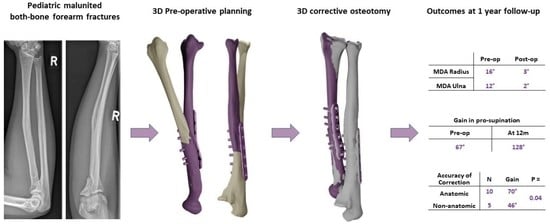
Accuracy of 3D Corrective Osteotomy for Pediatric Malunited Both-Bone Forearm Fractures
Abstract
1. Introduction
2. Materials and Methods
2.1. Outcome Measures
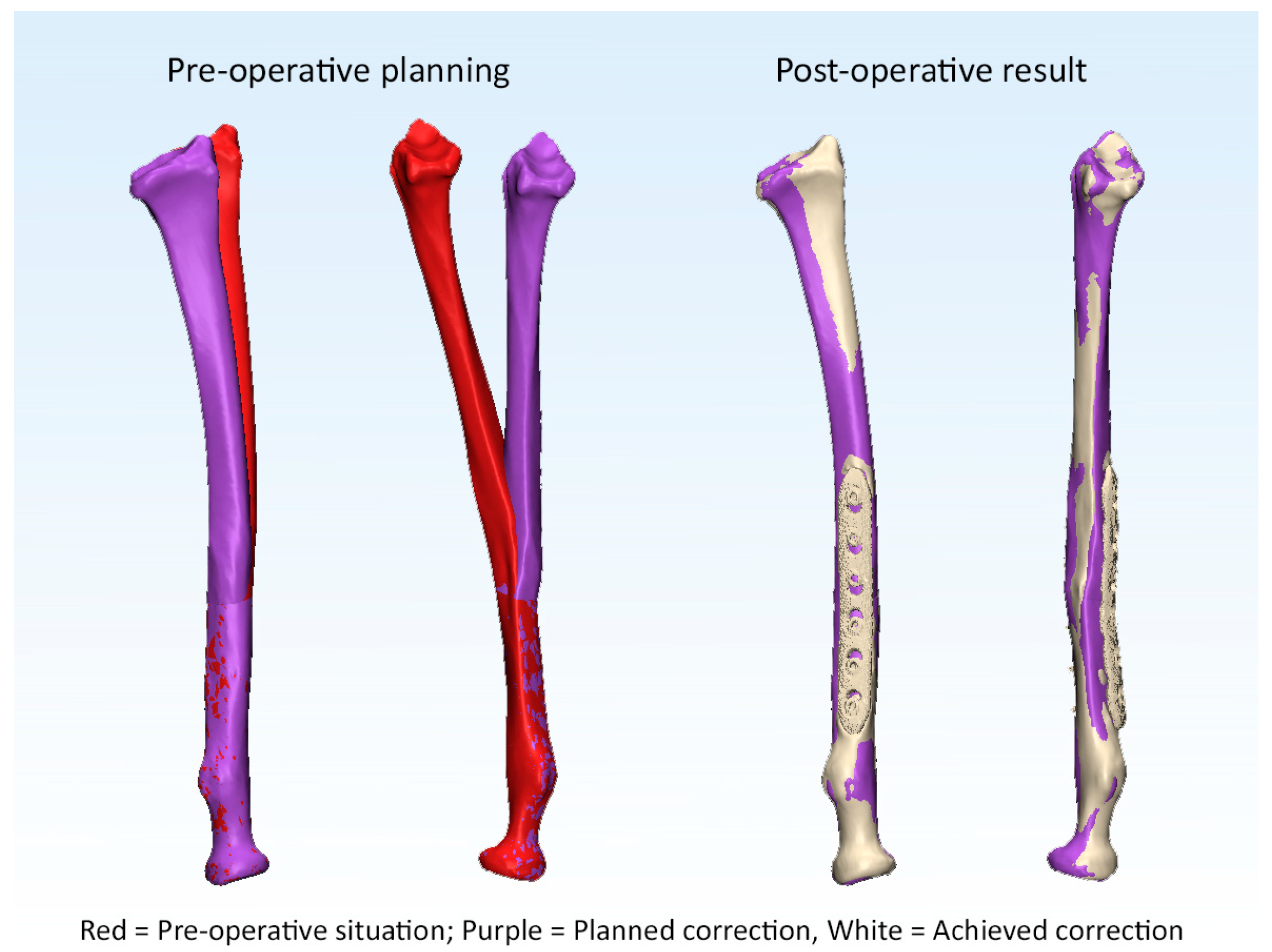
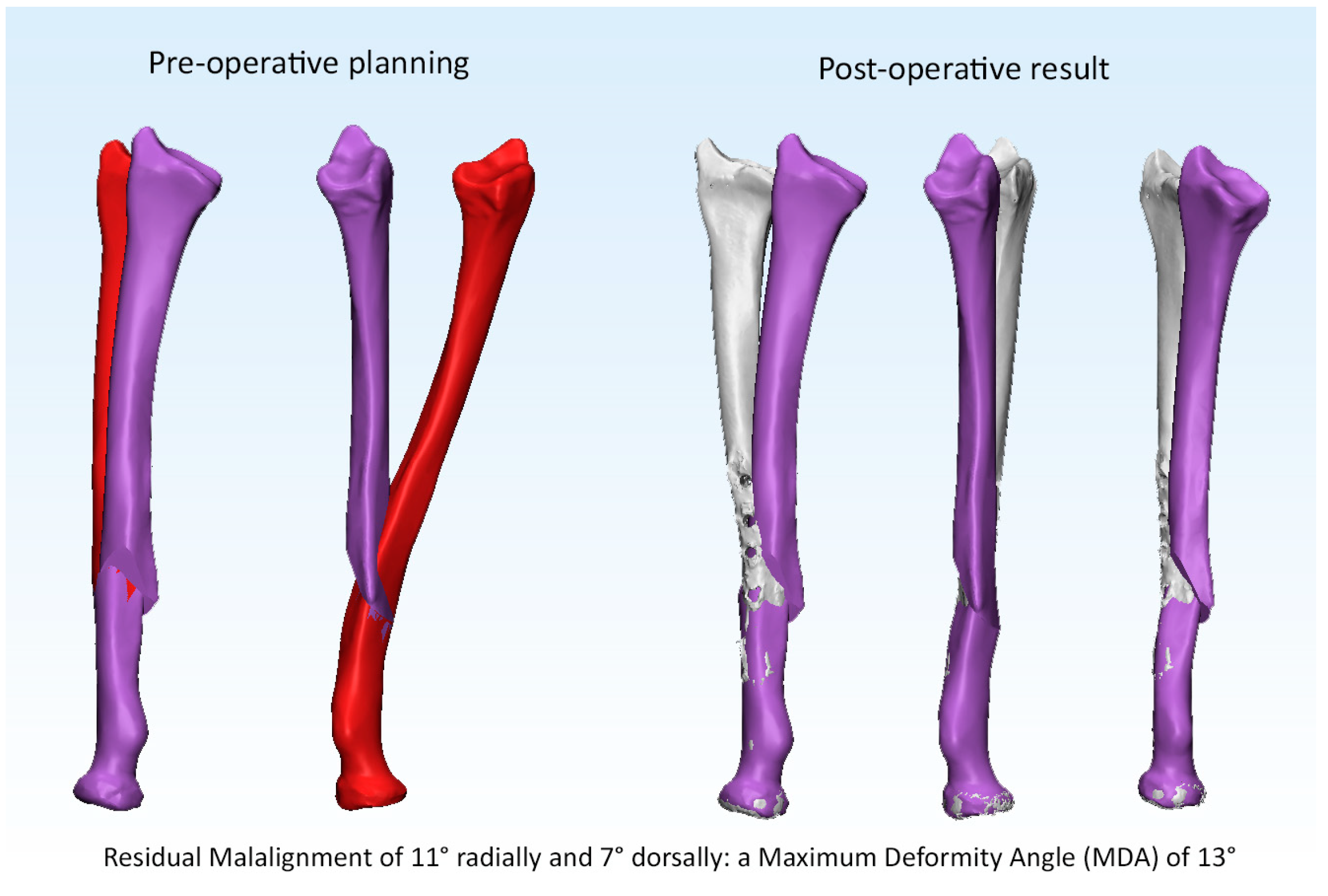
2.2. 3D Radiographic Assessment
2.3. Statistical Analysis
3. Results
3.1. Primary Outcomes
3.2. Is Anatomic Correction Associated with Greater Functional Outcomes?
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hughstone, J.C. Fractures of the forearm in children. J. Bone Jt. Surg.-Am. Vol. 1962, 44, 1678. [Google Scholar] [CrossRef]
- Murase, T.; Oka, K.; Moritomo, H.; Goto, A.; Yoshikawa, H.; Sugamoto, K. Three-dimensional corrective osteotomy of malunited fractures of the upper extremity with use of a computer simulation system. J. Bone Jt. Surg. Ser. A 2008, 90, 2375–2389. [Google Scholar] [CrossRef] [PubMed]
- Oka, K.; Tanaka, H.; Okada, K.; Sahara, W.; Myoui, A.; Yamada, T.; Yamamoto, M.; Kurimoto, S.; Hirata, H.; Murase, T. Three-Dimensional Corrective Osteotomy for Malunited Fractures of the Upper Extremity Using Patient-Matched Instruments: A Prospective, Multicenter, Open-Label, Single-Arm Trial. J. Bone Jt. Surg. Am. 2019, 101, 710–721. [Google Scholar] [CrossRef] [PubMed]
- Jayakumar, P.; Jupiter, J.B. Reconstruction of malunited diaphyseal fractures of the forearm. Hand 2014, 9, 265–273. [Google Scholar] [CrossRef]
- Miyake, J.; Murase, T.; Oka, K.; Moritomo, H.; Sugamoto, K.; Yoshikawa, H. Computer-assisted corrective osteotomy for malunited diaphyseal forearm fractures. J. Bone Jt. Surg. Ser. A 2012, 94, e150.151–e150.111. [Google Scholar] [CrossRef]
- Kataoka, T.; Oka, K.; Murase, T. Rotational Corrective Osteotomy for Malunited Distal Diaphyseal Radius Fractures in Children and Adolescents. J. Hand Surg. 2017, 3, 286.e1–286.e8. [Google Scholar] [CrossRef]
- Byrne, A.M.; Impelmans, B.; Bertrand, V.; Van Haver, A.; Verstreken, F. Corrective Osteotomy for Malunited Diaphyseal Forearm Fractures Using Preoperative 3-Dimensional Planning and Patient-Specific Surgical Guides and Implants. J. Hand Surg. 2017, 42, e836.e1–e836.e12. [Google Scholar] [CrossRef]
- Roth, K.C.; van Es, E.M.; Kraan, G.A.; Verhaar, J.A.N.; Stockmans, F.; Colaris, J.W. Outcomes of 3-D corrective osteotomies for paediatric malunited both-bone forearm fractures. J. Hand Surg. Eur. Vol. 2021, 47, 164–171. [Google Scholar] [CrossRef]
- Nagy, L.; Jankauskas, L.; Dumont, C.E. Correction of forearm malunion guided by the preoperative complaint. Clin. Orthop. Relat Res. 2008, 466, 1419–1428. [Google Scholar] [CrossRef]
- Krettek, C.; Miclau, T.; Grun, O.; Schandelmaier, P.; Tscherne, H. Intraoperative control of axes, rotation and length in femoral and tibial fractures. Technical note. Injury 1998, 29 (Suppl. S3), C29–C39. [Google Scholar] [CrossRef]
- Blossey, R.D.; Krettek, C.; Liodakis, E. [Posttraumatic torsional deformities of the forearm: Methods of measurement and decision guidelines for correction]. Unfallchirurg 2018, 121, 206–215. [Google Scholar] [CrossRef] [PubMed]
- MacDermid, J.; Solomon, G.; Valdes, K.; American Society of Hand, T. Clinical Assessment Recommendations; American Society of Hand Therapists: Chicago, IL, USA, 2015. [Google Scholar]
- Wu, G.; van der Helm, F.C.; Veeger, H.E.; Makhsous, M.; Van Roy, P.; Anglin, C.; Nagels, J.; Karduna, A.R.; McQuade, K.; Wang, X.; et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion--Part II: Shoulder, elbow, wrist and hand. J. Biomech. 2005, 38, 981–992. [Google Scholar] [CrossRef] [PubMed]
- Vroemen, J.C.; Dobbe, J.G.; Strackee, S.D.; Streekstra, G.J. Positioning evaluation of corrective osteotomy for the malunited radius: 3-D CT versus 2-D radiographs. Orthopedics 2013, 36, e193–e199. [Google Scholar] [CrossRef] [PubMed]
- Graham, T.J.; Fischer, T.J.; Hotchkiss, R.N.; Kleinman, W.B. Disorders of the forearm axis. Hand Clin. 1998, 14, 305–316. [Google Scholar] [CrossRef] [PubMed]
- Tarr, R.R.; Garfinkel, A.I.; Sarmiento, A. The effects of angular and rotational deformities of both bones of the forearm. An in vitro study. J. Bone Jt. Surg. Am. 1984, 66, 65–70. [Google Scholar] [CrossRef]
- Abe, S.; Murase, T.; Oka, K.; Shigi, A.; Tanaka, H.; Yoshikawa, H. In Vivo Three-Dimensional Analysis of Malunited Forearm Diaphyseal Fractures with Forearm Rotational Restriction. J. Bone Jt. Surg. Am. 2018, 100, e113. [Google Scholar] [CrossRef]
- Kataoka, T.; Oka, K.; Miyake, J.; Omori, S.; Tanaka, H.; Murase, T. 3-Dimensional prebent plate fixation in corrective osteotomy of malunited upper extremity fractures using a real-sized plastic bone model prepared by preoperative computer simulation. J. Hand Surg. Am. 2013, 38, 909–919. [Google Scholar] [CrossRef]
- Tevanov, I.; Liciu, E.; Chirila, M.; Dusca, A.; Ulici, A. The use of 3D printing in improving patient-doctor relationship and malpractice prevention. Rom. J. Leg. Med. 2017, 25, 279–282. [Google Scholar] [CrossRef]
- Kasten, P.; Krefft, M.; Hesselbach, J.; Weinberg, A.M. How does torsional deformity of the radial shaft influence the rotation of the forearm? A biomechanical study. J. Orthop. Trauma. 2003, 17, 57–60. [Google Scholar] [CrossRef]
- Tynan, M.C.; Fornalski, S.; McMahon, P.J.; Utkan, A.; Green, S.A.; Lee, T.Q. The effects of ulnar axial malalignment on supination and pronation. J. Bone Jt. Surg. Ser. A 2000, 82, 1726–1731. [Google Scholar] [CrossRef]
- Jeuken, R.M.; Hendrickx, R.P.M.; Schotanus, M.G.M.; Jansen, E.J. Near-anatomical correction using a CT-guided technique of a forearm malunion in a 15-year-old girl: A case report including surgical technique. Orthop. Traumatol. Surg. Res. 2017, 103, 783–790. [Google Scholar] [CrossRef] [PubMed]
- Bauer, A.S.; Storelli, D.A.R.; Sibbel, S.E.; McCarroll, H.R.; Lattanza, L.L. Preoperative computer simulation and patient-specific guides are safe and effective to correct forearm deformity in children. J. Pediatr. Orthop. 2017, 37, 504–510. [Google Scholar] [CrossRef] [PubMed]
- Trousdale, R.T.; Linscheid, R.L. Operative treatment of malunited fractures of the forearm. J. Bone Jt. Surg. Ser. A 1995, 77, 894–902. [Google Scholar] [CrossRef] [PubMed]
- Roth, K.C.; Walenkamp, M.M.J.; van Geenen, R.C.I.; Reijman, M.; Verhaar, J.A.N.; Colaris, J.W. Factors determining outcome of corrective osteotomy for malunited paediatric forearm fractures: A systematic review and meta-analysis. J. Hand Surg. Eur.Vol. 2017, 42, 810–816. [Google Scholar] [CrossRef] [PubMed]



| Radius | Ulna | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Operative | Final Follow-Up | Pre-Operative | Final Follow-Up | |||||||||||||
| Pt | Cor | Sag | MDA | Ax | Cor | Sag | MDA | RM | Cor | Sag | MDA | Ax | Cor | Sag | MDA | RM |
| 1 | 3 | 14 | 14 | −6 | 0 | 0 | 0 | 6 | 6 | −5 | 7 | 32 | −5 | 5 | 7 | −12 |
| 2 | 9 | 22 | 23 | 24 | 0 | 0 | 1 | −2 | 16 | 1 | 16 | −1 | 1 | 0 | 1 | 15 |
| 3 | −4 | 8 | 8 | −11 | −3 | 0 | 3 | −9 | 8 | −6 | 11 | −4 | 1 | 0 | 1 | −16 |
| 4 | 0 | 17 | 17 | −26 | 11 | 7 | 13 | −6 | 8 | −20 | 21 | 11 | 1 | −1 | 2 | 2 |
| 5 | −2 | 22 | 23 | −8 | −1 | 0 | 1 | 14 | 9 | −7 | 11 | 0 | 0 | 0 | 0 | 4 |
| 6 | 7 | 27 | 27 | −31 | 0 | −3 | 3 | −3 | 8 | −18 | 19 | 6 | 1 | 0 | 1 | 3 |
| 7 | −11 | 0 | 11 | −13 | 1 | −1 | 1 | −4 | −7 | 19 | 20 | 3 | 0 | 1 | 1 | −5 |
| 8 | 5 | 18 | 19 | 18 | −1 | −1 | 1 | −8 | 11 | 2 | 11 | −1 | −1 | 0 | 1 | 3 |
| 9 | 0 | 16 | 16 | 1 | −1 | −1 | 2 | 10 | 6 | −5 | 8 | −7 | 0 | −1 | 1 | 0 |
| 10 | 17 | 24 | 29 | −4 | 0 | −2 | 2 | −5 | 1 | −13 | 13 | 13 | −1 | −1 | 2 | 9 |
| 11 | 6 | 19 | 20 | −12 | 3 | 3 | 5 | 0 | 3 | −15 | 15 | −4 | 0 | 0 | 0 | 0 |
| 12 | 1 | 11 | 11 | 49 | −1 | 0 | 1 | −1 | 5 | −3 | 6 | −3 | −1 | −4 | 4 | 5 |
| 13 | 9 | 4 | 10 | 15 | −2 | 4 | 5 | 17 | 7 | 2 | 7 | −20 | 0 | 2 | 2 | 0 |
| 14 | −2 | 6 | 6 | −5 | 1 | 1 | 1 | −10 | 13 | −1 | 13 | −7 | 0 | 1 | 1 | −1 |
| 15 | −7 | 3 | 7 | −17 | 2 | 0 | 2 | −3 | 4 | 3 | 5 | 5 | −2 | −1 | 3 | −6 |
| Mean | 8.1 | 14.0 | 16.1 | 15.9 | 1.8 | 1.7 | 2.6 | 6.6 | 7.4 | 8.0 | 12.2 | 7.7 | 1.0 | 1.2 | 1.7 | 5.5 |
| SD | 9.4 | 8.4 | 7.2 | 12.4 | 2.7 | 2.0 | 3.1 | 4.8 | 3.7 | 6.9 | 5.2 | 8.7 | 1.2 | 1.4 | 1.7 | 5.3 |
| Anatomic Correction (n = 10) | Non-Anatomic Correction (n = 5) | p = | |
|---|---|---|---|
| Pre-op pro-supination | 67° (53–80°) | 66° (36–97°) | 0.97 |
| Pro-supination at FU | 136° (125–148°) | 112° (95–129°) | 0.01 |
| Gain in pro-supination | 70° (55–85°) | 46° (28–85°) | 0.04 |
| Pre-op QUICKDASH | 22 (13–30) | 31 (19–43) | 0.16 |
| QUICKDASH at FU | 13 (10–16) | 17 (14–20) | 0.07 |
| ∆ QUICKDASH | 8 (0–17) | 14 (2–26) | 0.38 |
| NRS pain score | 1.1 (−0.5–2.7) | 3.0 (−0.4–6.4) | 0.18 |
| NRS cosmetics | 2.3 (0.5–4.2) | 4.6 (1.3–8.0) | 0.13 |
| Grip strength (%) | 94 (88–98) | 90 (78–102) | 0.41 |
| Unstandardized Coefficients | |||
|---|---|---|---|
| Model | B | Std. Error | Significance |
| (Constant) | 79.0 | 8.4 | <0.001 |
| Residual malrotation Radius | −2.6 | 1.1 | 0.026 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roth, K.; van Es, E.; Kraan, G.; Eygendaal, D.; Colaris, J.; Stockmans, F. Accuracy of 3D Corrective Osteotomy for Pediatric Malunited Both-Bone Forearm Fractures. Children 2023, 10, 21. https://doi.org/10.3390/children10010021
Roth K, van Es E, Kraan G, Eygendaal D, Colaris J, Stockmans F. Accuracy of 3D Corrective Osteotomy for Pediatric Malunited Both-Bone Forearm Fractures. Children. 2023; 10(1):21. https://doi.org/10.3390/children10010021
Chicago/Turabian StyleRoth, Kasper, Eline van Es, Gerald Kraan, Denise Eygendaal, Joost Colaris, and Filip Stockmans. 2023. "Accuracy of 3D Corrective Osteotomy for Pediatric Malunited Both-Bone Forearm Fractures" Children 10, no. 1: 21. https://doi.org/10.3390/children10010021
APA StyleRoth, K., van Es, E., Kraan, G., Eygendaal, D., Colaris, J., & Stockmans, F. (2023). Accuracy of 3D Corrective Osteotomy for Pediatric Malunited Both-Bone Forearm Fractures. Children, 10(1), 21. https://doi.org/10.3390/children10010021