Alleviation of Plaque and Gingivitis with Dental Water Jet in Regular and Orthodontic Patients: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Data Extraction
- Author, date, study design, and setting.
- Characteristics of the participants: their number, age, and sex.
- Management of the intervention group and the type of water irrigator used.
- Management of the control group.
- Outcomes measured: PI, BI, and GI.
2.4. Data Synthesis and Statistical Analysis
2.5. Quality Assessment
2.6. Assessment of Certainty of Evidence
3. Results
3.1. Search Results
3.2. Characteristics of the Included Studies
3.3. Intergroup Comparison
| Author/Year | Country | Design | Control Groups | Test Groups | Groups Included in This Review | Other Groups not Included in This Review | Total Participants §/Drop Out % | Age Range (Mean) | Male/ Female % | Timing of Outcome Measurements | Outcomes Measured |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (A) Studies compared waterjet to manual floss on regular patients | |||||||||||
| Barnes/2005 [25] | USA | RCT | MB + MF (n = 35) | MB + WJ (n = 35) | 2/3 | SB + WJ | 70/10% | 19–70 | NA | 2 weeks 4 weeks | PI, GI, BoP |
| Rosema/ 2011 [26] | Netherlands | RCT | MB + MF (n = 36) | MB + WJ (n = 36) (standard tip) | 2/3 | MB + WJ (prototype tip) | 72/2.8% | 18–36 (21.8) | 29/71% | 2 weeks 4 weeks | PI, BoP |
| Akram/2015 & [42] | Iraq | RCT | MB alone (n = 15) MB + MF (n = 15) | MB + WJ (n = 15) | 3/3 | NA | 45/0% | 25–50 | NA | 3 weeks 6 weeks | PI, GI, BoP |
| Sasikumar/2016 [43] | India | RCT | MB + MF | MB + WJ | 2/2 | NA | 70/8.6% | 18–38 | 44/56% | 2 weeks 4 weeks | PI, GI, BoP |
| (B) Studies compared waterjet to manual floss on patients with a fixed orthodontic appliance | |||||||||||
| Sharma/2008 [32] | Canada | RCT | MB alone (n = 35) MB + MF (n = 35) | MB + WJ (n = 36) | 3/3 | NA | 106/0.9% | 11–17 (13.6) | 55.7/44.3% | 2 weeks 4 weeks | PI, BoP |
| Bruce/2013 [27] | USA | Split mouth | MB + MF (n = 40) | MB + WJ (n = 40) | 2/2 | NA | 40/0% | 13–20 (15.5) | 52.5/47.5% | 4 weeks | PI, GI, BoP |
| (C) Studies compared waterjet to brushing alone on regular patients | |||||||||||
| Flemmig/1990 [45] | USA | RCT | MB alone (n= 55) | MB + WJ (n= 54) | 2/4 | - CHX irrigation - CHX rinse | 109/ 11% at 3 M, 15.6% at 6 M | (36.6) | NA | 3 months 6 months | PI, GI, BoP |
| Jolkovsky/1990 [28] | USA | RCT | MB alone (n = 15) | MB + WJ (n = 15) | 2/4 | Prof. irr: - 0.12% CHX - 0.04% CHX | 30/3% | 22–75 (56) | 80/20% | 3 months | PI, GI |
| Chaves/1994 [29] | USA | RCT | MB alone (n = 31) | MB + WJ (n = 32) | 2/4 | - 0.125 CHX rinse - 0.04% CHX irr | 63/6.3% | 19–62 | 32/68% | 3 months 6 months | PI, GI, BoP |
| Newman/1994 [30] | Spain, Italy, Germany, France | RCT | MB alone (n = 59) | MB + WJ (n = 58) | 2/3 | zinc sulfate irr | 117/1.7% | 18–75 | NA | 6 months | PI, GI, BoP |
| Flemmig/1995 [44] | Germany | RCT | MB alone (n = 20) | MB + WJ (n = 20) | 2/3 | 0.3% ASA irr | 40/7.5% | 19–75 | NA | 6 months | PI, GI, BoP |
| Cutler/2000 [33] | USA | RCT | MB alone (n = 20) | MB + WJ (n = 20) | 2/3 | No oral hygiene | 40/0% | (Test 40.4) (Control 44) | 45/55% | 2 weeks | PI, GI, BoP |
| Ernst/2004 * [46] | Germany | RCT | MB alone (n = 15) | MB + WJ (Subgingival tip) (n = 15) | 2/3 | Herbal mouth rinse | 30/NA | 46.4 | NA | 4 weeks 8 weeks 3 months | PI, GI, BoP |
| Akram/2015 [42] | Iraq | RCT | MB alone (n = 15) MB + MF (n = 15) | MB + WJ (n = 15) | 3/3 | NA | 45/0% | 25–50 | NA | 3 weeks 6 weeks | PI, GI, BoP |
| Goyal/2018 [34] | Canada | RCT | MB alone (n = 36) | MB + WJ (n = 36) | 2/2 | NA | 72/0% | 25–70 (48.4) | 22/78% | 2 weeks 4 weeks | PI, GI, BoP |
| (D) Studies compared waterjet to brushing alone on patients with a fixed orthodontic appliance | |||||||||||
| Jackson/1991 [31] | USA | Cross over | MB only (n = 20) | MB + WJ (n = 20) | 2/4 | PB only PB + WJ | 20/0% | NA | 40/6% | 4 weeks | PI, GI |
| Burch/1994 [35] | USA | RCT | MB only (n = 15) | MB + WJ (n = 16) | 2/3 | PB + WJ | 31/0% | 21–48 | NA | 4 weeks 8 weeks | PI, GI, BoP |
| Sharma/2008 & [32] | Canada | RCT | MB alone (n = 35) MB + MF (n = 35) | MB + WJ (n = 36) | 3/3 | NA | 106/0.9% | 11–17 (13.6) | 55.7/ 44.3% | 2 weeks 4 weeks | PI, BoP |
| Patel/2015 [47] | India | RCT | MB only (n = 15) | MB + WJ (n = 15) | 2/4 | PB only PB + WJ | 30/0% | 21–22 | NA | 4 weeks 8 weeks | PI, GI |
| Mazzoleni/2019 * [41] | Italy | Split mouth | MB only (n = 20) | MB + WJ (n = 20) | 2/2 | NA | 20/NA | 13–32 | 50/5% | 1 month 3 months 6 months | PI, GI |
3.4. Outcome Measurement Indices
3.5. Outcome Measurement Timepoints
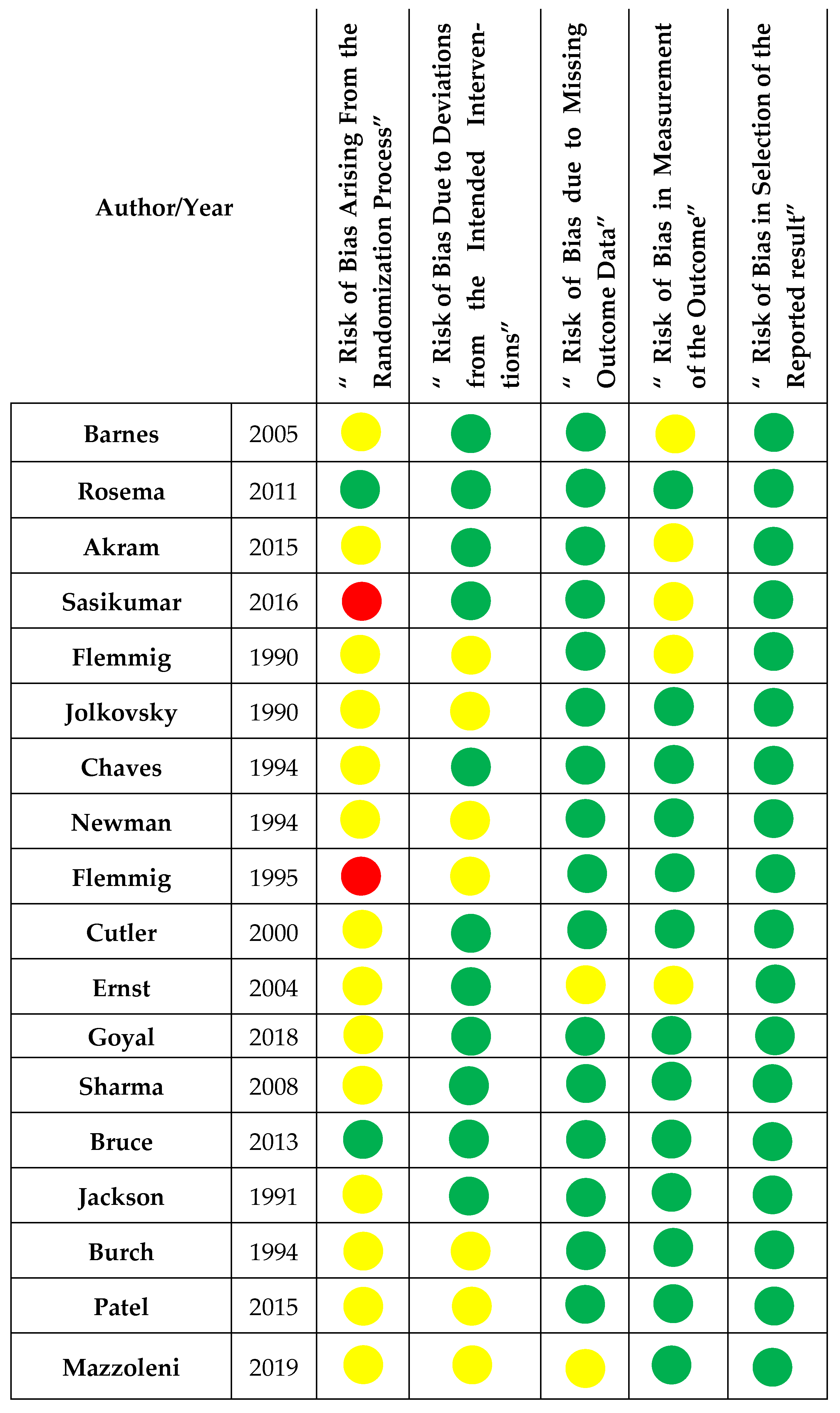
3.6. Risk of Bias
3.7. Descriptive Analysis of the Effect of WJs
3.7.1. Group A Comparison: WJ + MTB vs. Flossing + MTB (Regular Patients, Four Studies)
3.7.2. Group B Comparison: WJ + MTB vs. Flossing + MTB (Orthodontic Patients, Two Studies)
3.7.3. Group C Comparison: WJ + MTB vs. MTB Alone (Regular Patients, Nine Studies)
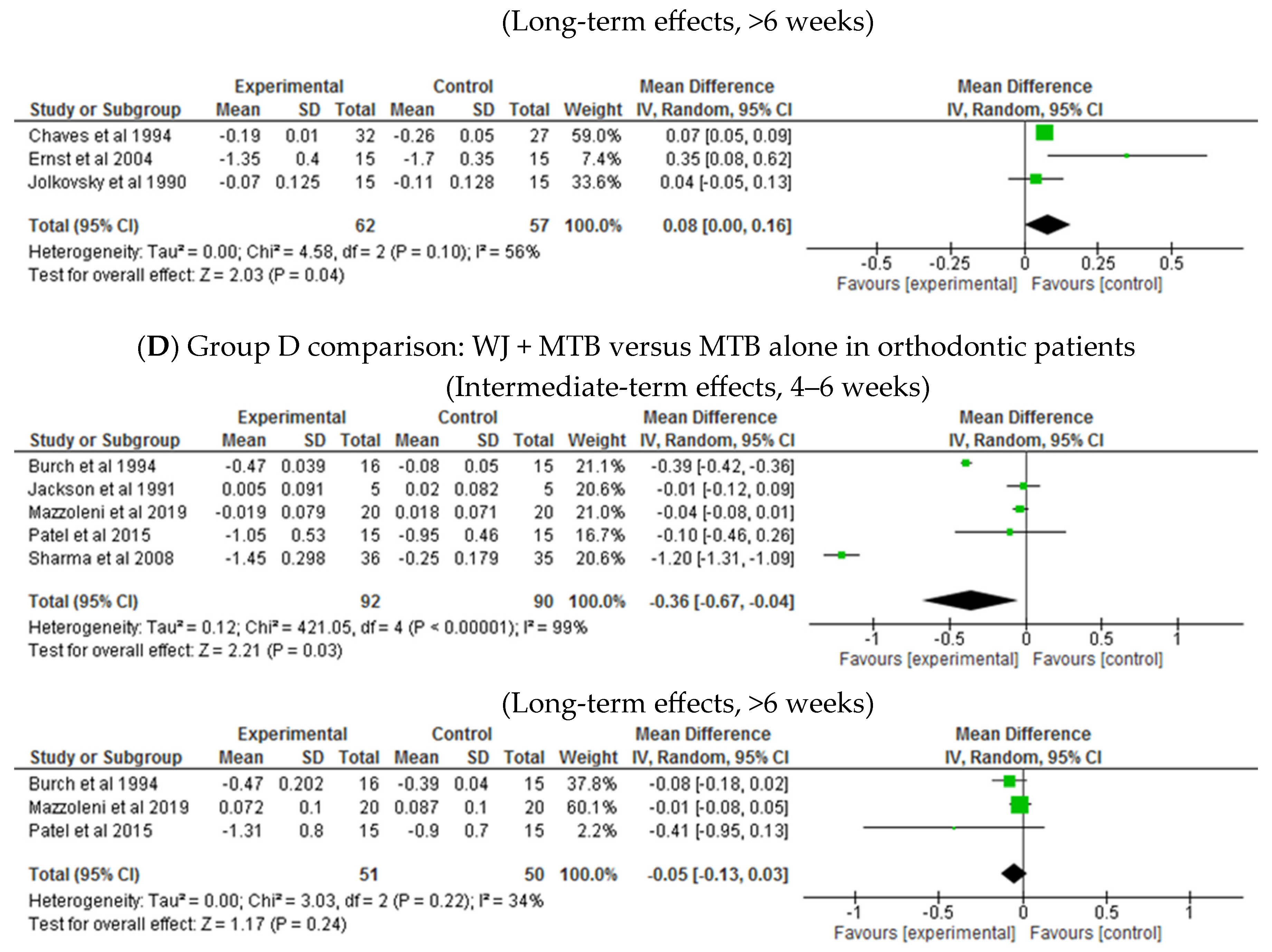
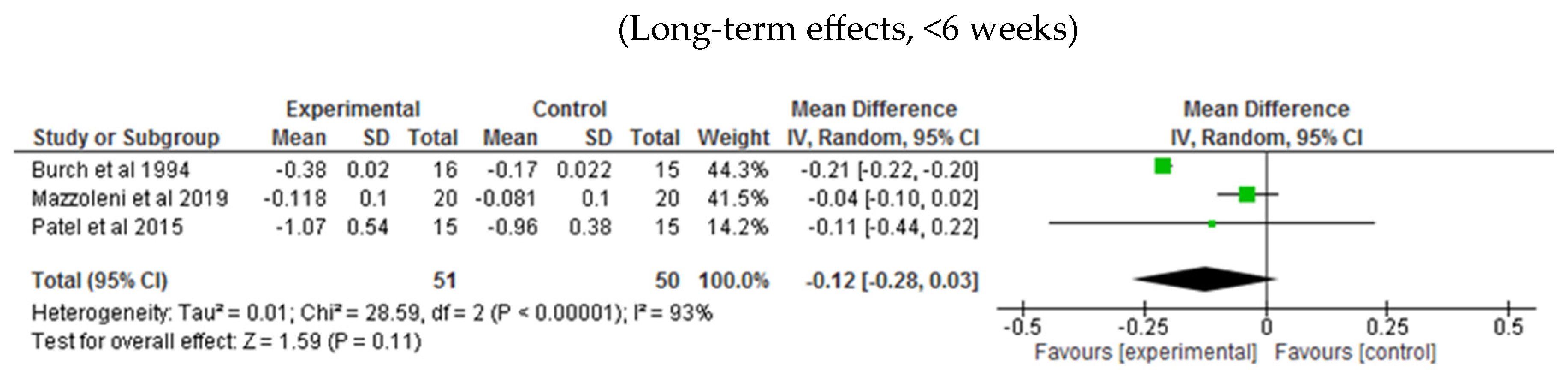
3.7.4. Group D Comparison: WJ + MTB vs. MBT Alone (Orthodontic Patients, Five Studies)
3.8. Quantitative Analysis of the Effect WJ on BI, PI, and GI
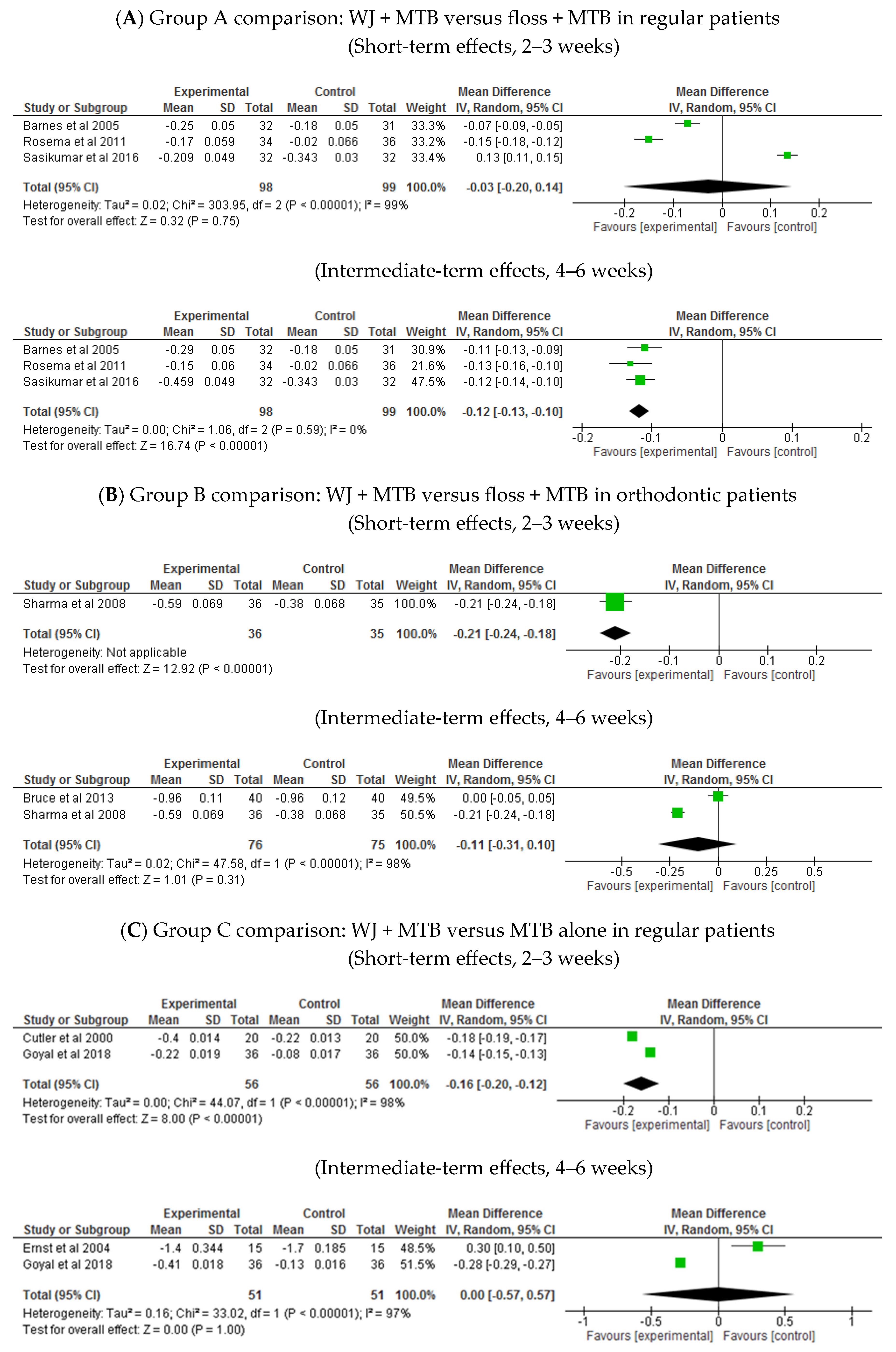
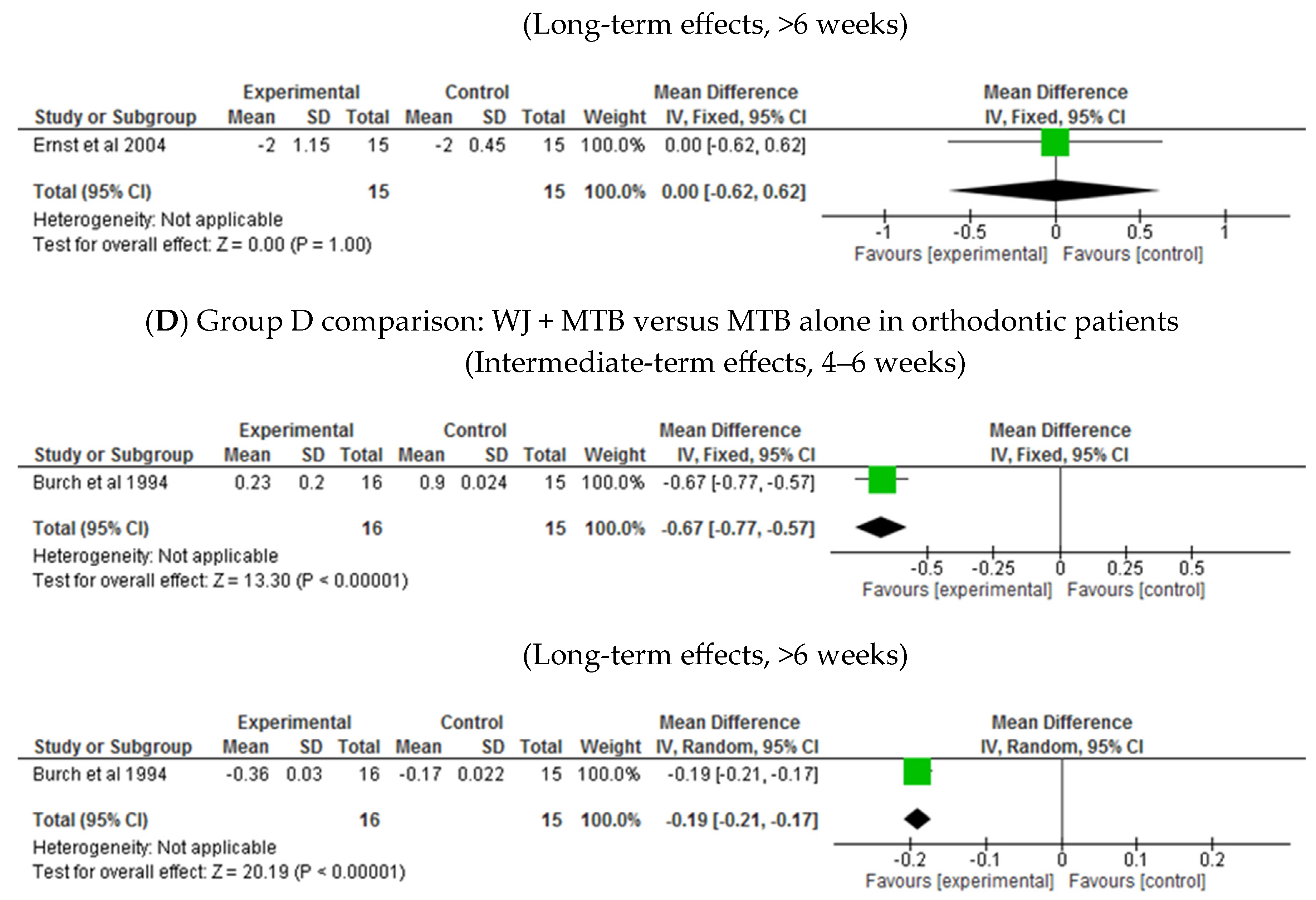
3.8.1. Bleeding Index
- Group A comparison: WJ + MTB versus floss + MTB in regular patients (Table 2: Grade summary of finding One)
- Group B comparison: WJ + MTB versus floss + MTB in orthodontic patients (Table 3: Grade summary of finding Two)
- Group C comparison: WJ + MTB versus MTB alone in regular patients (Table 4: Grade summary of finding Three)
- Group D comparison: WJ + MTB versus MTB alone in orthodontic patients (Table 5: Grade summary of finding Four)
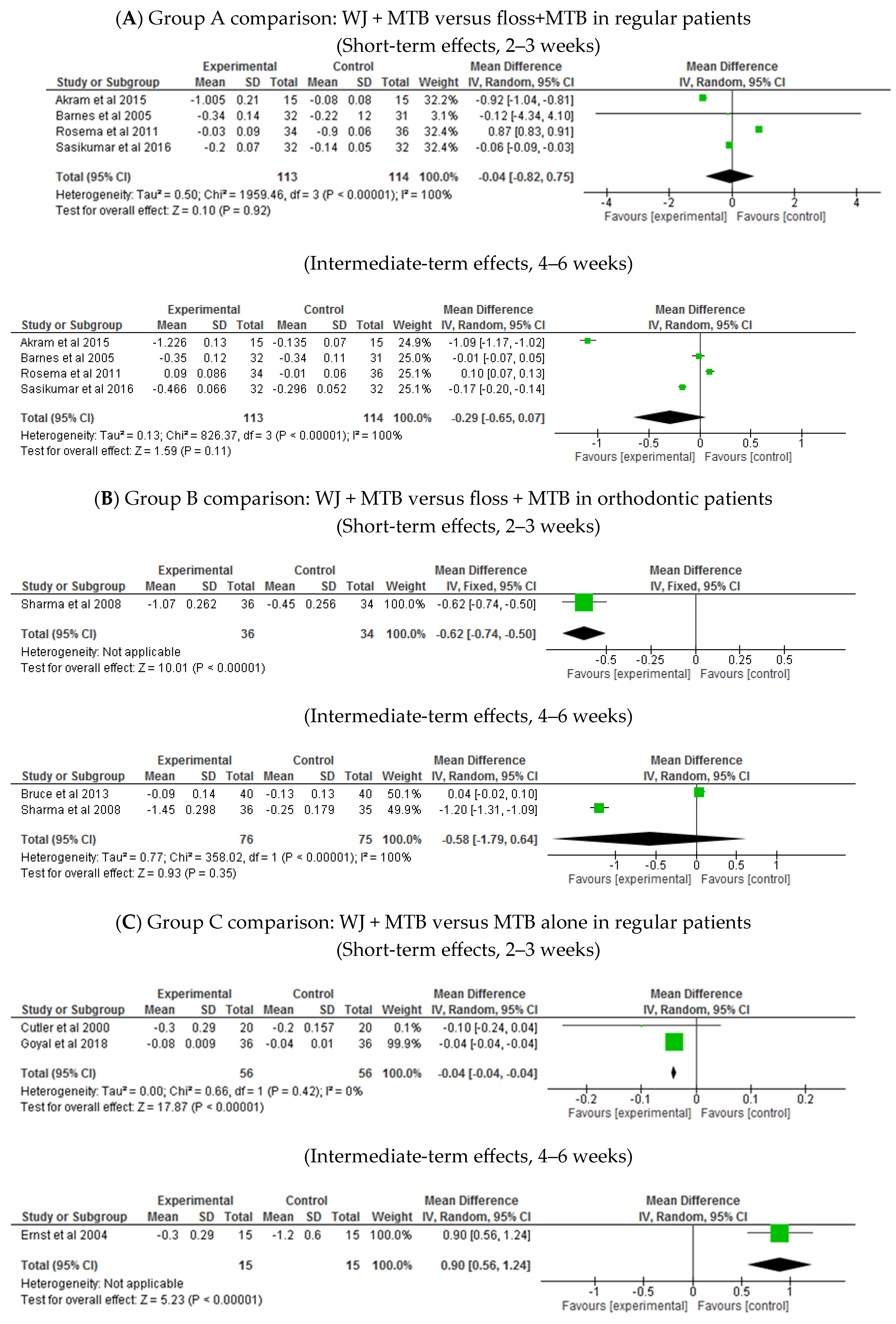
3.8.2. Plaque Index
- Group A comparison: WJ + MTB versus floss + MTB in regular patients (Table 2: Grade summary of finding One)
- Group B comparison: WJ + MTB versus floss + MTB in orthodontic patients (Table 3: Grade summary of finding Two)
- Group C comparison: WJ + MTB versus MTB alone in regular patients (Table 4: Grade summary of finding Three)
- Group D comparison: WJ + MTB versus MTB alone in orthodontic patients (Table 5: Grade summary of finding Four)
3.8.3. Gingival Index
- Group A comparison: WJ + MTB versus floss + MTB in regular patients (Table 2: Grade summary of finding One)
- Group C comparison: WJ + MTB versus MTB alone in regular patients (Table 4: Grade summary of finding Three)
- Group D comparison: WJ + MTB versus MTB alone in orthodontic patients (Table 5: Grade summary of finding Four)
| Patient or population: regular patients. Setting: daily oral care Intervention: waterjet Comparison: manual floss | ||||||
| Outcomes | Anticipated absolute effects * (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Regular floss | Waterjet | |||||
| Reduction in plaque index (PI) (lower scores means less plaque) follow-up: range 4 to 6 weeks | The mean reduction in PI was −0.2 | MD 0.29 lower (0.65 lower to 0.07 higher) | - | 227 (4 RCTs) | ⨁⨁◯◯ Low a,b | In regular patients, results showed equal benefits from waterjet and regular flossing in improving PI at 4–6 weeks. A similar effect was observed also in shorter-term (MD −0.04 [−0.82, 0.75], p = 0.92, 4 trials) |
| Reduction in bleeding index (BI) (lower scores means less bleeding) follow-up: range 4 to 6 weeks | The mean reduction in BI was −0.18 | MD 0.12 lower (0.13 lower to 0.1 lower) | - | 197 (3 RCTs) | ⨁⨁⨁◯ Moderate a | In regular patients, waterjet likely has a slightly better effect than regular floss in improving BI at four weeks and longer; shorter-term results showed no superior benefit for water jet over flossing (MD −0.03 [−0.20, 0.14], p < 0.75, 3 trials) |
| Reduction in gingival index (GI) (lower scores mean lower degree of gingivitis) follow-up: range 4 to 6 weeks | The mean reduction in GI was −0.35 | MD 0.14 lower (0.72 lower to 0.44 higher) | - | 157 (3 RCTs) | ⨁◯◯◯ Very low a,c | In regular patients, waterjet may result in no difference in improving GI over regular flossing; shorter-term results also have no benefit over flossing (MD −0.01 [−0.03, 0.40], p = 0.95, 3 trials) |
| * The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| Patient or population: patients with fixed orthodontic appliance Setting: daily oral care Intervention: water jet Comparison: regular floss | ||||||
| Outcomes | Anticipated absolute effects * (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Regular floss | Water jet | |||||
| Reduction in plaque index (PI) (lower score means less plaque) follow-up: range 4 to 6 weeks | The mean reduction in PI was −0.19 | MD 0.58 lower (1.79 lower to 0.64 higher) | - | 151 (2 RCTs) | ⨁⨁◯◯ Low a | In orthodontic patients, no difference was observed between water jet and manual flossing in improving PI at 4–6 weeks. Shorter-term showed slightly higher benefit for water jet (MD −0.62 [−0.74, −0.50], p < 0.00001, 1 trial) |
| Reduction in bleeding index (BI) (lower score means less bleeding) follow-up: range 4 to 6 weeks | The mean reduction in BI was −0.67 | MD 0.11 lower (0.31 lower to 0.1 higher) | - | 151 (2 RCTs) | ⨁⨁⨁◯ Moderate b | In orthodontic patients, water jet probably had similar effect on bleeding when compared to regular floss at 4–6 weeks; shorter-term showed slightly higher benefit for water jet over floss (MD −0.21 [−0.24, −0.18], p < 0.00001, 1 trial) |
| Reduction in gingival index (GI) not measured | No included studies comparing water jet to regular floss in orthodontic patients reported gingival index. | |||||
| * The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| Patient or population: regular patients Setting: daily oral care Intervention: waterjet plus toothbrushing Comparison: toothbrushing alone | ||||||
| Outcomes | Anticipated absolute effects * (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Toothbrushing alone | Waterjet plus toothbrushing | |||||
| Reduction in plaque index (PI) (lower score means less plaque) follow-up: range 2 to 3 weeks | The mean reduction in PI was −0.12 | MD 0.04 lower (0.04 lower to 0.04 lower) | - | 112 (2 RCTs) | ⨁⨁◯◯ Low a | In regular patients, waterjet plus toothbrushing may result in a very slight difference in improving PI than brushing alone in the short term of 3 weeks. Longer-term evidence (4–6 weeks) showed higher benefit for brushing alone (MD 0.90 [0.56, 1.24], p < 0.00001, 1 trial) as well as three-months data (MD 0.08 [0.00, 0.16], p = 0.04, 3 trial) |
| Reduction in bleeding index (BI) (lower score means less bleeding) follow-up: range 2 to 3 weeks | The mean reduction in BI was −0.15 | MD 0.16 lower (0.2 lower to 0.12 lower) | - | 112 (2 RCTs) | ⨁⨁⨁◯ Moderate b | In regular patients, waterjet plus toothbrushing may improve BI slightly more than brushing alone at 2–3 weeks; longer-term results (1 and 2 months) showed an equal effect of both (MD 0.00 [−0.6, −0.6], p = 1.00, 3 trials) |
| Reduction in gingival index (GI) (lower score means lower degree of gingivitis) follow-up: range 2 to 3 weeks | The mean reduction in GI was −0.13 | MD 0.17 lower (0.23 lower to 0.11 lower) | - | 112( 2 RCTs) | ⨁⨁⨁◯ Moderate b | In regular patients, waterjet plus toothbrushing may improve GI slightly more than brushing alone at 2–3 weeks; longer-term results showed an equal effect of both (MD −0.03 [−0.20, 0.13], p = 0.71, 3 trials) |
| * The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| Patient or population: patients with fixed orthodontic appliance Setting: daily oral care Intervention: waterjet plus toothbrushing Comparison: toothbrushing alone | ||||||
| Outcomes | Anticipated absolute effects * (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Toothbrushing alone | Waterjet plus toothbrushing | |||||
| Reduction in plaque index (PI) (lower score means less plaque) follow-up: range 4 to 6 weeks | The mean reduction in PI was −0.25 | MD 0.36 lower (0.67 lower to 0.04 lower) | - | 182 (5 RCTs) | ⨁◯◯◯ Very low a,b | In orthodontic patients, waterjet may result in a slight additional benefit over regular flossing in improving PI at 4–6 weeks; longer-term results showed no difference over flossing (MD −0.05 [−0.13, 0.03], p = 0.24, 3 trials) |
| Reduction in bleeding index (BI) (lower score means less bleeding) follow-up: range 4 to 6 weeks | The mean reduction in BI was 0.9 | MD 0.67 lower (0.77 lower to 0.57 lower) | - | 31 (1 RCT) | ⨁⨁⨁◯ Moderate c | In orthodontic patients, waterjet may result in slight additional benefit over regular flossing in improving BI at 4 weeks; also, at 2 months (MD −0.19 [−0.21, −0.17], p < 0.00001, 1 trial) |
| Reduction in gingival index (GI) (lower score means lower degree of gingivitis) follow-up: range 4 to 6 weeks | The mean reduction in GI was −0.14 | MD 0.06 lower (0.1 lower to 0.02 lower) | - | 111 (4 RCTs) | ⨁◯◯◯ Very low a,b | In orthodontic patients, waterjet may result in little to no difference in improving GI over brushing alone at 4–6 weeks; in the longer-term, results showed no difference between the two groups (MD −0.12 [−0.28, 0.03], p = 0.11, 3 trials) |
| * The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
4. Discussion
5. Clinical Implications and Recommendation
6. Study Limitations
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Loe, H.; Theilade, E.; Jensen, S.B. Experimental gingivitis in man. J. Periodontol. 1965, 36, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Theilade, E.; Wright, W.H.; Jensen, S.B.; Löe, H. Experimental gingivitis in man: II. A Longitudinal Clinical and Bacteriological Investigation. J. Periodontal Res. 1966, 1, 1–13. [Google Scholar] [CrossRef]
- Sanz, M.; Van Winkelhoff, A.J. Periodontal infections: Understanding the complexity—Consensus of the Seventh European Workshop on Periodontology. J. Clin. Periodontol. 2011, 38 (Suppl. 11), 3–6. [Google Scholar] [CrossRef] [PubMed]
- Marsh, P.D. Dental plaque as a biofilm and a microbial community—Implications for health and disease. BMC Oral Health 2006, 6 (Suppl. 1), S14. [Google Scholar] [CrossRef]
- Abdellatif, H.M.; Burt, B.A. An Epidemiological Investigation into the Relative Importance of Age and Oral Hygiene Status as Determinants of Periodontitis. J. Dent. Res. 1987, 66, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Lindhe, J.; Nyman, S. The effect of plaque control and surgical pocket elimination on the establishment and maintenance of periodontal health. A longitudinal study of periodontal therapy in cases of advanced disease. J. Clin. Periodontol. 1975, 2, 67–79. [Google Scholar] [CrossRef] [PubMed]
- Haffajee, A.D.; Socransky, S.S.; Goodson, J.M. Clinical parameters as predictors of destructive periodontal disease activity. J. Clin. Periodontol. 1983, 10, 257–265. [Google Scholar] [CrossRef]
- Lang, N.P.; Adler, R.; Joss, A.; Nyman, S. Absence of bleeding on probing An indicator of periodontal stability. J. Clin. Periodontol. 1990, 17, 714–721. [Google Scholar] [CrossRef] [PubMed]
- Greenwell, H. Committee on Research, Science and Therapy. American Academy of Periodontology. Position paper: Guidelines for periodontal therapy. J. Periodontol. 2001, 72, 1624–1628. [Google Scholar] [CrossRef] [PubMed]
- Lang, N.P.; Cumming, B.R.; Löe, H. Toothbrushing frequency as it relates to plaque development and gingival health. J. Periodontol. 1973, 44, 396–405. [Google Scholar] [CrossRef]
- Alexander, A.G. The effect of frequency of brushing and the type of bristle used on gingival inflammation, plaque and calculus accumulation. Dent. Pract. Dent. Rec. 1970, 20, 347–355. [Google Scholar] [PubMed]
- Van der Weijden, G.A.F.; van Loveren, C. Mechanical plaque removal in step-1 of care. Periodontol 2000 2023. [Google Scholar] [CrossRef] [PubMed]
- Wainwright, J.; Sheiham, A. An analysis of methods of toothbrushing recommended by dental associations, toothpaste and toothbrush companies and in dental texts. Br. Dent. J. 2014, 217, E5. [Google Scholar] [CrossRef] [PubMed]
- Bass, C.C. An effective method of personal oral hygiene. J. La. State Med Soc. 1954, 106, 100–112. [Google Scholar] [PubMed]
- Yaacob, M.; Worthington, H.V.; Deacon, A.S.; Deery, C.; Walmsley, A.D.; Robinson, P.G.; Glenny, A.-M. Powered versus manual toothbrushing for oral health. Cochrane Database Syst. Rev. 2014, 17, CD002281. [Google Scholar] [CrossRef]
- Thomassen, T.M.J.A.; Van der Weijden, F.G.A.; Slot, D.E. The efficacy of powered toothbrushes: A systematic review and network meta-analysis. Int. J. Dent. Hyg. 2022, 20, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Sälzer, S.; Slot, D.E.; Van der Weijden, F.A.; Dörfer, C.E. Efficacy of inter-dental mechanical plaque control in managing gingivitis—A meta-review. J. Clin. Periodontol. 2015, 42, S92–S105. [Google Scholar] [CrossRef] [PubMed]
- Kotsakis, G.A.; Lian, Q.; Ioannou, A.L.; Michalowicz, B.S.; John, M.T.; Chu, H. A network meta-analysis of interproximal oral hygiene methods in the reduction of clinical indices of inflammation. J. Periodontol. 2018, 89, 558–570. [Google Scholar] [CrossRef]
- Worthington, H.V.; MacDonald, L.; Poklepovic Pericic, T.; Sambunjak, D.; Johnson, T.M.; Imai, P.; Clarkson, J.E. Home use of interdental cleaning devices, in addition to toothbrushing, for preventing and controlling periodontal diseases and dental caries. Cochrane Database Syst. Rev. 2019, 4, CD012018. [Google Scholar] [CrossRef] [PubMed]
- Crocombe, L.A.; Brennan, D.S.; Slade, G.D.; Loc, D.O. Is self interdental cleaning associated with dental plaque levels, dental calculus, gingivitis and periodontal disease? J. Periodontal Res. 2012, 47, 188–197. [Google Scholar] [CrossRef] [PubMed]
- Chapple, I.L.C.; Van Der Weijden, F.; Doerfer, C.; Herrera, D.; Shapira, L.; Polak, D.; Madianos, P.; Louropoulou, A.; Machtei, E.; Donos, N.; et al. Primary prevention of periodontitis: Managing gingivitis. J. Clin. Periodontol. 2015, 42 (Suppl. 16), S71–S76. [Google Scholar] [CrossRef] [PubMed]
- Jahn, C.A. The dental water jet: A historical review of the literature. J. Dent. Hyg. JDH 2010, 84, 114–120. [Google Scholar] [PubMed]
- Frascella, J.A.; Fernández, P.; Gilbert, R.D.; Cugini, M. A randomized, clinical evaluation of the safety and efficacy of a novel oral irrigator. Am. J. Dent. 2000, 13, 55–58. [Google Scholar] [PubMed]
- Cobb, C.M.; Rodgers, R.L.; Killoy, W.J. Ultrastructural Examination of Human Periodontal Pockets Following the Use of an Oral Irrigation Device in Vivo. J. Periodontol. 1988, 59, 155–163. [Google Scholar] [CrossRef]
- Barnes, C.M.; Russell, C.M.; Reinhardt, R.A.; Payne, J.B.; Lyle, D.M. Comparison of irrigation to floss as an adjunct to tooth brushing: Effect on bleeding, gingivitis, and supragingival plaque. J Clin Dent. 2005, 16, 71–77. [Google Scholar]
- Rosema, N.A.M.; Hennequin-Hoenderdos, N.L.; Berchier, C.E.; Slot, D.E.; Lyle, D.M.; van der Weijden, G.A. The effect of different interdental cleaning devices on gingival bleeding. J. Int. Acad. Periodontol. 2011, 13, 2–10. [Google Scholar] [PubMed]
- Bruce, J.D. Effect of Philips Sonicare Airfloss on Plaque Index, Gingival Index, and Bleeding Index in Patients with Fixed Orthodontic Appliances. Master’s Thesis, Saint Louis University, St. Louis, MO, USA, 2013. [Google Scholar]
- Jolkovsky, D.L.; Waki, M.Y.; Newman, M.G.; Otomo-Corgel, J.; Madison, M.; Flemmig, T.F.; Nachnani, S.; Nowzari, H. Clinical and microbiological effects of subgingival and gingival marginal irrigation with chlorhexidine gluconate. J. Periodontol. 1990, 61, 663–669. [Google Scholar] [CrossRef] [PubMed]
- Chaves, E.S.; Kornman, K.S.; Manwell, M.A.; Jones, A.A.; Newbold, D.A.; Wood, R.C. Mechanism of irrigation effects on gingivitis. J. Periodontol. 1994, 65, 1016–1021. [Google Scholar] [CrossRef]
- Newman, M.G.; Cattabriga, M.; Etienne, D.; Flemmig, T.; Sanz, M.; Kornman, K.S.; Doherty, F.; Moore, D.J.; Ross, C. Effectiveness of adjunctive irrigation in early periodontitis: Multi-center evaluation. J. Periodontol. 1994, 65, 224–229. [Google Scholar] [CrossRef]
- Jackson, C.L. Comparison between electric toothbrushing and manual toothbrushing, with and without oral irrigation, for oral hygiene of orthodontic patients. Am. J. Orthod. Dentofac. Orthop. 1991, 99, 15–20. [Google Scholar] [CrossRef]
- Sharma, N.C.; Lyle, D.M.; Qaqish, J.G.; Galustians, J.; Schuller, R. Effect of a dental water jet with orthodontic tip on plaque and bleeding in adolescent patients with fixed orthodontic appliances. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 562–565. [Google Scholar] [CrossRef] [PubMed]
- Cutler, C.W.; Stanford, T.W.; Abraham, C.; Cederberg, R.A.; Boardman, T.J.; Ross, C. Clinical benefits of oral irrigation for periodontitis are related to reduction of pro-inflammatory cytokine levels and plaque. J. Clin. Periodontol. 2000, 27, 134–143. [Google Scholar] [CrossRef] [PubMed]
- Goyal, C.R.; Qaqish, J.G.; Schuller, R.; Lyle, D.M. Evaluation of the Addition of a Water Flosser to Manual Brushing on Gingival Health. J. Clin. Dent. 2018, 29, 81–86. [Google Scholar]
- Burch, J.G.; Lanese, R.; Ngan, P. A two-month study of the effects of oral irrigation and automatic toothbrush use in an adult orthodontic population with fixed appliances. Am. J. Orthod. Dentofac. Orthop. 1994, 106, 121–126. [Google Scholar] [CrossRef]
- Husseini, A.; Slot, D.E.; Van der Weijden, G.A. The efficacy of oral irrigation in addition to a toothbrush on plaque and the clinical parameters of periodontal inflammation: A systematic review. Int. J. Dent. Hyg. 2008, 6, 304–314. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- GRADEpro. GDT: GRADEpro Guideline Development Tool [Software], McMaster University and Evidence Prime: Hamilton, ON, Canada, 2024. Available online: https://www.gradepro.org/ (accessed on 1 September 2023).
- Schünemann, H.; Brożek, J.; Guyatt, G.; Oxman, A. (Eds.) GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations; Updated October 2013; The GRADE Working Group: Hamilton, ON, Canada, 2013; Available online: www.guidelinedevelopment.org/handbook (accessed on 1 September 2023).
- Mazzoleni, S.; De Stefani, A.; Bordin, C.; Balasso, P.; Bruno, G.; Gracco, A. Dental water jet efficacy in the plaque control of orthodontic patients wearing fixed appliance: A randomized controlled trial. J. Clin. Exp. Dent. 2019, 11, e957–e963. [Google Scholar] [CrossRef] [PubMed]
- Akram, H.M. Comparison between powerful Waterpik flosser with dental floss as an adjunct to tooth brushing. J. Baghdad Coll. Dent. 2015, 27, 89–92. [Google Scholar] [CrossRef]
- Sasikumar, P.K.; Shanmugam, S.; Devi, S.S.; Kirthika, M. Comparative Evaluation of Oral Irrigator and Dental Floss as an adjunct to Tooth Brushing on Reduction of Plaque and Gingivitis—A Randomized, Single Blind Clinical Study of Rural Patients. J. Appl. Dent. Med. Sci. 2016, 2, 101671413. [Google Scholar]
- Flemmig, T.F.; Epp, B.; Funkenhauser, Z.; Newman, M.G.; Kornman, K.S.; Haubitz, I.; Klaiber, B. Adjunctive supragingival irrigation with acetylsalicyclic acid in periodontal supportive therapy. J. Clin. Periodontol. 1995, 22, 427–433. [Google Scholar] [CrossRef]
- Flemmig, T.F.; Newman, M.G.; Doherty, F.M.; Grossman, E.; Meckel, A.H.; Bakdash, M.B. Supragingival irrigation with 0.06% chlorhexidine in naturally occurring gingivitis. I. 6 Month clinical observations. J. Periodontol. 1990, 61, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Ernst, C.-P.; Pittrof, M.; Fürstenfelder, S.; Willershausen, B. Does professional preventive care benefit from additional subgingival irrigation? Clin. Oral Investig. 2004, 8, 211–218. [Google Scholar] [CrossRef]
- Patel, D.; Mehta, F.; Trivedi, I.; Mehta, N.; Shah, U.; Vaghela, V. Study of the effects of oral irrigation and automatic tooth brush use in orthodontic patients with fixed appliances. J. Orthod. Res. 2015, 3, 4. [Google Scholar]
- Goyal, C.R.; Lyle, D.M.; Qaqish, J.G.; Schuller, R. The addition of a water flosser to power tooth brushing: Effect on bleeding, gingivitis, and plaque. J. Clin. Dent. 2012, 23, 57–63. [Google Scholar]
- Shibly, O.; Ciancio, S.G.; Shostad, S.; Mather, M.; Boardman, T.J. Clinical evaluation of an automatic flossing device vs. manual flossing. J. Clin. Dent. 2001, 12, 63–66. [Google Scholar] [PubMed]
- Mohapatra, S.; Rajpurohit, L.; Mohandas, R.; Patil, S. Comparing the effectiveness of water flosser and dental floss in plaque reduction among adults: A systematic review. J. Indian Soc. Periodontol. 2023, 27, 559–567. [Google Scholar] [CrossRef]
- AlMoharib, H.S.; AlAskar, M.H.; AlShabib, A.N.; Almadhoon, H.W.; AlMohareb, T.S. The effectiveness of dental water jet in reducing dental plaque and gingival bleeding in orthodontic patients: A systematic review and meta-analysis of randomized clinical trials. Int. J. Dent. Hyg. 2024, 22, 56–64. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Badahdah, A.; Hariri, M.A.; Aljohani, M.S.; Alshehri, L.S.; Natto, Z.S. Alleviation of Plaque and Gingivitis with Dental Water Jet in Regular and Orthodontic Patients: A Systematic Review and Meta-Analysis. Healthcare 2025, 13, 396. https://doi.org/10.3390/healthcare13040396
Badahdah A, Hariri MA, Aljohani MS, Alshehri LS, Natto ZS. Alleviation of Plaque and Gingivitis with Dental Water Jet in Regular and Orthodontic Patients: A Systematic Review and Meta-Analysis. Healthcare. 2025; 13(4):396. https://doi.org/10.3390/healthcare13040396
Chicago/Turabian StyleBadahdah, Arwa, Murooj Abdulrahim Hariri, Modi Salman Aljohani, Layan Saad Alshehri, and Zuhair S. Natto. 2025. "Alleviation of Plaque and Gingivitis with Dental Water Jet in Regular and Orthodontic Patients: A Systematic Review and Meta-Analysis" Healthcare 13, no. 4: 396. https://doi.org/10.3390/healthcare13040396
APA StyleBadahdah, A., Hariri, M. A., Aljohani, M. S., Alshehri, L. S., & Natto, Z. S. (2025). Alleviation of Plaque and Gingivitis with Dental Water Jet in Regular and Orthodontic Patients: A Systematic Review and Meta-Analysis. Healthcare, 13(4), 396. https://doi.org/10.3390/healthcare13040396