Excess Weight in Relation to Lifestyle Habits in Spanish First-Year University Students: Differences between Pre- and Post-COVID-19—A Serial Cross-Sectional Study Based on uniHcos Project
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
2.2. Study Variables and Instruments
2.3. Data Analysis
2.4. Ethical Aspects
3. Results
3.1. Prevalence of BMI Categories According to Different Variables
3.2. Relation of BMI and Different Lifestyle Habits
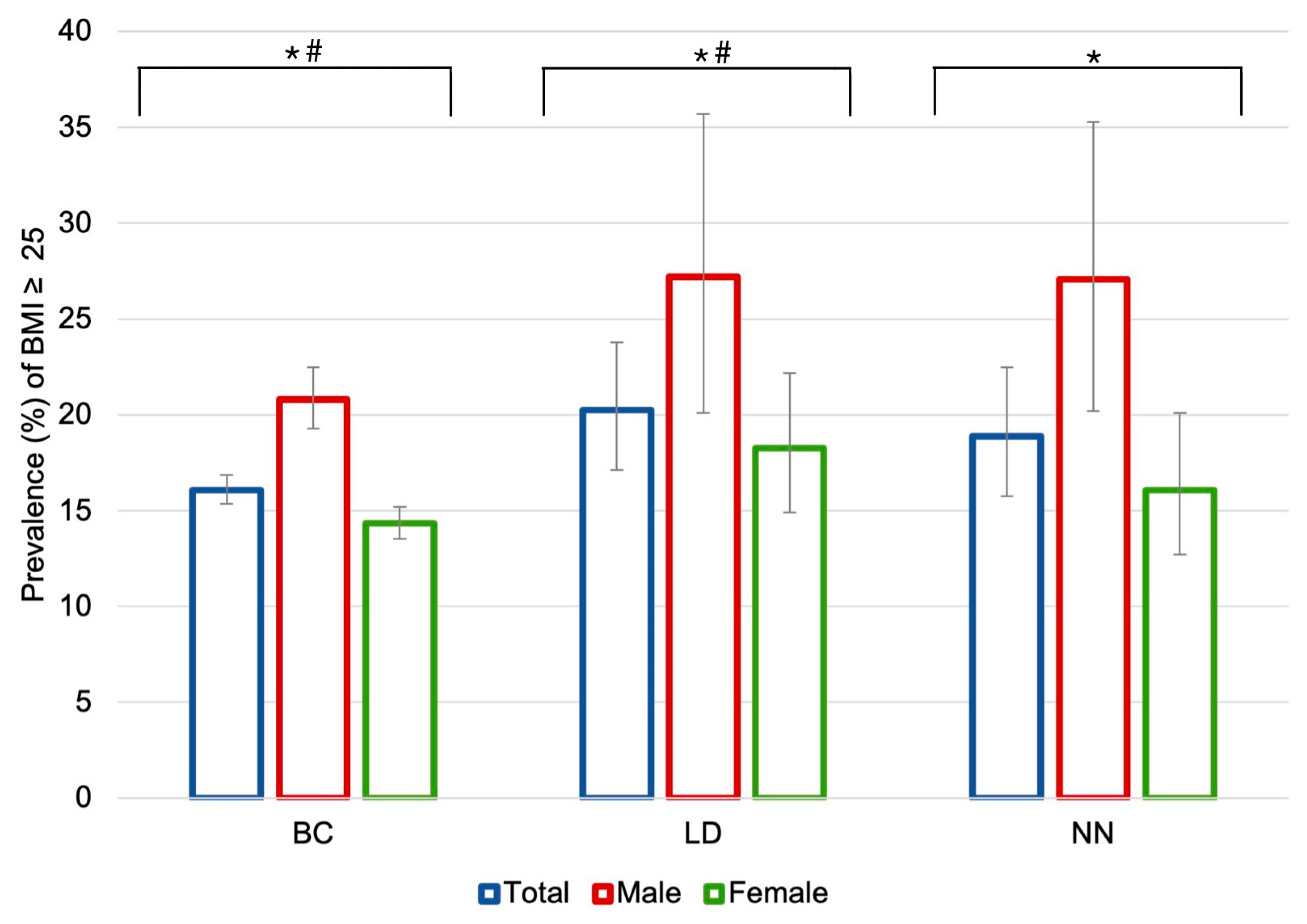
3.3. Differences in BMI by Period of Study and Sex
3.4. Differences in Lifestyle Habits by Period of Study and Sex
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aceijas, C.; Waldhäusl, S.; Lambert, N.; Cassar, S.; Bello-Corassa, R. Determinants of Health-Related Lifestyles among University Students. Perspect. Public Health 2017, 137, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Dietz, P.; Reichel, J.L.; Edelmann, D.; Werner, A.M.; Tibubos, A.N.; Schäfer, M.; Simon, P.; Letzel, S.; Pfirrmann, D. A Systematic Umbrella Review on the Epidemiology of Modifiable Health Influencing Factors and on Health Promoting Interventions Among University Students. Front. Public Health 2020, 8, 137. [Google Scholar] [CrossRef] [PubMed]
- Gropper, H.; John, J.M.; Sudeck, G.; Thiel, A. The Impact of Life Events and Transitions on Physical Activity: A Scoping Review. PLoS ONE 2020, 15, e0234794. [Google Scholar] [CrossRef] [PubMed]
- Maillet, M.A.; Grouzet, F.M.E. Understanding Changes in Eating Behavior during the Transition to University from a Self-Determination Theory Perspective: A Systematic Review. J. Am. Coll. Health 2023, 71, 422–439. [Google Scholar] [CrossRef] [PubMed]
- González Sandoval, C.E.; Díaz Burke, Y.; Mendizabal-Ruiz, P.; Medina Díaz, E.; Morales, J.A. Prevalencia de Obesidad y Perfil Lipídico Alterado En Jóvenes Universitarios. Nutr. Hosp. 2014, 29, 315–321. [Google Scholar] [PubMed]
- Tapera, R.; Merapelo, M.T.; Tumoyagae, T.; Maswabi, T.M.; Erick, P.; Letsholo, B.; Mbongwe, B. The Prevalence and Factors Associated with Overweight and Obesity among University of Botswana Students. Cogent Med. 2017, 4, 1357249. [Google Scholar] [CrossRef]
- Sprake, E.F.; Russell, J.M.; Cecil, J.E.; Cooper, R.J.; Grabowski, P.; Pourshahidi, L.K.; Barker, M.E. Dietary Patterns of University Students in the UK: A Cross-Sectional Study. Nutr. J. 2018, 17, 90. [Google Scholar] [CrossRef]
- Castro, O.; Bennie, J.; Vergeer, I.; Bosselut, G.; Biddle, S.J.H. Correlates of Sedentary Behaviour in University Students: A Systematic Review. Prev. Med. 2018, 116, 194–202. [Google Scholar] [CrossRef]
- Peltzer, K.; Pengpid, S.; Alafia Samuels, T.; Özcan, N.K.; Mantilla, C.; Rahamefy, O.H.; Wong, M.L.; Gasparishvili, A. Prevalence of Overweight/Obesity and Its Associated Factors among University Students from 22 Countries. Int. J. Environ. Res. Public Health 2014, 11, 7425–7441. [Google Scholar] [CrossRef]
- Oluwasanu, A.O.; Akinyemi, J.O.; Oluwasanu, M.M.; Oseghe, O.B.; Oladoyinbo, O.L.; Bello, J.; Ajuwon, A.J.; Jegede, A.S.; Danaei, G.; Akingbola, O. Temporal Trends in Overweight and Obesity and Chronic Disease Risks among Adolescents and Young Adults: A Ten-Year Review at a Tertiary Institution in Nigeria. PLoS ONE 2023, 18, e0283210. [Google Scholar] [CrossRef]
- Kes, D.; Can Cicek, S. Mindful Eating, Obesity, and Risk of Type 2 Diabetes in University Students: A Cross-Sectional Study. Nurs. Forum 2021, 56, 483–489. [Google Scholar] [CrossRef]
- Duan, Y.; Liang, W.; Zhu, L.; Zhang, T.; Wang, L.; Nie, Z.; Chen, Y.; He, L.; Jin, Y.; Yao, Y. Association between Serum Uric Acid Levels and Obesity among University Students (China). Nutr. Hosp. 2015, 31, 2407–2411. [Google Scholar] [CrossRef]
- Xue, B.; Zhang, X.; Li, T.; Gu, Y.; Wang, R.; Chen, W.; Ren, X.; Liu, X.; Chen, G.; Lin, Y.; et al. Knowledge, Attitude, and Practice of Obesity among University Students. Ann. Palliat. Med. 2021, 10, 4539–4546. [Google Scholar] [CrossRef]
- Tárraga López, P.J.; Tárraga Marcos, A.; Panisello Royo, J.M.; Herencia Carbayo, J.A.; Tárraga Marcos, M.L.; López Gil, J.F. Physical Activity and Its Association with Mediterranean Diet Patterns among Spanish University Students. Nutr. Hosp. 2022, 39, 603–609. [Google Scholar] [CrossRef]
- Martínez-Rodríguez, A.; Vidal-Martínez, L.; Martínez-Olcina, M.; Miralles-Amorós, L.; Sánchez-Sáez, J.A.; Ramos-Campo, D.J.; Sánchez-Sánchez, J.; Martínez-Amorós, N.; Cheikh-Moussa, K.; Asencio-Mas, N.; et al. Study the Effect of an Innovative Educational Program Promoting Healthy Food Habits on Eating Disorders, Mediterranean Diet Adherence and Body Composition in University Students. Healthcare 2023, 11, 965. [Google Scholar] [CrossRef]
- Maselli, M.; Ward, P.B.; Gobbi, E.; Carraro, A. Promoting Physical Activity Among University Students: A Systematic Review of Controlled Trials. Am. J. Health Promot. 2018, 32, 1602–1612. [Google Scholar] [CrossRef]
- Antonopoulou, M.; Mantzorou, M.; Serdari, A.; Bonotis, K.; Vasios, G.; Pavlidou, E.; Trifonos, C.; Vadikolias, K.; Petridis, D.; Giaginis, C. Evaluating Mediterranean Diet Adherence in University Student Populations: Does This Dietary Pattern Affect Students’ Academic Performance and Mental Health? Int. J. Health Plan. Manag. 2020, 35, 5–21. [Google Scholar] [CrossRef]
- Reuter, P.R.; Forster, B.L.; Brister, S.R. The Influence of Eating Habits on the Academic Performance of University Students. J. Am. Coll. Health 2021, 69, 921–927. [Google Scholar] [CrossRef]
- Arbués, E.R.; Abadía, B.M.; López, J.M.G.; Serrano, E.E.; García, B.P.; Vela, R.J.; Portillo, S.G.; Guinoa, M.S. Conducta Alimentaria y Su Relación Con El Estrés, La Ansiedad, La Depresión y El Insomnio En Estudiantes Universitarios. Nutr. Hosp. 2019, 36, 1339–1345. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 Guidelines on Physical Activity and Sedentary Behaviour. Br. J. Sports Med. 2020, 54, 20. [Google Scholar] [CrossRef]
- Memon, A.R.; Gupta, C.C.; Crowther, M.E.; Ferguson, S.A.; Tuckwell, G.A.; Vincent, G.E. Sleep and Physical Activity in University Students: A Systematic Review and Meta-Analysis. Sleep Med. Rev. 2021, 58, 101482. [Google Scholar] [CrossRef] [PubMed]
- Vankim, N.A.; Nelson, T.F. Vigorous Physical Activity, Mental Health, Perceived Stress, and Socializing among College Students. Am. J. Health Promot. 2013, 28, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Wunsch, K.; Fiedler, J.; Bachert, P.; Woll, A. The Tridirectional Relationship among Physical Activity, Stress, and Academic Performance in University Students: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 739. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.T.; Tan, C.X.; Tan, S.S. Physical Activity, Sedentary Behavior, and Weight Status of University Students during the COVID-19 Lockdown: A Cross-National Comparative Study. Int. J. Environ. Res. Public Health 2021, 18, 7125. [Google Scholar] [CrossRef]
- Meza-Miranda, E.R.; Parra-Soto, S.L.; Durán-Agüero, S.; Gomez, G.; Carpio-Arias, V.; Ríos-Castillo, I.; Murillo, A.G.; Araneda, J.; Morales, G.; Cavagnari, B.M.; et al. Body Weight in Relation to Hours of Sleep, and Physical Activity in Latin American University Students during the COVID-19 Pandemic. J. Am. Coll. Health 2022, 1–6. [Google Scholar] [CrossRef]
- Bertrand, L.; Shaw, K.A.; Ko, J.; Deprez, D.; Chilibeck, P.D.; Zello, G.A. The Impact of the Coronavirus Disease 2019 (COVID-19) Pandemic on University Students’ Dietary Intake, Physical Activity, and Sedentary Behaviour. Appl. Physiol. Nutr. Metab. 2021, 46, 265–272. [Google Scholar] [CrossRef]
- Dietz, P.; Watson, E.D.; van Poppel, M.; Tibubos, A.N. Editorial: Public Health Promotion in University Students. Front. Public Health 2022, 10, 993982. [Google Scholar] [CrossRef]
- Plotnikoff, R.C.; Costigan, S.A.; Williams, R.L.; Hutchesson, M.J.; Kennedy, S.G.; Robards, S.L.; Allen, J.; Collins, C.E.; Callister, R.; Germov, J. Effectiveness of Interventions Targeting Physical Activity, Nutrition and Healthy Weight for University and College Students: A Systematic Review and Meta-Analysis. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 45. [Google Scholar] [CrossRef]
- Vadeboncoeur, C.; Townsend, N.; Foster, C. A Meta-Analysis of Weight Gain in First Year University Students: Is Freshman 15 a Myth? BMC Obes. 2015, 2, 22. [Google Scholar] [CrossRef]
- Al-Awwad, N.J.; Al-Sayyed, H.F.; Zeinah, Z.A.; Tayyem, R.F. Dietary and Lifestyle Habits among University Students at Different Academic Years. Clin. Nutr. ESPEN 2021, 44, 236–242. [Google Scholar] [CrossRef]
- Vadeboncoeur, C.; Foster, C.; Townsend, N. Freshman 15 in England: A Longitudinal Evaluation of First Year University Student’s Weight Change. BMC Obes. 2016, 3, 45. [Google Scholar] [CrossRef]
- Wilson, O.W.A.; Galascio, M.M.; Bopp, M. Freshmen Weight and Body Composition Change Determinants: A Scoping Review. J. Am. Coll. Health 2021, 69, 298–307. [Google Scholar] [CrossRef]
- Derigny, T.; Schnitzler, C.; Gandrieau, J.; Potdevin, F. Resilience of Adolescents in Physical Activity during the COVID-19 Pandemic: A Preliminary Case Study in France. Phys. Act. Rev. 2022, 10, 86–97. [Google Scholar] [CrossRef]
- Sari, D.K.; Mani, S.; Fadli, M.; Ihksan, R.; Machrina, Y.; Arrasyid, N.K.; Siregar, K.B.; Sunarno, A. Is It Important to Increase Physical Activity among University Students during the Second-Wave COVID-19 Pandemic in Asian Countries? A Cross-Sectional Study of the Knowledge, Attitudes, and Practices in Asian Countries. J. Multidiscip Healthc. 2022, 15, 1559–1571. [Google Scholar] [CrossRef]
- Fernández-Villa, T.; Alguacil-Ojeda, J.; Ayán-Pérez, C.; Bueno-Cavanillas, A.; Cancela-Carral, J.M.; Capelo-Álvarez, R.; Delgado-Rodríguez, M.; Jiménez-Mejías, E.; Jiménez-Moleón, J.J.; Llorca-Díaz, J.; et al. Proyecto UNIHCOS: Cohorte Dinámica de Estudiantes Universitarios Para El Estudio Del Consumo de Drogas y Otras Adicciones. Rev. Esp. Salud Publica 2013, 87, 575–585. [Google Scholar] [CrossRef]
- Concha-Cisternas, Y.; Guzmán-Muñoz, E.; Valdés-Badilla, P.; Lira-Cea, C.; Petermann, F.; Celis-Morales, C. Factores de Riesgo Asociados a Bajo Nivel de Actividad Física y Exceso de Peso Corporal En Estudiantes Universitarios. Rev. Med. Chile 2018, 146, 840–849. [Google Scholar] [CrossRef]
- Cancela, J.; Ayán, C.; Vila, H.; Gutiérrez, J.; Gutiérrez-Santiago, A. Validez de Constructo Del Cuestionario Internacional de Actividad Física En Universitarios Españoles. Rev. Iberoam. Diagn. Eval. Aval. Psicol. 2019, 3, 5–14. [Google Scholar] [CrossRef]
- Rodríguez-Muñoz, S.; Corella, C.; Abarca-Sos, A.; Zaragoza, J. Validation of Three Short Physical Activity Questionnaires with Accelerometers among University Students in Spain. J. Sports Med. Phys. Fit. 2017, 57, 1669–1675. [Google Scholar] [CrossRef]
- Stamatakis, E.; Gale, J.; Bauman, A.; Ekelund, U.; Hamer, M.; Ding, D. Sitting Time, Physical Activity, and Risk of Mortality in Adults. J. Am. Coll. Cardiol. 2019, 73, 2062–2072. [Google Scholar] [CrossRef]
- Medina, C.; Tolentino-Mayo, L.; Ló pez-Ridaura, R.; Barquera, S. Evidence of Increasing Sedentarism in Mexico City during the Last Decade: Sitting Time Prevalence, Trends, and Associations with Obesity and Diabetes. PLoS ONE 2017, 12, e0188518. [Google Scholar] [CrossRef]
- Krebs-Smith, S.M.; Pannucci, T.R.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet. 2018, 118, 1591–1602. [Google Scholar] [CrossRef] [PubMed]
- Grupo Colaborativo de la Sociedad Española de Nutrición Comunitaria (SENC); Aranceta-Bartrina, J.; Arija-Val, V.; Maíz-Aldalur, E.; Martínez de Victoria-Muñoz, E.; Ortega-Anta, R.M.; Pérez-Rodrigo, C.; Quiles-Izquierdo, J.; Rodríguez-Martín, A.; Román-Viñas, B.; et al. Guías alimentarias para la población española; la nueva pirámide de la alimentación saludable. Nutr. Hosp. 2016, 33 (Suppl. 8), 1–48. [Google Scholar] [CrossRef] [PubMed]
- Real Decreto 463/2020, de 14 de Marzo, Por El Que Se Declara El Estado de Alarma Para La Gestión de La Situación de Crisis Sanitaria Ocasionada Por El COVID-19. Boletín Oficial del Estado. Núm. 67, de 14 de Marzo de 2020, Páginas 25390-25400. BOE-A-2020-3692. Available online: https://www.boe.es/eli/es/rd/2020/03/14/463 (accessed on 20 March 2023).
- Real Decreto 926/2020, de 25 de Octubre, Por El Que Se Declara El Estado de Alarma Para Contener La Propagación de Infecciones Causadas Por El SARS-CoV-2. Boletín Oficial del Estado. Núm. 282, de 25 de Octubre de 2020, Páginas 91912-91919. BOE-A-2020-12898. Available online: https://www.boe.es/eli/es/rd/2020/10/25/926 (accessed on 20 March 2023).
- Real Decreto-Ley 8/2021, de 4 de Mayo, Por El Que Se Adoptan Medidas Urgentes En El Orden Sanitario, Social y Jurisdiccional, a Aplicar Tras La Finalización de La Vigencia Del Estado de Alarma Declarado Por El Real Decreto 926/2020, de 25 de Octubre, Por El Que Se Declara El Estado de Alarma Para Contener La Propagación de Infecciones Causadas Por El SARS-CoV-2. Boletín Oficial del Estado. Núm. 107, de 5 de Mayo de 2021, Páginas 53407-53431 BOE-A-2021-7351. Available online: https://www.boe.es/eli/es/rdl/2021/05/04/8 (accessed on 20 March 2023).
- StataCorp. StataCorp 2019. Stata Statistical Software: Release 16; StataCorp LLC: College Station, TX, USA, 2019. [Google Scholar]
- Sun, F.; He, Q.; Sun, X.; Wang, J. The Association between Body Mass Index and Muscular Fitness in Chinese College Freshmen. Int. J. Environ. Res. Public Health 2022, 19, 14060. [Google Scholar] [CrossRef] [PubMed]
- Nicoteri, J.A.L.; Miskovsky, M.J. Revisiting the Freshman “15”: Assessing Body Mass Index in the First College Year and Beyond. J. Am. Assoc. Nurse Pract. 2014, 26, 220–224. [Google Scholar] [CrossRef] [PubMed]
- Wing Kwan, M.Y.; Bray, S.R.; Martin Ginis, K.A. Predicting Physical Activity of First-Year University Students: An Application of the Theory of Planned Behavior. J. Am. Coll. Health 2009, 58, 45–55. [Google Scholar] [CrossRef]
- Pengpid, S.; Peltzer, K. Skipping Breakfast and Its Association with Health Risk Behaviour and Mental Health Among University Students in 28 Countries. Diabetes Metab. Syndr. Obes. 2020, 13, 2889. [Google Scholar] [CrossRef]
- Jalal, S.M.; Beth, M.R.M.; Al-Hassan, H.J.M.; Alshealah, N.M.J. Body Mass Index, Practice of Physical Activity and Lifestyle of Students During COVID-19 Lockdown. J. Multidiscip Healthc. 2021, 14, 1901–1910. [Google Scholar] [CrossRef]
- Deng, Y.; Hwang, Y.J.; Kim, T.; Yli-Piipari, S. Changes in College Students’ Body Mass Index, Physical Activity, and Motivation Before and During the COVID-19 Third-Wave Lockdown. Int. J. Kinesiol. Sports Sci. 2022, 10, 34–41. [Google Scholar] [CrossRef]
- Hao, M.; Fang, Y.; Yan, W.; Gu, J.; Hao, Y.; Wu, C. Relationship between Body Dissatisfaction, Insufficient Physical Activity, and Disordered Eating Behaviors among University Students in Southern China. BMC Public Health 2022, 22, 2054. [Google Scholar] [CrossRef]
- Duan, H.; Gong, M.; Zhang, Q.; Huang, X.; Wan, B. Research on Sleep Status, Body Mass Index, Anxiety and Depression of College Students during the Post-Pandemic Era in Wuhan, China. J. Affect. Disord. 2022, 301, 189–192. [Google Scholar] [CrossRef]
- Shaun, M.M.A.; Nizum, M.W.R.; Munny, S.; Fayeza, F.; Mali, S.K.; Abid, M.T.; Hasan, A.R. Eating Habits and Lifestyle Changes among Higher Studies Students Post-Lockdown in Bangladesh: A Web-Based Cross-Sectional Study. Heliyon 2021, 7, e07843. [Google Scholar] [CrossRef]
- López-Valenciano, A.; Suárez-Iglesias, D.; Sanchez-Lastra, M.A.; Ayán, C. Impact of COVID-19 Pandemic on University Students’ Physical Activity Levels: An Early Systematic Review. Front. Psychol. 2021, 11, 3787. [Google Scholar] [CrossRef]
- Wilson, O.W.A.; Bopp, C.M.; Papalia, Z.; Duffey, M.; Bopp, M. Freshman Physical Activity Constraints Are Related to the Current Health Behaviors and Outcomes of College Upperclassmen. J. Am. Coll. Health 2022, 70, 1112–1118. [Google Scholar] [CrossRef]
- Martínez-de-Quel, Ó.; Suárez-Iglesias, D.; López-Flores, M.; Pérez, C.A. Physical Activity, Dietary Habits and Sleep Quality before and during COVID-19 Lockdown: A Longitudinal Study. Appetite 2021, 158, 105019. [Google Scholar] [CrossRef]
- McCarthy, H.; Potts, H.W.W.; Fisher, A. Physical Activity Behavior Before, during, and After COVID-19 Restrictions: Longitudinal Smartphone-Tracking Study of Adults in the United Kingdom. J. Med. Internet Res. 2021, 23, e23701. [Google Scholar] [CrossRef]
- Hargreaves, E.A.; Lee, C.; Jenkins, M.; Calverley, J.R.; Hodge, K.; Houge Mackenzie, S. Changes in Physical Activity Pre-, During and Post-Lockdown COVID-19 Restrictions in New Zealand and the Explanatory Role of Daily Hassles. Front. Psychol. 2021, 12, 410. [Google Scholar] [CrossRef]
- Kljajević, V.; Stanković, M.; Ðorđević, D.; Trkulja-Petković, D.; Jovanović, R.; Plazibat, K.; Oršolić, M.; Čurić, M.; Sporiš, G. Physical Activity and Physical Fitness among University Students—A Systematic Review. Int. J. Environ. Res. Public Health 2021, 19, 158. [Google Scholar] [CrossRef]
- Romero-Blanco, C.; Rodríguez-Almagro, J.; Onieva-Zafra, M.D.; Parra-Fernández, M.L.; Prado-Laguna, M.D.C.; Hernández-Martínez, A. Physical Activity and Sedentary Lifestyle in University Students: Changes during Confinement Due to the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 6567. [Google Scholar] [CrossRef]
- Rodríguez-Larrad, A.; Mañas, A.; Labayen, I.; González-Gross, M.; Espin, A.; Aznar, S.; Serrano-Sánchez, J.A.; Vera-Garcia, F.J.; González-Lamuño, D.; Ara, I.; et al. Impact of COVID-19 Confinement on Physical Activity and Sedentary Behaviour in Spanish University Students: Role of Gender. Int. J. Environ. Res. Public Health 2021, 18, 369. [Google Scholar] [CrossRef]
- Ten Velde, G.; Lubrecht, J.; Arayess, L.; van Loo, C.; Hesselink, M.; Reijnders, D.; Vreugdenhil, A. Physical Activity Behaviour and Screen Time in Dutch Children during the COVID-19 Pandemic: Pre-, during- and Post-School Closures. Pediatr. Obes. 2021, 16, e12779. [Google Scholar] [CrossRef]
- Peterson, N.E.; Sirard, J.R.; Kulbok, P.A.; DeBoer, M.D.; Erickson, J.M. Sedentary Behavior and Physical Activity of Young Adult University Students. Res. Nurs. Health 2018, 41, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Lamarche, B.; Brassard, D.; Lapointe, A.; Laramée, C.; Kearney, M.; Côté, M.; Bélanger-Gravel, A.; Desroches, S.; Lemieux, S.; Plante, C. Changes in Diet Quality and Food Security among Adults during the COVID-19–Related Early Lockdown: Results from NutriQuébec. Am. J. Clin. Nutr. 2021, 113, 984. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zhao, A.; Ke, Y.; Huo, S.; Ma, Y.; Zhang, Y.; Ren, Z.; Li, Z.; Liu, K. Dietary Behaviors in the Post-Lockdown Period and Its Effects on Dietary Diversity: The Second Stage of a Nutrition Survey in a Longitudinal Chinese Study in the COVID-19 Era. Nutrients 2020, 12, 3269. [Google Scholar] [CrossRef] [PubMed]

| N | % | |
|---|---|---|
| Total | 10,096 | 100 |
| Sex | ||
| Female | 7389 | 73.2 |
| Male | 2707 | 26.8 |
| Period of study | ||
| Before COVID-19 | 9030 | 89.4 |
| Lockdown | 552 | 5.5 |
| New Normal | 514 | 5.1 |
| Residence | ||
| Family household | 4640 | 46.0 |
| Rented apartment | 4006 | 39.7 |
| University hall of residence | 1254 | 12.4 |
| Other | 196 | 1.9 |
| People the student lives with | ||
| Family | 4765 | 47.2 |
| Roommates/Friends | 4509 | 44.7 |
| Alone | 822 | 8.1 |
| Branch of Knowledge | ||
| Social Sciences | 3993 | 39.6 |
| Health Sciences | 2252 | 22.3 |
| Science | 1589 | 15.8 |
| Art and Humanities | 1229 | 12.2 |
| Engineering and Architecture | 1024 | 10.2 |
| BMI | p-Value | ||||
|---|---|---|---|---|---|
| <18.5 kg/m2 | 18.5–24.9 kg/m2 | 25–29.9 kg/m2 | ≥30 kg/m2 | ||
| N (%) | N (%) | N (%) | N (%) | ||
| Total | 1080 (10.7) | 7358 (72.9) | 1347 (13.3) | 311 (3.1) | |
| Sex | <0.001 | ||||
| Female | 925 (12.5) | 5386 (72.9) | 869 (11.8) | 209 (2.8) | |
| Male | 155 (5.7) | 1972 (72.8) | 478 (17.7) | 102 (3.8) | |
| Physical activity | <0.001 | ||||
| Meets WHO criteria | 808 (10.2) | 5824 (73.7) | 1053 (13.3) | 220 (2.8) | |
| Does not meet WHO criteria | 272 (12.4) | 1534 (70.0) | 294 (13.4) | 91 (4.2) | |
| Sitting time (hours/day) | 0.015 | ||||
| <4 | 186 (9.9) | 1393 (74.1) | 243 (12.9) | 58 (3.1) | |
| 4–5 | 221 (10.7) | 1526 (74.0) | 270 (13.1) | 45 (2.2) | |
| 6–8 | 266 (10.7) | 1821 (73.5) | 327 (13.2) | 64 (2.6) | |
| >8 | 407 (11.1) | 2618 (71.2) | 507 (13.8) | 144 (3.9) | |
| Diet (adapted HEI) | 0.015 | ||||
| >80 good | 110 (8.8) | 929 (74.0) | 172 (13.7) | 44 (3.5) | |
| ≤80 needs improvement/poor | 970 (12.7) | 6429 (72.9) | 1175 (10.9) | 267 (3.5) | |
| Skipping breakfast | <0.001 | ||||
| Yes | 98 (10.1) | 684 (70.1) | 142 (14.6) | 51 (5.2) | |
| No | 982 (10.8) | 6674 (73.2) | 1205 (13.2) | 260 (2.9) | |
| BMI ≥ 25 kg/m2 | ||||
|---|---|---|---|---|
| OR (95% CI) | p-Value | aOR (95% CI) | p-Value | |
| Age | 1.14 (1.11–1.18) | <0.001 | 1.14 (1.11–1.18) | <0.001 |
| Sex | ||||
| Female/Male | 0.60 (0.56–0.70) | <0.001 | 0.62 (0.55–0.69) | <0.001 |
| People the student lives with | ||||
| Roommates/Friends vs. Family | 1.10 (0.98–1.22) | 0.143 | 1.10 (0.98–1.23) | 0.098 |
| Alone vs. Family | 1.27 (1.69–1.99) | 0.014 | 1.27 (1.05–1.55) | 0.013 |
| Physical activity | ||||
| Does not meet WHO criteria vs. meets WHO criteria | 1.11 (0.97–1.26) | 0.101 | 1.15 (1.01–1.31) | 0.029 |
| Sitting time | ||||
| Highly sedentary vs. not | 1.05 (1.00–1.10) | 0.039 | 1.06 (1.01–1.11) | 0.015 |
| Diet (adapted HEI) | ||||
| Poor diet vs. healthy diet | 0.93 (0.80–1.10) | 0.420 | 0.87 (0.74–1.03) | 0.092 |
| Skipping breakfast | ||||
| Yes vs. No | 1.29 (1.09–1.52) | 0.003 | 1.28 (1.08–1.52) | 0.004 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernández-Segura, N.; Botella-Juan, L.; Amezcua-Prieto, C.; Morales-Suárez-Varela, M.; Mateos-Campos, R.; Fernández-Villa, T.; Ortiz-Moncada, R.; Almaraz, A.; Narciso-Rufo, A.; Ayán-Pérez, C.; et al. Excess Weight in Relation to Lifestyle Habits in Spanish First-Year University Students: Differences between Pre- and Post-COVID-19—A Serial Cross-Sectional Study Based on uniHcos Project. Healthcare 2023, 11, 1547. https://doi.org/10.3390/healthcare11111547
Hernández-Segura N, Botella-Juan L, Amezcua-Prieto C, Morales-Suárez-Varela M, Mateos-Campos R, Fernández-Villa T, Ortiz-Moncada R, Almaraz A, Narciso-Rufo A, Ayán-Pérez C, et al. Excess Weight in Relation to Lifestyle Habits in Spanish First-Year University Students: Differences between Pre- and Post-COVID-19—A Serial Cross-Sectional Study Based on uniHcos Project. Healthcare. 2023; 11(11):1547. https://doi.org/10.3390/healthcare11111547
Chicago/Turabian StyleHernández-Segura, Natalia, Lorena Botella-Juan, Carmen Amezcua-Prieto, María Morales-Suárez-Varela, Ramona Mateos-Campos, Tania Fernández-Villa, Rocío Ortiz-Moncada, Ana Almaraz, Alicia Narciso-Rufo, Carlos Ayán-Pérez, and et al. 2023. "Excess Weight in Relation to Lifestyle Habits in Spanish First-Year University Students: Differences between Pre- and Post-COVID-19—A Serial Cross-Sectional Study Based on uniHcos Project" Healthcare 11, no. 11: 1547. https://doi.org/10.3390/healthcare11111547
APA StyleHernández-Segura, N., Botella-Juan, L., Amezcua-Prieto, C., Morales-Suárez-Varela, M., Mateos-Campos, R., Fernández-Villa, T., Ortiz-Moncada, R., Almaraz, A., Narciso-Rufo, A., Ayán-Pérez, C., Molina, A. J., & UniHcos Project Working Group. (2023). Excess Weight in Relation to Lifestyle Habits in Spanish First-Year University Students: Differences between Pre- and Post-COVID-19—A Serial Cross-Sectional Study Based on uniHcos Project. Healthcare, 11(11), 1547. https://doi.org/10.3390/healthcare11111547












