The Problem of Assigning Patients to Appropriate Health Institutions Using Multi-Criteria Decision Making and Goal Programming in Health Tourism
Abstract
1. Introduction
2. Literature Review
3. Materials and Methods
3.1. Factors Affecting Hospital Selection in Health Tourism and Finding Them
3.1.1. Health Services Fees
3.1.2. Duration of Treatment
3.1.3. Marketing Activities and Recognition (Reputation)
3.1.4. Infrastructure and Technological Facilities of Health Facilities
3.1.5. Health Tourism Department and Number of Staff Fluent in Foreign Languages
3.1.6. Accreditations and Service Quality
3.1.7. Medical Expertise and Experience
3.1.8. Relationships and Agreements with Intermediary Insurance Companies
3.1.9. Additional Services and Facilities
3.2. Multi-Criteria Decision-Making Methods
3.2.1. Group Best-Worst Method (G-BWM)
3.2.2. The Technique for Order of Preference by Similarity to Ideal Solution Method (TOPSIS)
- Initially, the weight values () for the evaluation factors are to be determined.
3.2.3. Goal Programming
- The decision variables are expressed as follows:
- : Positive deviation for goal 1
- : Negative deviation for goal 1
- : Positive deviation for goal 2
- : Negative deviation for goal 2
- Parameters
- Scalars:
- Goals:
- Objective Function
- Constraints
4. Results
4.1. Demographic Data
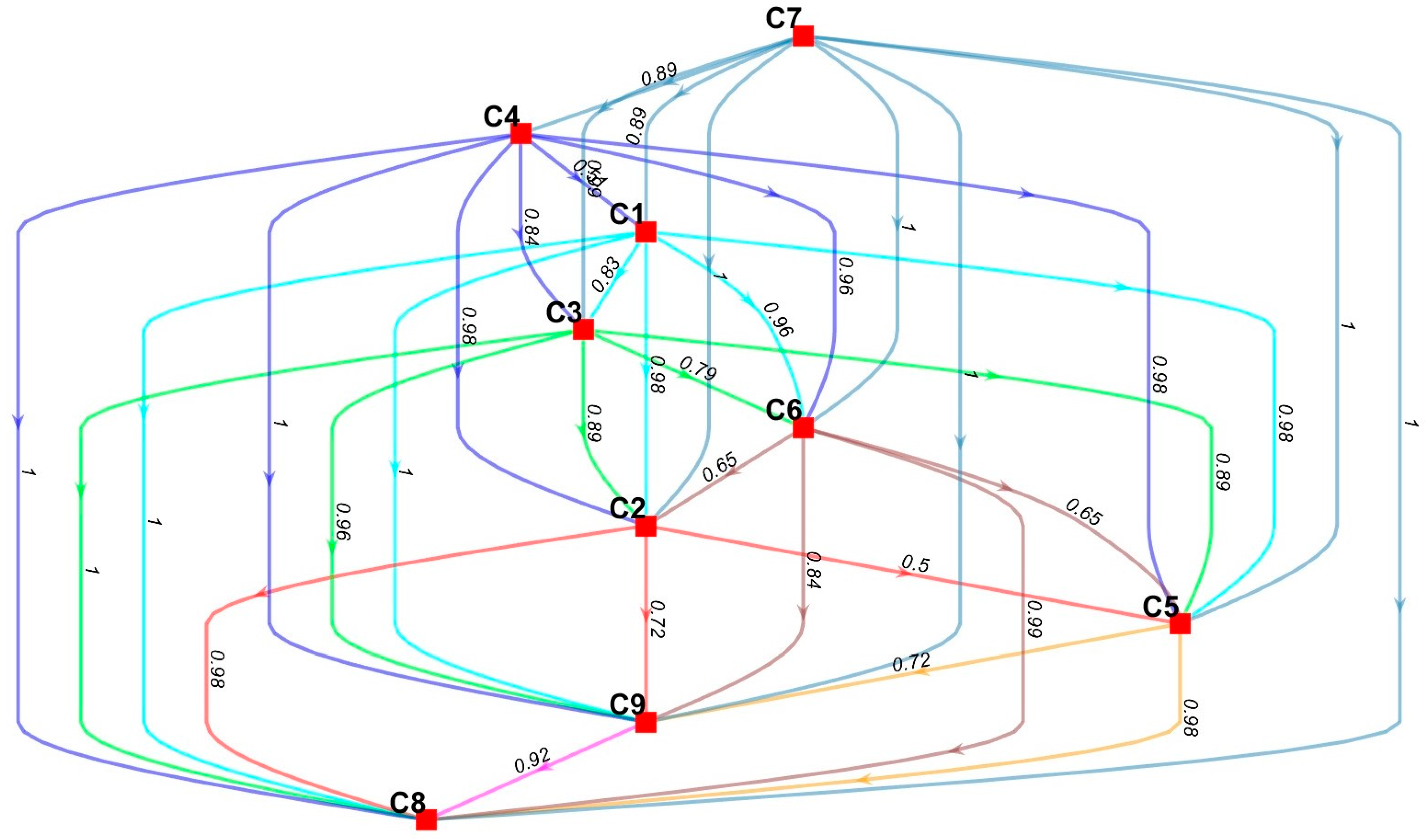
4.2. Group Best-Worst Results
4.3. TOPSIS Results
4.4. Goal Programming Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
- i patient index /1*998/
- j health institution index /1*9/;
- z;
- P1, P2, dR_pos, dR_neg, dS_pos, dS_neg;
- x(i,j);
- R targeted total health institution revenue /9414600/
- S targeted total health institution score /1829.16396/;
- c(j) capacity of the j th health institution
- f(j) treatment fee of the j th health institution
- p(j) institution score of the j th health institution
- objective
- constraint1
- constraint2
- constraint3
- constraint4
- constraint5
- constraint6;
- objective… z =e= P1+P2;
- constraint1… P1 =e= dR_neg/R;
- constraint2… P2 =e= dS_neg/S;
- constraint3… sum((i,j), f(j)*x(i,j))+dR_neg-dR_pos =e= R;
- constraint4… sum((i,j), p(j)*x(i,j))+dS_neg-dS_pos =e= S;
- constraint5(j)… sum(i, x(i,j)) =l= c(j);
- constraint6(i)… sum(j, x(i,j)) =l= 1;
References
- Heung, V.C.S.; Kucukusta, D.; Song, H. A conceptual model of medical tourism: Implications for future research. J. Travel Tour. Mark. 2010, 27, 236–251. [Google Scholar] [CrossRef]
- Tengilimoğlu, D. Sağlık Turizmi; Siyasal Kitabevi: Ankara, Turkey, 2013. [Google Scholar]
- Precedenceresearch. Medical Tourism Market (By Treatment Type: Dental Treatment, Cardiovascular Treatment, Cancer Treatment, Cosmetic Treatment, Orthopedic Treatment, Fertility Treatment, Neurological Treatment, and Other Treatment)—Global Industry Analysis, Size, Share, Growth, Trends, Regional Outlook, and Forecast 2023–2032. 2023. Available online: https://www.precedenceresearch.com/medical-tourism-market (accessed on 4 March 2023).
- Uner, M.M.; Cetin, B.; Cavusgil, S.T. On the internationalization of Turkish hospital chains: A dynamic capabilities perspective. Int. Bus. Rev. 2020, 29, 101693. [Google Scholar] [CrossRef]
- Kurtulmuş, S.; Öztürk, A.O. The rise of medical tourism in Turkey and the unique case of patients from Germany. In Turkish German Affairs from an Interdisciplinary Perspective; Peter Lang GmbH: Berlin, Germany, 2015; pp. 323–352. [Google Scholar]
- Karadayi-Usta, S.; SerdarAsan, S. A Conceptual Model of Medical Tourism Service Supply Chain. J. Ind. Eng. Manag. JIEM 2020, 13, 246–265. [Google Scholar] [CrossRef]
- Karadayi-Usta, S.; Bozdag, C.E. Healthcare service provider type selection of the medical tourists by using neutrosophic sets. In Advances in Intelligent Systems and Computing; Springer: Berlin/Heidelberg, Germany, 2020; Volume 1029, pp. 674–682. [Google Scholar]
- Figueiredo, N.; Abrantes, J.L.; Costa, S. Mapping the sustainable development in health tourism: A systematic literature review. Sustainability 2024, 16, 1901. [Google Scholar] [CrossRef]
- Jalali, M.; Haghgoshayie, E.; Janati, A.; Yoshari, P.; Khodayari-Zarnaq, R. Health tourism: A global perspective on the barriers and facilitators. Discov. Public Health 2025, 22, 157. [Google Scholar] [CrossRef]
- Koç, A. Kayseri İlinin Sağlik Turizmi Potansiyelinin Tespitine Yönelik Nitel Bir Araştirma. İstanbul Kent Üniversitesi İnsan Ve Toplum Bilim. Dergisi 2023, 4, 15–28. [Google Scholar]
- Akın, M.H. Kayseri’nin Sağlık Turizmi Potansiyeline İlişkin Öncelikli Kriterlerin Tespitine Yönelik Bir Araştırma. Yaşar Üniversitesi E Derg. 2024, 19, 352–372. [Google Scholar] [CrossRef]
- Aktunc, E.A.; Tekin, E. Nurse scheduling with shift preferences in a surgical suite using goal programming. In Industrial Engineering in the Industry 4.0 Era; Springer: Vienna, Austria, 2018; pp. 23–36. [Google Scholar]
- Knight, D.R.T.; Aakre, C.A.; Anstine, C.V.; Munipalli, B.; Biazar, P.; Mitri, G.; Valery, J.R.; Brigham, T.; Niazi, S.K.; Perlman, A.I. Artificial intelligence for patient scheduling in the real-world health care setting: A metanarrative review. Health Policy Technol. 2023, 12, 100824. [Google Scholar] [CrossRef]
- Abdalkareem, Z.A.; Amir, A.; Al-Betar, M.A.; Ekhan, P.; Hammouri, A.I. Healthcare scheduling in optimization context: A review. Health Technol. 2021, 11, 445–469. [Google Scholar] [CrossRef]
- Youn, S.; Geismar, H.N.; Pinedo, M. Planning and scheduling in healthcare for better care coordination: Current understanding, trending topics, and future opportunities. Prod. Oper. Manag. 2022, 31, 4407–4423. [Google Scholar] [CrossRef]
- Asadi, R.; Daryaei, M. Strategies for development of Iran health tourism. Euro. J. Soc. Sci 2011, 23, 329–344. [Google Scholar]
- Büyüközkan, G.; Mukul, E.; Kongar, E. Health tourism strategy selection via SWOT analysis and integrated hesitant fuzzy linguistic AHP-MABAC approach. Socio Econ. Plan. Sci. 2021, 74, 100929. [Google Scholar] [CrossRef]
- Riaz, M.; Qamar, F.; Tariq, S.; Alsager, K. AI-Driven LOPCOW-AROMAN Framework and Topological Data Analysis Using Circular Intuitionistic Fuzzy Information: Healthcare Supply Chain Innovation. Mathematics 2024, 12, 3593. [Google Scholar] [CrossRef]
- Attaallah, A.; al-Sulbi, K.; Alasiry, A.; Marzougui, M.; Ansar, S.A.; Agrawal, A.; Ansari, M.T.; Khan, R.A. Fuzzy-Based Unified Decision-Making Technique to Evaluate Security Risks: A Healthcare Perspective. Mathematics 2023, 11, 2554. [Google Scholar] [CrossRef]
- Frej, E.A.; Roselli, L.R.; Alberti, A.R.; Britto, M.A.; de Barros Campelo Júnior, E.; Ferreira, R.J.; de Almeida, A.T. Collaborative Decision Model for Allocating Intensive Care Units Beds with Scarce Resources in Health Systems: A Portfolio Based Approach under Expected Utility Theory and Bayesian Decision Analysis. Mathematics 2023, 11, 659. [Google Scholar] [CrossRef]
- Habib, A.; Khan, Z.A.; Riaz, M.; Marinkovic, D. Performance Evaluation of Healthcare Supply Chain in Industry 4.0 with Linear Diophantine Fuzzy Sine-Trigonometric Aggregation Operations. Mathematics 2023, 11, 2611. [Google Scholar] [CrossRef]
- Lubowiecki-Vikuk, A.; Białk-Wolf, A. Medical tourism research in Poland: A scoping review. Worldw. Hosp. Tour. Themes 2025, 17, 2. [Google Scholar] [CrossRef]
- Chanda, R. Medical value travel in India: Prospects and challenges. In Travelling Well: Essays in Medical Tourism; Institute of Population Health at the University of Ottawa: Ottawa, ON, Canada, 2013. [Google Scholar]
- Ferrer, M.; Medhekar, A. The factors impacting on the management of global medical tourism service supply chain. GSTF J. Bus. Rev. (GBR) 2012, 2. [Google Scholar]
- Islam, F.; Sarwar, A.; Khan, N. Medical Tourism in Malaysia: Community Perspectives on Quality of Life and Healthcare Accessibility. Sustainability 2025, 17, 1226. [Google Scholar] [CrossRef]
- Jain, V.; Ajmera, P. Quantifying the variables affecting Indian medical tourism sector by graph theory and matrix approach. Manag. Sci. Lett. 2018, 8, 225–240. [Google Scholar] [CrossRef]
- Fetscherin, M.; Stephano, R.M. The medical tourism index: Scale development and validation. Tour. Manag. 2016, 52, 539–556. [Google Scholar] [CrossRef]
- Ghosh, T.; Mandal, S. Medical Tourism Experience: Conceptualization, Scale Development, and Validation. J. Travel Res. 2018, 58, 1288–1301. [Google Scholar] [CrossRef]
- Kilavuz, E. Medical tourism competition: The case of Turkey. Int. J. Health Manag. Tour. 2018, 3, 42–58. [Google Scholar] [CrossRef]
- Sevim, E.; Sevim, E. Medikal turizm tercihini etkileyen faktörlerin incelenmesi: Türkiye örneği. Hacet. Sağlık İdaresi Derg. 2019, 22, 633–652. [Google Scholar]
- Üstün, U.; Uslu, Y.D. Türkiye’nin Sağlık Turizminde Tercih Edilme Nedenleri Üzerine Bir Çalışma: Medikal Turizm Endeksi. Avrupa Bilim Ve Teknol. Dergisi 2022, 33, 344–353. [Google Scholar] [CrossRef]
- Ozisik, P.A.; Ozdener, K.M.; Ural, B.; Er, U.; Savas, A. Clinical and ethical perspective of neurosurgical care in patients from beyond the southern border of Turkey: Challenges of patients in war. J. Public Health Heidelb. 2022, 30, 1431–1440. [Google Scholar] [CrossRef]
- Yildiz, M.S.; Khan, M.M. Opportunities for reproductive tourism: Cost and quality advantages of Turkey in the provision of in-vitro Fertilization (IVF) services. BMC Health Serv. Res. 2016, 16, 1–8. [Google Scholar] [CrossRef]
- Ulas, D.; Anadol, Y. A case study for medical tourism: Investigating a private hospital venture in Turkey. Anatolia Int. J. Tour. Hosp. Res. 2016, 27, 327–338. [Google Scholar] [CrossRef]
- Ozan-Rafferty, M.E.; Johnson, J.A.; Shah, G.H.; Kursun, A. In the Words of the Medical Tourist: An Analysis of Internet Narratives by Health Travelers to Turkey. J. Med. Internet Res. 2014, 16, e2694. [Google Scholar] [CrossRef]
- Kowalewski, P.K.; Rogula, T.G.; Lagardere, A.O.; Khwaja, H.A.; Waledziak, M.S.; Janik, M.R. Current Practice of Global Bariatric Tourism-Survey-Based Study. Obes. Surg. 2019, 29, 3553–3559. [Google Scholar] [CrossRef]
- Bayram, H.S.; Akkülah, A.U. Kayseri Sağlik Turizminin Geliştirilmesi Mevcut Durum Analizi Ve 2021–2030 Eylem Plani. 2020. Available online: https://www.kalkinmakutuphanesi.gov.tr/assets/upload/dosyalar/saglik-turizmi-eylem-plani_070920_1445.pdf (accessed on 4 March 2023).
- Zarei, A.; Feiz, D.; Minbashrazgah, M.M.; Maleki, F. Factors influencing selection of medical tourism destinations: A special niche market. Int. J. Healthc. Manag. 2020, 13, 192–198. [Google Scholar] [CrossRef]
- Yildiz, M.S.; Khan, M.M. Factors Affecting the Choice of Medical Tourism Destination: A Case Study of Medical Tourists from the Arab Region in Turkey. J. Health Manag. 2019, 21, 465–475. [Google Scholar] [CrossRef]
- Aydin, G.; Karamehmet, B. Factors affecting health tourism and international health-care facility choice. Int. J. Pharm. Healthc. Mark. 2017, 11, 16–36. [Google Scholar] [CrossRef]
- Oberoi, S.; Kansra, P. Factors influencing medical tourism in India: A critical review. SAMVAD 2019, 17, 9–16. [Google Scholar]
- Mahmoudifar, Y.; Tabibi, S.J.; Nasiripour, A.A.; Riahi, L. Factors affecting development of medical tourism industry in West Azerbaijan province of Iran. Int. J. Health Stud. 2016, 2, 25–31. [Google Scholar]
- Hanefeld, J.; Lunt, N.; Smith, R.; Horsfall, D. Why do medical tourists travel to where they do? The role of networks in determining medical travel. Soc. Sci. Med. 2015, 124, 356–363. [Google Scholar] [CrossRef]
- Sağlık Hizmetleri Genel Müdürlüğü. Sağlıkta Kalite Standartları. 2020. Available online: https://shgmkalitedb.saglik.gov.tr/TR-8850/saglikta-kalite-standartlari.html# (accessed on 14 May 2025).
- Rezaei, J. Best-worst multi-criteria decision-making method. Omega Int. J. Manag. Sci. 2015, 53, 49–57. [Google Scholar] [CrossRef]
- Mohammadi, M.; Rezaei, J. Bayesian best-worst method: A probabilistic group decision making model. Omega Int. J. Manag. Sci. 2020, 96, 102075. [Google Scholar] [CrossRef]
- Rezaei, J. Best-worst multi-criteria decision-making method: Some properties and a linear model. Omega 2016, 64, 126–130. [Google Scholar] [CrossRef]
- Haseli, G.; Sheikh, R.; Wang, J.; Tomaskova, H.; Tirkolaee, E.B. A novel approach for group decision making based on the best–worst method (G-bwm): Application to supply chain management. Mathematics 2021, 9, 1881. [Google Scholar] [CrossRef]
- Çakır, E.; Can, M. Best-Worst Yöntemine Dayalı ARAS Yöntemi ile Dış Kaynak Kullanım Tercihinin Belirlenmesi: Turizm Sektöründe Bir Uygulama. J. Grad. Sch. Soc. Sci. 2019, 23, 1273–1300. [Google Scholar]
- Hwang, C.; Yoon, K. Multiple Attribute Decision Making: Methods and Application; Springer: Berlin/Heidelberg, Germany, 1981. [Google Scholar]
- Güngör, A.; Kocamış, T.U. Halka Açik Futbol Kulüplerinde Finansal Performansin Topsis Yöntemi İle Analizi: İngiltere Uygulamasi. Hitit Üniversitesi Sos. Bilim. Enstitüsü Derg. 2018, 11, 1846–1859. [Google Scholar] [CrossRef]
- Winston, W.L. Operations Research: Applications and Algorithms; Cengage Learning: Boston, MA, USA, 2022. [Google Scholar]
- Sahin, Y. Analitik Hiyerarşi Süreci Yardımıyla Orman ürünleri Sektöründe Lojistik Problemlerin Hedef Programlama Ile çözümlenmesi. Doctoral Thesis, Kahramanmaraş Sütçü İmam University, Onikişubat, Türkiye, 2022. [Google Scholar]
- Hasmukhbhai, C.; Khanna, D.; Patel, D. Practical and Adaptable Applications of Goal Programming: A Literature Review. J. Adv. Zool. 2023, 44, 2938–2946. [Google Scholar] [CrossRef]
- Saaty, T.L. Decision making with the analytic hierarchy process. Int. J. Serv. Sci. 2008, 1, 83–98. [Google Scholar] [CrossRef]
- Mathew, M. Multi-Criteria-Decision-Making TOPSIS. 2018. Available online: https://github.com/MMathew4788/Multi-Criteria-Decision-Making/blob/main/TOPSIS/TOPSIS.m (accessed on 10 March 2025).
- İletişim Başkanlığı. Cumhurbaşkanı Erdoğan’dan 2024 Değerlendirmesi. 2024. Available online: https://www.iletisim.gov.tr/turkce/haberler/detay/cumhurbaskani-erdogandan-2024-degerlendirmesi (accessed on 11 March 2025).
- Turizmdays. Erdoğan, “Turizmde Hedef 90 Milyon Turist ve 100 Milyar Dolar Turizm Geliridir”. 2023. Available online: https://www.turizmdays.com/news/erdogan-turizmde-hedef-90-milyon-turist-ve-100-milyar-dolar-turizm-geliridir-20516 (accessed on 11 March 2025).
| Demographic Information | Gender | Age Range | Education Status | Sector of the Organization | Position in the Organization | Total Range of Work Experience |
|---|---|---|---|---|---|---|
| Expert 1 | Male | 25–34 | Master | Public | Researcher/Scholar | 2–5 years |
| Expert 2 | Female | 18–24 | Associate | Private | International Health Services Consultant | Less than 2 years |
| Expert 3 | Male | 35–44 | Doctorate | Public | Chief Physician | 11–15 years |
| Expert 4 | Female | 45–54 | Master | Private | Hospital Director | 20+ years |
| Expert 5 | Male | 54+ | Master | Private | Hospital Director | 20+ years |
| Expert 6 | Male | 35–44 | Bachelor | Private | Deputy Business Director | 20+ years |
| Expert 7 | Female | 35–44 | Master | Private | Quality Expert | 20+ years |
| Expert 8 | Female | 35–44 | Bachelor | Private | Director of Health Services | 20+ years |
| Expert 9 | Female | 35–44 | Associate | Private | Corporate Communication Officer | 20+ years |
| Expert 10 | Female | 35–44 | Associate | Private | Quality Management Officer | 16–20 years |
| Expert 11 | Male | 25–34 | Bachelor | Private | Corporate Marketing Expert | 6–10 years |
| Experts/Criterion (Best to Others) | The Best Criteria | C1 | C2 | C3 | C4 | C5 | C6 | C7 | C8 | C9 |
|---|---|---|---|---|---|---|---|---|---|---|
| Expert 1 | C7 | 3 | 9 | 5 | 3 | 5 | 2 | 1 | 9 | 8 |
| Expert 2 | C1 | 1 | 3 | 3 | 2 | 3 | 4 | 3 | 6 | 3 |
| Expert 3 | C4 | 6 | 6 | 5 | 1 | 6 | 4 | 5 | 9 | 3 |
| Expert 4 | C4 | 2 | 7 | 7 | 1 | 7 | 7 | 9 | 3 | 3 |
| Expert 5 | C7 | 2 | 5 | 8 | 3 | 7 | 4 | 1 | 6 | 9 |
| Expert 6 | C7 | 7 | 5 | 7 | 9 | 3 | 7 | 1 | 9 | 9 |
| Expert 7 | C7 | 3 | 3 | 3 | 7 | 9 | 3 | 1 | 8 | 4 |
| Expert 8 | C7 | 7 | 5 | 7 | 3 | 9 | 7 | 1 | 9 | 9 |
| Expert 9 | C7 | 5 | 7 | 3 | 2 | 7 | 9 | 1 | 9 | 8 |
| Expert 10 | C3 | 9 | 7 | 1 | 7 | 7 | 7 | 7 | 9 | 9 |
| Expert 11 | C1 | 1 | 9 | 3 | 5 | 7 | 6 | 3 | 9 | 5 |
| Experts/Criterion (Others to Worst) | The Worst Criteria | C1 | C2 | C3 | C4 | C5 | C6 | C7 | C8 | C9 |
|---|---|---|---|---|---|---|---|---|---|---|
| Expert 1 | C2 | 7 | 1 | 6 | 8 | 5 | 8 | 9 | 4 | 3 |
| Expert 2 | C8 | 9 | 8 | 7 | 7 | 8 | 6 | 8 | 1 | 7 |
| Expert 3 | C8 | 6 | 5 | 4 | 9 | 6 | 4 | 5 | 1 | 4 |
| Expert 4 | C8 | 3 | 6 | 6 | 9 | 7 | 8 | 9 | 1 | 5 |
| Expert 5 | C9 | 8 | 6 | 4 | 7 | 3 | 5 | 9 | 3 | 1 |
| Expert 6 | C9 | 9 | 8 | 7 | 8 | 9 | 6 | 9 | 7 | 1 |
| Expert 7 | C8 | 6 | 8 | 8 | 8 | 6 | 6 | 9 | 1 | 8 |
| Expert 8 | C2 | 7 | 1 | 5 | 8 | 7 | 5 | 9 | 7 | 5 |
| Expert 9 | C8 | 7 | 8 | 9 | 8 | 6 | 3 | 9 | 1 | 7 |
| Expert 10 | C4 | 9 | 7 | 9 | 1 | 7 | 3 | 7 | 9 | 9 |
| Expert 11 | C5 | 9 | 3 | 5 | 5 | 1 | 7 | 8 | 6 | 3 |
| Criterion | Criteria Weights |
|---|---|
| C1 (Health Services Fees ($)) | 0.134 |
| C2 (Duration of Treatment (Day)) | 0.0969 |
| C3 (Marketing Activities and Recognition (Reputation) (1–5)) | 0.1163 |
| C4 (Infrastructure and Technological Facilities of Health Facilities (1–5)) | 0.1345 |
| C5 (Health Tourism Department and Number of Staff Fluent in Foreign Languages (Number of Languages)) | 0.0968 |
| C6 (Accreditations and Service Quality (HQS Score)) | 0.1029 |
| C7 (Medical Expertise and Experience (Years)) | 0.1601 |
| C8 (Relationships and Agreements with Intermediary-Insurance Companies (1–5)) | 0.0703 |
| C9 (Additional Services and Facilities (1–5)) | 0.0882 |
| HFN/C | C1 | C2 | C3 | C4 | C5 | C6 | C7 | C8 | C9 |
|---|---|---|---|---|---|---|---|---|---|
| H1 | 2500 | 7 | 5 | 3 | 7 | 94.6 | 0 | 5 | 5 |
| H2 | 2500 | 2.67 | 5 | 4 | 6 | 88 | 20.4 | 5 | 5 |
| H3 | 2750 | 2.33 | 3 | 4 | 3 | 96.6 | 23.33 | 3 | 4 |
| H4 | 2370 | 2.33 | 5 | 5 | 4 | 88 | 16.67 | 4 | 4 |
| H5 | 12000 | 1.56 | 2 | 3 | 3 | 97.74 | 17.5 | 3 | 2 |
| H6 | 2750 | 5 | 2 | 4 | 3 | 92 | 20.5 | 1 | 3 |
| H7 | 3833 | 4 | 5 | 4 | 10 | 88 | 16.5 | 5 | 2 |
| H8 | 2500 | 2.67 | 2 | 3 | 4 | 86 | 14 | 5 | 5 |
| H9 | 3550 | 4 | 1 | 5 | 2 | 97.3 | 30 | 2 | 2 |
| HFN | TOPSIS Score |
|---|---|
| H2 | 0.76209 |
| H4 | 0.69233 |
| H7 | 0.68973 |
| H3 | 0.6829 |
| H9 | 0.61436 |
| H8 | 0.6079 |
| H6 | 0.59111 |
| H1 | 0.5196 |
| H5 | 0.37526 |
| HFN | NPT-Q1 | NPT-Q2 | NPT-Q3 | NPT-Q4 | CP-Q1 | CP-Q2 | CP-Q3 | CP-Q4 |
|---|---|---|---|---|---|---|---|---|
| H1 | 15 | 10 | 10 | 5 | 0 | 0 | 0 | 0 |
| H2 | 720 | 540 | 810 | 450 | 1350 | 1350 | 1350 | 1350 |
| H3 | 0 | 0 | 1 | 0 | 60 | 60 | 60 | 60 |
| H4 | 230 | 250 | 275 | 108 | 270 | 270 | 270 | 270 |
| H5 | 6 | 4 | 0 | 0 | 60 | 60 | 60 | 60 |
| H6 | 17 | 15 | 18 | 13 | 15 | 15 | 15 | 15 |
| H7 | 1 | 1 | 1 | 0 | 225 | 225 | 225 | 225 |
| H8 | 9 | 8 | 12 | 7 | 900 | 900 | 900 | 900 |
| H9 | 0 | 0 | 0 | 0 | 90 | 90 | 90 | 90 |
| (a) | ||||||||
| Scenario | Quarter | SNP | SIR | TIR | MRT (%) | SIS | TIS | MST (%) |
| 1 | 1 | 998 | 3,459,425 | 9,414,600 | 36.75 | 707.779 | 1829.164 | 38.69 |
| 1 | 2 | 828 | 3,034,425 | 9,414,600 | 32.23 | 578.224 | 1829.164 | 31.61 |
| 1 | 3 | 1127 | 3,781,925 | 9,414,600 | 40.17 | 806.089 | 1829.164 | 44.07 |
| 1 | 4 | 583 | 2,421,925 | 9,414,600 | 25.73 | 391.512 | 1829.164 | 21.40 |
| 2 | 1 | 1996 | 5,941,995 | 9,414,600 | 63.11 | 1448.874 | 1829.164 | 79.21 |
| 2 | 2 | 1656 | 5,104,425 | 9,414,600 | 54.22 | 1209.235 | 1829.164 | 66.11 |
| 2 | 3 | 2254 | 6,583,075 | 9,414,600 | 69.92 | 1610.442 | 1829.164 | 88.04 |
| 2 | 4 | 1166 | 3,879,425 | 9,414,600 | 41.21 | 835.810 | 1829.164 | 45.69 |
| 3 | 1 | 2994 | 8,373,075 | 9,414,600 | 88.94 | 2045.699 | 1829.164 | 111.84 |
| 3 | 2 | 2484 | 7,158,075 | 9,414,600 | 76.03 | 1750.259 | 1829.164 | 95.69 |
| 3 | 3 | 3381 | 8,373,075 | 9,414,600 | 88.94 | 2045.699 | 1829.164 | 111.84 |
| 3 | 4 | 1749 | 5,342,925 | 9,414,600 | 56.75 | 1278.208 | 1829.164 | 69.88 |
| (b) | ||||||||
| Scenario | Quarter | dR_pos | dR_neg | dS_pos | dS_neg | P1 | P2 | Z |
| 1 | 1 | 0 | 5,955,175 | 0.000 | 1121.385 | 0.633 | 0.613 | 1.246 |
| 1 | 2 | 0 | 6,380,175 | 0.000 | 1250.940 | 0.678 | 0.684 | 1.362 |
| 1 | 3 | 0 | 5,632,675 | 0.000 | 1023.075 | 0.598 | 0.559 | 1.158 |
| 1 | 4 | 0 | 6,992,675 | 0.000 | 1437.652 | 0.743 | 0.786 | 1.529 |
| 2 | 1 | 0 | 3,472,605 | 0.000 | 380.290 | 0.369 | 0.208 | 0.577 |
| 2 | 2 | 0 | 4,310,175 | 0.000 | 619.929 | 0.458 | 0.339 | 0.797 |
| 2 | 3 | 0 | 2,831,525 | 0.000 | 218.722 | 0.301 | 0.120 | 0.420 |
| 2 | 4 | 0 | 5,535,175 | 0.000 | 993.354 | 0.588 | 0.543 | 1.131 |
| 3 | 1 | 0 | 1,041,525 | 216.535 | 0.000 | 0.111 | 0.000 | 0.111 |
| 3 | 2 | 0 | 2,256,525 | 0.000 | 78.905 | 0.240 | 0.043 | 0.283 |
| 3 | 3 | 0 | 1,041,525 | 216.535 | 0.000 | 0.111 | 0.000 | 0.111 |
| 3 | 4 | 0 | 4,071,675 | 0.000 | 550.956 | 0.432 | 0.301 | 0.734 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arsav, M.S.; Ayvaz-Çavdaroğlu, N.; Şenyiğit, E. The Problem of Assigning Patients to Appropriate Health Institutions Using Multi-Criteria Decision Making and Goal Programming in Health Tourism. Mathematics 2025, 13, 1684. https://doi.org/10.3390/math13101684
Arsav MS, Ayvaz-Çavdaroğlu N, Şenyiğit E. The Problem of Assigning Patients to Appropriate Health Institutions Using Multi-Criteria Decision Making and Goal Programming in Health Tourism. Mathematics. 2025; 13(10):1684. https://doi.org/10.3390/math13101684
Chicago/Turabian StyleArsav, Murat Suat, Nur Ayvaz-Çavdaroğlu, and Ercan Şenyiğit. 2025. "The Problem of Assigning Patients to Appropriate Health Institutions Using Multi-Criteria Decision Making and Goal Programming in Health Tourism" Mathematics 13, no. 10: 1684. https://doi.org/10.3390/math13101684
APA StyleArsav, M. S., Ayvaz-Çavdaroğlu, N., & Şenyiğit, E. (2025). The Problem of Assigning Patients to Appropriate Health Institutions Using Multi-Criteria Decision Making and Goal Programming in Health Tourism. Mathematics, 13(10), 1684. https://doi.org/10.3390/math13101684







