Alerts in Clinical Decision Support Systems (CDSS): A Bibliometric Review and Content Analysis
Abstract
:1. Introduction
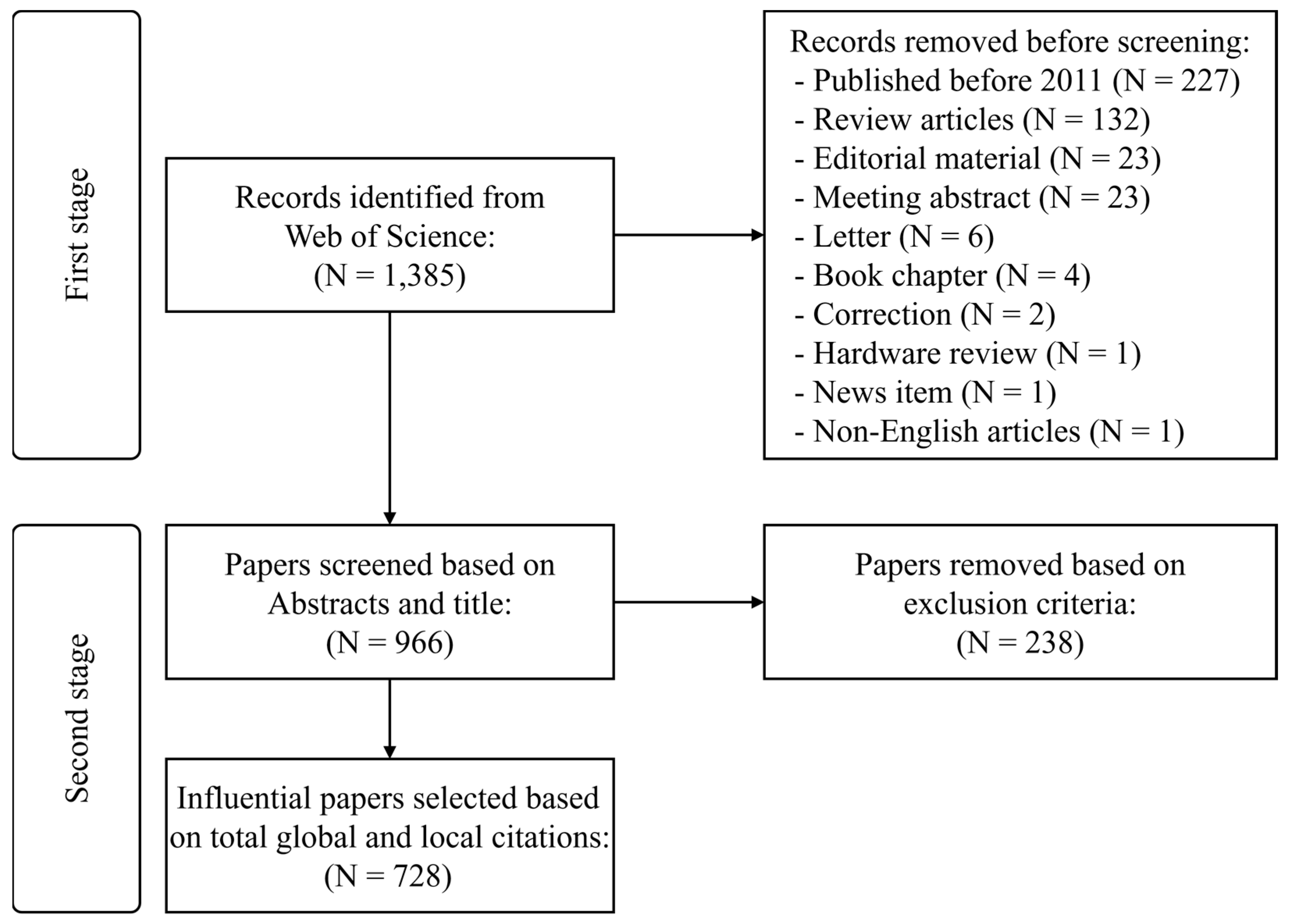
2. Materials and Methods
2.1. Bibliometric Analysis
2.1.1. Performance Analysis Using Citation Numbers
2.1.2. Citation Analysis
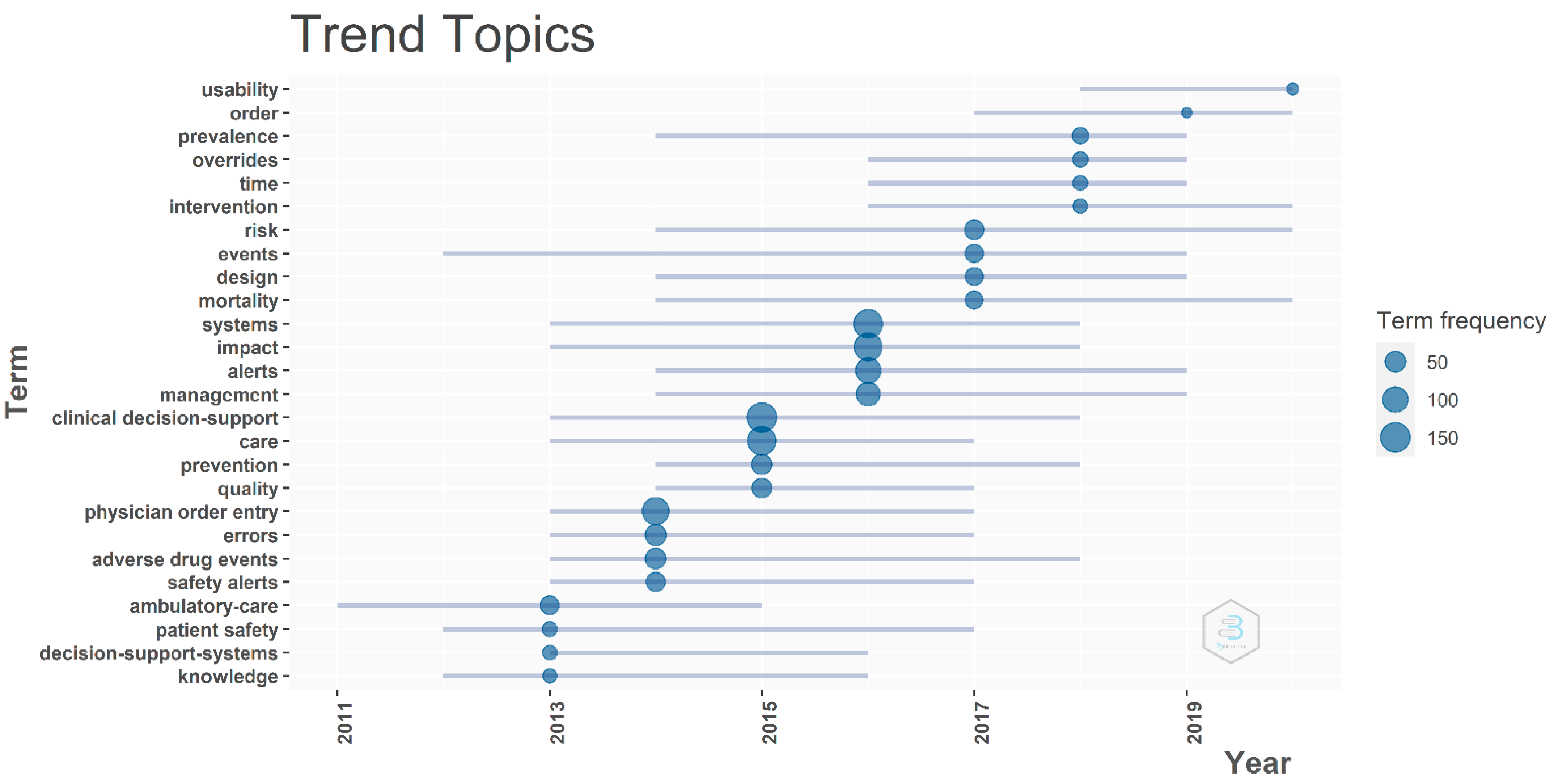
2.1.3. Trending Research Concepts Using Keywords
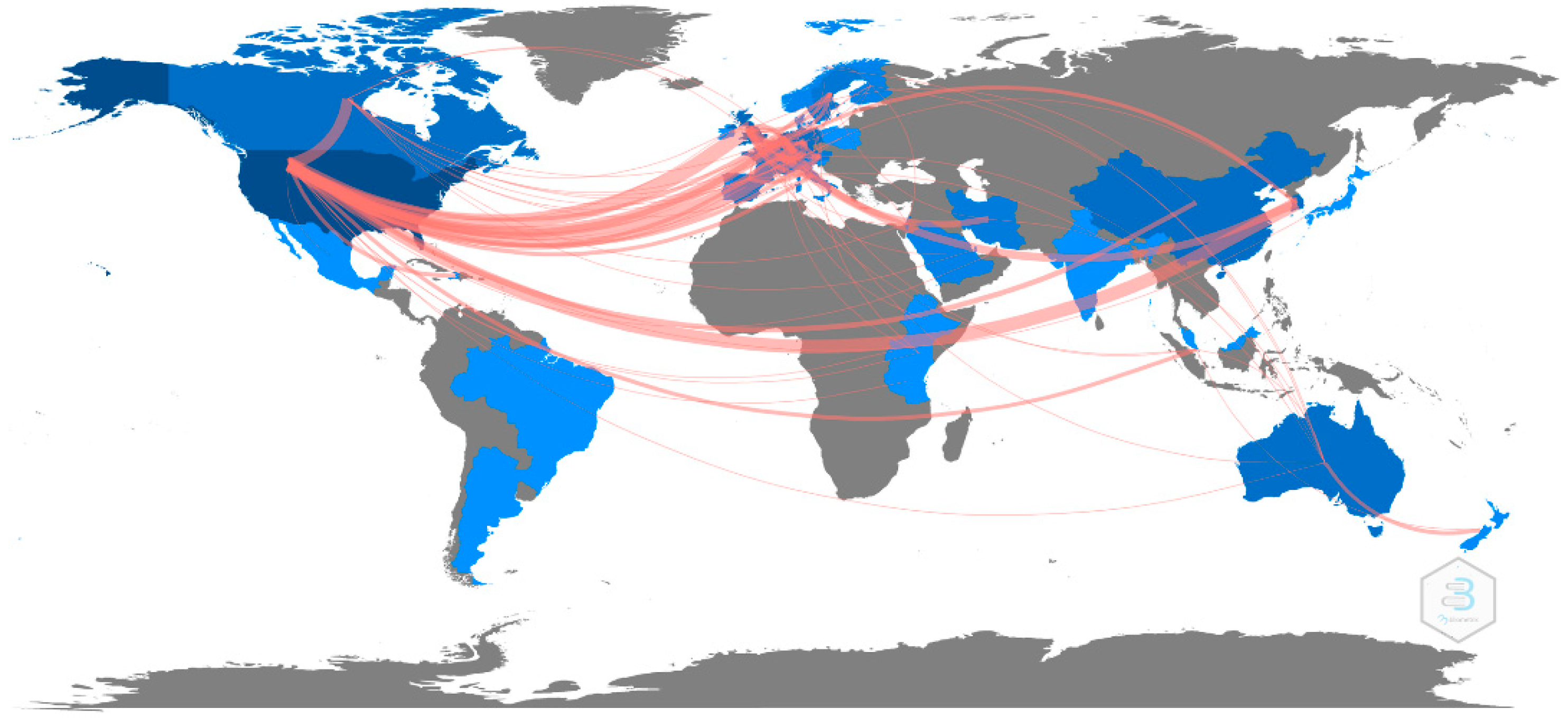
2.1.4. Country Collaboration Map
2.2. Content Analysis
2.3. Data Extraction Process
3. Results
3.1. Initial Paper Selection Result
3.2. Most Relevant Journals, Authors, Institutions, and Articles
3.3. Bibliographic Coupling
3.4. Trending Research Concepts Using Keywords
3.5. Country Collaboration Map
3.6. Content Analysis
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Laski, H.J.J.S. The limitations of the expert. Society 2020, 57, 371–377. [Google Scholar] [CrossRef] [PubMed]
- GY, D.D.; Sowmya, S.; Darshini, P.; Nanda, P. ACCIDENT ALERT SYSTEM. Int. J. Adv. Res. Eng. Technol. 2020, 11, 560–567. [Google Scholar]
- Jerry, D.J.; Thomas, L.; Panicker, S.T.; Shalu, R.; Mathew, J.T.; VS, B.V.J. Safety alert systems using dedicated short range communication for on road vehicles. In Proceedings of the 2018 International CET Conference on Control, Communication, and Computing (IC4), Thiruvananthapuram, India, 5–7 July 2018. [Google Scholar]
- Singh, N.R.; Rothe, P.; Rathkanthiwar, A. Implementation of safety alert system for elderly people using multi-sensors. In Proceedings of the 2017 International Conference of Electronics, Communication and Aerospace Technology (ICECA), Coimbatore, India, 20–22 April 2017. [Google Scholar]
- Kawamoto, K.; Lobach, D.F. Clinical decision support provided within physician order entry systems: A systematic review of features effective for changing clinician behavior. AMIA Annu. Symp. Proc. 2003, 2003, 361–365. [Google Scholar]
- Chazard, E.; Boudry, A.; Beeler, P.E.; Dalleur, O.; Hubert, H.; Tréhou, E.; Beuscart, J.-B.; Bates, D.W. Towards The Automated, Empirical Filtering of Drug-Drug Interaction Alerts in Clinical Decision Support Systems: Historical Cohort Study of Vitamin K Antagonists. JMIR Med. Inform. 2021, 9, e20862. [Google Scholar] [CrossRef] [PubMed]
- Kinlay, M.; Ho, L.M.R.; Zheng, W.Y.; Burke, R.; Juraskova, I.; Moles, R.; Baysari, M.J.A.C.I. Electronic Medication Management Systems: Analysis of Enhancements to Reduce Errors and Improve Workflow. Appl. Clin. Inform. 2021, 12, 1049–1060. [Google Scholar] [CrossRef] [PubMed]
- Sessions, L.C.; Nemeth, L.S.; Catchpole, K.; Kelechi, T.J. Nurses’ perceptions of high-alert medication administration safety: A qualitative descriptive study. J. Adv. Nurs. 2019, 75, 3654–3667. [Google Scholar] [CrossRef]
- Islam, M. An efficient human computer interaction through hand gesture using deep convolutional neural network. SN Comput. Sci. 2020, 1, 211. [Google Scholar] [CrossRef]
- Islam, M.M.; Iqbal, H.; Haque, M.R.; Hasan, M.K. Prediction of breast cancer using support vector machine and K-Nearest neighbors. In Proceedings of the 2017 IEEE Region 10 Humanitarian Technology Conference (R10-HTC), Dhaka, Bangladesh, 21–23 December 2017. [Google Scholar]
- Ayon, S.I.; Islam, M.M. Diabetes prediction: A deep learning approach. Int. J. Inf. Eng. Electron. Bus. 2019, 10, 21. [Google Scholar]
- Akter, L.; Islam, M.; Al-Rakhami, M.S.; Haque, M.J.S.C.S. Prediction of cervical cancer from behavior risk using machine learning techniques. SN Comput. Sci. 2021, 2, 177. [Google Scholar] [CrossRef]
- Akter, L.; Islam, M.M. Hepatocellular carcinoma patient’s survival prediction using oversampling and machine learning techniques. In Proceedings of the 2021 2nd International Conference on Robotics, Electrical and Signal Processing Techniques (ICREST), Dhaka, Bangladesh, 5–7 January 2021. [Google Scholar]
- Nasr, M.; Islam, M.M.; Shehata, S.; Karray, F.; Quintana, Y. Smart Healthcare in the Age of AI: Recent Advances, Challenges, and Future Prospects. IEEE Access 2021, 9, 145248–145270. [Google Scholar] [CrossRef]
- Islam, M.M.; Karray, F.; Alhajj, R.; Zeng, J. A Review on Deep Learning Techniques for the Diagnosis of Novel Coronavirus (COVID-19). IEEE Access 2021, 9, 30551–30572. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.M.; Tayan, O.; Islam, M.R.; Islam, M.S.; Nooruddin, S.; Kabir, M.N.; Islam, M.R.J.I.A. Deep learning based systems developed for fall detection: A review. IEEE Access 2020, 8, 166117–166137. [Google Scholar] [CrossRef]
- Islam, M.Z.; Islam, M.M.; Asraf, A. A combined deep CNN-LSTM network for the detection of novel coronavirus (COVID-19) using X-ray images. Inform. Med. Unlocked 2020, 20, 100412. [Google Scholar] [CrossRef] [PubMed]
- Muhammad, L.; Islam, M.; Usman, S.S.; Ayon, S.I.J.S.C.S. Predictive data mining models for novel coronavirus (COVID-19) infected patients’ recovery. SN Comput. Sci. 2020, 1, 206. [Google Scholar] [CrossRef]
- Rahman, M.M.; Manik, M.M.H.; Islam, M.M.; Mahmud, S.; Kim, J.-H. An automated system to limit COVID-19 using facial mask detection in smart city network. In Proceedings of the 2020 IEEE International IOT, Electronics and Mechatronics Conference (IEMTRONICS), Vancouver, BC, Canada, 9–12 September 2020. [Google Scholar]
- Ayon, S.I.; Islam, M.M.; Hossain, M.R. Coronary artery heart disease prediction: A comparative study of computational intelligence techniques. IETE J. Res. 2020, 1–20. [Google Scholar] [CrossRef]
- Haque, M.R.; Islam, M.M.; Iqbal, H.; Reza, M.S.; Hasan, M.K. Performance evaluation of random forests and artificial neural networks for the classification of liver disorder. In Proceedings of the 2018 International Conference on Computer, Communication, Chemical, Material and Electronic Engineering (IC4ME2), Rajshahi, Bangladesh, 8–9 February 2018. [Google Scholar]
- Islam, M.; Haque, M.; Iqbal, H.; Hasan, M.; Hasan, M.; Kabir, M.N. Breast cancer prediction: A comparative study using machine learning techniques. SN Comput. Sci. 2020, 1, 290. [Google Scholar] [CrossRef]
- Islam, M.R.; Moni, M.A.; Islam, M.M.; Rashed-Al-Mahfuz, M.; Islam, M.S.; Hasan, M.K.; Hossain, M.S.; Ahmad, M.; Uddin, S.; Azad, A. Emotion recognition from EEG signal focusing on deep learning and shallow learning techniques. IEEE Access 2021, 9, 94601–94624. [Google Scholar] [CrossRef]
- Islam, M.R.; Islam, M.M.; Rahman, M.M.; Mondal, C.; Singha, S.K.; Ahmad, M.; Awal, A.; Islam, M.S.; Moni, M.A. EEG channel correlation based model for emotion recognition. Comput. Biol. Med. 2021, 136, 104757. [Google Scholar] [CrossRef]
- Powers, E.M.; Shiffman, R.N.; Melnick, E.R.; Hickner, A.; Sharifi, M. Efficacy and unintended consequences of hard-stop alerts in electronic health record systems: A systematic review. J. Am. Med. Inform. Assoc. 2018, 25, 1556–1566. [Google Scholar] [CrossRef] [Green Version]
- Chien, S.-C.; Chin, Y.-P.; Yoon, C.H.; Islam, M.M.; Jian, W.-S.; Hsu, C.-K.; Chen, C.-Y.; Chien, P.-H.; Li, Y.-C. A novel method to retrieve alerts from a homegrown Computerized Physician Order Entry (CPOE) system of an academic medical center: Comprehensive alert characteristic analysis. PLoS ONE 2021, 16, e0246597. [Google Scholar] [CrossRef]
- Donthu, N.; Kumar, S.; Mukherjee, D.; Pandey, N.; Lim, W.M. How to conduct a bibliometric analysis: An overview and guidelines. J. Bus. Res. 2021, 133, 285–296. [Google Scholar] [CrossRef]
- Olakotan, O.O.; Mohd Yusof, M. The appropriateness of clinical decision support systems alerts in supporting clinical workflows: A systematic review. Health Inform. J. 2021, 27, 14604582211007536. [Google Scholar] [CrossRef] [PubMed]
- Aktürk, C. Bibliometric Analysis of Clinical Decision Support Systems. Acta Inform. Pragensia 2021, 10, 61–74. [Google Scholar] [CrossRef]
- Green, B.F.; Hall, J.A. Quantitative methods for literature reviews. Annu. Rev. Psychol. 1984, 35, 37–54. [Google Scholar] [CrossRef]
- Stremersch, S.; Verniers, I.; Verhoef, P. The Quest for Citations: Drivers of Article Impact. J. Mark. 2006, 71, 171–193. [Google Scholar] [CrossRef] [Green Version]
- Boyack, K.; Klavans, R. Co-Citation Analysis, Bibliographic Coupling, and Direct Citation: Which Citation Approach Represents the Research Front Most Accurately? J. Am. Soc. Inf. Sci. Technol. 2010, 61, 2389–2404. [Google Scholar] [CrossRef]
- Martyn, J. Bibliographic coupling. J. Doc. 1964, 20, 236. [Google Scholar] [CrossRef]
- Kessler, M.M.J.A.d. Bibliographic coupling between scientific papers. Am. Doc. 1963, 14, 10–25. [Google Scholar] [CrossRef]
- Bornmann, L.; Haunschild, R.; Hug, S.E. Visualizing the context of citations referencing papers published by Eugene Garfield: A new type of keyword co-occurrence analysis. Scientometrics 2018, 114, 427–437. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Yu, Q.; Zheng, F.; Long, C.; Lu, Z.; Duan, Z. Comparing keywords plus of WOS and author keywords: A case study of patient adherence research. J. Assoc. Inf. Sci. Technol. 2016, 67, 967–972. [Google Scholar] [CrossRef]
- Hsieh, H.-F.; Shannon, S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef] [PubMed]
- Gaur, A.; Kumar, M. A systematic approach to conducting review studies: An assessment of content analysis in 25 years of IB research. J. World Bus. 2018, 53, 280–289. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Mongeon, P.; Paul-Hus, A. The journal coverage of Web of Science and Scopus: A comparative analysis. Scientometrics 2016, 106, 213–228. [Google Scholar] [CrossRef]
- Alon, I.; Anderson, J.; Munim, Z.H.; Ho, A. A review of the internationalization of Chinese enterprises. Asia Pac. J. Manag. 2018, 35, 573–605. [Google Scholar] [CrossRef]
- Aria, M.; Cuccurullo, C. bibliometrix: An R-tool for comprehensive science mapping analysis. J. Informetr. 2017, 11, 959–975. [Google Scholar] [CrossRef]
- Hunter, J.D. Matplotlib: A 2D Graphics Environment. Comput. Sci. Eng. 2007, 9, 90–95. [Google Scholar] [CrossRef]
- Nanji, K.C.; Slight, S.P.; Seger, D.L.; Cho, I.; Fiskio, J.M.; Redden, L.M.; Volk, L.A.; Bates, D.W. Overrides of medication-related clinical decision support alerts in outpatients. J. Am. Med. Inform. Assoc. 2014, 21, 487–491. [Google Scholar] [CrossRef] [Green Version]
- Bohmer, R.M.J. The Four Habits of High-Value Health Care Organizations. N. Engl. J. Med. 2011, 365, 2045–2047. [Google Scholar] [CrossRef]
- Saha, P.; Sadi, M.S.; Islam, M.M. EMCNet: Automated COVID-19 diagnosis from X-ray images using convolutional neural network and ensemble of machine learning classifiers. Inform. Med. Unlocked 2021, 22, 100505. [Google Scholar] [CrossRef]
- Rahman, M.M.; Islam, M.; Manik, M.; Hossen, M.; Al-Rakhami, M.S. Machine learning approaches for tackling novel coronavirus (COVID-19) pandemic. SN Comput. Sci. 2021, 2, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Asraf, A.; Islam, M.; Haque, M. Deep learning applications to combat novel coronavirus (COVID-19) pandemic. SN Comput. Sci. 2020, 1, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Al-Rakhami, M.S.; Islam, M.M.; Islam, M.Z.; Asraf, A.; Sodhro, A.H.; Ding, W.J.M. Diagnosis of COVID-19 from X-rays using combined CNN-RNN architecture with transfer learning. MedRxiv 2021. [CrossRef]
- Baysari, M.T.; Westbrook, J.I.; Richardson, K.L.; Day, R.O. The influence of computerized decision support on prescribing during ward-rounds: Are the decision-makers targeted? J. Am. Med. Inform. Assoc. 2011, 18, 754–759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riedmann, D.; Jung, M.; Hackl, W.O.; Stühlinger, W.; van der Sijs, H.; Ammenwerth, E. Development of a context model to prioritize drug safety alerts in CPOE systems. BMC Med. Inform. Decis. Mak. 2011, 11, 35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olakotan, O.O.; Yusof, M.M. Evaluating the alert appropriateness of clinical decision support systems in supporting clinical workflow. J. Biomed. Inform. 2020, 106, 103453. [Google Scholar] [CrossRef]
- Chien, S.-C.; Chin, Y.-P.; Yoon, C.-H.; Chen, C.-Y.; Hsu, C.-K.; Chien, C.-H.; Li, Y.-C. A Tool to Retrieve Alert Dwell Time from a Homegrown Computerized Physician Order Entry (CPOE) System of an Academic Medical Center: An Exploratory Analysis. Appl. Sci. 2021, 11, 12004. [Google Scholar] [CrossRef]
- McDaniel, R.B.; Burlison, J.D.; Baker, D.K.; Hasan, M.; Robertson, J.; Hartford, C.; Howard, S.C.; Sablauer, A.; Hoffman, J.M. Alert dwell time: Introduction of a measure to evaluate interruptive clinical decision support alerts. J. Am. Med. Inform. Assoc. 2016, 23, e138–e141. [Google Scholar] [CrossRef] [Green Version]
- Nanji, K.C.; Seger, D.L.; Slight, S.P.; Amato, M.G.; Beeler, P.E.; Her, Q.L.; Dalleur, O.; Eguale, T.; Wong, A.; Silvers, E.R.; et al. Medication-related clinical decision support alert overrides in inpatients. J. Am. Med. Inform. Assoc. 2018, 25, 476–481. [Google Scholar] [CrossRef]
- Ancker, J.S.; Edwards, A.; Nosal, S.; Hauser, D.; Mauer, E.; Kaushal, R. Effects of workload, work complexity, and repeated alerts on alert fatigue in a clinical decision support system. BMC Med. Inform. Decis. Mak. 2017, 17, 36. [Google Scholar] [CrossRef] [Green Version]
- Légat, L.; Van Laere, S.; Nyssen, M.; Steurbaut, S.; Dupont, A.G.; Cornu, P. Clinical decision support systems for drug allergy checking: Systematic review. J. Med. Internet Res. 2018, 20, e258. [Google Scholar] [CrossRef] [PubMed]
- Phansalkar, S.; Van der Sijs, H.; Tucker, A.D.; Desai, A.A.; Bell, D.S.; Teich, J.M.; Middleton, B.; Bates, D.W. Drug—drug interactions that should be non-interruptive in order to reduce alert fatigue in electronic health records. J. Am. Med. Inform. Assoc. 2013, 20, 489–493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blecker, S.; Austrian, J.S.; Horwitz, L.I.; Kuperman, G.; Shelley, D.; Ferrauiola, M.; Katz, S.D. Interrupting providers with clinical decision support to improve care for heart failure. Int. J. Med. Inform. 2019, 131, 103956. [Google Scholar] [CrossRef] [PubMed]
- Khreis, N.; Lau, A.; Al-Jedai, A.; Al-Khani, S.M.; Alruwaili, E.H. An Evaluation of Clinical Decision Support and Use of Machine Learning to Reduce Alert Fatigue. Int. J. Comput. Commun. Eng. 2019, 8, 32–39. [Google Scholar] [CrossRef] [Green Version]
- Baron, J.M.; Huang, R.; McEvoy, D.; Dighe, A.S. Use of machine learning to predict clinical decision support compliance, reduce alert burden, and evaluate duplicate laboratory test ordering alerts. JAMIA Open 2021, 4, ooab006. [Google Scholar] [CrossRef]
- Payne, T.H.; Hines, L.E.; Chan, R.C.; Hartman, S.; Kapusnik-Uner, J.; Russ, A.L.; Chaffee, B.W.; Hartman, C.; Tamis, V.; Galbreth, B.; et al. Recommendations to improve the usability of drug-drug interaction clinical decision support alerts. J. Am. Med. Inform. Assoc. 2015, 22, 1243–1250. [Google Scholar] [CrossRef] [Green Version]
- Bright, T.J.; Wong, A.; Dhurjati, R.; Bristow, E.; Bastian, L.; Coeytaux, R.R.; Samsa, G.; Hasselblad, V.; Williams, J.W.; Musty, M.D.; et al. Effect of Clinical Decision-Support Systems. Ann. Intern. Med. 2012, 157, 29–43. [Google Scholar] [CrossRef]
- Roumeliotis, N.; Sniderman, J.; Adams-Webber, T.; Addo, N.; Anand, V.; Rochon, P.; Taddio, A.; Parshuram, C. Effect of Electronic Prescribing Strategies on Medication Error and Harm in Hospital: A Systematic Review and Meta-analysis. J. Gen. Intern. Med. 2021, 34, 2210–2223. [Google Scholar] [CrossRef]
- Steitz, B.D.; Li, G.; Wright, A.; Dunworth, B.; Freundlich, R.E.; Wanderer, J.P. Non-Interruptive Clinical Decision Support to Improve Perioperative Electronic Positive Patient Identification. J. Med. Syst. 2022, 46, 15. [Google Scholar] [CrossRef]
- Seidling, H.M.; Phansalkar, S.; Seger, D.L.; Paterno, M.D.; Shaykevich, S.; Haefeli, W.E.; Bates, D.W. Factors influencing alert acceptance: A novel approach for predicting the success of clinical decision support. J. Am. Med. Inform. Assoc. 2011, 18, 479–484. [Google Scholar] [CrossRef]
- McCoy, A.B.; Waitman, L.R.; Lewis, J.B.; Wright, J.A.; Choma, D.P.; Miller, R.A.; Peterson, J.F. A framework for evaluating the appropriateness of clinical decision support alerts and responses. J. Am. Med. Inform. Assoc. 2012, 19, 346–352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bryant, A.D.; Fletcher, G.S.; Payne, T.H. Drug interaction alert override rates in the Meaningful Use era. Appl. Clin. Inform. 2014, 5, 802–813. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seidling, H.M.; Klein, U.; Schaier, M.; Czock, D.; Theile, D.; Pruszydlo, M.G.; Kaltschmidt, J.; Mikus, G.; Haefeli, W.E. What, if all alerts were specific–estimating the potential impact on drug interaction alert burden. Int. J. Med. Inform. 2014, 83, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Coleman, J.J.; van der Sijs, H.; Haefeli, W.E.; Slight, S.P.; McDowell, S.E.; Seidling, H.M.; Eiermann, B.; Aarts, J.; Ammenwerth, E.; Ferner, R.E.; et al. On the alert: Future priorities for alerts in clinical decision support for computerized physician order entry identified from a European workshop. BMC Med. Inform. Decis. Mak. 2013, 13, 1–8. [Google Scholar]
- Slight, S.P.; Seger, D.L.; Nanji, K.C.; Cho, I.; Maniam, N.; Dykes, P.C.; Bates, D.W. Are we heeding the warning signs? Examining providers’ overrides of computerized drug-drug interaction alerts in primary care. PLoS ONE 2013, 8, e85071. [Google Scholar] [CrossRef] [Green Version]
- Saverno, K.R.; Hines, L.E.; Warholak, T.L.; Grizzle, A.J.; Babits, L.; Clark, C.; Taylor, A.M.; Malone, D.C. Ability of pharmacy clinical decision-support software to alert users about clinically important drug—drug interactions. J. Am. Med. Inform. Assoc. 2011, 18, 32–37. [Google Scholar] [CrossRef] [Green Version]
- Carspecken, C.W.; Sharek, P.J.; Longhurst, C.; Pageler, N.M. A clinical case of electronic health record drug alert fatigue: Consequences for patient outcome. Pediatrics 2013, 131, e1970–e1973. [Google Scholar] [CrossRef] [Green Version]
- Bell, G.C.; Crews, K.R.; Wilkinson, M.R.; Haidar, C.E.; Hicks, J.K.; Baker, D.K.; Kornegay, N.M.; Yang, W.; Cross, S.J.; Howard, S.C.; et al. Development and use of active clinical decision support for preemptive pharmacogenomics. J. Am. Med. Inform. Assoc. 2014, 21, e93–e99. [Google Scholar] [CrossRef]
- Wright, A.; Hickman, T.T.T.; McEvoy, D.; Aaron, S.; Ai, A.; Andersen, J.M.; Hussain, S.; Ramoni, R.; Fiskio, J.; Sittig, D.F.; et al. Analysis of clinical decision support system malfunctions: A case series and survey. J. Am. Med. Inform. Assoc. 2016, 23, 1068–1076. [Google Scholar] [CrossRef] [Green Version]
- Russ, A.L.; Zillich, A.J.; McManus, M.S.; Doebbeling, B.N.; Saleem, J.J. Prescribers’ interactions with medication alerts at the point of prescribing: A multi-method, in situ investigation of the human–computer interaction. Int. J. Med. Inform. 2012, 81, 232–243. [Google Scholar] [CrossRef]
- Eppenga, W.L.; Derijks, H.J.; Conemans, J.M.; Hermens, W.A.; Wensing, M.; De Smet, P.A. Comparison of a basic and an advanced pharmacotherapy-related clinical decision support system in a hospital care setting in the Netherlands. J. Am. Med. Inform. Assoc. 2012, 19, 66–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scott, G.P.; Shah, P.; Wyatt, J.C.; Makubate, B.; Cross, F.W. Making electronic prescribing alerts more effective: Scenario-based experimental study in junior doctors. J. Am. Med. Inform. Assoc. 2011, 18, 789–798. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duke, J.D.; Li, X.; Dexter, P. Adherence to drug—drug interaction alerts in high-risk patients: A trial of context-enhanced alerting. J. Am. Med. Inform. Assoc. 2013, 20, 494–498. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scheife, R.T.; Hines, L.E.; Boyce, R.D.; Chung, S.P.; Momper, J.D.; Sommer, C.D.; Abernethy, D.R.; Horn, J.R.; Sklar, S.J.; Wong, S.K.; et al. Consensus recommendations for systematic evaluation of drug-drug interaction evidence for clinical decision support. Drug Saf. 2015, 38, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Russ, A.L.; Zillich, A.J.; Melton, B.L.; Russell, S.A.; Chen, S.; Spina, J.R.; Weiner, M.; Johnson, E.G.; Daggy, J.K.; McManus, M.S.; et al. Applying human factors principles to alert design increases efficiency and reduces prescribing errors in a scenario-based simulation. J. Am. Med. Inform. Assoc. 2014, 21, e287–e296. [Google Scholar] [CrossRef] [Green Version]
- Topaz, M.; Seger, D.L.; Slight, S.P.; Goss, F.; Lai, K.; Wickner, P.G.; Blumenthal, K.; Dhopeshwarkar, N.; Chang, F.; Bates, D.W.; et al. Rising drug allergy alert overrides in electronic health records: An observational retrospective study of a decade of experience. J. Am. Med. Inform. Assoc. 2016, 23, 601–608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Romano, M.J.; Stafford, R.S. Electronic health records and clinical decision support systems: Impact on national ambulatory care quality. Arch. Intern. Med. 2011, 171, 897–903. [Google Scholar] [CrossRef]
- Wright, A.; Sittig, D.F.; Ash, J.S.; Bates, D.W.; Feblowitz, J.; Fraser, G.; Maviglia, S.M.; McMullen, C.; Nichol, W.P.; Pang, J.E.; et al. Governance for clinical decision support: Case studies and recommended practices from leading institutions. J. Am. Med. Inform. Assoc. 2011, 18, 187–194. [Google Scholar] [CrossRef] [Green Version]
- Hoffman, J.M.; Haidar, C.E.; Wilkinson, M.R.; Crews, K.R.; Baker, D.K.; Kornegay, N.M.; Yang, W.; Pui, C.H.; Reiss, U.M.; Gaur, A.H.; et al. PG4KDS: A model for the clinical implementation of pre-emptive pharmacogenetics. Am. J. Med. Genetics. Part C Semin. Med. Genet. 2014, 166c, 45–55. [Google Scholar] [CrossRef] [Green Version]

| # | Journals | Item | TGC | TGC per Item | IF (2020) | |
|---|---|---|---|---|---|---|
| N | % | |||||
| 1 | Journal of the American Medical Informatics Association | 93 | 22.7 | 2798 | 30.1 | 4.50 |
| 2 | Applied Clinical Informatics | 74 | 18.1 | 232 | 3.1 | 2.34 |
| 3 | International Journal of Medical Informatics | 47 | 11.5 | 558 | 11.9 | 4.05 |
| 4 | BMC Medical Informatics and Decision Making | 34 | 8.3 | 258 | 7.6 | 2.80 |
| 5 | American Journal of Health-system Pharmacy | 16 | 3.9 | 289 | 18.1 | 2.64 |
| 6 | JMIR Medical Informatics | 16 | 3.9 | 18 | 1.1 | 2.96 |
| 7 | PLoS ONE | 15 | 3.7 | 157 | 10.5 | 3.24 |
| 8 | International Journal of Clinical Pharmacy | 14 | 3.4 | 57 | 4.1 | 2.05 |
| 9 | Journal of Clinical Pharmacy and Therapeutics | 11 | 2.7 | 89 | 8.1 | 2.51 |
| 10 | Drug Safety | 9 | 2.2 | 201 | 22.3 | 5.61 |
| 11 | BMJ Quality & Safety | 9 | 2.2 | 88 | 9.8 | 7.04 |
| 12 | Artificial Intelligence in Medicine | 9 | 2.2 | 63 | 7.0 | 5.33 |
| 13 | CIN-COMPUTERS INFORMATICS NURSING | 9 | 2.2 | 32 | 3.6 | 1.99 |
| 14 | Journal of General Internal Medicine | 8 | 2.0 | 311 | 38.9 | 5.13 |
| 15 | Journal of Biomedical Informatics | 8 | 2.0 | 265 | 33.1 | 6.32 |
| 16 | Pharmacoepidemiology and Drug Safety | 8 | 2.0 | 135 | 16.9 | 2.89 |
| 17 | Journal of Medical Systems | 8 | 2.0 | 40 | 5.0 | 4.46 |
| 18 | Medical Care | 7 | 1.7 | 141 | 20.1 | 2.98 |
| 19 | American Journal of Medical Quality | 7 | 1.7 | 36 | 5.1 | 1.85 |
| 20 | American Journal of Clinical Pathology | 7 | 1.7 | 34 | 4.9 | 2.49 |
| # | Institutions | N | Location |
|---|---|---|---|
| 1 | University of Washington | 86 | Seattle, WA, USA |
| 2 | Brigham and Women’s Hospital | 79 | Boston, MA, USA |
| 3 | Harvard Medical School | 70 | Boston, MA, USA |
| 4 | University of Pittsburgh | 68 | Pittsburgh, PA, USA |
| 5 | Harvard University | 66 | Boston, MA, USA |
| 6 | Vanderbilt University | 65 | Nashville, TN, USA |
| 7 | Stanford University | 49 | Stanford, CA, USA |
| 8 | Taipei Medical University | 47 | Taipei, TW |
| 9 | Mayo Clinic | 43 | Scottsdale, AZ, USA |
| 10 | University of Pennsylvania | 43 | Philadelphia, PA, USA |
| 11 | Columbia University | 36 | New York, NY, USA |
| 12 | Partners HealthCare International | 33 | Boston, MA, USA |
| 13 | Indiana University School of Medicine | 32 | Indianapolis, IN, USA |
| 14 | Cincinnati Children’s Hospital Medical Center | 31 | Cincinnati, OH, USA |
| 15 | University of Michigan | 31 | Ann Arbor, MI, USA |
| 16 | Case Western Reserve University | 28 | Cleveland, OH, USA |
| 17 | University of California, Los Angeles | 28 | Los Angeles, CA, USA |
| 18 | Icahn School of Medicine at Mount Sinai | 27 | New York, NY, USA |
| 19 | Indiana University School of Medicine | 26 | Indianapolis, IN, USA |
| 20 | Oregon Health & Science University | 26 | Portland, OR, USA |
| # | Current Research Gap | Suggestion |
|---|---|---|
| 1 | Usually used only a single metric to evaluate the alert system’s efficiency. | Adopting multiple metrics to comprehensively collect perspectives. |
| 2 | Most of the studies focused on specific types of CDSS alerts. | Consider including all types of CDSS alerts to grasp a holistic view of alert usage. |
| 3 | The majority of alerting system designs are rule-based/silo. | An AI-based precision alert system should be considered to implement in the next generation of CDSS. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chien, S.-C.; Chen, Y.-L.; Chien, C.-H.; Chin, Y.-P.; Yoon, C.H.; Chen, C.-Y.; Yang, H.-C.; Li, Y.-C. Alerts in Clinical Decision Support Systems (CDSS): A Bibliometric Review and Content Analysis. Healthcare 2022, 10, 601. https://doi.org/10.3390/healthcare10040601
Chien S-C, Chen Y-L, Chien C-H, Chin Y-P, Yoon CH, Chen C-Y, Yang H-C, Li Y-C. Alerts in Clinical Decision Support Systems (CDSS): A Bibliometric Review and Content Analysis. Healthcare. 2022; 10(4):601. https://doi.org/10.3390/healthcare10040601
Chicago/Turabian StyleChien, Shuo-Chen, Ya-Lin Chen, Chia-Hui Chien, Yen-Po Chin, Chang Ho Yoon, Chun-You Chen, Hsuan-Chia Yang, and Yu-Chuan (Jack) Li. 2022. "Alerts in Clinical Decision Support Systems (CDSS): A Bibliometric Review and Content Analysis" Healthcare 10, no. 4: 601. https://doi.org/10.3390/healthcare10040601
APA StyleChien, S.-C., Chen, Y.-L., Chien, C.-H., Chin, Y.-P., Yoon, C. H., Chen, C.-Y., Yang, H.-C., & Li, Y.-C. (2022). Alerts in Clinical Decision Support Systems (CDSS): A Bibliometric Review and Content Analysis. Healthcare, 10(4), 601. https://doi.org/10.3390/healthcare10040601







