Bilateral Congenital Knee Dislocation in Colombia: Case Report and Literature Review
Abstract
1. Introduction
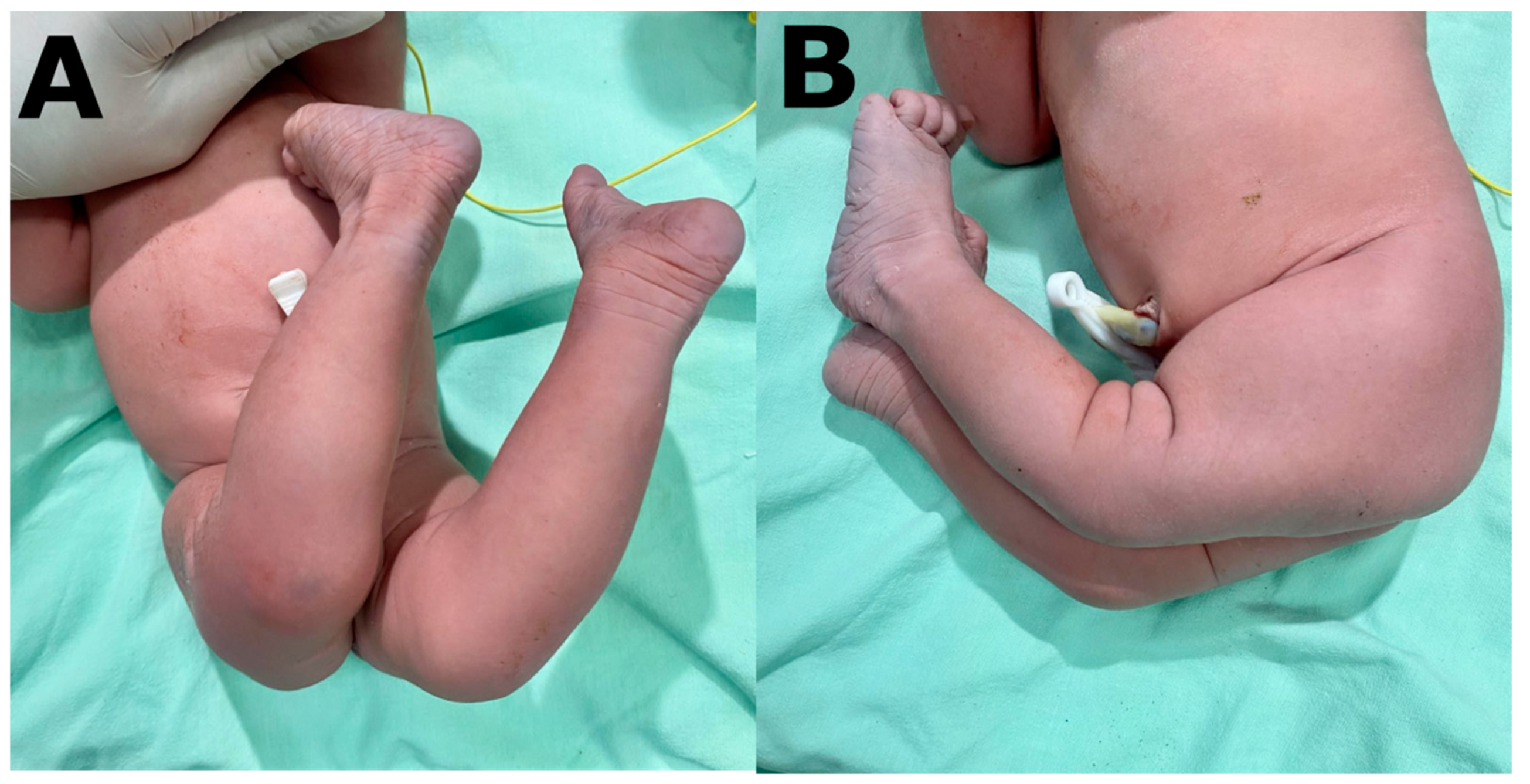
2. Case Presentation
3. Discussion
- Larsen’s syndrome. This describes patients with facial dysmorphism, joint hyperelasticity and multiple dislocations and whose frequency is 1 per 100,000 live births [18].
- Down’s syndrome. Patients may have muscular hypotonia and ligamentous hyperlaxity, which favors the appearance of conditions of this type [19].
- Arthrogryposis. This consists of congenital, non-progressive and symmetrical joint contractures affecting at least two different areas of the human body [20].
- Myelomeningocele, in the condition of paralysis [21].
- These have also been associated, but with less prevalence, with camptodactyly, Ehlers–Danlos syndrome, mongolism, cryptorchidism, angiomas, facial palsy and imperforate anus [1].
- Grade I. Represents hyperextension of the knee joint at birth without displacement of the articular surfaces of the femur in relation to the tibia (the axes of the long bones are opposite each other in the joint line).
- Grade II. Represents subluxation, the tibial epiphysis slipping on the anterior aspect of the femur over the articular surface of the condyle.
- Grade III. Represents total dislocation of the tibial epiphysis in front of the femoral condyles. In our case, the patient corresponded to a grade III.
- If >90° of passive flexion. Treatment will be by serial casts, which are maintained for about 2–4 weeks. Immobilization is performed under control with entry scopy without maintained traction.
- If flexion is 30° to 90°. Initially treated with weekly casts and mobility is re-evaluated after 4 weeks. If >90° is achieved, conservative treatment with casts is maintained, while a quadricipital tenotomy is recommended if flexion after those 4 weeks is still <90°.
- If flexion less than 90° is still maintained after tenotomy, V-Y plasty associated with arthrotomy is recommended. If more than 30° of passive flexion is not achieved, and in case of recurrences, a V-Y plasty associated with an arthrotomy would be performed to release the ligamentous structures that are displaced anteriorly.
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ochoa Del Portillo, G.; Montañez, L.F.D.; Salamanca, L.M.C. Luxación congénita de rodilla bilateral. Reporte de caso. Rev. Colomb. Ortop. Traumatol. 2018, 32, 66–90. [Google Scholar] [CrossRef]
- Morales-Roselló, J.; Loscalzo, G.; Hueso-Villanueva, M.; Buongiorno, S.; Jakaitė, V.; Perales-Marín, A. Congenital Knee Dislocation, Case Report and Review of the Literature. J. Matern. Fetal Neonatal Med. 2022, 35, 809–811. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, K.; Vopalecky, F. Congenital Dislocation of the Knee. Acta Orthop. Scand. 1985, 56, 1–7. [Google Scholar] [CrossRef]
- McFarlane, A.L. A Report on Four Cases of Congenital Genu Recurvatum Occurring in One Family. Br. J. Surg. 2005, 34, 388–391. [Google Scholar] [CrossRef] [PubMed]
- Niebauer, J.J.; King, D.E. Congenital Dislocation of the Knee. J. Bone Joint Surg. Am. 1960, 42-A, 207–225. [Google Scholar] [CrossRef]
- Finder, J.G.; Strange, F.G.S. Congenital Hyperextension of the Knee. J. Bone Joint Surg. 1964, 46, 783. [Google Scholar]
- Katz, M.P.; Grogono, B.J.; Soper, K.C. The Etiology and Treatment of Congenital Dislocation of the Knee. J. Bone Joint Surg. Br. 1967, 49, 112–120. [Google Scholar] [CrossRef]
- PROVENZANO, R.W. Congenital Dislocation of the Knee; Report of a Case. N. Engl. J. Med. 1947, 236, 360–362. [Google Scholar] [CrossRef]
- Mehrafshan, M.; Wicart, P.; Ramanoudjame, M.; Seringe, R.; Glorion, C.; Rampal, V. Congenital Dislocation of the Knee at Birth – Part I: Clinical Signs and Classification. Orthop. Traumatol. Surg. Res. 2016, 102, 631–633. [Google Scholar] [CrossRef]
- Morrissy, R.T.; Weinstein, S.L. Lovell & Winter’s Pediatric Orthopaedics, 6th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2001. [Google Scholar]
- Çıraklı, S.; Çıraklı, A. Neglected Intrauterine Bilateral Congenital Knee Dislocation. Jt. Dis. Relat. Surg. 2021, 32, 542–545. [Google Scholar] [CrossRef]
- Mesa Rivero, M.E.; Cienfuegos López, A.; Holgado Álvarez, M. Tratamiento conservador de la luxación congénita de rodilla. Nuestra experiencia. Rev. S. And. Traum. Ort. 2012, 29, 95–100. [Google Scholar]
- Martínez, P.B.; Pastor, J.Q.; Luna, A.R.; Martín, P.M.; Brik, B.M.; Martín, M.G. Luxación congénita de rodilla. A propósito de un caso. Acta Pediatr Esp. 2007, 65, 183–185. [Google Scholar]
- Lage, J. de A.; Guarniero, R.; de Barros Filho, T.E.; de Camargo, O.P. Intrauterine Diagnosis of Congenital Dislocation of the Knee. J. Pediatr. Orthop. 1986, 6, 110–111. [Google Scholar] [CrossRef] [PubMed]
- Elchalal, U.; Itzhak, I.; Ben-Meir, G.; Zalel, Y. Antenatal Diagnosis of Congenital Dislocation of the Knee: A Case Report. Am. J. Perinatol. 2008, 10, 194–196. [Google Scholar] [CrossRef] [PubMed]
- Gorincour, G.; Chotel, F.; Rudigoz, R.C.; Guibal-Baggio, A.L.; Berard, J.; Pracros, J.P.; Guibaud, L. Prenatal Diagnosis of Congenital Genu Recurvatum Following Amniocentesis Complicated by Leakage: Congenital Genu Recurvatum. Ultrasound Obstet. Gynecol. 2003, 22, 643–645. [Google Scholar] [CrossRef] [PubMed]
- Uguet de Resaire, C.; Martínez Cortés, L.; Rubio López, A.; Ponce Salamanca, S.; Pelayo Delgado, I. Luxación congénita bilateral de rodilla. Prog. Obstet. Ginecol. 2002, 45, 101–105. [Google Scholar] [CrossRef]
- Rampal, V.; Mehrafshan, M.; Ramanoudjame, M.; Seringe, R.; Glorion, C.; Wicart, P. Congenital Dislocation of the Knee at Birth – Part 2: Impact of a New Classification on Treatment Strategies, Results and Prognostic Factors. Orthop. Traumatol. Surg. Res. 2016, 102, 635–638. [Google Scholar] [CrossRef]
- Camacho Franco, L.A.C.; Haces Garcia, F.; Galván Lizárraga, R.; Verdugo Hernández, A. Síndrome de Larsen: 22 casos, evolución y tratamiento. ACTA ORTOPÉDICA Mex. 2007, 21, 20–23. [Google Scholar]
- Zamora, A.A.; Cánovas, C.S. Trastornos ortopédicos en niños con síndrome de Down. Rev. Esp. Pediatría 2012, 68, 5. [Google Scholar]
- Álvarez Quiroz, P.; Yokoyama Rebollar, E. Abordaje clínico y diagnóstico de la artrogriposis. Acta Pediátrica México 2019, 40, 44. [Google Scholar] [CrossRef]
- Abdelaziz, T.H.; Samir, S. Congenital Dislocation of the Knee: A Protocol for Management Based on Degree of Knee Flexion. J. Child. Orthop. 2011, 5, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Hirade, T.; Katsube, K.; Kato, F. Bilateral Congenital Dislocation of the Knee. J. Pediatr. 2021, 229, 299–300. [Google Scholar] [CrossRef] [PubMed]
- Candel, M.; Barra, A.; Chapa, A.; Gascó, J. Luxación congénita irreductible de rodilla. Caso clínico. 2021, 65, 172–179. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salguero-Sánchez, J.A.; Sánchez-Duque, S.A.; Lozada-Martínez, I.D.; Liscano, Y.; Díaz-Vallejo, J.A. Bilateral Congenital Knee Dislocation in Colombia: Case Report and Literature Review. Children 2023, 10, 20. https://doi.org/10.3390/children10010020
Salguero-Sánchez JA, Sánchez-Duque SA, Lozada-Martínez ID, Liscano Y, Díaz-Vallejo JA. Bilateral Congenital Knee Dislocation in Colombia: Case Report and Literature Review. Children. 2023; 10(1):20. https://doi.org/10.3390/children10010020
Chicago/Turabian StyleSalguero-Sánchez, Jefferson Augusto, Santiago Andrés Sánchez-Duque, Ivan David Lozada-Martínez, Yamil Liscano, and Jhony Alejandro Díaz-Vallejo. 2023. "Bilateral Congenital Knee Dislocation in Colombia: Case Report and Literature Review" Children 10, no. 1: 20. https://doi.org/10.3390/children10010020
APA StyleSalguero-Sánchez, J. A., Sánchez-Duque, S. A., Lozada-Martínez, I. D., Liscano, Y., & Díaz-Vallejo, J. A. (2023). Bilateral Congenital Knee Dislocation in Colombia: Case Report and Literature Review. Children, 10(1), 20. https://doi.org/10.3390/children10010020





