A Retrospective Study Comparing Outcomes of Paravertebral Clonidine Infusion for Pediatric Patients Undergoing Nuss Procedure
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol Description
2.2. Old Protocol (Paravertebral Catheter Infusion with Ropivacaine 0.2%)
2.3. The New Protocol (Paravertebral Catheter Ropivacaine and Clonidine Infusion)
2.4. Analyses
3. Results
3.1. Demographics
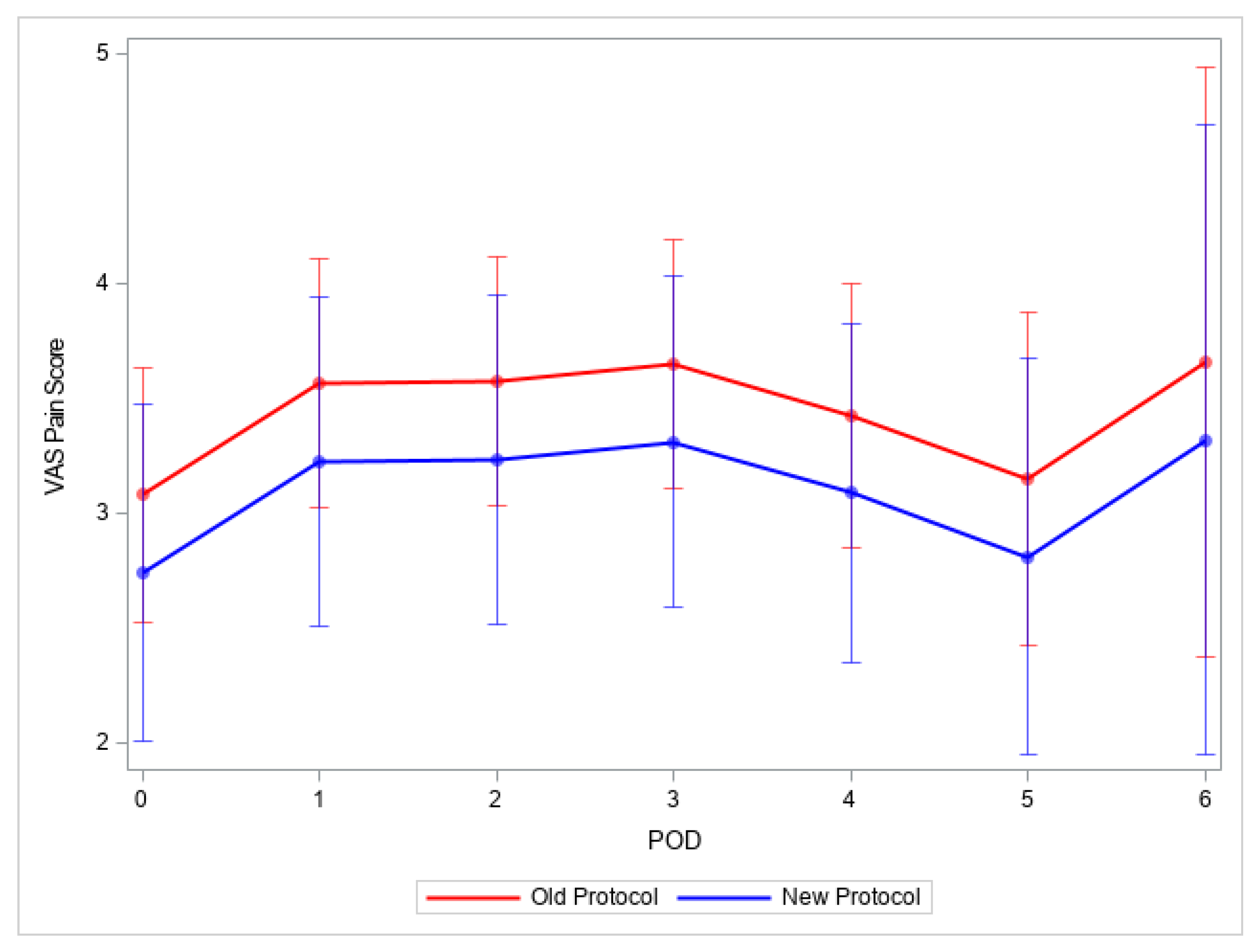
3.1.1. Pain Scores
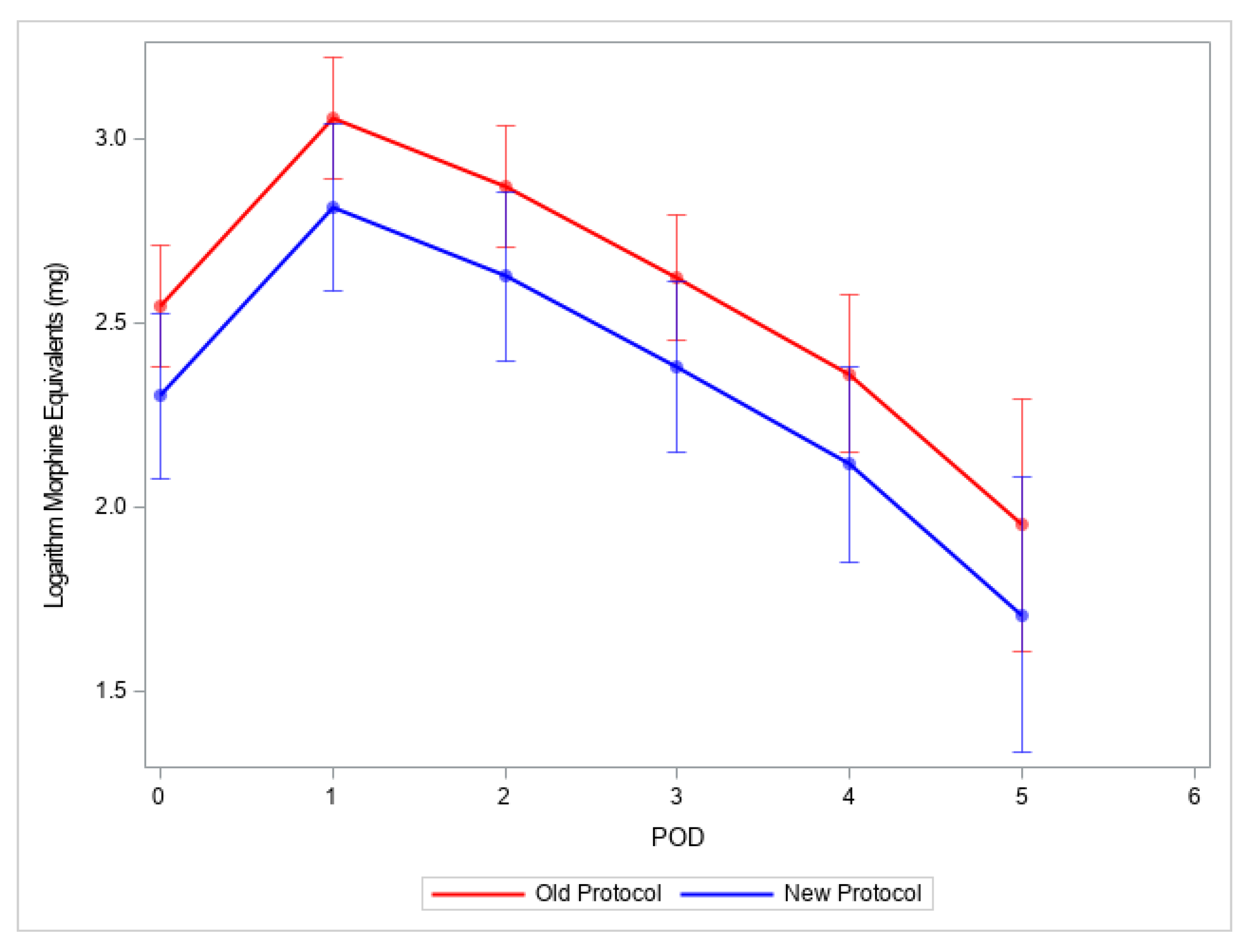
3.1.2. Analgesic Administration
3.1.3. Postoperative Outcomes
3.1.4. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Obermeyer, R.J.; Goretsky, M.J. Chest Wall Deformities in Pediatric Surgery. Surg. Clin. N. Am. 2012, 92, 669–684. [Google Scholar] [CrossRef] [PubMed]
- Malek, M.H.; Fonkalsrud, E.W.; Cooper, C.B. Ventilatory and Cardiovascular Responses to Exercise in Patients with Pectus Excavatum. Chest 2003, 124, 870–882. [Google Scholar] [CrossRef] [PubMed]
- Kelly, R.E.; Goretsky, M.J.; Obermeyer, R.; Kuhn, M.A.; Redlinger, R.; Haney, T.S.; Moskowitz, A.; Nuss, D. Twenty-One Years of Experience With Minimally Invasive Repair of Pectus Excavatum by the Nuss Procedure in 1215 Patients. Ann. Surg. 2010, 252, 1072–1081. [Google Scholar] [CrossRef] [PubMed]
- Fraser, J.A.; Briggs, K.B.; Svetanoff, W.J.; Aguayo, P.; Juang, D.; Fraser, J.D.; Snyder, C.L.; Oyetunji, T.A.; Peter, S.D.S. Short and long term outcomes of using cryoablation for postoperative pain control in patients after pectus excavatum repair. J. Pediatr. Surg. 2022, 57, 1050–1055. [Google Scholar] [CrossRef] [PubMed]
- Densmore, J.C.; Peterson, D.B.; Stahovic, L.L.; Czarnecki, M.L.; Hainsworth, K.R.; Davies, H.W.; Cassidy, L.D.; Weisman, S.J.; Oldham, K.T. Initial surgical and pain management outcomes after Nuss procedure. J. Pediatr. Surg. 2010, 45, 1767–1771. [Google Scholar] [CrossRef] [PubMed]
- Muhly, W.T.; Maxwell, L.G.; Cravero, J.P. Pain management following the Nuss procedure: A survey of practice and review. Acta Anaesthesiol. Scand. 2014, 58, 1134–1139. [Google Scholar] [CrossRef] [PubMed]
- Gurnaney, H.G.; Maxwell, L.G.; Kraemer, F.W.; Goebel, T.; Nance, M.L.; Ganesh, A. Prospective randomized observer-blinded study comparing the analgesic efficacy of ultrasound-guided rectus sheath block and local anaesthetic infiltration for umbilical hernia repair. Br. J. Anaesth. 2011, 107, 790–795. [Google Scholar] [CrossRef] [PubMed]
- Walter, C.M.; Lee, C.S.; Moore, D.L.; Abbasian, N.; Clay, S.J.; Mecoli, M.D.; Olbrecht, V.A.; Batra, M.; Ding, L.; Yang, F.; et al. Retrospective Study Comparing Outcomes of Multimodal Epidural and Erector Spinae Catheter Pain Protocols after Pectus Surgery. J. Pediatr. Surg. 2022; Online ahead of print. [Google Scholar] [CrossRef]
- Mehl, S.C.; Sun, R.C.; Anbarasu, C.R.; Portuondo, J.I.; Espinoza, A.F.; Whitlock, R.S.; Shah, S.R.; Nuchtern, J.G.; Minifee, P.K.; Rodriguez, J.R.; et al. Association of Intercostal Nerve Cryoablation During Nuss Procedure with Complications and Costs. Ann. Thorac. Surg. 2022; Online ahead of print. [Google Scholar] [CrossRef]
- Man, J.Y.; Gurnaney, H.G.; Dubow, S.R.; DiMaggio, T.J.; Kroeplin, G.R.; Adzick, N.S.; Muhly, W.T. A retrospective comparison of thoracic epidural infusion and multimodal analgesia protocol for pain management following the minimally invasive repair of pectus excavatum. Pediatr. Anesth. 2017, 27, 1227–1234. [Google Scholar] [CrossRef] [PubMed]
- Muhly, W.T.; Beltran, R.J.; Bielsky, A.; Bryskin, R.B.; Chinn, C.; Choudhry, D.K.; Cucchiaro, G.; Fernandez, A.; Glover, C.D.; Haile, D.T.; et al. Perioperative Management and In-Hospital Outcomes After Minimally Invasive Repair of Pectus Excavatum. Obstet. Anesth. Dig. 2019, 128, 315–327. [Google Scholar] [CrossRef] [PubMed]
- Boretsky, K.; Visoiu, M.; Bigeleisen, P. Ultrasound-guided approach to the paravertebral space for catheter insertion in infants and children. Pediatr. Anesth. 2013, 23, 1193–1198. [Google Scholar] [CrossRef] [PubMed]
- Pöpping, D.M.; Elia, N.; Marret, E.; Wenk, M.; Tramèr, M.R.; Warner, D.S.; Warner, M.A. Clonidine as an Adjuvant to Local Anesthetics for Peripheral Nerve and Plexus Blocks. Anesthesiology 2009, 111, 406–415. [Google Scholar] [CrossRef] [PubMed]
- Cucchiaro, G.; Ganesh, A. The Effects of Clonidine on Postoperative Analgesia After Peripheral Nerve Blockade in Children. Obstet. Anesth. Dig. 2007, 104, 532–537. [Google Scholar] [CrossRef] [PubMed]
- Visoiu, M.; Scholz, S.; Malek, M.M.; Carullo, P.C. The addition of clonidine to ropivacaine in rectus sheath nerve blocks for pediatric patients undergoing laparoscopic appendectomy: A double blinded randomized prospective study. J. Clin. Anesth. 2021, 71, 110254. [Google Scholar] [CrossRef] [PubMed]
- Petroheilou, K.; Livanios, S.; Zavras, N.; Hager, J.; Fassoulaki, A. Sciatic lateral popliteal block with clonidine alone or clonidine plus 0.2% ropivacaine: Effect on the intra-and postoperative analgesia for lower extremity surgery in children: A randomized prospective controlled study. BMC Anesthesiol. 2012, 12, 2. [Google Scholar] [CrossRef] [PubMed]
- Trifa, M.; Ben Khalifa, S.; Jendoubi, A.; Zribi, N.; Regaya, T.; Engelhardt, T. Clonidine does not improve quality of ropivacaine axillary brachial plexus block in children. Pediatr. Anesth. 2012, 22, 425–429. [Google Scholar] [CrossRef] [PubMed]
- Dagher, C.; Yazigi, A.; Rkaibe, N. Clonidine as adjuvant for bupivacaine in ilioinguinal block does not prolong postoperative analgesia in pediatric and also in adult patients. Pediatr. Anesth. 2006, 16, 224–225. [Google Scholar] [CrossRef] [PubMed]
- Kaabachi, O.; Zerelli, Z.; Methamem, M.; Ben Abdelaziz, A.; Moncer, K.; Toumi, M. Clonidine administered as adjuvant for bupivacaine in ilioinguinal-iliohypogastric nerve block does not prolong postoperative analgesia. Pediatr. Anesth. 2005, 15, 586–590. [Google Scholar] [CrossRef] [PubMed]
- Bhatnagar, S.; Mishra, S.; Madhurima, S.; Gurjar, M.; Mondal, A.S. Clonidine as an Analgesic Adjuvant to Continuous Paravertebral Bupivacaine for Post-thoracotomy Pain. Anaesth. Intensiv. Care 2006, 34, 586–591. [Google Scholar] [CrossRef]
- Das, A.; Mayur, N.; Biswas, H.; Chhaule, S.; Chattopadhyay, S.; Mitra, T.; RoyBasunia, S.; Mandal, S.K. Effect of clonidine as adjuvant in thoracic paravertebral block for patients undergoing breast cancer surgery: A prospective, randomized, placebo-controlled, double-blind study. Anesth. Essays Res. 2017, 11, 864–870. [Google Scholar] [CrossRef]
- Ilfeld, B.M.; Finneran, J.J.; Swisher, M.W.; Said, E.T.; Gabriel, R.A.; Sztain, J.F.; Khatibi, B.; Armani, A.; Trescot, A.; Donohue, M.C.; et al. Preoperative Ultrasound-guided Percutaneous Cryoneurolysis for the Treatment of Pain after Mastectomy: A Randomized, Participant- and Observer-masked, Sham-controlled Study. Anesthesiology 2022, 137, 529–542. [Google Scholar] [CrossRef] [PubMed]
| Median (Q1, Q3) or N (%) | |||
|---|---|---|---|
| Old Protocol/ Ropivacaine | New Protocol/ Ropivacaine Clonidine | p-Value | |
| Number of patients | N = 45 | N = 18 | |
| Age (years) | 15 (14, 16) | 15 (14, 16) | 0.8740 |
| Gender (male, %) | 37 (82) | 15 (83) | 1.0000 |
| Weight (kg) | 56.00 (49.30, 59.40) | 52.00 (46.40, 61.90) | 0.2130 |
| BMI | 18.00 (16.90, 19.80) | 18.00 (17.00, 19.00) | 0.7340 |
| Haller index | 4.80 (4.10, 6.60) | 6.45 (4.80, 9.40) | 0.0130 |
| Bars | 0.7290 | ||
| 1 bar | 37 (82) | 14 (78) | |
| 2 bars | 8 (18) | 4 (22) | |
| ASA class | 1.0000 | ||
| I/II/III | 9 (20)/34 (76)/2 (4) | 4 (22)/13 (72)/1 (6) | |
| Surgical service | 0.3396 | ||
| Cardiac surgery | 12 (27) | 7 (39) | |
| General surgery | 33 (73) | 11 (61) | |
| Nerve block procedure time (min) | 22.00 (16.00, 26.00) | 20.50 (15.00, 25.00) | 0.5446 |
| Nerve block type | |||
| Paravertebral block catheters | 45 (100) | 18 (100) | |
| Nerve block level | 0.0639 | ||
| T4 | 1 (2) | 0 (0) | |
| T5 | 33 (73) | 8 (44) | |
| T6 | 9 (20) | 9 (50) | |
| T7 | 2 (4) | 1 (6) | |
| Nerve block sedation | 0.0104 | ||
| Awake/sedation | 30 (67) | 5 (28) | |
| General anesthesia | 15 (33) | 13 (72) | |
| Catheter infusion duration (days) | 3.60 (2.90, 3.80) | 3.35 (2.80, 4.20) | 0.8973 |
| Anesthesia time (min) | 178.00 (163.00, 207.00) | 204.00 (177.00, 238.00) | 0.0569 |
| Surgical time (min) | 79.00 (68.00, 97.00) | 96.50 (83.00, 134.00) | 0.0199 |
| Hospital LOS (days) | 4.40 (4.00, 5.10) | 4.30 (4.10, 5.10) | 0.9637 |
| Old Protocol Ropivacaine | New Protocol Ropivacaine with Clonidine | p-Value | |||
|---|---|---|---|---|---|
| Frequency N(%) | Amount | Frequency N(%) | Amount | ||
| Morphine equivalents | |||||
| mg | 15.36 (12.68, 20.00) | 14.02 (12.50, 23.04) | |||
| mg/kg | 0.30 (0.20, 0.40) | 0.30 (0.20, 0.40) | |||
| Fentanyl (mcg) | 44 (98) | 150.00 (100.00, 200.00) | 17 (94) | 100.00 (100.00, 150.00) | 0.3651 |
| Hydromorphone (mg) | 13 (29) | 0.00 (0.00, 0.30) | 8 (44) | 0.00 (0.00, 0.60) | 0.1151 |
| Morphine (mg) | 10 (22) | 0.00 (0.00, 0.00) | 2 (11) | 0.00 (0.00, 0.00) | - |
| Dexmedetomidine (mcg) | 34 (76) | 20.00 (8.00, 20.00) | 14 (78) | 18.00 (8.00, 20.00) | 0.9127 |
| Ketorolac (mg) | 5 (11) | 0.00 (0.00, 0.00) | 6 (33) | 0.00 (0.00, 15.00) | 0.0683 |
| Ketamine (mg) | 39 (87) | 50.00 (40.00, 60.00) | 12 (67) | 37.50 (0.00, 50.00) | 0.2382 |
| Acetaminophen (mg) | 32 (71) | 750.00 (0.00, 870.00) | 15 (83) | 737.50 (650.00, 850.00) | 0.9878 |
| Ondansetron (mg) | 43 (96) | 4.00 (4.00, 4.00) | 17 (94) | 4.00 (4.00, 4.00) | 0.9001 |
| Diphenhydramine (mg) | 2 (4) | 0.00 (0.00, 0.00) | 1 (6) | - | - |
| Diazepam (mg) | 2 (4) | 0.00 (0.00, 0.00) | 0 (0) | - | - |
| Midazolam (mg) | 37 (82) | 4.00 (3.00, 5.00) | 15 (83) | 4.00 (2.00, 6.00) | 0.9814 |
| Dexamethasone(mg) | 32 (71) | 6.00 (0.00, 8.00) | 12 (67) | 4.00 (0.00, 8.00) | 0.6207 |
| Initial ropivacaine bolus | |||||
| mg | 148.00 (100.00, 150.00) | 113.50 (90.00, 200.00) | |||
| mg/kg | 2.60 (2.10, 3.00) | 2.35 (1.60, 3.60) | |||
| Old Protocol Ropivacaine | New Protocol Ropivacaine with Clonidine | p-Value | |||
|---|---|---|---|---|---|
| Frequency N(%) | Amount | Frequency N(%) | Amount | ||
| Total morphine equivalents | |||||
| mg | 2.01 (0.00, 4.34) | 1.15 (0.00, 5.00) | |||
| mg/kg | 0.04 (0.00, 0.08) | 0.03 (0.00, 0.10) | |||
| Fentanyl (mcg) | 20 (44) | 0.00 (0.00, 27.70) | 9 (50) | 11.50 (0.00, 50.00) | 0.5862 |
| Hydromorphone (mg) | 7 (16) | 0.00 (0.00, 0.00) | 2 (11) | 0.00 (0.00, 0.00) | 0.6275 |
| Morphine (mg) | 7 (16) | 0.00 (0.00, 0.00) | 3 (17) | 0.00 (0.00, 0.00) | 1.0000 |
| Ketorolac (mg) | 2 (4) | 0.00 (0.00, 0.00) | 2 (11) | 0.00 (0.00, 0.00) | - |
| Acetaminophen (mg) | 8 (18) | 0.00 (0.00, 0.00) | 2 (11) | 0.00 (0.00, 0.00) | - |
| Diazepam (mg) | 2 (4) | 0.00 (0.00, 0.00) | 0 (0) | - | - |
| Old Protocol Ropivacaine | New Protocol Ropivacaine with Clonidine | p-Value | |||
|---|---|---|---|---|---|
| POD 1 | N | N | |||
| Ketorolac (mg) | 36 | 30.00 (30.00, 45.00) | 16 | 45.00 (30.00, 60.00) | 0.1153 |
| Acetaminophen (mg) | 45 | 3000.00 (2680.00, 3464.00) | 18 | 2755.50 (2250.00, 4000.00) | 0.5341 |
| Ketamine (mg) | 43 | 120.00 (79.20, 144.00) | 17 | 96.00 (60.00, 120.00) | 0.1170 |
| Cyclobenzaprine (mg) | 37 | 10.00 (10.00, 20.00) | 17 | 10.00 (5.00, 10.00) | 0.0684 |
| Diazepam (mg) | 7 | 2.00 (2.00, 3.00) | 5 | 5.00 (5.00, 5.00) | 0.0665 |
| Gabapentin (mg) | 43 | 300.00 (300.00, 300.00) | 6 | 300.00 (300.00, 300.00) | 0.3093 |
| POD 2 | |||||
| Ketorolac (mg) | 42 | 60.00 (45.00, 60.00) | 18 | 30.00 (30.00, 60.00) | 0.0012 |
| Acetaminophen (mg) | 44 | 2728.50 (2362.50, 3359.00) | 17 | 2795.00 (2250.00, 3640.00) | 0.8916 |
| Ketamine (mg) | 41 | 96.00 (60.00, 120.00) | 17 | 39.60 (35.00, 60.00) | 0.0003 |
| Cyclobenzaprine (mg) | 42 | 10.00 (10.00, 20.00) | 18 | 10.00 (10.00, 10.00) | 0.0411 |
| Diazepam (mg) | 7 | 2.50 (2.00, 2.50) | 6 | 3.75 (2.50, 6.00) | 0.2230 |
| Gabapentin (mg) | 42 | 300.00 (300.00, 300.00) | 6 | 300.00 (300.00, 300.00) | 0.1326 |
| Ibuprofen (mg) | 5 | 800.00 (600.00, 800.00) | 8 | 800.00 (400.00, 1000.00) | 1.0000 |
| POD 3 | |||||
| Ketorolac (mg) | 37 | 45.00 (30.00, 60.00) | 6 | 37.50 (30.00, 45.00) | 0.6917 |
| Acetaminophen (mg) | 45 | 2600.00 (2400.00, 3044.00) | 17 | 2600.00 (2250.00, 4000.00) | 0.5420 |
| Ketamine (mg) | 29 | 58.50 (40.60, 72.00) | 4 | 38.75 (32.25, 52.50) | 0.2544 |
| Cyclobenzaprine (mg) | 42 | 10.00 (10.00, 20.00) | 17 | 10.00 (10.00, 15.00) | 0.3943 |
| Diazepam (mg) | 7 | 3.00 (2.50, 4.00) | 8 | 4.25 (2.25, 11.50) | 0.4946 |
| Gabapentin (mg) | 36 | 300.00 (300.00, 300.00) | 8 | 300.00 (300.00, 350.00) | 0.0395 |
| Ibuprofen (mg) | 30 | 800.00 (600.00, 1200.00) | 15 | 1200.00 (800.00, 2000.00) | 0.0959 |
| POD 4 | |||||
| Ketorolac (mg) | 11 | 30.00 (30.00, 60.00) | 1 | - | - |
| Acetaminophen (mg) | 39 | 2250.00 (1625.00, 3000.00) | 15 | 2000.00 (1300.00, 3000.00) | 0.7868 |
| Ketamine (mg) | 6 | 37.75 (25.00, 60.00) | 1 | 25.00 (25.00, 25.00) | 0.6319 |
| Cyclobenzaprine (mg) | 37 | 10.00 (10.00, 15.00) | 15 | 10.00 (5.00, 15.00) | 0.4740 |
| Diazepam (mg) | 1 | - | 6 | 3.25 (2.00, 10.00) | - |
| Gabapentin (mg) | 19 | 300.00 (300.00, 300.00) | 4 | 300.00 (300.00, 350.00) | 0.0509 |
| Ibuprofen (mg) | 33 | 1200.00 (800.00, 1600.00) | 14 | 1400.00 (1200.00, 1600.00) | 0.3570 |
| POD 5 | |||||
| Ketorolac (mg) | 4 | 30.00 (22.50, 45.00) | 0 | - | |
| Acetaminophen (mg) | 22 | 2537.50 (1300.00, 3000.00) | 7 | 1950.00 (1500.00, 2600.00) | 0.5094 |
| Ketamine (mg) | 2 | 65.75 (27.50, 104.00) | 0 | - | |
| Cyclobenzaprine (mg) | 20 | 5.00 (5.00, 10.00) | 8 | 10.00 (5.00, 10.00) | 0.7010 |
| Diazepam (mg) | 1 | - | 3 | 5.00 (2.50, 10.00) | 0.4370 |
| Gabapentin (mg) | 4 | 300.00 (300.00, 300.00) | 2 | 350.00 (300.00, 400.00) | 0.3374 |
| Ibuprofen (mg) | 19 | 1200.00 (800.00, 1200.00) | 8 | 800.00 (700.00, 1600.00) | 0.4204 |
| POD 6 | |||||
| Ketorolac (mg) | 1 | 30.00 (30.00, 30.00) | 0 | - | |
| Acetaminophen (mg) | 7 | 1300.00 (1300.00, 1950.00) | 3 | 1500.00 (1300.00, 1950.00) | 0.8121 |
| Cyclobenzaprine (mg) | 5 | 5.00 (5.00, 10.00) | 3 | 5.00 (5.00, 10.00) | 1.0000 |
| Ibuprofen (mg) | 6 | 1200.00 (800.00, 1200.00) | 3 | 800.00 (800.00, 1200.00) | 0.4774 |
| N | Old Protocol Ropivacaine (mg/kg) | N | New Protocol Ropivacaine Clonidine (mg/kg) | p-Value | |
|---|---|---|---|---|---|
| Intraoperatively | 45 | 0.30 (0.20, 0.40) | 18 | 0.30 (0.20, 0.40) | |
| PACU | 45 | 0.04 (0.00, 0.08) | 18 | 0.03 (0.00, 0.10) | |
| POD 1 | 45 | 0.26 (0.18, 0.32) | 18 | 0.21 (0.11, 0.31) | 0.3046 |
| POD 2 | 45 | 0.47 (0.29, 0.61) | 18 | 0.24 (0.22, 0.31) | 0.0026 |
| POD 3 | 45 | 0.31 (0.24, 0.43) | 18 | 0.32 (0.22, 0.37) | 0.5650 |
| POD 4 | 45 | 0.23 (0.14, 0.37) | 18 | 0.22 (0.14, 0.37) | 0.6656 |
| POD 5 | 45 | 0.00 (0.00, 0.22) | 18 | 0.00 (0.00, 0.22) | 0.7678 |
| POD 6 | 45 | 0.00 (0.00, 0.00) | 18 | 0.00 (0.00, 0.00) | 0.9820 |
| Old Protocol/ Ropivacaine | New Protocol/ Ropivacaine Clonidine | p-Value | |
|---|---|---|---|
| N | N | ||
| Nausea | 26 (58) | 8 (44) | 0.3375 |
| Pruritis | 10 (22) | 5 (28) | 0.7457 |
| Muscle spasm | 16 (36) | 11 (61) | 0.0641 |
| Urinary retention | 4 (9) | 1 (6) | 1.0000 |
| Respiratory depression | 2 (4) | 2 (11) | 0.5712 |
| Oversedation | 0 (0) | 1 (6) | 0.2857 |
| Constipation | 6 (13) | 2 (11) | 1.0000 |
| Other | 2 (4) | 3 (17) | 0.1357 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Visoiu, M.; Sadhasivam, S. A Retrospective Study Comparing Outcomes of Paravertebral Clonidine Infusion for Pediatric Patients Undergoing Nuss Procedure. Children 2023, 10, 193. https://doi.org/10.3390/children10020193
Visoiu M, Sadhasivam S. A Retrospective Study Comparing Outcomes of Paravertebral Clonidine Infusion for Pediatric Patients Undergoing Nuss Procedure. Children. 2023; 10(2):193. https://doi.org/10.3390/children10020193
Chicago/Turabian StyleVisoiu, Mihaela, and Senthilkumar Sadhasivam. 2023. "A Retrospective Study Comparing Outcomes of Paravertebral Clonidine Infusion for Pediatric Patients Undergoing Nuss Procedure" Children 10, no. 2: 193. https://doi.org/10.3390/children10020193
APA StyleVisoiu, M., & Sadhasivam, S. (2023). A Retrospective Study Comparing Outcomes of Paravertebral Clonidine Infusion for Pediatric Patients Undergoing Nuss Procedure. Children, 10(2), 193. https://doi.org/10.3390/children10020193







