Vertebral Body Tethering in AIS Management—A Preliminary Report
Abstract
1. Introduction
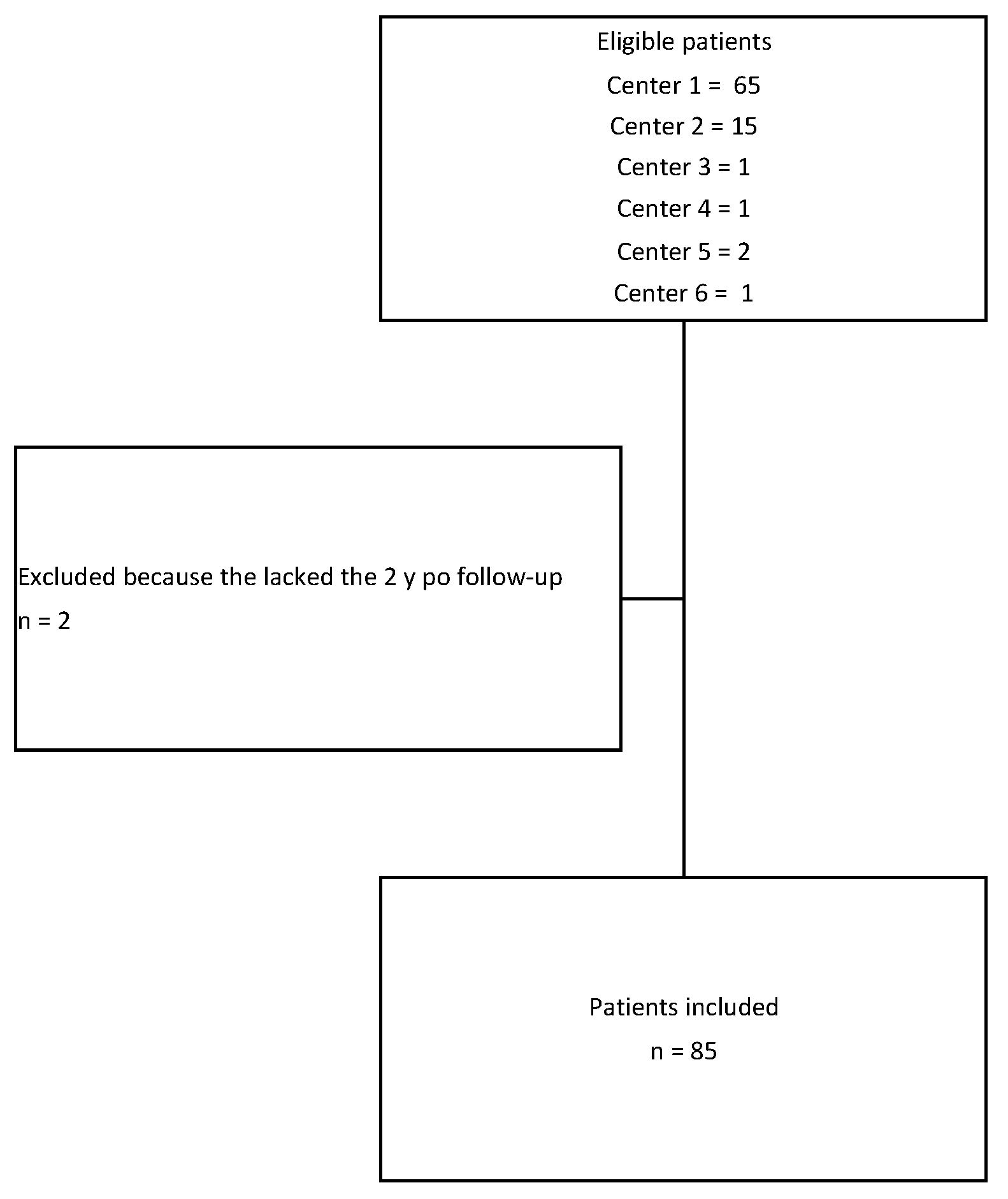
2. Materials and Methods
2.1. Patient Selection
- -
- Diagnosis of idiopathic scoliosis from 9 to 14 years old;
- -
- Severe curve (>40° for thoracic scoliosis/>35° for lumbar scoliosis);
- -
- Skeletal immaturity assessed by a Risser index between 0 and 2;
- -
- Surgical treatment using the “vertebral growth modulation” technique using screws and synthetic tether.
2.2. Surgical Technique
2.2.1. Right Thoracic Curves
2.2.2. Lumbar Curves
2.2.3. Double Curves
2.3. Post-Operative Management
2.4. Outcomes of Interest
2.5. Statistical Analysis
3. Results
3.1. Patient Selection and Demographic Data
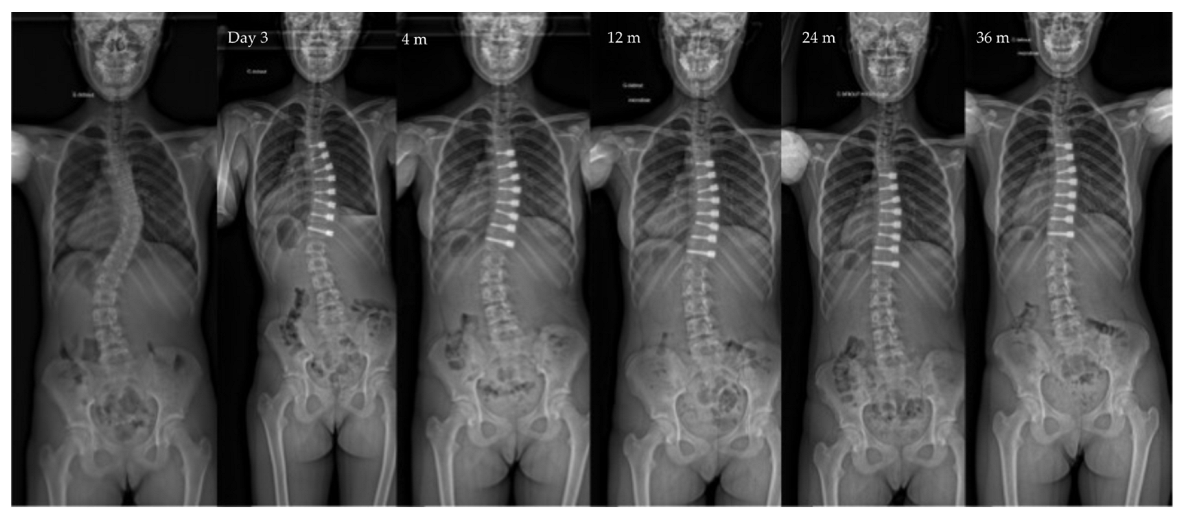
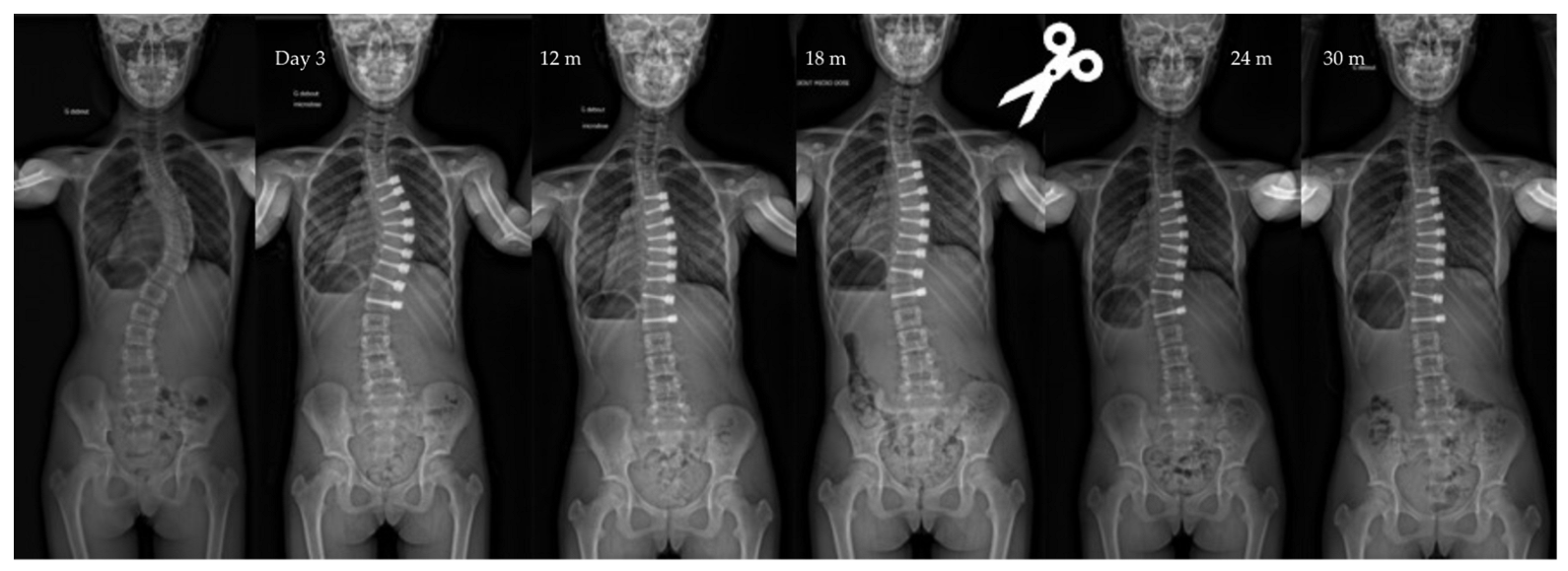
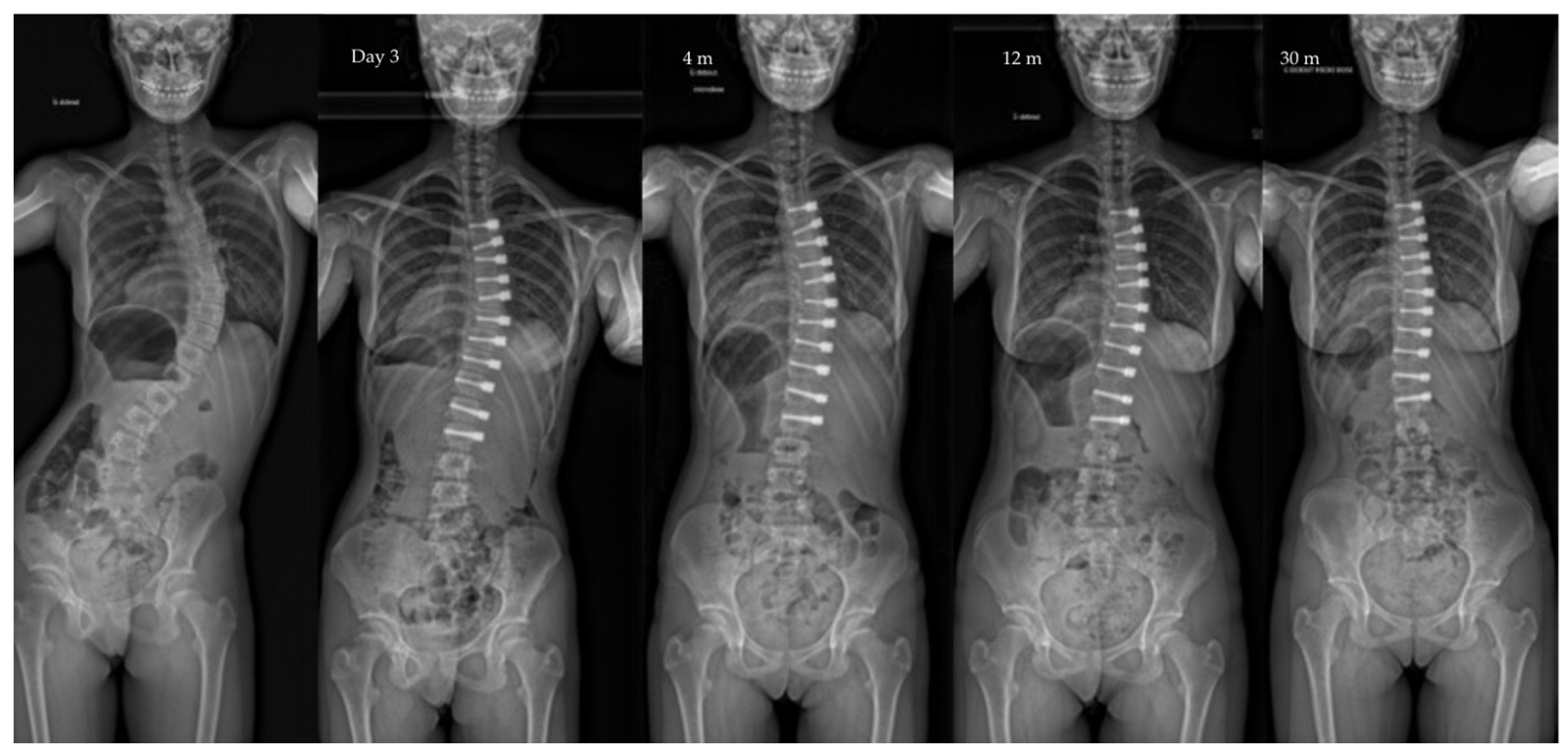
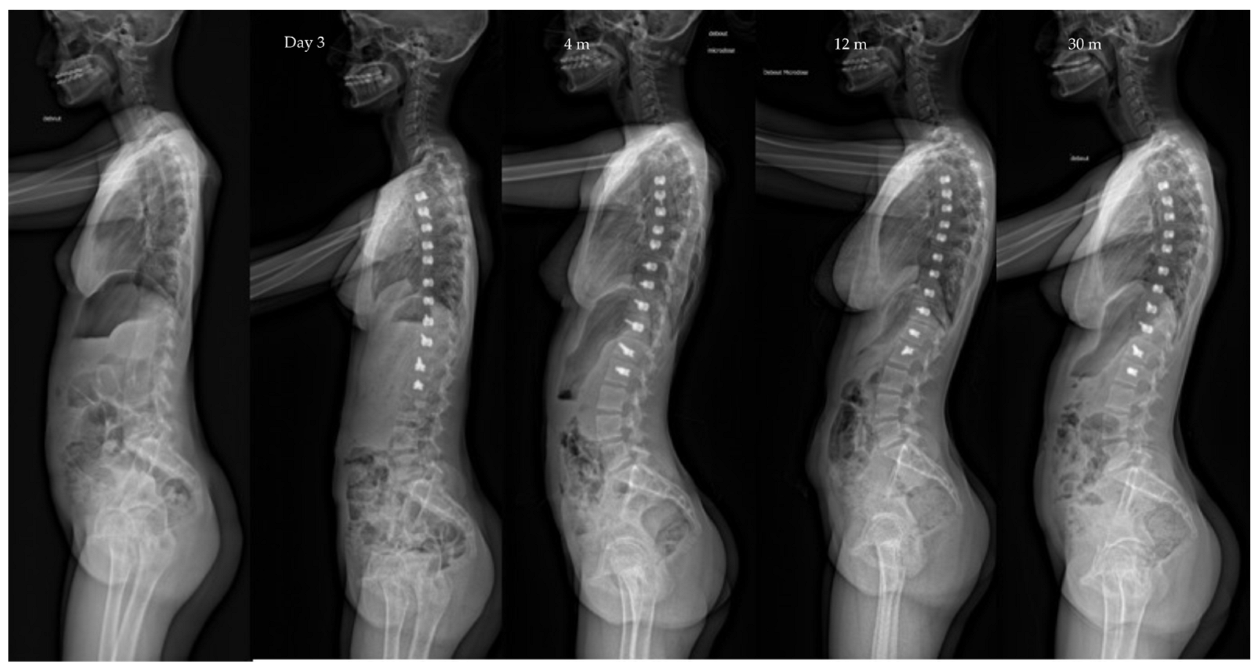
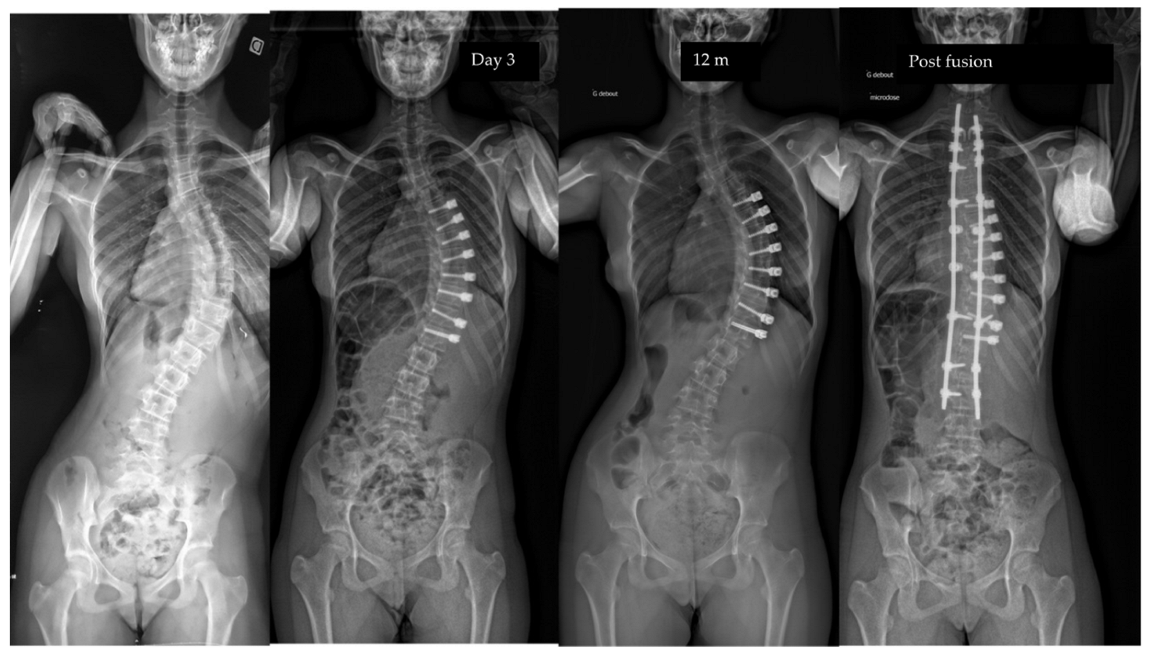
3.2. Radiological Outcome at Last Follow-Up
3.3. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Crawford, C.H., 3rd; Lenke, L.G. Growth modulation by means of anterior tethering resulting in progressive correction of juvenile idiopathic scoliosis: A case report. J. Bone Jt. Surg. 2010, 92, 202–209. [Google Scholar] [CrossRef]
- Parent, S.; Shen, J. Anterior Vertebral Body Growth-Modulation Tethering in Idiopathic Scoliosis: Surgical Technique. J. Am. Acad. Orthop. Surg. 2020, 28, 693–699. [Google Scholar] [CrossRef]
- Newton, P.O.; Kluck, D.G.; Saito, W.; Yaszay, B.; Bartley, C.E.; Bastrom, T.P. Anterior Spinal Growth Tethering for Skeletally Immature Patients with Scoliosis: A Retrospective Look Two to Four Years Postoperatively. J. Bone Jt. Surg. 2018, 100, 1691–1697. [Google Scholar] [CrossRef] [PubMed]
- Samdani, A.F.; Ames, R.J.; Kimball, J.S.; Pahys, J.M.; Grewal, H.; Pelletier, G.J.; Betz, R.R. Anterior vertebral body tethering for immature adolescent idiopathic scoliosis: One-year results on the first 32 patients. Eur. Spine J. 2015, 24, 1533–1539. [Google Scholar] [CrossRef] [PubMed]
- Samdani, A.F.; Ames, R.J.; Kimball, J.S.; Pahys, J.M.; Grewal, H.; Pelletier, G.J.; Betz, R.R. Anterior vertebral body tethering for idiopathic scoliosis: Two-year results. Spine 2014, 39, 1688–1693. [Google Scholar] [CrossRef]
- Mariscal, G.; Morales, J.; Perez, S.; Rubio-Belmar, P.A.; Bovea-Marco, M.; Bas, J.L.; Bas, P.; Bas, T. Meta-analysis on the efficacy and safety of anterior vertebral body tethering in adolescent idiopathic scoliosis. Eur. Spine J. 2022. [Google Scholar] [CrossRef]
- Samdani, A.F.; Pahys, J.M.; Ames, R.J.; Grewal, H.; Pelletier, G.J.; Hwang, S.W.; Betz, R.R. Prospective Follow-up Report on Anterior Vertebral Body Tethering for Idiopathic Scoliosis: Interim Results from an FDA IDE Study. J. Bone Jt. Surg. 2021, 103, 1611–1619. [Google Scholar] [CrossRef]
- Rushton, P.R.P.; Nasto, L.; Parent, S.; Turgeon, I.; Aldebeyan, S.; Miyanji, F. Anterior Vertebral Body Tethering for Treatment of Idiopathic Scoliosis in the Skeletally Immature: Results of 112 Cases. Spine 2021, 46, 1461–1467. [Google Scholar] [CrossRef]
- Lonner, B.; Weiner, D.A.; Miyanji, F.; Hoernschemeyer, D.G.; Eaker, L.; Samdani, A.F. Vertebral Body Tethering: Rationale, Results, and Revision. Instr. Course Lect. 2022, 71, 413–425. [Google Scholar]
- Duarte, M.P.; Aubin, C.E.; Cobetto, N.; Roy-Beaudry, M.; Bellefleur, C.; Turgeon, I.; Labelle, H.; Guy, A.; Barchi, S.; Parent, S. 3D Radiological Outcomes and Quality of Life of Patients with Moderate Idiopathic Scoliosis Treated with Anterior Vertebral Growth Modulation vs Bracing: 2-Year Follow-up. Spine 2022, 47, 1063–1070. [Google Scholar] [CrossRef]
- Bernard, J.; Bishop, T.; Herzog, J.; Haleem, S.; Lupu, C.; Ajayi, B.; Lui, D.F. Dual modality of vertebral body tethering: Anterior scoliosis correction versus growth modulation with mean follow-up of five years. Bone Jt. Open 2022, 3, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, Y.; Saito, W.; Yaszay, B.; Bartley, C.E.; Bastrom, T.P.; Newton, P.O. Rate of Scoliosis Correction After Anterior Spinal Growth Tethering for Idiopathic Scoliosis. J. Bone Jt. Surg. 2021, 103, 1718–1723. [Google Scholar] [CrossRef] [PubMed]
- Pehlivanoglu, T.; Oltulu, I.; Erdag, Y.; Korkmaz, E.; Sarioglu, E.; Ofluoglu, E.; Aydogan, M. Double-sided vertebral body tethering of double adolescent idiopathic scoliosis curves: Radiographic outcomes of the first 13 patients with 2 years of follow-up. Eur. Spine J. 2021, 30, 1896–1904. [Google Scholar] [CrossRef] [PubMed]
- Pehlivanoglu, T.; Oltulu, I.; Erdag, Y.; Akturk, U.D.; Korkmaz, E.; Yildirim, E.; Sarioglu, E.; Ofluoglu, E.; Aydogan, M. Comparison of clinical and functional outcomes of vertebral body tethering to posterior spinal fusion in patients with adolescent idiopathic scoliosis and evaluation of quality of life: Preliminary results. Spine Deform. 2021, 9, 1175–1182. [Google Scholar] [CrossRef]
- Hegde, S.K.; Venkatesan, M.; Akbari, K.K.; Badikillaya, V.M. Efficacy of Anterior Vertebral Body Tethering in Skeletally Mature Children with Adolescent Idiopathic Scoliosis: A Preliminary Report. Int. J. Spine Surg. 2021, 15, 995–1003. [Google Scholar] [CrossRef]
- Baker, C.E.; Milbrandt, T.A.; Larson, A.N. Anterior Vertebral Body Tethering for Adolescent Idiopathic Scoliosis: Early Results and Future Directions. Orthop. Clin. N. Am. 2021, 52, 137–147. [Google Scholar] [CrossRef]
- Baker, C.E.; Kiebzak, G.M.; Neal, K.M. Anterior vertebral body tethering shows mixed results at 2-year follow-up. Spine Deform. 2021, 9, 481–489. [Google Scholar] [CrossRef]
- Pehlivanoglu, T.; Oltulu, I.; Ofluoglu, E.; Sarioglu, E.; Altun, G.; Korkmaz, M.; Yildirim, K.; Aydogan, M. Thoracoscopic Vertebral Body Tethering for Adolescent Idiopathic Scoliosis: A Minimum of 2 Years’ Results of 21 Patients. J. Pediatr. Orthop. 2020, 40, 575–580. [Google Scholar] [CrossRef]
- Newton, P.O.; Bartley, C.E.; Bastrom, T.P.; Kluck, D.G.; Saito, W.; Yaszay, B. Anterior Spinal Growth Modulation in Skeletally Immature Patients with Idiopathic Scoliosis: A Comparison with Posterior Spinal Fusion at 2 to 5 Years Postoperatively. J. Bone Jt. Surg. 2020, 102, 769–777. [Google Scholar] [CrossRef]
- Hoernschemeyer, D.G.; Boeyer, M.E.; Robertson, M.E.; Loftis, C.M.; Worley, J.R.; Tweedy, N.M.; Gupta, S.U.; Duren, D.L.; Holzhauser, C.M.; Ramachandran, V.M. Anterior Vertebral Body Tethering for Adolescent Scoliosis with Growth Remaining: A Retrospective Review of 2 to 5-Year Postoperative Results. J. Bone Jt. Surg. 2020, 102, 1169–1176. [Google Scholar] [CrossRef]
- Wong, H.K.; Ruiz, J.N.M.; Newton, P.O.; Gabriel Liu, K.P. Non-Fusion Surgical Correction of Thoracic Idiopathic Scoliosis Using a Novel, Braided Vertebral Body Tethering Device: Minimum Follow-up of 4 Years. JBJS Open Access 2019, 4, e0026. [Google Scholar] [CrossRef] [PubMed]
- Ergene, G. Early-term postoperative thoracic outcomes of videothoracoscopic vertebral body tethering surgery. Turk. J. Thorac. Cardiovasc. Surg. 2019, 27, 526–531. [Google Scholar] [CrossRef] [PubMed]
- Joshi, V.; Cassivi, S.D.; Milbrandt, T.A.; Larson, A.N. Video-assisted thoracoscopic anterior vertebral body tethering for the correction of adolescent idiopathic scoliosis of the spine. Eur. J. Cardio Thoracic Surg. 2018, 54, 1134–1136. [Google Scholar] [CrossRef] [PubMed]
- Baroncini, A.; Trobisch, P.; Blau, C.; Golias, C.; Kobbe, P.; Eschweiler, J.; Tingart, M.; Migliorini, F. Analysis of the pulmonary function in patients undergoing vertebral body tethering for adolescent idiopathic scoliosis. Eur. Spine J. 2021. [Google Scholar] [CrossRef] [PubMed]
- Trobisch, P.; Migliorini, F.; Vanspauwen, T.; Baroncini, A. Pulmonary Complications after Vertebral Body Tethering: Incidence, Treatment, Outcomes and Risk Factor Analysis. J. Clin. Med. 2022, 11, 3778. [Google Scholar] [CrossRef]
- Shin, M.; Arguelles, G.R.; Cahill, P.J.; Flynn, J.M.; Baldwin, K.D.; Anari, J.B. Complications, Reoperations, and Mid-Term Outcomes Following Anterior Vertebral Body Tethering Versus Posterior Spinal Fusion: A Meta-Analysis. JBJS Open Access 2021, 6, e21.00002. [Google Scholar] [CrossRef]
- Shen, J.; Parent, S. Iatrogenic dural tear after growth modulation in AIS: An unusual complication and its management. Spine Deform. 2021, 9, 1699–1703. [Google Scholar] [CrossRef]
- Meyers, J.; Eaker, L.; von Treuheim, T.D.P.; Dolgovpolov, S.; Lonner, B. Early operative morbidity in 184 cases of anterior vertebral body tethering. Sci. Rep. 2021, 11, 23049. [Google Scholar] [CrossRef]
- Abdullah, A.; Parent, S.; Miyanji, F.; Smit, K.; Murphy, J.; Skaggs, D.; Gupta, P.; Vitale, M.; Ouellet, J.; Saran, N.; et al. Risk of early complication following anterior vertebral body tethering for idiopathic scoliosis. Spine Deform. 2021, 9, 1419–1431. [Google Scholar] [CrossRef]
- Baroncini, A.; Trobisch, P.; Eschweiler, J.; Migliorini, F. Analysis of the risk factors for early tether breakage following vertebral body tethering in adolescent idiopathic scoliosis. Eur. Spine J. 2022, 31, 2348–2354. [Google Scholar] [CrossRef]
- Newton, P.O.; Takahashi, Y.; Yang, Y.; Yaszay, B.; Bartley, C.E.; Bastrom, T.P.; Munar, C. Anterior vertebral body tethering for thoracic idiopathic scoliosis leads to asymmetric growth of the periapical vertebrae. Spine Deform. 2022, 10, 553–561. [Google Scholar] [CrossRef] [PubMed]
- McDonald, T.C.; Shah, S.A.; Hargiss, J.B.; Varghese, J.; Boeyer, M.E.; Pompliano, M.; Neal, K.; Lonner, B.S.; Larson, A.N.; Yaszay, B.; et al. When successful, anterior vertebral body tethering (VBT) induces differential segmental growth of vertebrae: An in vivo study of 51 patients and 764 vertebrae. Spine Deform. 2022, 31, 2348–2354. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Mathew, S.; Milbrandt, T.A.; Potter, D.D.; Larson, A.N. Thoracic paravertebral nerve catheter reduces postoperative opioid use for vertebral body tethering patients. Spine Deform. 2021, 9, 1601–1607. [Google Scholar] [CrossRef] [PubMed]
- Da Paz, S.; Trobisch, P.; Baroncini, A. The use of electronic conductivity devices can effectively reduce radiation exposure in vertebral body tethering. Eur. Spine J. 2022. [Google Scholar] [CrossRef]
- Ruzic, J.C.; Moreno, A.; Morin, C. [Simplified technique for thoracic drainage in anterior surgery of scoliosis in the child]. Rev. Chir. Orthop. Reparatrice Appar. Mot. 1998, 84, 550–553. [Google Scholar]
- Baroncini, A.; Courvoisier, A.; Berjano, P.; Migliorini, F.; Eschweiler, J.; Kobbe, P.; Hildebrand, F.; Trobisch, P.D. The effects of vertebral body tethering on sagittal parameters: Evaluations from a 2-years follow-up. Eur. Spine J. 2021, 31, 1060–1066. [Google Scholar] [CrossRef]
- Alanay, A.; Yucekul, A.; Abul, K.; Ergene, G.; Senay, S.; Ay, B.; Cebeci, B.O.; Yalinay Dikmen, P.; Zulemyan, T.; Yavuz, Y.; et al. Thoracoscopic Vertebral Body Tethering for Adolescent Idiopathic Scoliosis: Follow-up Curve Behavior According to Sanders Skeletal Maturity Staging. Spine 2020, 45, E1483–E1492. [Google Scholar] [CrossRef]

| Patients’ Characteristics | ||||
|---|---|---|---|---|
| n | Total | |||
| Age surgery (years) | 12.5 (9; 14) | |||
| Follow-up (years) | 2.6 (2; 7) | |||
| Risser | 0 | TRC Open | 15 (17%) | 85 |
| TRC closed | 46 (55%) | |||
| 1 | 13 (15%) | |||
| 2 | 11 (13%) | |||
| Gender | F | 73 (85%) | ||
| M | 12 (15%) | |||
| Lenke types | 1A | 40 (47%) | ||
| 1B | 12 (14%) | |||
| 1C | 17 (20%) | |||
| 5C | 5 (6%) | |||
| 2A | 11 (13%) | |||
| Pre-op | Post-op Day 3 | Post-op 1y | Last f/u | p-Value | |
|---|---|---|---|---|---|
| Major curve | 49°(8,9°) | 27°(12°) | 22°(12°) | 19°(14°) | <0.01 |
| Secondary curve | 27°(14°) | 23°(15°) | 22°(11°) | 17°(10°) | <0.01 |
| Instrumented curve | NA | 26°(11°) | 23°(10°) | 20°(14°) | <0.01 |
| Kyphosis (T1–T12) | 20°(13°) | 23°(13°) | 25°(12°) | 24°(14°) | 0.06 |
| Lordosis (L1–L5) | 36°(12°) | 32°(13°) | 40°(7°) | 40°(8°) | 0.07 |
| Complications | Patients | Curve Type | Treatment | Time to Diagnosis |
|---|---|---|---|---|
| Right shoulder pain | 14 (15%) | 10 right thor./5 Double | Painkillers | Immediate post-op |
| Aseptic pleural effusion | 1 (1%) | Right thor. | Drainage 2 weeks | 45 days po |
| Pneumothorax | 2 (2%) | Right thor. | Drainage 2 days | Immediate post-op |
| Overcorrection | 10 (11%) | 10 right thor. | 5 tether release | Between 1,5, and 2 y po |
| Tether breakage | 2 (2%) | Lumbar | - | 2 y po |
| Cranial screw slippage | 6 (7%) | Thor. | - | 18 months po |
| Curve progression | 5 (2 adding-on) (5%) | Thor. | Fusion | 1 y po |
| Authors | Patients | f/u (y) | Age | Pre-op (°) | Last f/u (°) | Kyphosis Pre-op (°) | Kyphosis Last f/u (°) | Lordosis Pre-op (°) | Lordosis Last f/u (°) | Complications | Revisions |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Samdani 2014 [5] | 11 | 2 | 12.3 | 44.2 | 13.5 | 20.8 | 21.6 | 47.5 | 54.9 | 1 atélectasia | 2 OC |
| Wong 2019 [21] | 5 | 4 | 11 | 41.1 | 32.1 | - | - | - | - | 1 pneumonia, 2PTX, 2 pleural effusion | 1 OC, 1 Fusion |
| Alanay 2020 [38] | 31 | 2.2 | 12.1 | 46 | 12 | - | - | - | - | 2 atelectasia, 1 chylothorax, 1 pleural effusion | 2 OC |
| Hoernschemeyer 2020 [20] | 29 | 3.1 | 12.7 | 49 | 19 | - | - | - | - | 1 PTX, 1 syncope, | 2 fusions, 4 OC |
| Newton 2018 [3] | 17 | 2.5 | 11 | 52 | 27 | 25 | 22 | - | - | 2 atelectasia | 4 OC, 4 fusions, 1 rupture |
| Newton 2020 [19] | 23 | 3.4 | 12 | 53 | 33 | 25 | 19 | - | - | 1 atelectasia, 1 Horner | 3 OC, 3 tether rupture, 1 fusion |
| Pehlivanoglu 2020 [18] | 21 | 2 | 11.1 | 48.2 | 10 | 26.8 | 26 | 51.3 | 51.8 | 1 chylothorax | 1 re-VBT |
| Baroncini 2021 [37] | 86 | 2 | 13.2 | 52 | 28.5 | 28.3 | 33 | 47.5 | 48.4 | 5 pleural effusion | 5 re-VBT/1 irritation psoas |
| Samdani 2021 [7] | 57 | 4.6 | 12.4 | 40.4 | 18.7 | 15.5 | 19.6 | - | - | - | 5 OC/2 fusions |
| Rushton 2021 [8] | 112 | 3.1 | 12.7 | 50.8 | 25.7 | - | - | - | 25 complications | 15 (7 fusions) | |
| Courvoisier 2022 | 85 | 2.6 | 12.5 | 49 | 19 | 20 | 24 | 36 | 40 | 1 pleural effusion, 2 PTX | 5 fusions, 10 OC |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Courvoisier, A.; Baroncini, A.; Jeandel, C.; Barra, C.; Lefevre, Y.; Solla, F.; Gouron, R.; Métaizeau, J.-D.; Maximin, M.-C.; Cunin, V. Vertebral Body Tethering in AIS Management—A Preliminary Report. Children 2023, 10, 192. https://doi.org/10.3390/children10020192
Courvoisier A, Baroncini A, Jeandel C, Barra C, Lefevre Y, Solla F, Gouron R, Métaizeau J-D, Maximin M-C, Cunin V. Vertebral Body Tethering in AIS Management—A Preliminary Report. Children. 2023; 10(2):192. https://doi.org/10.3390/children10020192
Chicago/Turabian StyleCourvoisier, Aurélien, Alice Baroncini, Clément Jeandel, Clémentine Barra, Yan Lefevre, Federico Solla, Richard Gouron, Jean-Damien Métaizeau, Marie-Christine Maximin, and Vincent Cunin. 2023. "Vertebral Body Tethering in AIS Management—A Preliminary Report" Children 10, no. 2: 192. https://doi.org/10.3390/children10020192
APA StyleCourvoisier, A., Baroncini, A., Jeandel, C., Barra, C., Lefevre, Y., Solla, F., Gouron, R., Métaizeau, J.-D., Maximin, M.-C., & Cunin, V. (2023). Vertebral Body Tethering in AIS Management—A Preliminary Report. Children, 10(2), 192. https://doi.org/10.3390/children10020192








