Quality of Life in Older Adults with Benign Prostatic Hyperplasia
Abstract
1. Introduction
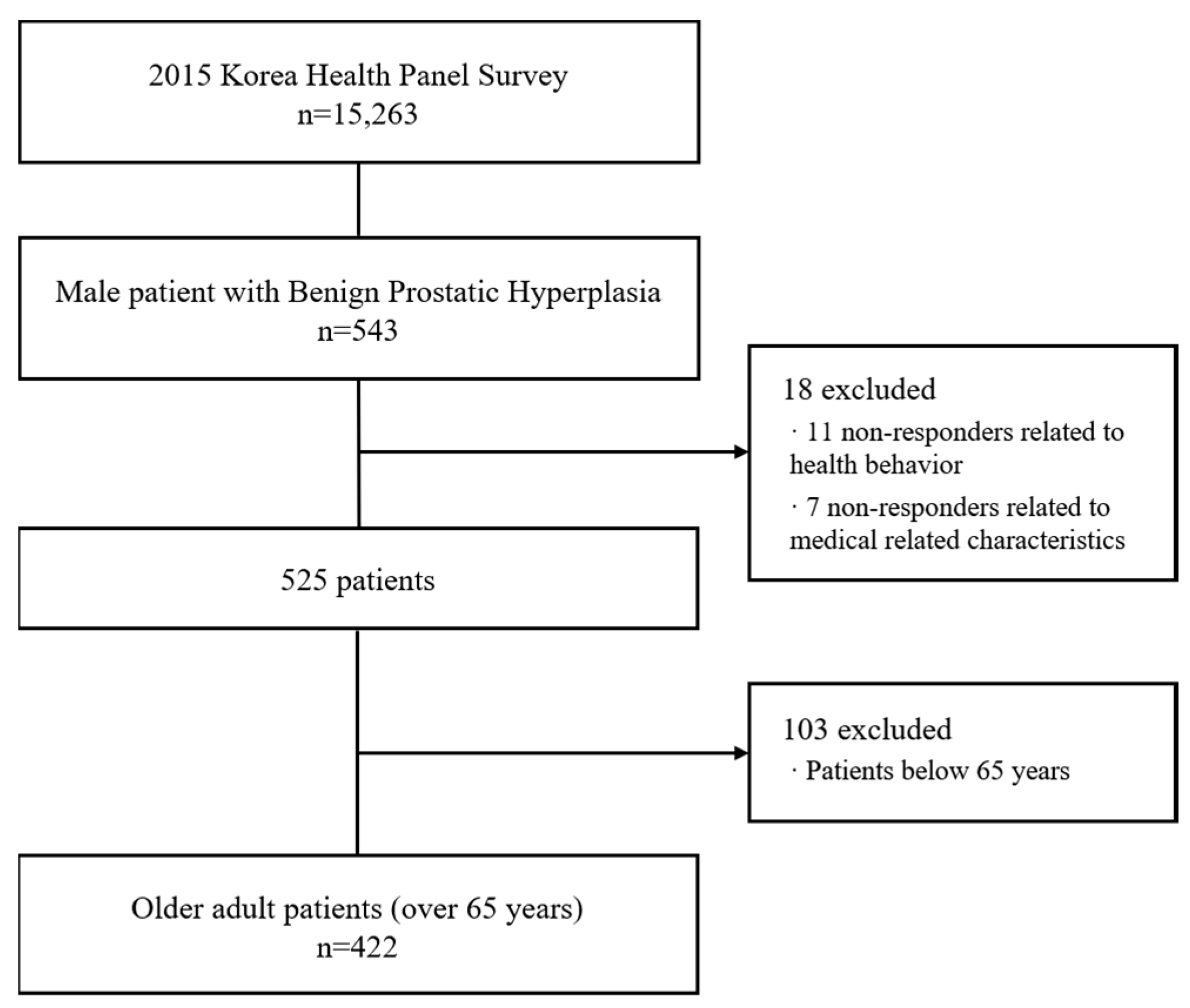
2. Methods
2.1. Data Source
2.2. Description of Variables
2.2.1. General Characteristics of Subjects
2.2.2. Characteristics of Health Behavior and Medical Related Characteristics of Research Subjects
2.2.3. Health Related Quality of Life
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Tourani, S.; Behzadifar, M.; Martini, M.; Aryankhesal, A.; Mirghaed, M.T.; Salemi, M.; Behzadifar, M.; Bragazzi, N.L. Health-related quality of life among healthy elderly Iranians: A systematic review and meta-analysis of the literature. Health Qual. Life Outcomes 2018, 16, 18. [Google Scholar] [CrossRef]
- Lim, W.S.; Wong, S.F.; Leong, I.; Choo, P.; Pang, W.S. Forging a frailty-ready healthcare system to meet population ageing. Int. J. Environ. Res. Public Health 2017, 14, 1448. [Google Scholar] [CrossRef] [PubMed]
- Rowe, J.W.; Fulmer, T.; Fried, L. Preparing for better health and health care for an aging population. Jama 2016, 316, 1643–1644. [Google Scholar] [CrossRef] [PubMed]
- Gusmano, M.K.; Okma, K.G. Population Aging and the Sustainability of the Welfare State. Hastings Cent. Rep. 2018, 48, S57–S61. [Google Scholar] [CrossRef]
- Foster, H.E.; Barry, M.J.; Dahm, P.; Gandhi, M.C.; Kaplan, S.A.; Kohler, T.S.; Lerner, L.B.; Lightner, D.J.; Parsons, J.K.; Roehrborn, C.G. Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline. J. Urol. 2018, 200, 612–619. [Google Scholar] [CrossRef]
- Vignozzi, L.; Gacci, M.; Maggi, M. Lower urinary tract symptoms, benign prostatic hyperplasia and metabolic syndrome. Nat. Rev. Urol. 2016, 13, 108. [Google Scholar] [CrossRef] [PubMed]
- Rohrmann, S.; Katzke, V.; Kaaks, R. Prevalence and progression of lower urinary tract symptoms in an aging population. Urology 2016, 95, 158–163. [Google Scholar] [CrossRef]
- Khalaf, K.M.; Coyne, K.S.; Globe, D.R.; Malone, D.C.; Armstrong, E.P.; Patel, V.; Burks, J. The impact of lower urinary tract symptoms on health-related quality of life among patients with multiple sclerosis. Neurourol. Urodyn. 2016, 35, 48–54. [Google Scholar] [CrossRef]
- Karimi, M.; Brazier, J. Health, health-related quality of life, and quality of life: What is the difference? Pharmacoeconomics 2016, 34, 645–649. [Google Scholar] [CrossRef]
- Barry, M.J. Evaluation of symptoms and quality of life in males with benign prostatic hyperplasia. Urology 2001, 58, 25–32. [Google Scholar] [CrossRef]
- Braeckman, J.; Denis, L. Management of BPH then 2000 and now 2016–From BPH to BPO. Asian J. Urol. 2017, 4, 138–147. [Google Scholar] [CrossRef] [PubMed]
- Kosilov, K.; Loparev, S.; Kuzina, I.; Kosilova, L.; Ivanovskaya, M.; Prokofyeva, A. Health-related quality of life’s dependence on socio-economic status and demographic characteristics among males with benign prostatic hyperplasia. Andrologia 2018, 50, e12892. [Google Scholar] [CrossRef] [PubMed]
- Fourcade, R.-O.; Lacoin, F.; Rouprêt, M.; Slama, A.; Le Fur, C.; Michel, E.; Sitbon, A.; Cotté, F.-E. Outcomes and general health-related quality of life among patients medically treated in general daily practice for lower urinary tract symptoms due to benign prostatic hyperplasia. World J. Urol. 2012, 30, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Erkoc, M.; Otunctemur, A.; Besiroglu, H.; Altunrende, F. Evaluation of quality of life in patients undergoing surgery for benign prostatic hyperplasia. Aging Male 2018, 21, 238–242. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Chen, H.; Xue, M.; Liu, H.; Deng, D.; Liufu, L.; Chen, R. Effect of continued self-efficacy health education after discharge on patients with benign prostatic hyperplasia. Mod. Clin. Nurs. 2016, 15, 70–74. [Google Scholar]
- Hammarsten, J.; Högstedt, B. Clinical Anthropometric, metabolic and insulin profile of males with fast annual growth rates of benign prostatic hyperplasia. Blood Press. 1999, 8, 29–36. [Google Scholar]
- Parsons, J.K. Benign prostatic hyperplasia and male lower urinary tract symptoms: Epidemiology and risk factors. Curr. Bladder Dysfunct. Rep. 2010, 5, 212–218. [Google Scholar] [CrossRef]
- DiSantostefano, R.L.; Biddle, A.K.; Lavelle, J.P. An evaluation of the economic costs and patient-related consequences of treatments for benign prostatic hyperplasia. BJU Int. 2006, 97, 1007–1016. [Google Scholar] [CrossRef]
- Kim, J.; Kim, T.H.; Park, E.-C.; Cho, W.H. Factors influencing unmet need for health care services in Korea. Asia Pac. J. lPublic Health 2015, 27, NP2555–NP2569. [Google Scholar] [CrossRef]
- Kim, D.; Lim, B.; Kim, C. Relationship between patient satisfaction with medical doctors and the use of traditional Korean medicine in Korea. BMC Complementary Altern. Med. 2015, 15, 355. [Google Scholar] [CrossRef]
- Doo Yong, P.; On, L.; Yeon Soo, K. The Association between Sitting Time, Physical Activity Level and Chronic Kidney Disease in the Healthy Adults. Korean J. Sports Med. 2017, 35, 32–39. [Google Scholar]
- Chun, M.Y. Validity and reliability of korean version of international physical activity questionnaire short form in the elderly. Korean J. Fam. Med. 2012, 33, 144. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.J.; Kang, M.-Y. Chronic diseases, health behaviors, and demographic characteristics as predictors of ill health retirement: Findings from the Korea Health Panel Survey (2008–2012). PLoS ONE 2016, 11, e0166921. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.E.; Park, E.-C.; Chun, S.Y.; Park, H.K.; Kim, T.H. Socio-demographic and clinical factors contributing to smoking cessation among men: A four-year follow up study of the Korean Health Panel Survey. BMC Public Health 2016, 16, 908. [Google Scholar] [CrossRef]
- Park, B.; Ock, M.; Lee, H.A.; Lee, S.; Han, H.; Jo, M.-W.; Park, H. Multimorbidity and health-related quality of life in Koreans aged 50 or older using KNHANES 2013–2014. Health Qual. Life Outcomes 2018, 16, 186. [Google Scholar] [CrossRef]
- Joe, S.; Lee, I.; Park, B. Factors influencing health-related quality of life of young adults and elderly with multimorbiditiy: A secondary analysis of the 2013 Korea Health Panel data. J. Korean Acad. Community Health Nurs. 2016, 27, 358–369. [Google Scholar] [CrossRef]
- Ju, Y.J.; Kim, T.H.; Han, K.-T.; Lee, H.J.; Kim, W.; Ah Lee, S.; Park, E.-C. Association between unmet healthcare needs and health-related quality of life: A longitudinal study. Eur. J. Public Health 2017, 27, 631–637. [Google Scholar] [CrossRef]
- Roohafza, H.; Sadeghi, M.; Talaei, M.; Pourmoghaddas, Z.; Sarrafzadegan, N. Psychological status and quality of life in relation to the metabolic syndrome: Isfahan Cohort Study. Int. J. Endocrinol. 2012, 2012. [Google Scholar] [CrossRef]
- Localio, A.R.; Margolis, D.J.; Berlin, J.A. Relative risks and confidence intervals were easily computed indirectly from multivariable logistic regression. J. Clin. Epidemiol. 2007, 60, 874–882. [Google Scholar] [CrossRef]
- Norman, G.; Streiner, D. Logistic regression. In Biostatistics: The Bare Essentials; BC Decker Inc.: Hamilton, FL, USA, 2000. [Google Scholar]
- Lee, M.; Yoon, K. Effects of the Health Promotion Programs on Happiness. Sustainability 2020, 12, 528. [Google Scholar] [CrossRef]
- Duong, J.; Bradshaw, C.P. Household income level as a moderator of associations between chronic health conditions and serious mental illness. J. Community Psychol. 2016, 44, 367–383. [Google Scholar] [CrossRef]
- Lee, M.; Park, S.; Lee, K.-S. Relationship between Morbidity and Health Behavior in Chronic Diseases. J. Clin. Med. 2020, 9, 121. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Kim, B.; Kim, S. Poverty and working status in changes of unmet health care need in old age. Health Policy 2016, 120, 638–645. [Google Scholar] [CrossRef] [PubMed]
- De Nunzio, C.; Tubaro, A. BPH: Unmet needs in managing LUTS—A European perspective. Nat. Rev. Urol. 2012, 9, 9. [Google Scholar] [CrossRef]
- Lee, M.; Yoon, K. Catastrophic Health Expenditures and Its Inequality in Households with Cancer Patients: A Panel Study. Processes 2019, 7, 39. [Google Scholar] [CrossRef]
- Lee, M.; Yoon, K.; Choi, M. Private health insurance and catastrophic health expenditures of households with cancer patients in South Korea. Eur. J. Cancer 2018, 27, e12867. [Google Scholar] [CrossRef]
- Koh, J.S.; Ko, H.J.; Wang, S.-M.; Cho, K.J.; Kim, J.C.; Lee, S.-J.; Pae, C.-U. The relationship between depression, anxiety, somatization, personality and symptoms of lower urinary tract symptoms suggestive of benign prostatic hyperplasia. Psychiatry Investig. 2015, 12, 268. [Google Scholar] [CrossRef][Green Version]
- Kim, T.H.; Han, D.H.; Ryu, D.-S.; Lee, K.-S. The impact of lower urinary tract symptoms on quality of life, work productivity, depressive symptoms, and sexuality in Korean males aged 40 years and older: A population-based survey. Int. Neurourol. J. 2015, 19, 120. [Google Scholar] [CrossRef]
- Dunphy, C.; Laor, L.; Te, A.; Kaplan, S.; Chughtai, B. Relationship between depression and lower urinary tract symptoms secondary to benign prostatic hyperplasia. Rev. Urol. 2015, 17, 51. [Google Scholar]
- Pinto, J.D.O.; He, H.G.; Chan, S.W.C.; Wang, W. Health-related quality of life and psychological well-being in males with benign prostatic hyperplasia: An integrative review. Japan J. Nurs. Sci. 2016, 13, 309–323. [Google Scholar] [CrossRef]
- Rebar, A.L.; Duncan, M.J.; Short, C.; Vandelanotte, C. Differences in health-related quality of life between three clusters of physical activity, sitting time, depression, anxiety, and stress. BMC Public Health 2014, 14, 1088. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Park, S.; Choi, M.; Lee, K.-S. Unmet Medical Needs of Patients with Benign Prostate Enlargement. Journal of Clinical Medicine 2020, 9, 895. [Google Scholar] [CrossRef] [PubMed]
- Wolin, K.Y.; GRUBB III, R.L.; Pakpahan, R.; Ragard, L.; Mabie, J.; Andriole, G.L.; Sutcliffe, S. Physical activity and benign prostatic hyperplasia-related outcomes and nocturia. Med. Sci. Sports Exerc. 2015, 47, 581. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.W.; Kim, S.A.; Nam, J.W.; Kim, M.K.; Choi, B.Y.; Moon, H.S. The study about physical activity for subjects with prevention of benign prostate hyperplasia. Int. Neurourol. J. 2014, 18, 155. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Meneguci, J.; Sasaki, J.E.; da Silva Santos, Á.; Scatena, L.M.; Damião, R. Socio-demographic, clinical and health behavior correlates of sitting time in older adults. BMC Public Health 2015, 15, 65. [Google Scholar] [CrossRef] [PubMed]
- Temple, N.J. What Are the Health Implications of Alcohol Consumption? Nutr. J. 2012, 323–334. [Google Scholar] [CrossRef]
- Bradley, C.S.; Erickson, B.A.; Messersmith, E.E.; Pelletier-Cameron, A.; Lai, H.H.; Kreder, K.J.; Yang, C.C.; Merion, R.M.; Bavendam, T.G.; Kirkali, Z. Evidence of the impact of diet, fluid intake, caffeine, alcohol and tobacco on lower urinary tract symptoms: A systematic review. J. Urol. 2017, 198, 1010–1020. [Google Scholar] [CrossRef]
- Temple, N.J. What are the health implications of alcohol consumption? In Beverage Impacts on Health and Nutrition; Springer: Berlin/Heidelberg, Germany, 2016; pp. 69–81. [Google Scholar]
| Characteristic | Categories | N | % |
|---|---|---|---|
| Education | <High school | 362 | 85.8 |
| ≥High school | 60 | 14.2 | |
| Income | <300 | 253 | 60.0 |
| ≥300 | 169 | 40.0 | |
| Economic activity | Y | 270 | 64.0 |
| N | 152 | 36.0 | |
| Type of insurance | National health insurance | 371 | 87.9 |
| Assistance | 51 | 12.1 | |
| Subjective health status | Good | 141 | 33.4 |
| Poor | 281 | 66.6 | |
| Unmet medical care | Y | 79 | 18.7 |
| N | 343 | 81.3 | |
| Chronic disease | Y | 222 | 52.6 |
| N | 200 | 47.4 | |
| Moderate physical activity | Y | 280 | 66.4 |
| N | 142 | 33.6 | |
| Intense physical activity | Y | 220 | 52.1 |
| N | 202 | 47.9 | |
| Sitting time | <8 h | 256 | 60.7 |
| ≥8 h | 166 | 39.3 | |
| Smoking | Y | 50 | 11.8 |
| N | 372 | 88.2 | |
| Drinking | Y | 197 | 46.7 |
| N | 225 | 53.3 |
| Variable (Reference) | B | S.E. | Wald | p | Exp(B) | 95% Cl for Exp(B) | ||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Education (under high school) | Over high school | 0.548 | 0.334 | 2.691 | 0.101 | 1.730 | 0.899 | 3.331 |
| Income (under KRW 3 million) | Over 3 million | −0.179 | 0.222 | 0.649 | 0.420 | 0.836 | 0.541 | 1.292 |
| Economic activity (no) | Yes | 0.903 | 0.241 | 14.064 | 0.000 | 2.467 *** | 1.539 | 3.955 |
| Type of insurance (assistance) | National Health Insurance | 0.785 | 0.311 | 6.371 | 0.012 | 2.193 ** | 1.192 | 4.036 |
| Variable (Reference) | B | S.E. | Wald | p | Exp(B) | 95% Cl for Exp(B) | ||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Subjective health status (good) | Poor | −1.340 | 0.261 | 26.385 | 0.000 | 0.262 *** | 0.157 | 0.437 |
| Unmet medical care (no) | Yes | −1.872 | 0.317 | 34.857 | 0.000 | 0.154 *** | 0.083 | 0.286 |
| Chronic disease (no) | Yes | −0.100 | 0.256 | 0.153 | 0.696 | 0.905 | 0.547 | 1.495 |
| Moderate physical activity (no) | Yes | 0.939 | 0.358 | 6.871 | 0.009 | 2.557 ** | 1.267 | 5.158 |
| Intense physical activity (no) | Yes | −0.124 | 0.340 | 0.133 | 0.715 | 0.883 | 0.453 | 1.721 |
| Sitting time (under 8 h) | Over 8 h | −0.793 | 0.255 | 9.703 | 0.002 | 0.452 ** | 0.275 | 0.745 |
| Smoking (no) | Yes | 0.304 | 0.402 | 0.572 | 0.449 | 1.356 | 0.616 | 2.984 |
| Drinking (no) | Yes | −0.652 | 0.259 | 6.345 | 0.012 | 0.521 ** | 0.314 | 0.865 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, S.; Ryu, J.-m.; Lee, M. Quality of Life in Older Adults with Benign Prostatic Hyperplasia. Healthcare 2020, 8, 158. https://doi.org/10.3390/healthcare8020158
Park S, Ryu J-m, Lee M. Quality of Life in Older Adults with Benign Prostatic Hyperplasia. Healthcare. 2020; 8(2):158. https://doi.org/10.3390/healthcare8020158
Chicago/Turabian StylePark, Sewon, Jeong-min Ryu, and Munjae Lee. 2020. "Quality of Life in Older Adults with Benign Prostatic Hyperplasia" Healthcare 8, no. 2: 158. https://doi.org/10.3390/healthcare8020158
APA StylePark, S., Ryu, J.-m., & Lee, M. (2020). Quality of Life in Older Adults with Benign Prostatic Hyperplasia. Healthcare, 8(2), 158. https://doi.org/10.3390/healthcare8020158






