Effects of School Nurse-Led Interventions in Collaboration with Kinesiologists in Promoting Physical Activity and Reducing Sedentary Behaviors in Children and Adolescents: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Search Strategy, and Selection Criteria
2.2. Data Extraction
2.3. Quality Assessment and Risk Bias
3. Results
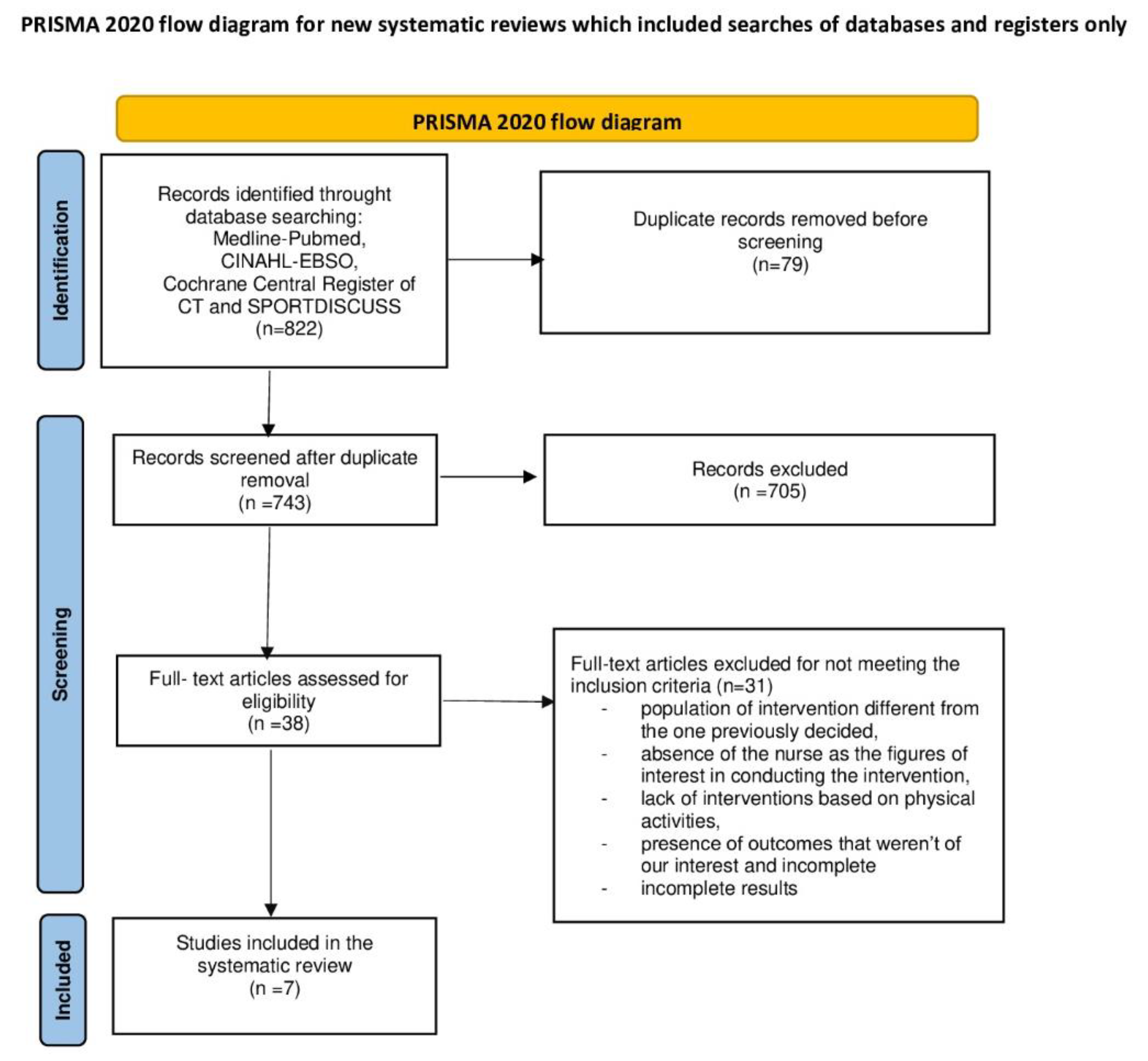
3.1. Search Results
3.2. Study Characteristics and Data Extraction
3.3. Quality Assessment and Risk of Bias Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roberts, C.; Currie, C.; Samdal, O.; Currie, D.; Smith, R.; Maes, L. Measuring the health and health behaviours of adolescents through cross-national survey research: Recent developments in the Health Behaviour in School-aged Children (HBSC) study. J. Public Health 2007, 15, 179–186. [Google Scholar] [CrossRef]
- Kimiecik, J.; Horn, T.; Newman, T.J.; Kimiecik, C.M. Moving adolescents for a lifetime of physical activity: Shifting to interventions aligned with the third health revolution. Health Psychol. Rev. 2020, 14, 486–503. [Google Scholar] [CrossRef] [PubMed]
- Esposito, F.; Sanmarchi, F.; Marini, S.; Masini, A.; Scrimaglia, S.; Adorno, E.; Soldà, G.; Arrichiello, F.; Ferretti, F.; Rangone, M.; et al. Weekday and Weekend Differences in Eating Habits, Physical Activity and Screen Time Behavior among a Sample of Primary School Children: The “Seven Days for My Health” Project. Int. J. Environ. Res. Public Health 2022, 19, 4215. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, K.M.; Barnes, C.; Yoong, S.; Campbell, E.; Wyse, R.; Delaney, T.; Brown, A.; Stacey, F.; Davies, L.; Lorien, S.; et al. School-Based Nutrition Interventions in Children Aged 6 to 18 Years: An Umbrella Review of Systematic Reviews. Nutrients 2021, 13, 4113. [Google Scholar] [CrossRef]
- Barnett, T.A.; Kelly, A.S.; Young, D.R.; Perry, C.K.; Pratt, C.A.; Edwards, N.M.; Rao, G.; Vos, M.B. Sedentary Behaviors in Today’s Youth: Approaches to the Prevention and Management of Childhood Obesity: A Scientific Statement From the American Heart Association. Circulation 2018, 138, e142–e159. [Google Scholar] [CrossRef]
- Masini, A.; Ceciliani, A.; Dallolio, L.; Gori, D.; Marini, S. Evaluation of feasibility, effectiveness, and sustainability of school-based physical activity “active break” interventions in pre-adolescent and adolescent students: A systematic review. Can. J. Public Health 2022, 113, 713–725. [Google Scholar] [CrossRef]
- Filho, V.C.B.; Pereira, W.M.G.; Farias, B.O.; Moreira, T.M.M.; Guerra, P.H.; Queiroz, A.C.M.; Castro, V.H.S.; Silva, K.S. Scoping Review on Interventions for Physical Activity and Physical Literacy Components in Brazilian School-Aged Children and Adolescents. Int. J. Environ. Res. Public Health 2021, 18, 8349. [Google Scholar] [CrossRef]
- Whitehead, D. The health-promoting school: What role for nursing? J. Clin. Nurs. 2006, 15, 264–271. [Google Scholar] [CrossRef]
- Pozzi, F.; Passarelli, M.; Manganello, F.; Alvino, S.; Dagnino, F.M.; Mazzarino, B.; Sasso, L.; Bagnasco, A.M.; Zanini, M.; Catania, G.; et al. Development of a European Curriculum for Family and Community Nurses. In Development, Implementation and Evaluation of Curricula in Nursing and Midwifery Education; Darmann-Finck, I., Reiber, K., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 169–191. [Google Scholar] [CrossRef]
- Camedda, C.; Scalorbi, S.; Longobucco, Y. The Family and Community Nurse Core Competencies: Integrating European standards into the Italian context. Acta Biomed. 2021, 92, e2021329. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. Open. Med. 2009, 3, e123–e130. [Google Scholar]
- Higgins, J.G.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; Wiley: Hoboken, NJ, USA, 2008. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Hernán, M.A.; McAleenan, A.; Reeves, B.C.; Higgins, J.P.T. Assessing risk of bias in a non-randomized study. In Cochrane Handbook for Systematic Reviews of Interventions; Wiley: Hoboken, NJ, USA, 2019. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Robbins, L.B.; Ling, J.; Sharma, D.B.; Dalimonte-Merckling, D.M.; Voskuil, V.R.; Resnicow, K.; Kaciroti, N.; Pfeiffer, K.A. Intervention Effects of “Girls on the Move” on Increasing Physical Activity: A Group Randomized Trial. Ann. Behav. Med. 2019, 53, 493–500. [Google Scholar] [CrossRef] [PubMed]
- Robbins, L.B.; Pfeiffer, K.A.; Maier, K.S.; Lo, Y.-J.; Wesolek, S.M. Pilot Intervention to Increase Physical Activity Among Sedentary Urban Middle School Girls: A Two-Group Pretest–Posttest Quasi-Experimental Design. J. Sch. Nurs. 2012, 28, 302–315. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pbert, L.; Druker, S.; Barton, B.; Schneider, K.L.; Olendzki, B.; Gapinski, M.A.; Kurtz, S.; Osganian, S. A School-Based Program for Overweight and Obese Adolescents: A Randomized Controlled Trial. J. Sch. Health 2016, 86, 699–708. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wright, K.; Norris, K.; Newman Giger, J.; Suro, Z. Improving healthy dietary behaviors, nutrition knowledge, and self-efficacy among underserved school children with parent and community involvement. Child. Obes. 2012, 8, 347–356. [Google Scholar] [CrossRef]
- Ham, O.K.; Sung, K.M.; Lee, B.G.; Choi, H.W.; Im, E.O. Transtheoretical Model Based Exercise Counseling Combined with Music Skipping Rope Exercise on Childhood Obesity. Asian Nurs. Res. (Korean Soc. Nurs. Sci.) 2016, 10, 116–122. [Google Scholar] [CrossRef][Green Version]
- Choo, J.; Yang, H.M.; Jae, S.Y.; Kim, H.J.; You, J.; Lee, J. Effects of the Healthy Children, Healthy Families, Healthy Communities Program for Obesity Prevention among Vulnerable Children: A Cluster-Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 2895. [Google Scholar] [CrossRef][Green Version]
- Altunkurek, S.Z.; Bebis, H. The effects of wellness coaching on the wellness and health behaviors of early adolescents. Public Health Nurs. 2019, 36, 488–497. [Google Scholar] [CrossRef]
- Pender, N.J.; Murdaugh, C.L.; Parsons, M.A. Health Promotion in Nursing Practice, 5th ed.; Prentice Hall: Upper Saddle River, NJ, USA, 2006. [Google Scholar]
- Ryan, R.M.; Deci, E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 2000, 55, 68–78. [Google Scholar] [CrossRef]
- Monzavi, R.; Dreimane, D.; Geffner, M.E.; Braun, S.; Conrad, B.; Klier, M.; Kaufman, F.R. Improvement in risk factors for metabolic syndrome and insulin resistance in overweight youth who are treated with lifestyle intervention. Pediatrics 2006, 117, e1111–e1118. [Google Scholar] [CrossRef]
- McKenzie, T.L.; Nader, P.R.; Strikmiller, P.K.; Yang, M.; Stone, E.J.; Perry, C.L.; Taylor, W.C.; Epping, J.N.; Feldman, H.A.; Luepker, R.V.; et al. School physical education: Effect of the Child and Adolescent Trial for Cardiovascular Health. Prev. Med. 1996, 25, 423–431. [Google Scholar] [CrossRef]
- Owen, F.K.; Öğretmen, T. Five Factor Wellness Inventory—Teen Version: Turkish Adolescents. In Inonu University Journal of the Faculty of Education; Inonu University: Malatya, Turkey, 2013. [Google Scholar]
- Grunbaum, J.A.; Kann, L.; Kinchen, S.A.; Williams, B.; Ross, J.G.; Lowry, R.; Kolbe, L. Youth risk behavior surveillance—United States, 2001. MMWR Surveill. Summ. 2002, 51, 1–62. [Google Scholar] [CrossRef]
- Lytle, L.A.; Nichaman, M.Z.; Obarzanek, E.; Glovsky, E.; Montgomery, D.; Nicklas, T.; Zive, M.; Feldman, H. Validation of 24-hour recalls assisted by food records in third-grade children. The CATCH Collaborative Group. J. Am. Diet. Assoc. 1993, 93, 1431–1436. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, R.E.; Ory, M.G.; Klesges, L.M.; Cifuentes, M.; Fernald, D.H.; Green, L.A. Practical and relevant self-report measures of patient health behaviors for primary care research. Ann. Fam. Med. 2005, 3, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Artinian, N.T.; Fletcher, G.F.; Mozaffarian, D.; Kris-Etherton, P.; Van Horn, L.; Lichtenstein, A.H.; Kumanyika, S.; Kraus, W.E.; Fleg, J.L.; Redeker, N.S.; et al. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: A scientific statement from the American Heart Association. Circulation 2010, 122, 406–441. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Battjes-Fries, M.C.E.; Haveman-Nies, A.; Zeinstra, G.G.; van Dongen, E.J.I.; Meester, H.J.; van den Top-Pullen, R.; Van’t Veer, P.; de Graaf, K. Effectiveness of Taste Lessons with and without additional experiential learning activities on children’s willingness to taste vegetables. Appetite 2017, 109, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Prochaska, J.O.; Redding, C.A.; Evers, K.E. The transtheoretical model and stages of change. In Health Behavior and Health Education: Theory, Research, and Practice, 4th ed.; Jossey-Bass: San Francisco, CA, USA, 2008; pp. 97–121. [Google Scholar]
- Marcus, B.H.; Owen, N. Motivational readiness, self-efficacy and decision-making for exercise. J. Appl. Social. Psychol. 1992, 22, 3–16. [Google Scholar] [CrossRef][Green Version]
- Hauner, H. Overweight--not such a big problem? Dtsch. Arztebl. Int. 2009, 106, 639–640. [Google Scholar] [CrossRef]
- Pierannunzio, D.; Spinelli, A.; Berchialla, P.; Borraccino, A.; Charrier, L.; Dalmasso, P.; Lazzeri, G.; Vieno, A.; Ciardullo, S.; Nardone, P. Physical Activity among Italian Adolescents: Association with Life Satisfaction, Self-Rated Health and Peer Relationships. Int. J. Environ. Res. Public Health 2022, 19, 4799. [Google Scholar] [CrossRef]
- Gott, M.; O’Brien, M. The role of the nurse in health promotion. Health Promot. Int. 1990, 5, 137–143. [Google Scholar] [CrossRef]
- Melariri, H.; Osoba, T.A.; Williams, M.M.; Melariri, P. An assessment of nurses’ participation in Health Promotion: A knowledge, perception, and practice perspective. J. Prev. Med. Hyg. 2022, 63, E27–E34. [Google Scholar] [CrossRef] [PubMed]
- Bright, T.; Burdett, T. Smoking cessation and the health promotion role of community nurses. J. Community Nurs. 2019, 33, 56–60. [Google Scholar]
- Wang, L.Y.; Vernon-Smiley, M.; Gapinski, M.A.; Desisto, M.; Maughan, E.; Sheetz, A. Cost-benefit study of school nursing services. JAMA Pediatr. 2014, 168, 642–648. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Blair, S.N.; Franklin, B.A.; Jakicic, J.M.; Kibler, W.B. New vision for health promotion within sports medicine. Am. J. Health Promot. 2003, 18, 182–185. [Google Scholar] [CrossRef] [PubMed]
- George, T.R.; Marquez, A.A.; Coble, C.J.; Williams, A.S. Reimagining Sport Management Programs Within Kinesiology and Public Health. Kinesiol. Rev. 2022, 11, 323–331. [Google Scholar] [CrossRef]
| Parameter | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | Children and adolescence | Preschool children 3–6 years old |
| Any gender and ethnicity | Adults | |
| 6–18 years old | Workers | |
| Intervention | Nurse-led interventions also in collaboration with kinesiologists that promote physical activity intervention, reduce sedentary behaviors, and improve healthy lifestyle behaviors. Interventions involving school setting | Studies focused on multicomponent intervention based only on healthy nutrition and sleep hygiene |
| Comparator | Studies with or without control group in which participants did not receive any intervention or received interventions that are not based on school nursing | |
| Outcome | Physical activity levels, sedentary behavior, lifestyle behaviors | Absence of physical activity levels |
| Study design | Experimental or observational studies with original primary data and full-text studies written in English | Study protocols or other papers without original data |
| Author; Year; Country; Study Design | Study Population | Intervention | Outcomes | Results |
|---|---|---|---|---|
| Robbins L. B. et al. [15]. 2019; USA; RCT | n = 1519 (EG:753; CG:766) Males: n = 0 (0.00%) Age: EG:12.05 ± 0.99; CG:12.05 ± 1.02 Enrollment period: 2011–2016 Setting: Public Schools (5th–8th grades) | EG: The intervention was based on the Health Promotion Model and Self-Determination Theory and included three components: (i) an afterschool PA club at each school conducted by a club manager and three to four instructors; (ii) two face-to-face motivational, individually tailored counseling sessions (one at the beginning and other at the end of intervention) with a health professional having experience with adolescents (e.g., registered/school nurse); and (iii) an interactive Internet-basedsession via an iPad set up by the researchers at each school. CG: No intervention. Time: (i) 90 min of exercise; (ii) 15–20 min for each counseling session. Duration: 3 days/week (17 weeks). | Primary Outcomes: Physical Activity Levels (MVPA); BMI (kg/m2) Methods/Questionnaire/Test: ActiGraph GT3X+ accelerometers; BMI (kg/m2) Other Outcomes: Pubertal Stage (Pubertal Development Scale) | T0 vs. T1 differences between EG and CG. Physical Activity Levels: T0 EG: 3.03 min/h, T1 EG: 3.27 min/h; T0 CG: 2.92 min/h, T1 CG: 3.27 min/h; (p = n.s.). BMI: No information. |
| Wright K. et al. [18] 2012; USA; RCT | n = 251 (EG:121; CG:130) Males: n = 101 (40.24%) Age: EG:9.0 ± 1.6; CG:8.3 ± 1.1 Enrollment period: January 2008–September 2010 Setting: Primary Schools | EG: The intervention is conducted by registered nurses, trained community health workers and a physical education specialist. Sessions consisted of three components: physical activity, nutrition education/behavior modification, and family involvement. CG: The group participated in the standard physical activity program given by their respective schools and did not receive any physical or nutrition education. Time: 90 min. Duration: 6 weeks. | Primary Outcomes: Physical Activity Levels; Sedentary Behavior; BMI (kg/m2) Methods/Questionnaire/Test: CATCH SPAN Questionnaire (daily physical activity, attends PE class, TV viewing); BMI (kg/m2) Other Outcomes: Blood Pressure | T0 vs. T1 differences between EG and CG. Physical Activity Levels: T0 vs. T1 Increased participation in MVPA for male and female The effect was for both males (p = 0.002) and females (p = 0.005) at 12 months. T0 vs. T1 Increased participation in PE The effect was sustained for both males (p = 0.003) and females (p = 0.002). Sedentary Behavior: T0 vs. T1 Decreased TV viewing The effect was sustained at 12 months for males only (p = 0.030). BMI: In female students in the KNF group, BMI (p = 0.047) and BMI z-score (p = 0.05) decreased The effects were sustained for 12 months. While BMI and BMI z-scores decreased in males, this was not significant |
| Ham O. K. et al. [19] 2016; South Korea; Quasi-experimental study | n = 75 (EG: 48; CG: 27) Males: n = 43 (57.33%) Age: EG:10.77 ± 1.17; CG:10.26 ± 0.86 Enrollment period: April 2011–December 2011 Setting: Primary Schools | EG: eight-session individual counseling, 12 week music skipping rope exercise and booster counseling 3 months after the intervention. CG: one-session individual counseling, 12 week music skipping rope exercise. Time: (i) 30 min each TTM counseling (eight counseling sessions: four consecutive weeks for the first month and every other week for the last 2 months); (ii) 60 min of skipping rope exercise each week. Duration: 3 months. | Primary Outcomes: Stages of Change in Exercise Behavior; BMI (kg/m2) Methods/Questionnaire/Test: One question developed by Marcus and Owen aimed at the classification of the participant to one out of five categories; Electronic scales for measuring height and weight; Fourteen items of decisional balance developed by Marcus and Owen; BMI (kg/m2) Other Outcomes: Exercise; Self-Efficacy; Glucose Tolerance and Lipid Profile | T0 vs. T1 differences between EG and CG. Stages of Change in Exercise Behavior: 36.2% of EG and 17.4% CG advanced their exercise behavior by at least one stage; (p = n.s.). BMI: T0 EG 24.35 ± 2.73, T1 EG 24.37 ± 2.73; (p = 0.010) T0 CG 24.22 ± 2.24, T1 CG 24.99 ± 2.55; (p = n.s.). |
| Robbins L. B. et al. [16] 2012; USA; Quasi-experimental study | n = 69 (EG: 37; CG: 32) Males: n = 0 (0.00%) Age: EG:11.49 ± 0.67; CG:11.44 ± 0.84 Enrollment period: Spring 2009 Setting: Middle Schools | EG: (i) A 90 min after-school physical activity club offered at the middle school 5 days a week for 6 months (total of 98 sessions) and (ii) a face-to-face motivational, individually tailored counseling session with a registered (school) nurse during the school day every other month over the 6 months (total of three 20 min sessions were planned). The counseling sessions the girls had with the nurse occurred during the school day to capitalize on required school attendance. CG: (i) A 90 min after-school workshop once a month for 6 months (total of six workshops) and (ii) a face-to-face session with a registered (school) nurse during the school day every other month over the 6 months (total of three 20 min sessions were planned). Each workshop focused on one of the following health-promoting topics: (1) caring for my body; (2) fashion, hair, and nail tips; (3) sun and food safety; (4) healthy relationships and friendship; (5) building self-esteem; and (6) career exploration. The same workshop was offered on two consecutive days each month to enhance the opportunity for participation. Each session with the nurse included a discussion of two of the six topics. Time: (i) 90 min after-school physical activity club 5 days a week for 6 months (total of 98 sessions); (ii) face-to-face counseling sessions during the school day every other month over the 6 months (total of three 20 min sessions). Duration: 24 weeks. | Primary Outcomes: Physical Activity Levels (Minutes of MVPA/Hour); Cardiovascular Fitness (Progressive Aerobic Cardiovascular Endurance Run-PACER); BMI (kg/m2); Percentage Body Fat; Waist Circumference Methods/Questionnaire/Test: ActiGraph GT1M accelerometers; BMI (kg/m2) Other Outcomes: Perceived Benefits of and Barriers to Physical Activity; Perceived Physical Activity Self-Efficacy; Interpersonal Influences; Enjoyment of Physical Activity | T0 vs. T1 differences between EG and CG. Physical Activity Levels: T0 EG 0.69 ± 0.28, T1 EG 1.05 ± 0.41; T0 CG 1.08 ± 0.69, T1 CG 1.20 ± 0.65; (p = n.s.). Cardiovascular Fitness: T0 EG 10.50 ± 4.72, T1 EG 11.29 ± 7.28; T0 CG 14.10 ± 7.44, T1 CG 12.73 ± 7.54; (p = n.s.). BMI: T0 EG 25.94 ± 7.39, T1 EG 26.59 ± 7.40; T0 CG 24.88 ± 7.98, T1 CG 25.50 ± 7.90; (p = n.s.). Percentage Body Fat: T0 EG 34.02 ± 11.28, T1 EG 34.02 ± 10.83; T0 CG 31.98 ± 11.60, T1 CG 32.74 ± 11.25; (p = n.s.). Waist Circumference: T0 EG 80.78 ± 18.45, T1 EG 80.45 ± 17.17; T0 CG 79.57 ± 17.80, T1 CG 79.10 ± 15.58; (p = n.s.). |
| Altunkurek S. Z. et al. [21] 2019; Turkey; RCT | n = 132 (Wellness Coaching Program Group-WCPG: 33; Health Education Group-HEG: 33; Control Group-CG: 66) Males: n = 64 (48.5%) Age: 12–15 years old Enrollment period: September 2016–December 2016 Setting: 8th Grade Schools | WCPG (Wellness Coaching Program Group): Three main parts: physical activity, individual interviews, and group education. HEG (Health Education Group): A warm-up game was played in the first 5 min, and the last 10 min were devoted to questions and discussion. The content of the sessions was similar to the wellness coaching education. CG: No intervention. Time: (i) 90 min session 1 day a week of WCPG; (ii) 45–60 min once a week of HEG. Duration: 12 weeks. | Primary Outcomes: Five-Factor Wellness Scale-Adolescent Form (5F-Wellness-AF) Total Average; Adolescent Lifestyle Scale (ALPS) Total Average; BMI Methods/Questionnaire/Test: Five-Factor Wellness Scale-Adolescent Form (5F-Wellness-AF); Adolescent Lifestyle Scale (ALPS); Wellness Coach Individual Interview; Demographic Information Form; BMI Other Outcomes: --- | T0 vs. T1 differences between EG and CG. 5F-Wellness-AF Total Average: T0: WCPG < CG = 114.45 ± 16.55 < 128.33 ± 17.16; (p < 0.001). WCPG < HEG = 114.45 ± 16.55 < 125.73 ± 12.73; (p = 0.003). CG > HEG = 128.33 ± 17.16 > 125.73 ± 12.73; (p = n.s.). T1: WCPG < CG = 151.33 ± 6.02 > 126.82 ± 16.48; (p < 0.001). WCPG < HEG = 151.33 ± 6.02 > 129.03 ± 13.87; (p < 0.001): CG > HEG = 126.82 ± 16.48 < 129.03 ± 13.87; (p = n.s.). ALPS total average: T0: WCPG < CG = 112.88 ± 16.79 < 123.39 ± 18.70; (p = 0.021) WCPG < HEG = 112.88 ± 16.79 < 122.76 ± 17.49; (p = n.s.). CG > HEG = 123.39 ± 18.70 > 122.76 ± 17.49; (p = n.s.). T1: WCPG < CG = 158.82 ± 8.20 > 125.50 ± 18.62; (p < 0.001). WCPG < HEG = 158.82 ± 8.20 > 127.94 ± 20.03; (p < 0.001). CG > HEG = 125.50 ± 18.62 < 127.94 ± 20.03; (p = n.s.). BMI: T0 vs. T1 no differences in number of overweight (p = n.s.) |
| Pbert L. et al. [17] 2016; USA; RCT | n = 126 (EG: 58; CG: 68) Males: n = 42 (37.83%) Age: EG:16.5 ± 1.23; CG:16.3 ± 1.20 Enrollment period: September 2012–June 2013 Setting: High Schools | EG: Lookin’ Good Feelin’ Good. (i) School nurse-delivered counseling intervention; (ii) After-school exercise program. CG: No intervention. Time: (i) Phase of six weekly 30 min individual sessions followed by a maintenance phase of six monthly sessions and brief weekly weigh-ins; (ii) three sessions per week structured to increase exercise enjoyment. Duration: 8 months. | Primary Outcomes: Physical Activity Levels (number of days physically active in past 7 days); Sedentary Behavior (hours play video/computer games or watching TV on average school day in past 7 days); BMI; Dietary Intake Methods/Questionnaire/Test: ActiGraph Model GT1M (for a 7 day period); two items from the Youth Risk Behavior Survey; BMI (kg/m2); 24 h dietary recall interview Other Outcomes: --- | T0 vs. T1 differences between EG and CG. Physical Activity Levels (number days physically active in past 7 days): 0.89 (0.25–1.53); (p = 0.007). Physical Activity Levels (%Time spent in MVPA each day): −0.76 (−4.63–3.10); (p = n.s). Sedentary Behavior: −0.01 (−0.43–0.41); (p = n.s.). BMI: −0.14 (−1.09–0.81); (p = n.s.). Dietary Intake: Students in EG compared with CG schools reported eating breakfast on significantly more days/week. The other data on dietary intake are not statistically significant. |
| Choo J. et al. [20] 2020; South Korea; RCT | n = 104 (EG:49; CG:55) Males: n = 57 (54.8%) Age: EG:9.9 ± 1.18; CG:10.1 ± 1.27 Enrollment period: Recruitment in June 2017 Setting: Community Child Centers | EG: Multi-level interventions of child, parent, and center-level strategies. (i) Child-level: six weekly sessions for healthy eating and six weekly sessions for healthy activity; (ii) Parent-level: one session of group teaching, two home visits, three telephone counseling sessions, 12 weekly text messages; center-level: 12 sessions educational curriculum for heathy eating and activity and secured the physical environment for operating educational classes; the researcher educated the faculty members (directors, teachers, cooks) to be aware about obesity, to display posters regarding lifestyle, to adopt policies such as no sugar-sweetened. CG: No intervention. Time: No information. Duration: 12 weeks. | Primary Outcomes: Knowledge of Healthy Lifestyle Behaviors; Healthy Lifestyle Behavior; Obesity Status; BMI z score Methods/Questionnaire/Test: 18 item questionnaire developed by the PI (score 0–18); Healthy Lifestyle Behaviors = Self-Reported (score 0–9); BMI z score Other Outcomes: Parenting Behaviors | T0 vs. T1 differences between EG and CG. Knowledge of Healthy Lifestyle Behaviors: T0 EG 13.0 ± 1.74, T1 EG 14.8 ± 1.45; T0 CG 13.7 ± 2.04, T1 CG 14.2 ± 1.88; (p = 0.026). Healthy Lifestyle Behaviors: T0 EG 2.4 ± 1.56, T1 EG 3.4 ± 2.12; CG T0 3.3 ± 1.68, T1 CG 2.9 ± 1.62; (p < 0.01). Obesity Status: T0 EG 32.7%, T1 EG 36.7%; T0 CG 38.2%, T1 CG 41.8%; (p = n.s.). BMI z-score: T0 EG 0.8 ± 1.36, T1 EG 0.9 ± 1.36; T0 CG 1.3 ± 1.24, T1 CG 1.3 ± 1.22; (p = 0.05). |
| Authors | Study Design | Tool for Assessment | Quality |
|---|---|---|---|
| Choo et al., 2020 [20] | RCT | Cochrane ROB2 Tool | Some concern |
| Pbert et al., 2016 [17] | RCT | Cochrane ROB Tool | Some concern |
| Robbins et al., 2019 [15] | RCT | Cochrane ROB Tool | High |
| Altunkurek et al., 2018 [21] | RCT | Cochrane ROB2 Tool | Some concern |
| Wright et al., 2013 [18] | RCT | Cochrane ROB2 Tool | Some concern |
| Ham et al., 2016 [19] | Quasi-experimental | ROBBINS-I | Moderate |
| Robbins et al., 2012 [16] | Quasi-experimental | ROBBINS-I | Low |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Longobucco, Y.; Ricci, M.; Scrimaglia, S.; Camedda, C.; Dallolio, L.; Masini, A. Effects of School Nurse-Led Interventions in Collaboration with Kinesiologists in Promoting Physical Activity and Reducing Sedentary Behaviors in Children and Adolescents: A Systematic Review. Healthcare 2023, 11, 1567. https://doi.org/10.3390/healthcare11111567
Longobucco Y, Ricci M, Scrimaglia S, Camedda C, Dallolio L, Masini A. Effects of School Nurse-Led Interventions in Collaboration with Kinesiologists in Promoting Physical Activity and Reducing Sedentary Behaviors in Children and Adolescents: A Systematic Review. Healthcare. 2023; 11(11):1567. https://doi.org/10.3390/healthcare11111567
Chicago/Turabian StyleLongobucco, Yari, Matteo Ricci, Susan Scrimaglia, Claudia Camedda, Laura Dallolio, and Alice Masini. 2023. "Effects of School Nurse-Led Interventions in Collaboration with Kinesiologists in Promoting Physical Activity and Reducing Sedentary Behaviors in Children and Adolescents: A Systematic Review" Healthcare 11, no. 11: 1567. https://doi.org/10.3390/healthcare11111567
APA StyleLongobucco, Y., Ricci, M., Scrimaglia, S., Camedda, C., Dallolio, L., & Masini, A. (2023). Effects of School Nurse-Led Interventions in Collaboration with Kinesiologists in Promoting Physical Activity and Reducing Sedentary Behaviors in Children and Adolescents: A Systematic Review. Healthcare, 11(11), 1567. https://doi.org/10.3390/healthcare11111567







