, M.; et al. Spinal fusion on adolescent idiopathic scoliosis patients with the level of L4 or lower can increase lumbar disc degeneration with sagittal imbalance 35 years after surgery. Spine Surg. Relat. Res. 2017, 1, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, N.; Johnston, C.E.; Browne, R.H. The Prevalence of Back Pain in Children Who Have Idiopathic Scoliosis. J. Bone Jt. Surg. 1997, 79, 364–368. [Google Scholar] [CrossRef] [PubMed]
- Sieberg, C.B.; Simons, L.E.; Edelstein, M.R.; DeAngelis, M.R.; Pielech, M.; Sethna, N.; Hresko, M.T. Pain Prevalence and Trajectories Following Pediatric Spinal Fusion Surgery. J. Pain 2013, 14, 1694–1702. [Google Scholar] [CrossRef] [PubMed]
- Voepel-Lewis, T.; Caird, M.S.; Tait, A.R.; Malviya, S.; Farley, F.A.; Li, Y.; Abbott, M.D.; van Veen, T.; Hassett, A.L.; Clauw, D.J. A High Preoperative Pain and Symptom Profile Predicts Worse Pain Outcomes for Children After Spine Fusion Surgery. Anesth. Analg. 2017, 124, 1594–1602. [Google Scholar] [CrossRef]
- Upasani, V.V.; Caltoum, C.; Petcharaporn, M.; Bastrom, T.P.; Pawelek, J.B.; Betz, R.R.; Clements, D.H.; Lenke, L.G.; Lowe, T.G.; Newton, P.O. Adolescent Idiopathic Scoliosis Patients Report Increased Pain at Five Years Compared with Two Years after Surgical Treatment. Spine 2008, 33, 1107–1112. [Google Scholar] [CrossRef]
- Sato, T.; Hirano, T.; Ito, T.; Morita, O.; Kikuchi, R.; Endo, N.; Tanabe, N. Back pain in adolescents with idiopathic scoliosis: Epidemiological study for 43,630 pupils in Niigata City, Japan. Eur. Spine J. 2011, 20, 274–279. [Google Scholar] [CrossRef]
- Balagué, F.; Pellisé, F. Adolescent idiopathic scoliosis and back pain. Scoliosis Spinal Disord. 2016, 11, 27. [Google Scholar] [CrossRef]
- Grabala, P.; Helenius, I.; Buchowski, J.M.; Larson, A.N.; Shah, S.A. Back Pain and Outcomes of Pregnancy After Instrumented Spinal Fusion for Adolescent Idiopathic Scoliosis. World Neurosurg. 2019, 124, e404–e410. [Google Scholar] [CrossRef]
- Saraiva, B.M.; Araujo, G.S.; Sperandio, E.F.; Gotfryd, A.O.; Dourado, V.Z.; Vidotto, M.C. Impact of Scoliosis Severity on Functional Capacity in Patients with Adolescent Idiopathic Scoliosis. Pediatr. Exerc. Sci. 2018, 30, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Bumpass, D.B.; Lenke, L.G.; Bridwell, K.H.; Stallbaumer, J.J.; Kim, Y.J.; Wallendorf, M.J.; Min, W.-K.; Sides, B.A. Pulmonary Function Improvement After Vertebral Column Resection for Severe Spinal Deformity. Spine 2014, 39, 587–595. [Google Scholar] [CrossRef]
- Auerbach, J.D.; Lenke, L.G.; Bridwell, K.H.; Sehn, J.K.; Milby, A.H.; Bumpass, D.; Crawford, C.H.; Oʼshaughnessy, B.A.; Buchowski, J.M.; Chang, M.S.; et al. Major Complications and Comparison Between 3-Column Osteotomy Techniques in 105 Consecutive Spinal Deformity Procedures. Spine 2012, 37, 1198–1210. [Google Scholar] [CrossRef]
- Schroeder, J.E.; Michaeli, T.; Luria, M.; Itshayek, E.; Kaplan, L. Long-Term Effects on Sexual Function in Women Treated with Scoliosis Correction for Adolescent Idiopathic Scoliosis. Glob. Spine J. 2022. [Google Scholar] [CrossRef]
- Daniels, A.H.; Reid, D.; Durand, W.; Disilvestro, K.; Hamilton, D.K.; Passias, P.; Kim, H.J.; Protopsaltis, T.; LaFage, V.; Smith, J.S.; et al. Sexual Dysfunction Secondary to Lumbar Stiffness in Adult Spinal Deformity Patients Before and After Long-Segment Spinal Fusion. World Neurosurg. 2020, 139, e474–e479. [Google Scholar] [CrossRef] [PubMed]
- Riley, M.S.; Lenke, L.G.; Chapman, T.M.; Sides, B.A.; Blanke, K.M.; Kelly, M.P. Clinical and Radiographic Outcomes After Posterior Vertebral Column Resection for Severe Spinal Deformity with Five-Year Follow-up. J. Bone Jt. Surg. 2018, 100, 396–405. [Google Scholar] [CrossRef]




| SG (N = 88) | MG (N = 107) | p Value * | |
|---|---|---|---|
| Mean (SD) age at surgery, yrs | 14.3 (2.8) | 15 (2.6) | 0.921 |
| Male | 10 | 14 | |
| Female | 78 | 93 | |
| Mean (SD) follow-up, yrs | 4 (3.5) | 4 (2.5) | 0.922 |
| Mean (SD) BMI, kg/m2 | 19.2 (2.4) | 18.7 (2.2) | 0.671 |
| Mean (SD) preoperative Cobb, deg | 131 (13.8) | 60 (9.5) | <0.001 |
| Mean (SD) Cobb at final follow-up, deg p-value * (pre vs. follow-up) | 61 (19.2) | 18 (9.2) | <0.001 |
| <0.001 | <0.001 | ||
| Mean (SD) preoperative thoracic kyphosis T5-T12, deg | 83 (35.9) | 25 (14.2) | <0.001 |
| Mean (SD) thoracic kyphosis T5-T12 at final follow-up, deg p-value * (pre vs. follow-up) | 35 (9.6) | 22 (8.2) | 0.24 |
| <0.001 | <0.324 | ||
| Mean (SD) preoperative lumbar lordosis T12-S1, deg | −66.1 (10.8) | −52 (11) | 0.329 |
| Mean (SD) lumbar lordosis T12-S1 at final follow-up, deg p-value * (pre vs. follow-up) | −16.8 (8.8) | −18 (12) | 0.897 |
| <0.001 | <0.001 | ||
| Mean (SD) preoperative apical vertebral translation, mm | 92 (32.4) | 65 (14.8) | <0.001 |
| Mean (SD) apical vertebral translation at final follow-up, mm p-value * (pre vs. follow-up) | 31 (9.8) | 22 (6.8) | 0.22 |
| <0.001 | <0.001 | ||
| Mean (SD) preoperative forced vital capacity, percentage of predicted | 51.2 (12.8) | 83 (11.2) | <0.001 |
| Mean (SD) forced vital capacity, percentage of predicted at final follow-up p-value * (pre vs. follow-up) | 69.9 (11.2) | 79 (13.2) | 0.486 |
| <0.001 | 0.12 | ||
| Mean (SD) preoperative forced expiratory volume in one second, percentage of predicted | 60.8 (13.9) | 77 (12.8) | <0.001 |
| Mean (SD) forced expiratory volume in one second, percentage of predicted at final follow-up p-value * (pre vs. follow-up) | 76.9 (14.5) | 81 (12.8) | 0.282 |
| <0.001 | 0.09 | ||
| Mean (SD) preoperative rib hump difference, cm | 8.6 (2.4) | 4.2 (1.9) | <0.001 |
| Mean (SD) rib hump difference, cm, at final follow-up p-value * (pre vs. follow-up) | 2.4 (1.8) | 1.61 (2.1) | 0.682 |
| <0.001 | <0.001 | ||
| Mean (SD) preoperative trunk height difference, cm | 31.8 (2.8) | 29.2 (4.2) | <0.001 |
| Mean (SD) trunk height difference, cm, at final follow-up p-value * (pre vs. follow-up) | 41.8 (3.2) | 38 (3.6) | 0.472 |
| <0.001 | <0.001 | ||
| Mean (SD) number of levels fused | 11 (4.0) | 9 (3.0) | 0.964 |
| Percentage (n) of patients fused below L3 | 41% (41) | NA | 0.543 |
| Halo Gravity Traction (n) | 28 | NA | |
| Halo Gravity Traction, Mean (SD) days of traction | 42 (8) | NA | |
| Temporary Internal Distraction (n) | 35 | NA | |
| Temporary Internal Distraction Mean (SD) time between initial and final surgery, days | 28 (7) | NA | |
| Intraoperative Traction (n) | 25 | NA |
| SRS-22R | SG (N = 88) | MG (N = 107) | ||||
|---|---|---|---|---|---|---|
| Parameter | Preoperative (N = 88) | Final Follow-Up (N = 88) | p-Values * | Preoperative (N = 107) | Final Follow-Up (N = 107) | p-Values * |
| Function | 2.80 (0.82) | 4.42 (0.66) | <0.001 | 4.10 (0.52) | 4.32 (0.52) | 0.309 |
| Pain | 3.22 (0.76) | 3.98 (0.78) | <0.001 | 3.92 (0.55) | 3.98 (0.60) | 0.268 |
| Self-image | 2.86 (0.76) | 4.12 (0.66) | <0.001 | 3.86 (0.52) | 3.96 (0.72) | 0.421 |
| Mental health | 2.68 (0.72) | 4.02 (0.70) | <0.001 | 4.02 (0.72) | 4.12 (0.70) | 0.629 |
| Satisfaction | 2.60 (0.80) | 4.30 (0.60) | <0.001 | 3.80 (0.76) | 4.22 (0.70) | <0.001 |
| Total score | 2.96 (0.82) | 4.36 (0.55) | <0.001 | 3.82 (0.82) | 4.26 (0.75) | <0.001 |
| p-Values * | <0.001 | |||||
| Parameter (Mean) | SG (N = 88) | MG (N = 107) | p-Value |
|---|---|---|---|
| EQ-5D | |||
| Preoperative | 56 (18) | 73 (18) | <0.001 |
| At FFU | 73 (23) | 78 (20) | 0.391 |
| p-Value | <0.001 | 0.12 | |
| VAS score | |||
| Preoperative | 5.9 (2.2) | 5.15 (2.5) | <0.001 |
| At FFU | 2.9 (2.0) | 3.1 (2.2) | <0.001 |
| p-Value | <0.001 | <0.001 | |
| ODI | |||
| Preoperative | 36.4 (18) | 31.4 (16) | <0.001 |
| At FFU | 10.4 (8) | 8.5 (6.2) | 0.29 |
| p-Value | <0.001 | <0.001 | |
| FSDS | |||
| Preoperative | 13.6 (3.8) | 10.2 (2.6) | <0.001 |
| At FFU | 6.8 (3.2) | 4.5 (3.8) | 0.621 |
| p-Value | <0.001 | 0.22 | |
| SRS-22R (total) | |||
| Preoperative | 2.96 (0.82) | 3.82 (0.82) | <0.001 |
| At FFU | 4.36 (0.55) | 4.26 (0.75) | <0.001 |
| p-Value | <0.001 | <0.001 |
| Rate of Complications Following Posterior Final Fusion | SG (N = 88) | MG (N = 107) |
|---|---|---|
| Intraoperative neuromonitoring changes | 5 (5.68%) | 6 (5.6%) |
| Superficial infection | 3 (3.40%) | 5 (4.67%) |
| Pneumonia | 2 (2.27%) | 3 (2.80%) |
| Paresthesia from the lateral cutaneous nerve of the lower limb | 1 (1.13%) | 6 (5.6%) |
| Superior mesenteric artery syndrome | 2 (2.27%) | 0 |
| Deep infection/revision surgery | 2 (2.27%) | 1 (0.93%) |
| Radiculopathy | 1 (1.13%) | 2 (1.86%) |
| Implant failure (broken rod/screws/pull out) | 2 (2.27%) | 1 (0.93%) |
| TOTAL | 17 (19.31%) | 24 (22.42%) |
| Authors | Surgical Technique | Mean Coronal Cobb (Degree) | Mean Cobb Correction (%) |
|---|---|---|---|
| Yu Wang et al. [4] | Halo pelvic traction/posterior fusion | 131.5 | 64.1 |
| Yu Wang et al. [4] | Halo pelvic traction/posterior column resection | 133.6 | 65.4 |
| Skaggs et al. [10] | Temporary internal distraction rods | 113 | 54 |
| Hui-Min Hu et al. [11] | Temporary internal Distraction rods | 148.8 | 63 |
| Zhang et al. [12] | Posterior fusion/Ponte osteotomy | 98.5 | 56.7 |
| Zhang et al. [12] | Posterior vertebral column resection | 108.9 | 49.2 |
| Koller et al. [13] | Temporary treatment with magnetically controlled growing rod for surgical correction of severe adolescent idiopathic thoracic scoliosis greater than 100°. | 118 | 67 |
| Wang et al. [25] | VCR | 108.9 | 66.1 |
| Rinella et al. [27] | Halo-gravity traction | 84 | 59 |
| Nemani et al. [28] | Halo-gravity traction | 131 | 56 |
| Hamzaoglu et al. [33] | Halo-gravity traction and PSF | 122 | 51 |
| Lenke et al. [39] | VCR | 85 | 51 |
| Jasiewicz et al. [40] | Anterior release, cranio-femoral traction, and PSF | 129 | 44 |
| Potaczek T et al. [41] | Halo-femoral traction with PSF, anterior release with halo-femoral traction, and PSF | 125 | 52.7 and 51.7 |
| Lenke et al. [42] | Posterior vertebral column resection | 85 | 69 |
| Di Silvestre et al. [43] | Severe adolescent idiopathic scoliosis: posterior staged correction using a temporary magnetically controlled growing rod. | 98.2 | 59 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grabala, P.; Helenius, I.J.; Buchowski, J.M.; Shah, S.A. The Efficacy of a Posterior Approach to Surgical Correction for Neglected Idiopathic Scoliosis: A Comparative Analysis According to Health-Related Quality of Life, Pulmonary Function, Back Pain and Sexual Function. Children 2023, 10, 299. https://doi.org/10.3390/children10020299
Grabala P, Helenius IJ, Buchowski JM, Shah SA. The Efficacy of a Posterior Approach to Surgical Correction for Neglected Idiopathic Scoliosis: A Comparative Analysis According to Health-Related Quality of Life, Pulmonary Function, Back Pain and Sexual Function. Children. 2023; 10(2):299. https://doi.org/10.3390/children10020299
Chicago/Turabian StyleGrabala, Pawel, Ilkka J. Helenius, Jacob M. Buchowski, and Suken A. Shah. 2023. "The Efficacy of a Posterior Approach to Surgical Correction for Neglected Idiopathic Scoliosis: A Comparative Analysis According to Health-Related Quality of Life, Pulmonary Function, Back Pain and Sexual Function" Children 10, no. 2: 299. https://doi.org/10.3390/children10020299
APA StyleGrabala, P., Helenius, I. J., Buchowski, J. M., & Shah, S. A. (2023). The Efficacy of a Posterior Approach to Surgical Correction for Neglected Idiopathic Scoliosis: A Comparative Analysis According to Health-Related Quality of Life, Pulmonary Function, Back Pain and Sexual Function. Children, 10(2), 299. https://doi.org/10.3390/children10020299







