Arabic Translation, Cultural Adaptation, and Validation of the Hyperhidrosis Disease Severity Scale (Ar-HDSS)
Abstract
1. Introduction
2. Methodology
2.1. Study Design, Participants, and Setting
2.2. Questionnaire
2.2.1. Hyperhidrosis Disease Severity Scale
2.2.2. Hyperhidrosis Quality of Life Index
2.3. Instrument Translation Process
2.4. Psychometric Analysis for Validity and Reliability
2.5. Ethical Considerations
2.6. Statistical Analysis
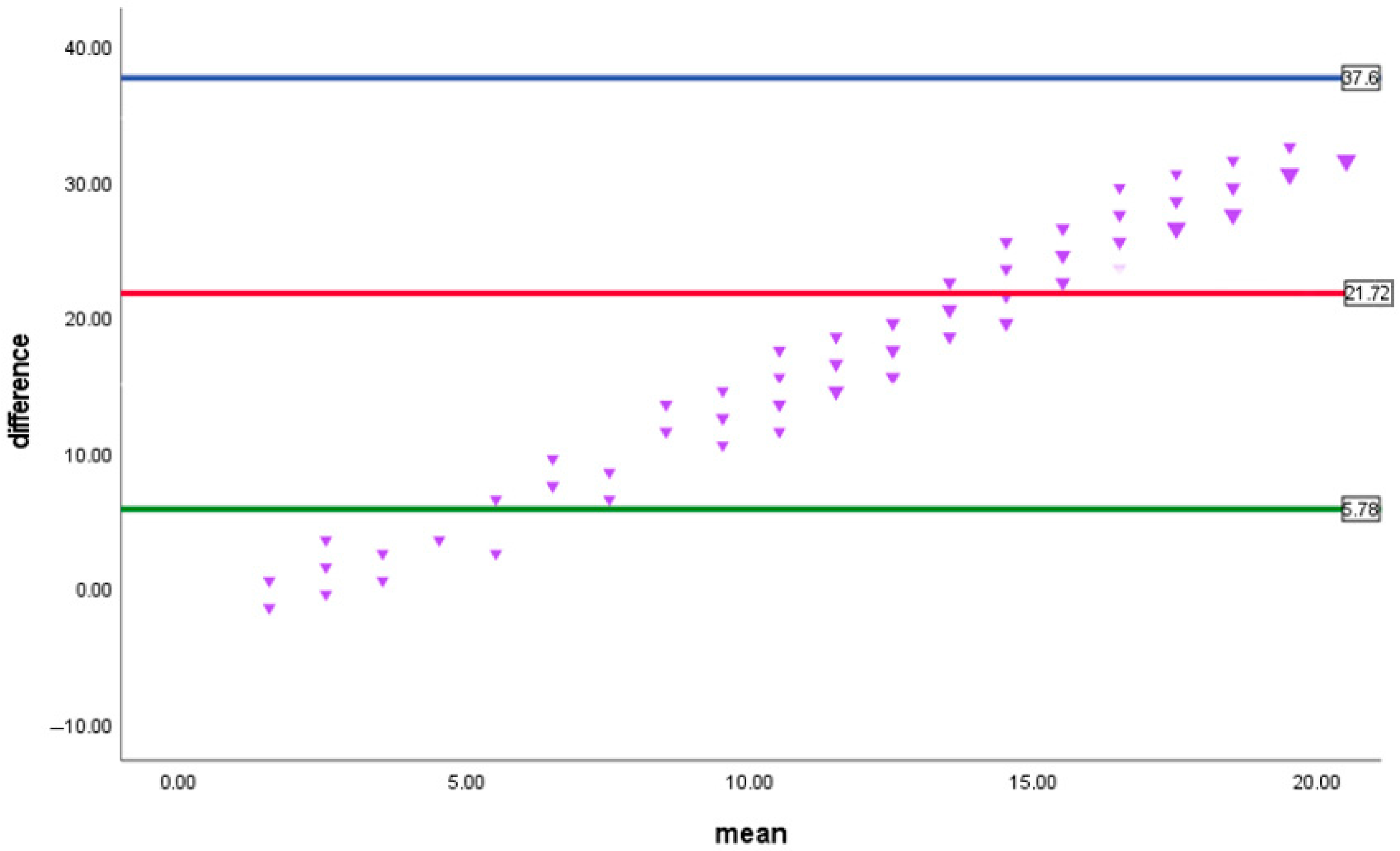
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brackenrich, J.; Fagg, C. Hyperhidrosis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Nawrocki, S.; Cha, J. The Etiology, Diagnosis, and Management of Hyperhidrosis: A Comprehensive Review: Therapeutic Options. J. Am. Acad. Dermatol. 2019, 81, 669–680. [Google Scholar] [CrossRef] [PubMed]
- Kisielnicka, A.; Szczerkowska-Dobosz, A.; Purzycka-Bohdan, D.; Nowicki, R.J. Hyperhidrosis: Disease Aetiology, Classification and Management in the Light of Modern Treatment Modalities. Postepy Dermatol. Allergol. 2022, 39, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Abusailik, M.A.; Mustafa, S.M.B.; Alzboun, H.M.; Al-issa, H.A.; Oweis, S.W.; Alshudeifat, A.Y.; Nawaiseh, M.B. Primary Hyperhidrosis: Prevalence, Severity, and Impact on Quality of Life among Jordanian Patients. Indian J. Dermatol. 2021, 66, 573. [Google Scholar] [CrossRef] [PubMed]
- Sultan, A.A.; Kaliyadan, F.; Aldhafiri, M. The Impact of Primary Hyperhidrosis on Quality Of Life Among Residents In Al-Ahsa City, Saudi Arabia. J. Pharm. Negat. Results 2022, 13, 670–677. [Google Scholar] [CrossRef]
- Strutton, D.R.; Kowalski, J.W.; Glaser, D.A.; Stang, P.E. US Prevalence of Hyperhidrosis and Impact on Individuals with Axillary Hyperhidrosis: Results from a National Survey. J. Am. Acad. Dermatol. 2004, 51, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Doolittle, J.; Walker, P.; Mills, T.; Thurston, J. Hyperhidrosis: An Update on Prevalence and Severity in the United States. Arch. Dermatol. Res. 2016, 308, 743–749. [Google Scholar] [CrossRef] [PubMed]
- Augustin, M.; Radtke, M.A.; Herberger, K.; Kornek, T.; Heigel, H.; Schaefer, I. Prevalence and Disease Burden of Hyperhidrosis in the Adult Population. Dermatol. Basel Switz. 2013, 227, 10–13. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, T.; Kawahara, K.; Yokozeki, H. Epidemiological Study and Considerations of Primary Focal Hyperhidrosis in Japan: From Questionnaire Analysis. J. Dermatol. 2013, 40, 886–890. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Bahar, R.; Kalia, S.; Huang, R.Y.; Phillips, A.; Su, M.; Yang, S.; Zhang, X.; Zhou, P.; Zhou, Y. Hyperhidrosis Prevalence and Demographical Characteristics in Dermatology Outpatients in Shanghai and Vancouver. PLoS ONE 2016, 11, e0153719. [Google Scholar] [CrossRef] [PubMed]
- Kowalski, J.W.; Eadie, N.; Dagget, S.; Lai, P.-Y. Validity and Reliability of the Hyperhidrosis Disease Severity Scale (HDSS)1. J. Am. Acad. Dermatol. 2004, 50, P51. [Google Scholar] [CrossRef]
- Varella, A.Y.M.; Fukuda, J.M.; Teivelis, M.P.; Campos, J.R.M.D.; Kauffman, P.; Cucato, G.G.; Puech-Leão, P.; Wolosker, N. Translation and Validation of Hyperhidrosis Disease Severity Scale. Rev. Assoc. Medica Bras. 1992 2016, 62, 843–847. [Google Scholar] [CrossRef] [PubMed]
- Kamudoni, P.; Mueller, B.; Salek, M.S. The Development and Validation of a Disease-Specific Quality of Life Measure in Hyperhidrosis: The Hyperhidrosis Quality of Life Index (HidroQOL©). Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2015, 24, 1017–1027. [Google Scholar] [CrossRef] [PubMed]
- Donhauser, T.; Apfelbacher, C.; Kann, G.; Masur, C.; Kamudoni, P.; Salek, S.; Abels, C.; Gabes, M. Hyperhidrosis Quality of Life Index (HidroQoL): Further Validation by Applying Classical Test Theory and Item Response Theory Using Data from a Phase III Clinical Trial. J. Patient-Rep. Outcomes 2023, 7, 55. [Google Scholar] [CrossRef] [PubMed]
- Gabes, M.; Jourdan, C.; Schramm, K.; Masur, C.; Abels, C.; Kamudoni, P.; Salek, S.; Apfelbacher, C. Hyperhidrosis Quality of Life Index (HidroQoL©): Further Validation and Clinical Application in Patients with Axillary Hyperhidrosis Using Data from a Phase III Randomized Controlled Trial. Br. J. Dermatol. 2021, 184, 473–481. [Google Scholar] [CrossRef] [PubMed]
- Almuhaideb, Q.A.; AbuDujain, N.M.; Alghamdi, K.M. The Creation of the Arabic Version of the Hyperhidrosis Quality of Life Index (HidroQoL©) with Validation and Cross-Cultural Adaptation. Clin. Cosmet. Investig. Dermatol. 2025, 18, 251–263. [Google Scholar] [CrossRef] [PubMed]
- Lucas, R.E.; Donnellan, M.B. Estimating the Reliability of Single-Item Life Satisfaction Measures: Results from Four National Panel Studies. Soc. Indic. Res. 2011, 105, 323. [Google Scholar] [CrossRef] [PubMed]
- The Arabic Version of the Dermatology Life Quality Index for Morocco: Psychometric Properties in Psoriatics. J. Am. Acad. Dermatol. 2010, 62, AB138. [CrossRef]
| Variable | n (%) | |
|---|---|---|
| Sex | Male | 102 (61.1%) |
| Female | 65 (38.9%) | |
| Age | Mean ± SD | 29 ± 9.02 |
| Range | 16–63 | |
| Nationality | Saudi | 155 (92.8%) |
| Non-Saudi | 12 (7.2%) | |
| Level of education | High-school and below | 27 (16.2%) |
| Bachelor’s degree | 126 (75.4%) | |
| Postgraduate degree | 14 (8.4%) | |
| Monthly income | Less than SAR 5000 | 75 (44.9%) |
| from SAR 5000 to less than SAR 15,000 | 59 (35.3%) | |
| from SAR 15,000 to less than SAR 30,000 | 29 (17.4%) | |
| More than SAR 30,000 | 4 (2.4%) | |
| Chronic medical illness | Yes | 26 (15.7%) |
| No | 141 (84.3%) | |
| Affected Regions | n (%) |
|---|---|
| Axilla | 97 (58.1%) |
| Palms | 133 (79.6%) |
| Soles of the feet | 125 (74.9%) |
| Body trunk | 34 (20.4%) |
| Face and scalp | 41 (24.6%) |
| Genitalia | 25 (15.0%) |
| Scores computed for the number of sites affected | |
| One site only | 20 (12.0%) |
| Two sites | 68 (40.7%) |
| Three sites | 42 (25.1%) |
| Four sites | 21 (12.6%) |
| Five sites | 8 (4.8%) |
| Six sites | 8 (4.8%) |
| Median (IQR) | 2 (2–3) |
| Management used for HH | |
| None | 31 (18.6%) |
| Topical antiperspirants (such as aluminum chloride) | 78 (46.7%) |
| Oral antiperspirants (such as glycopyrrolate or oxybutynin) | 9 (5.4%) |
| Botulinum toxin injection | 56 (33.5%) |
| Anti-hyperhidrosis machine (iontophoresis, radiofrequency, etc.) | 16 (9.6%) |
| Surgical intervention (such as thoracic sympathectomy) | 72 (43.1%) |
| Statement | n (%) |
|---|---|
| My sweating is never noticeable and never interferes with my daily activities. | 3 (1.8%) |
| My sweating is tolerable but sometimes interferes with my daily activities. | 31 (18.6%) |
| My sweating is barely tolerable and frequently interferes with my daily activities. | 44 (26.3%) |
| My sweating is intolerable and always interferes with my daily activities. | 89 (53.3%) |
| r | p Value | |
|---|---|---|
| Daily life domain | 0.41 * | <0.001 |
| Psychological domain | 0.37 * | <0.001 |
| HidroQoL | 0.43 * | <0.001 |
| Sites of involvement score | 0.08 | 0.33 |
| Age | 0.1 | 0.2 |
| Age since HH started | −0.23 | 0.03 |
| Test–Retest Correlation | |||||
|---|---|---|---|---|---|
| Mean | Std. Deviation | Mean Difference | R2 (p Value) | ||
| HDSS tool | (test) | 3.26 | 0.75 | 0.13 ± 0.55 | 0.76 |
| (retest) | 3.13 | 0.81 | |||
| Test–retest level of agreement | |||||
| HDSS tool (retest) | Kappa measure of agreement | ||||
| 2 | 3 | 4 | |||
| HDSS tool (test) | 2 | 4 | 0 | 0 | 0.73 |
| 3 | 1 | 7 | 1 | ||
| 4 | 1 | 1 | 8 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
AbuDujain, N.M.; Almuhaideb, Q.A.; Alghamdi, K.M. Arabic Translation, Cultural Adaptation, and Validation of the Hyperhidrosis Disease Severity Scale (Ar-HDSS). Healthcare 2025, 13, 397. https://doi.org/10.3390/healthcare13040397
AbuDujain NM, Almuhaideb QA, Alghamdi KM. Arabic Translation, Cultural Adaptation, and Validation of the Hyperhidrosis Disease Severity Scale (Ar-HDSS). Healthcare. 2025; 13(4):397. https://doi.org/10.3390/healthcare13040397
Chicago/Turabian StyleAbuDujain, Nasser M., Qais A. Almuhaideb, and Khalid M. Alghamdi. 2025. "Arabic Translation, Cultural Adaptation, and Validation of the Hyperhidrosis Disease Severity Scale (Ar-HDSS)" Healthcare 13, no. 4: 397. https://doi.org/10.3390/healthcare13040397
APA StyleAbuDujain, N. M., Almuhaideb, Q. A., & Alghamdi, K. M. (2025). Arabic Translation, Cultural Adaptation, and Validation of the Hyperhidrosis Disease Severity Scale (Ar-HDSS). Healthcare, 13(4), 397. https://doi.org/10.3390/healthcare13040397






