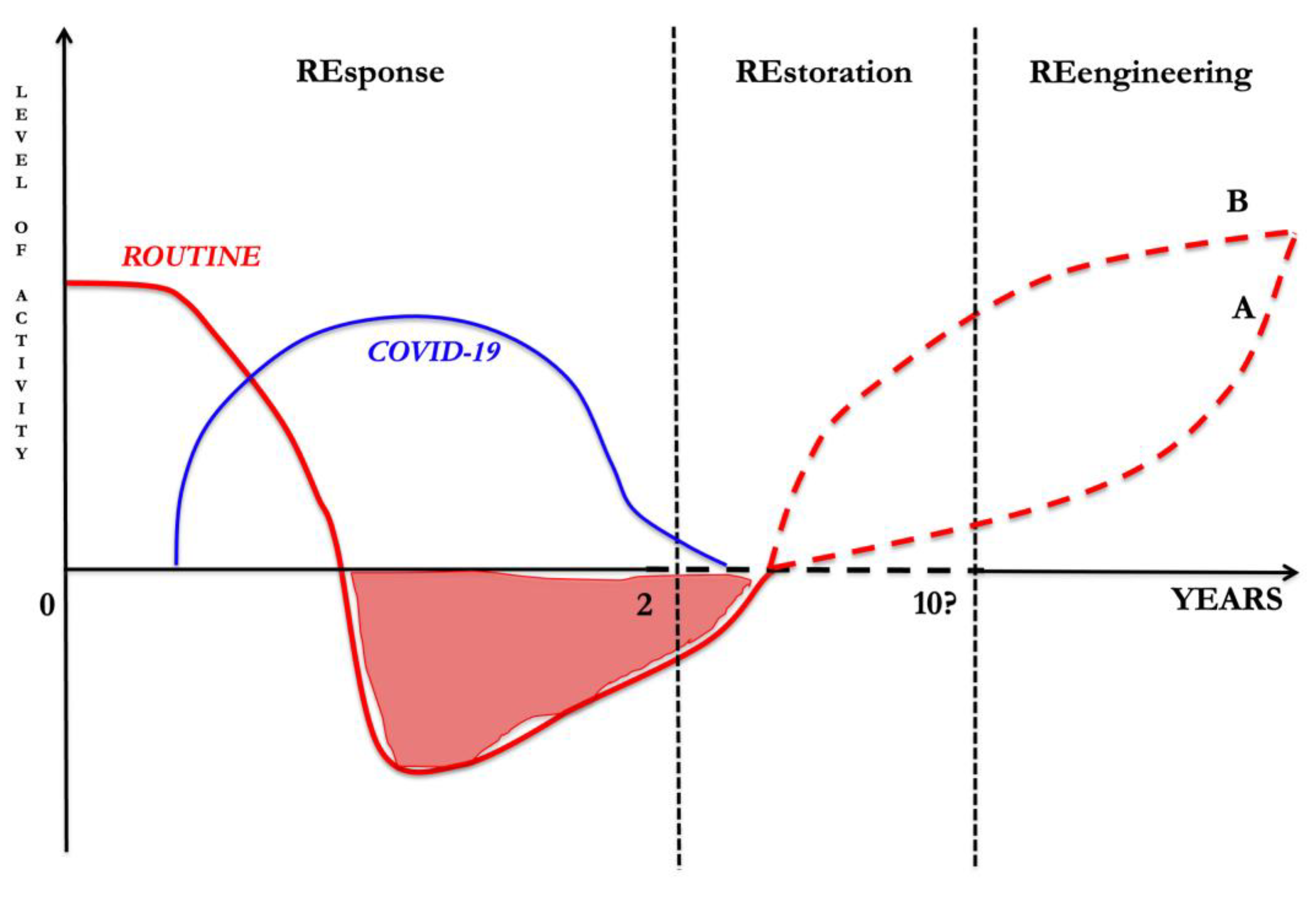
COVID-19 Hurricane: Recovering the Worldwide Health System with the RE.RE.RE. (REsponse–REstoration–REengineering) Approach—Who Will Get There First?
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Available online: https://www.weather.gov/jetstream/katrina (accessed on 28 February 2022).
- Available online: https://covid19.who.int (accessed on 28 February 2022).
- Deana, C.; Rovida, S.; Orso, D.; Bove, T.; Bassi, F.; De Monte, A.; Vetrugno, L. Learning from the Italian experience during COVID-19 pandemic waves: Be prepared and mind some crucial aspects. Acta Biomed. 2021, 92, e2021097. [Google Scholar] [CrossRef] [PubMed]
- Sprung, C.L.; Joynt, G.M.; Christian, M.D.; Truog, R.D.; Rello, J.; Nates, J.L. Adult ICU Triage During the Coronavirus Disease 2019 Pandemic: Who Will Live and Who Will Die? Recommendations to Improve Survival. Crit. Care Med. 2020, 48, 1196–1202. [Google Scholar] [CrossRef] [PubMed]
- Lombardi, Y.; Azoyan, L.; Szychowiak, P.; Bellamine, A.; Lemaitre, G.; Bernaux, M.; Daniel, C.; Leblanc, J.; Riller, Q.; Steichen, O.; et al. External validation of prognostic scores for COVID-19: A multicenter cohort study of patients hospitalized in Greater Paris University Hospitals. Intensive Care Med. 2021, 47, 1426–1439. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.salute.gov.it/portale/nuovocoronavirus/dettaglioNotizieNuovoCoronavirus.jsp?lingua=italiano&id=4186 (accessed on 28 February 2022).
- Alhalaseh, Y.N.; Elshabrawy, H.A.; Erashdi, M.; Shahait, M.; Abu-Humdan, A.M.; Al-Hussaini, M. Allocation of the “Already” Limited Medical Resources amid the COVID-19 Pandemic, an Iterative Ethical Encounter Including Suggested Solutions from a Real Life Encounter. Front. Med. 2021, 7, 616277. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Antonelli, M.; Cabrini, L.; Castelli, A.; Cereda, D.; Coluccello, A.; Foti, G.; Fumagalli, R.; et al. Baseline Characteristics and Outcomes of 1591 Patients Infected with SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 2020, 323, 1574–1581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grieco, D.L.; Maggiore, S.M.; Roca, O.; Spinelli, E.; Patel, B.K.; Thille, A.W.; Barbas, C.S.V.; de Acilu, M.G.; Cutuli, S.L.; Bongiovanni, F.; et al. Non-invasive ventilatory support and high-flow nasal oxygen as first-line treatment of acute hypoxemic respiratory failure and ARDS. Intensive Care Med. 2021, 47, 851–866. [Google Scholar] [CrossRef] [PubMed]
- Chandel, A.; Patolia, S.; Brown, A.W.; Collins, A.C.; Sahjwani, D.; Khangoora, V.; Cameron, P.C.; Desai, M.; Kasarabada, A.; Kilcullen, J.K.; et al. High-Flow Nasal Cannula Therapy in COVID-19: Using the ROX Index to Predict Success. Respir. Care 2021, 66, 909–919. [Google Scholar] [CrossRef] [PubMed]
- Ranieri, V.M.; Tonetti, T.; Navalesi, P.; Nava, S.; Antonelli, M.; Pesenti, A.; Grasselli, G.; Grieco, D.L.; Menga, L.S.; Pisani, L.; et al. High Flow Nasal Oxygen for Severe Hypoxemia: Oxygenation Response and Outcome in COVID-19 Patients. Am. J. Respir. Crit. Care Med. 2021, 205, 431–439. [Google Scholar] [CrossRef] [PubMed]
- Vetrugno, L.; Baciarello, M.; Bignami, E.; Bonetti, A.; Saturno, F.; Orso, D.; Girometti, R.; Cereser, L.; Bove, T. The “pandemic” increase in lung ultrasound use in response to Covid-19: Can we complement computed tomography findings? A narrative review. Ultrasound J. 2020, 12, 39. [Google Scholar] [CrossRef] [PubMed]
- Vetrugno, L.; Sala, A.; Orso, D.; Meroi, F.; Fabbro, S.; Boero, E.; Valent, F.; Cammarota, G.; Restaino, S.; Vizzielli, G.; et al. Lung Ultrasound Signs and Their Correlation with Clinical Symptoms in COVID-19 Pregnant Women: The “PINK-CO” Observational Study. Front. Med. 2022, 8, 768261. [Google Scholar] [CrossRef]
- Deshpande, C. Thromboembolic Findings in COVID-19 Autopsies: Pulmonary Thrombosis or Embolism? Ann. Intern. Med. 2020, 173, 394–395. [Google Scholar] [CrossRef]
- Gattinoni, L.; Chiumello, D.; Rossi, S. COVID-19 pneumonia: ARDS or not? Crit. Care 2020, 24, 154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Griffin, S. Covid-19: Waiting times in England reach record highs. BMJ 2020, 370, m3557. [Google Scholar] [CrossRef] [PubMed]
- COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: Global predictive modelling to inform surgical recovery plans. Br. J. Surg. 2020, 107, 1440–1449. [Google Scholar] [CrossRef]
- Blecker, S.; Jones, S.A.; Petrilli, C.M.; Admon, A.J.; Weerahandi, H.; Francois, F.; Horwitz, L.I. Hospitalizations for chronic disease and acute conditions in the time of COVID-19. JAMA Intern. Med. 2021, 181, 269–271. [Google Scholar] [CrossRef] [PubMed]
- Kates, R.W.; Colten, C.E.; Laska, S.; Leatherman, S.P. Reconstruction of New Orleans after Hurricane Katrina: A research perspective. Proc. Natl. Acad. Sci. USA 2006, 103, 14653–14660. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Available online: http://www.quotidianosanita.it/studi-e-analisi/articolo.php?articolo_id=102539&fr=n (accessed on 28 February 2022).
- Haldane, V.; De Foo, C.; Abdalla, S.M.; Jung, A.-S.; Tan, M.; Wu, S.; Chua, A.; Verma, M.; Shrestha, P.; Singh, S.; et al. Health systems resilience in managing the COVID-19 pandemic: Lessons from 28 countries. Nat. Med. 2021, 27, 964–980. [Google Scholar] [CrossRef] [PubMed]
- Bokolo, A.J. Exploring the adoption of telemedicine and virtual software for care of outpatients during and after COVID-19 pandemic. Ir. J. Med. Sci. 2021, 190, 1–10. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vetrugno, L.; Deana, C.; Maggiore, S.M. COVID-19 Hurricane: Recovering the Worldwide Health System with the RE.RE.RE. (REsponse–REstoration–REengineering) Approach—Who Will Get There First? Healthcare 2022, 10, 602. https://doi.org/10.3390/healthcare10040602
Vetrugno L, Deana C, Maggiore SM. COVID-19 Hurricane: Recovering the Worldwide Health System with the RE.RE.RE. (REsponse–REstoration–REengineering) Approach—Who Will Get There First? Healthcare. 2022; 10(4):602. https://doi.org/10.3390/healthcare10040602
Chicago/Turabian StyleVetrugno, Luigi, Cristian Deana, and Salvatore Maurizio Maggiore. 2022. "COVID-19 Hurricane: Recovering the Worldwide Health System with the RE.RE.RE. (REsponse–REstoration–REengineering) Approach—Who Will Get There First?" Healthcare 10, no. 4: 602. https://doi.org/10.3390/healthcare10040602
APA StyleVetrugno, L., Deana, C., & Maggiore, S. M. (2022). COVID-19 Hurricane: Recovering the Worldwide Health System with the RE.RE.RE. (REsponse–REstoration–REengineering) Approach—Who Will Get There First? Healthcare, 10(4), 602. https://doi.org/10.3390/healthcare10040602





