Graph Network Techniques to Model and Analyze Emergency Department Patient Flow
Abstract
:1. Introduction
1.1. New Contribution
1.2. Medical Knowledge Graphs
1.3. Graph Databases
1.4. Implementation of Knowledge Graph in Emergency Department
1.5. Contributions
2. Methods
2.1. Graph Network Modeling
2.2. Graph Network Metrics
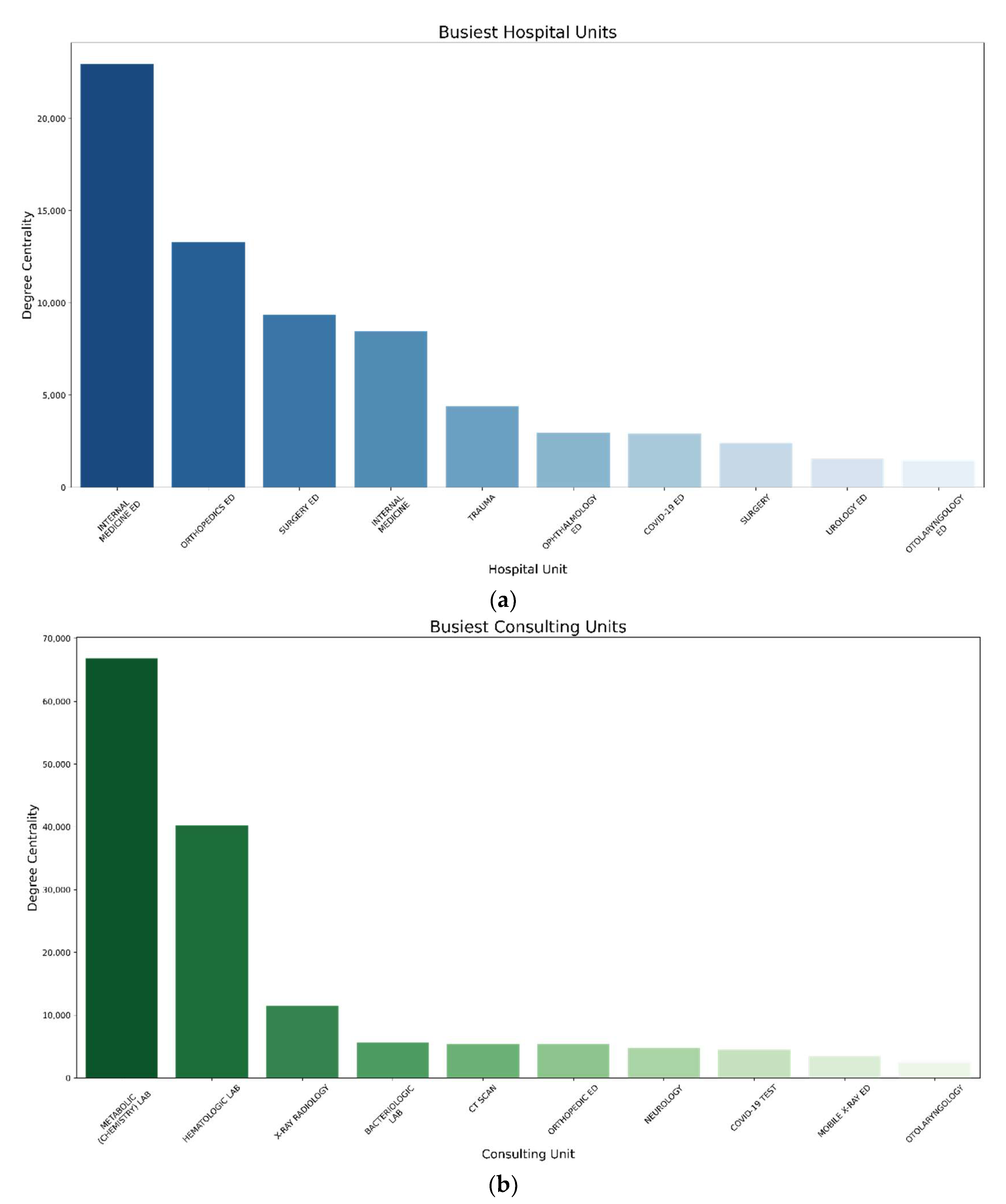
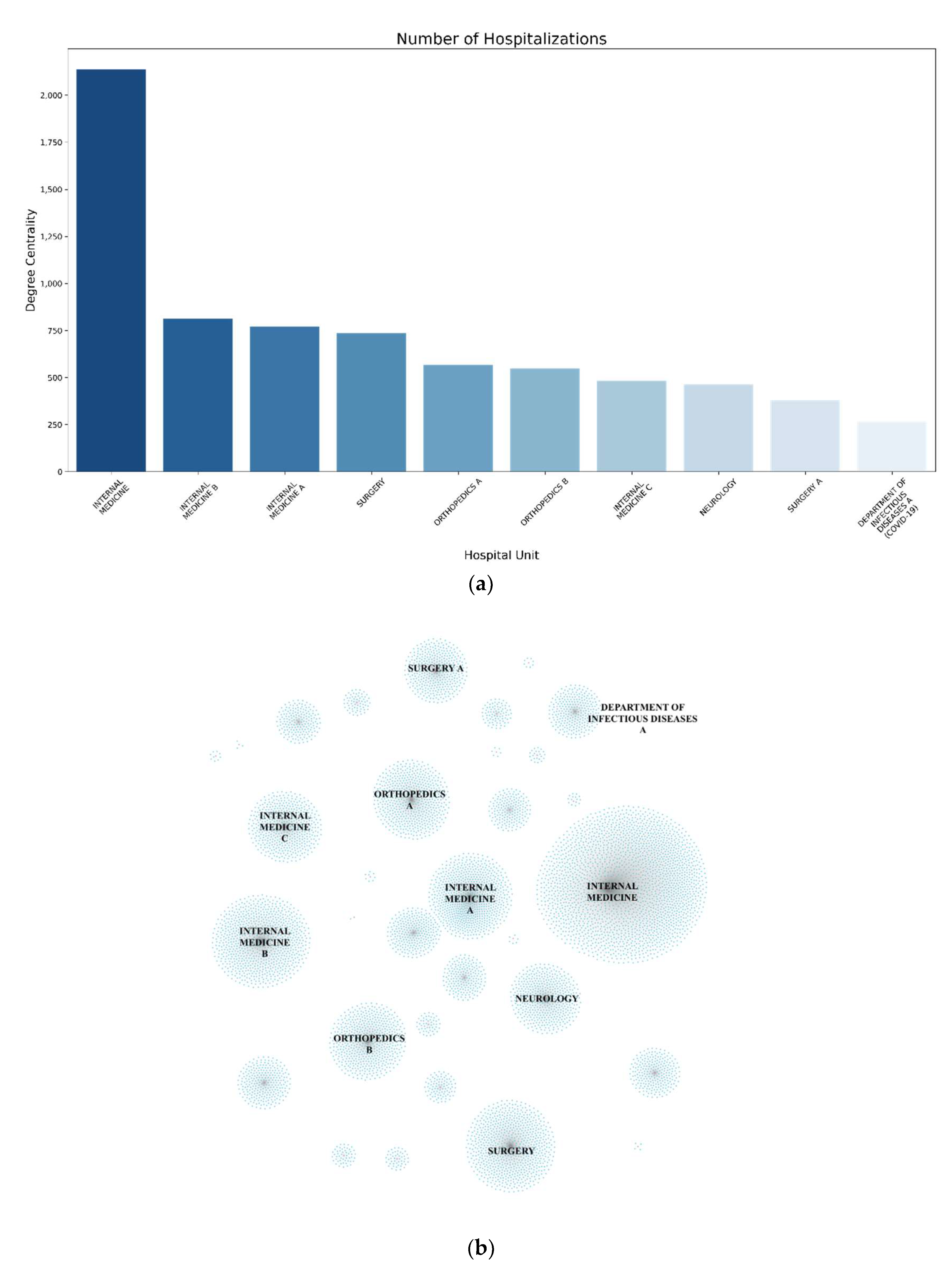
2.2.1. Degree Centrality and Weighted Degree Centrality
2.2.2. Path Analysis
2.3. Approach
Dataset
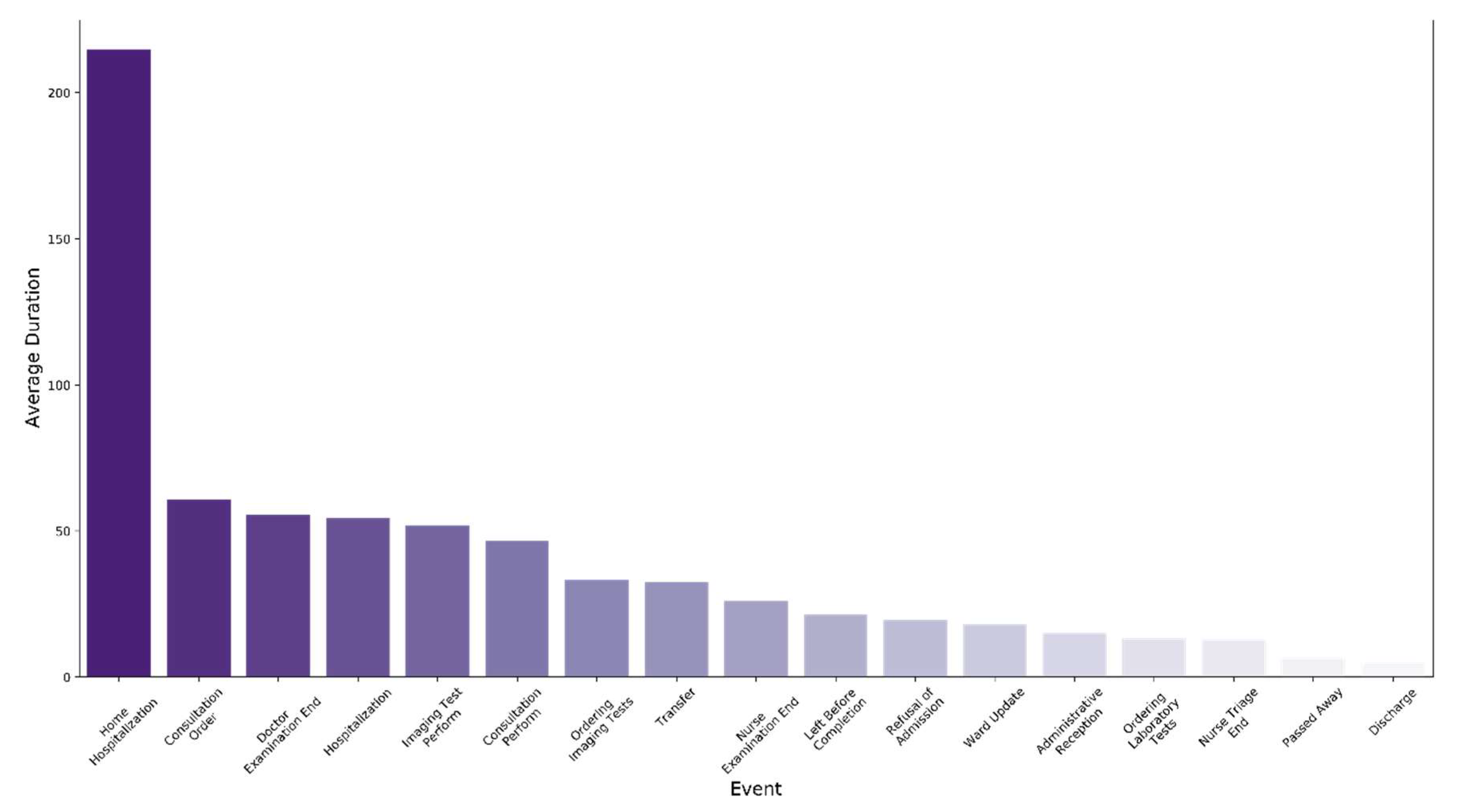
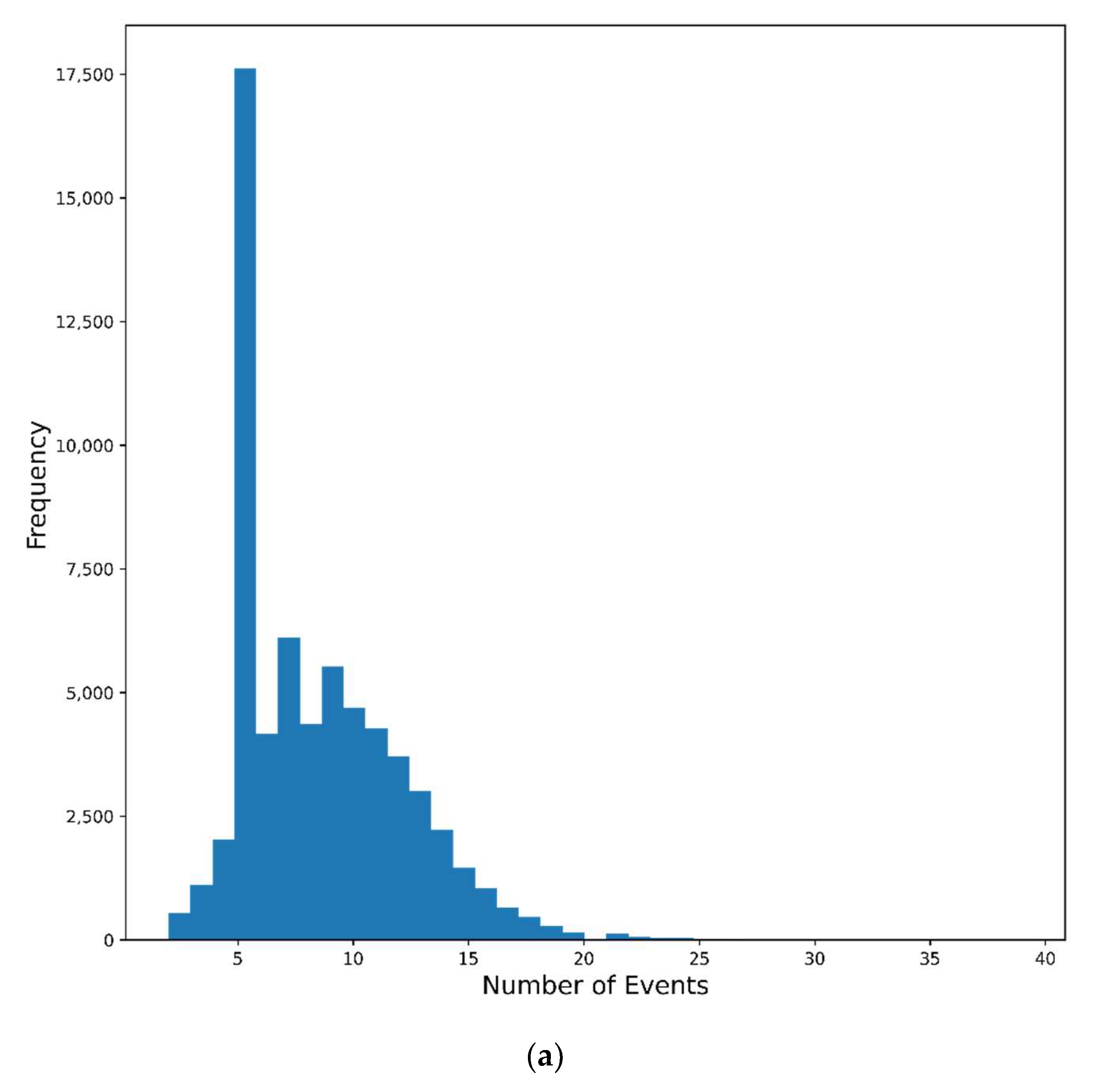
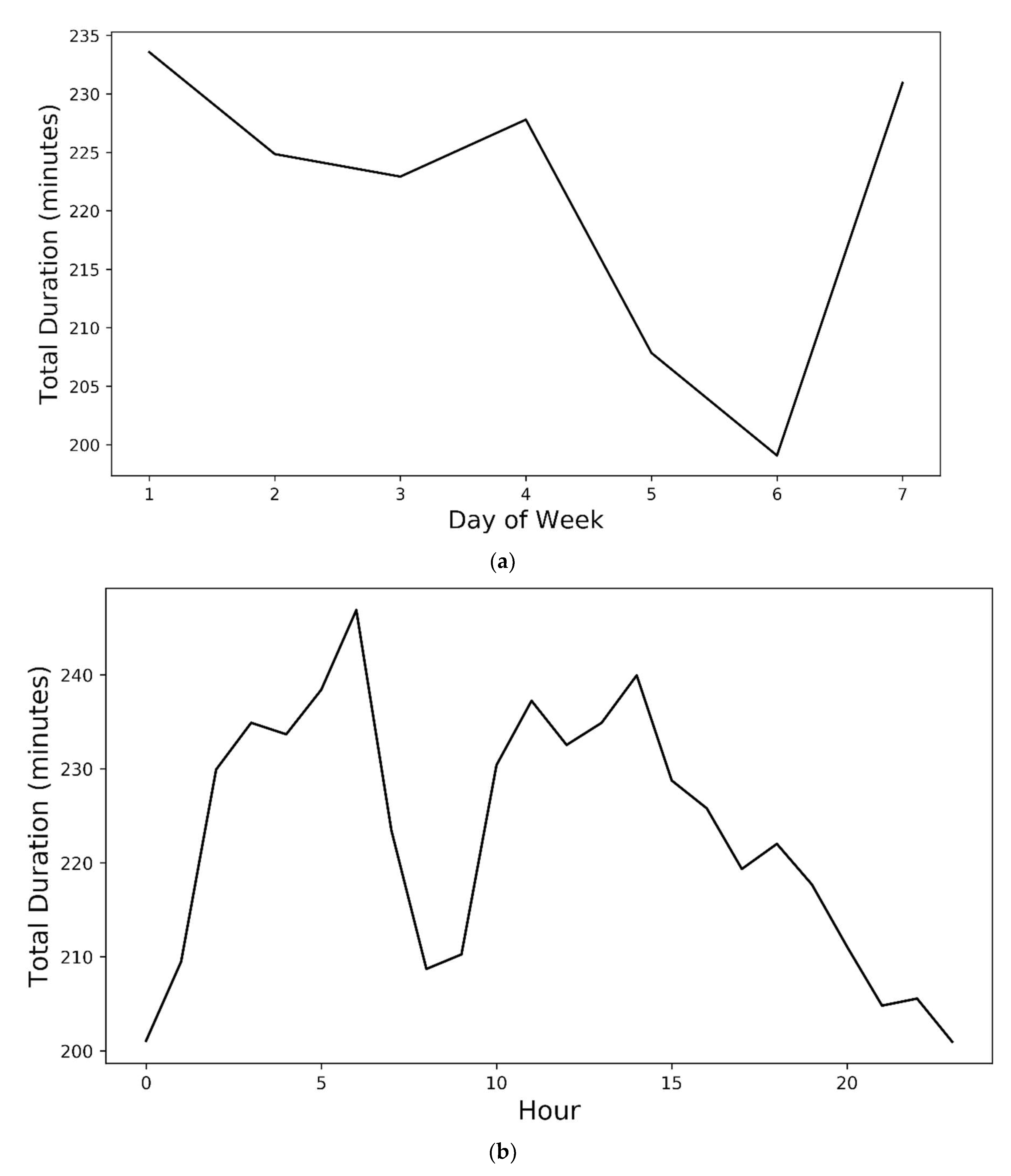
3. Results and Discussion
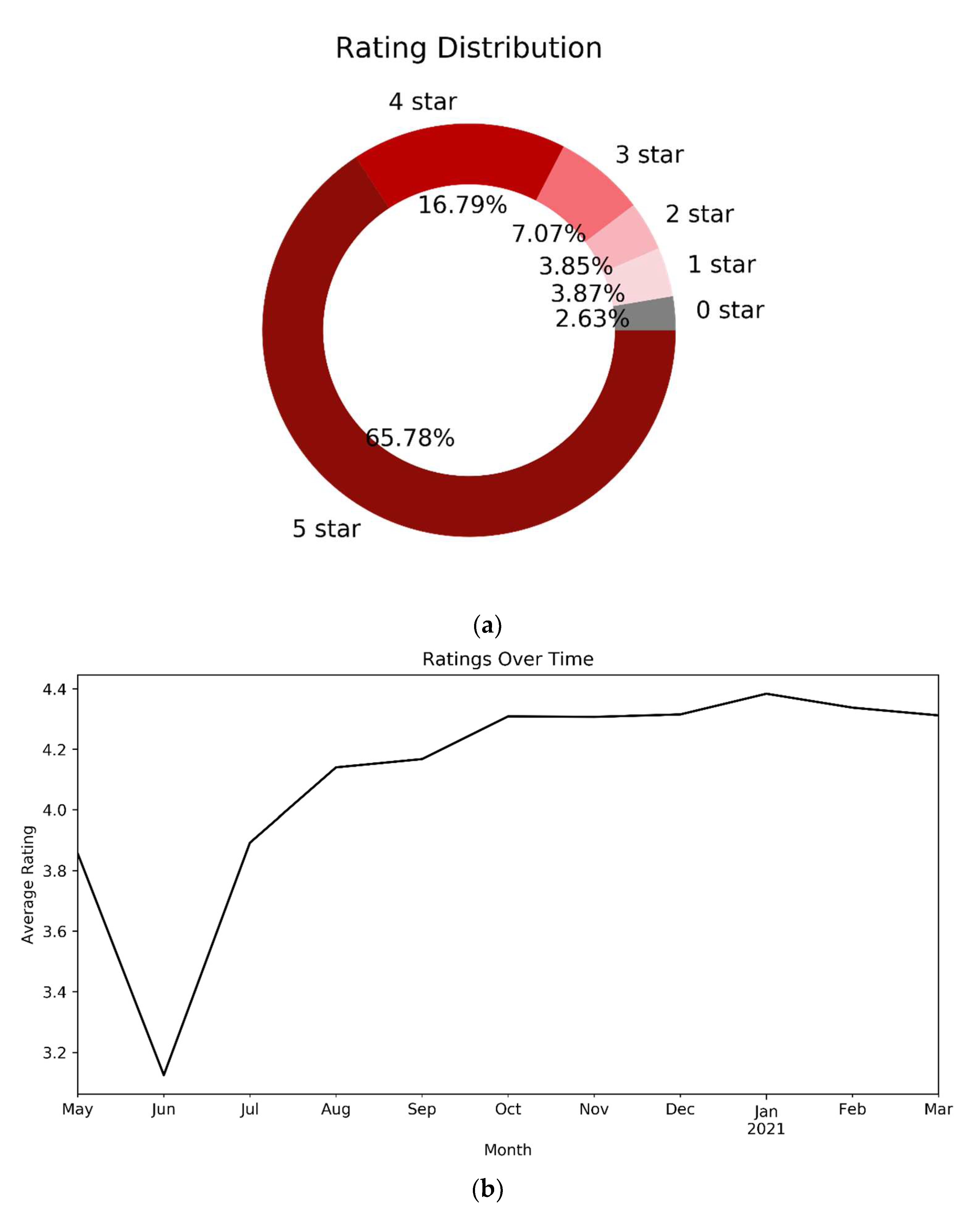
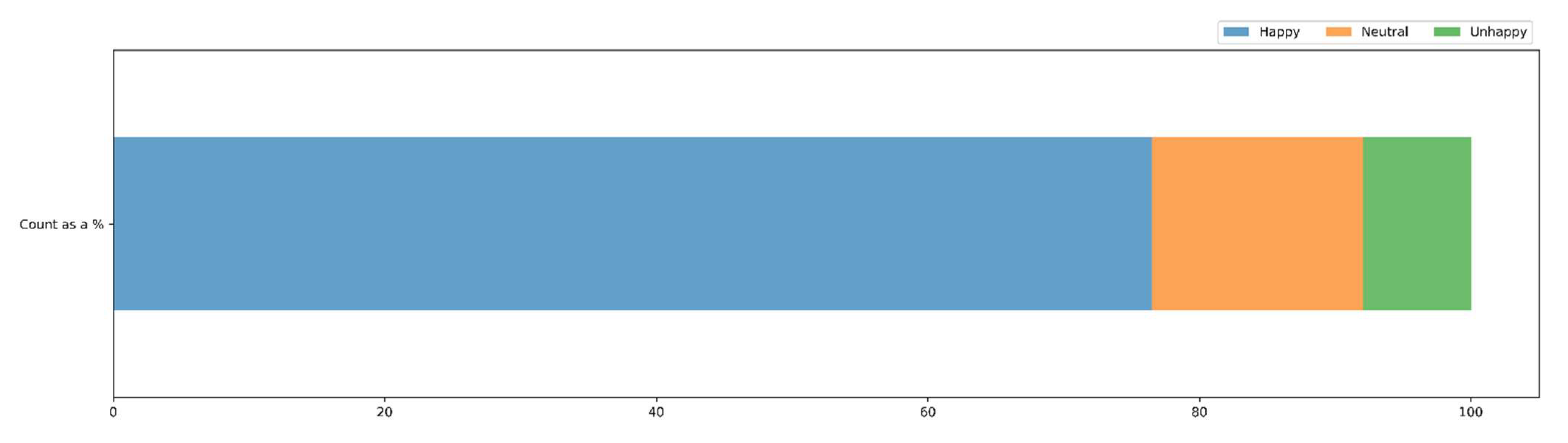
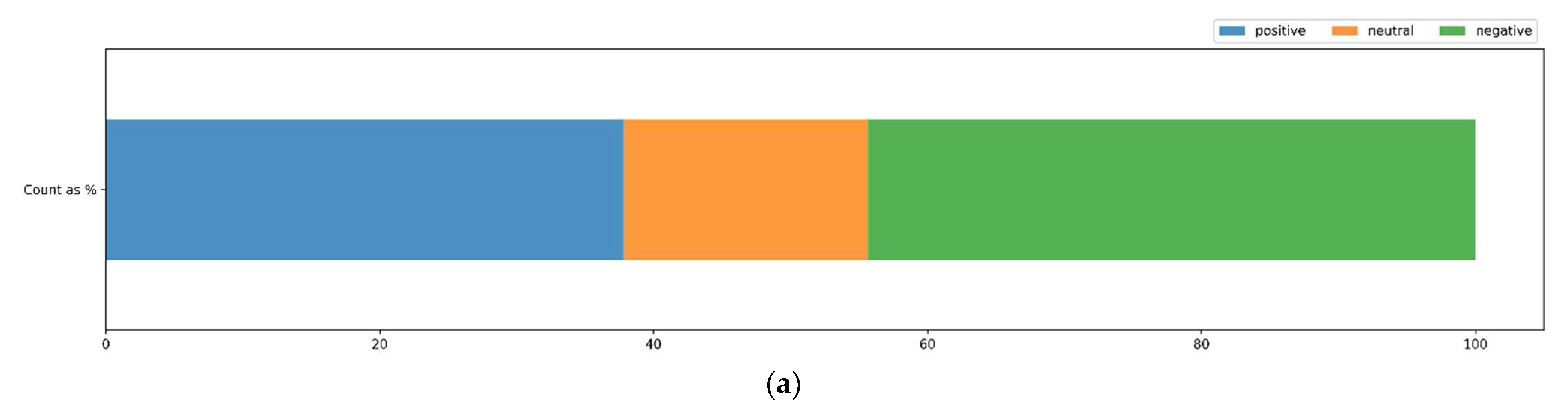
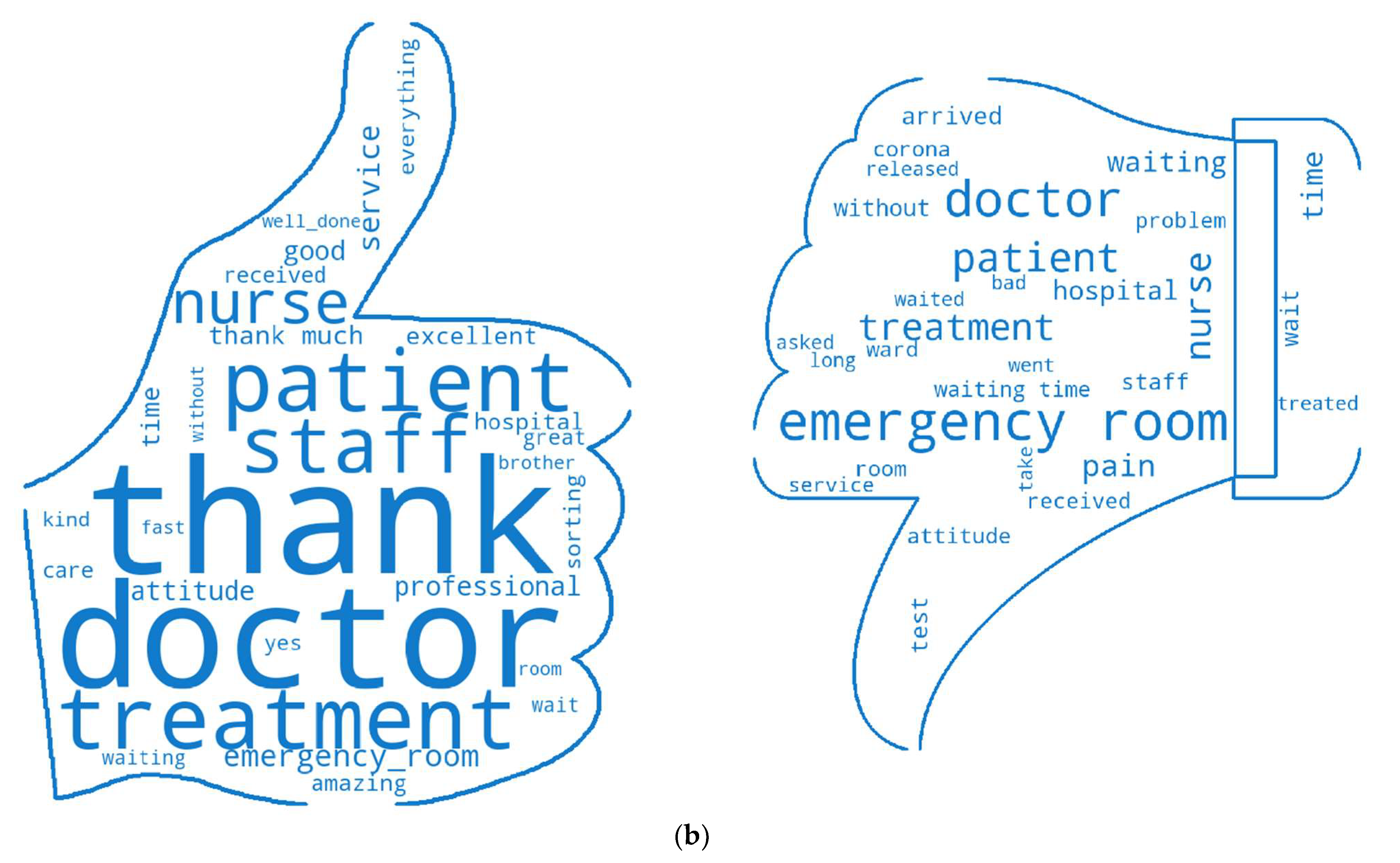
Patients’ Satisfaction Data Analysis
4. Conclusions
4.1. Contributions to Practice
4.2. Limitations
4.3. Medical Ethics
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rathert, C.; Wyrwich, M.D.; Boren, S.A. Patient-Centered Care and Outcomes: A Systematic Review of the Literature. Med. Care Res. Rev. 2013, 70, 351–379. [Google Scholar] [CrossRef] [PubMed]
- Hearld, L.R.; Alexander, J.A. Patient-Centered Care and Emergency Department Utilization: A Path Analysis of the Mediating Effects of Care Coordination and Delays in Care. Med. Care Res. Rev. 2012, 69, 560–580. [Google Scholar] [CrossRef] [PubMed]
- Pham, J.C.; Seth Trueger, N.; Hilton, J.; Khare, R.K.; Smith, J.P.; Bernstein, S.L. Interventions to Improve Patient-Centered Care during Times of Emergency Department Crowding. Acad. Emerg. Med. 2011, 18, 1289–1294. [Google Scholar] [CrossRef] [PubMed]
- Sariyer, G.; Ataman, M.G. The Likelihood of Requiring a Diagnostic Test: Classifying Emergency Department Patients with Logistic Regression. Health Inf. Manag. J. 2022, 51, 13–22. [Google Scholar] [CrossRef]
- Huang, Q.; Zhao, C.; Zhang, X.; Wang, X.; Yi, D. Centrality Measures in Temporal Networks with Time Series Analysis. EPL Europhys. Lett. 2017, 118, 36001. [Google Scholar] [CrossRef]
- Khurana, U. An Introduction to Temporal Graph Data Management. Ph.D. Thesis, Computer Science Department, University of Maryland, College Park, MD, USA, 2012. Available online: https//www.cs.umd.edu/sites/default/files/scholarly_papers/Khurana_SchPaper_1.pdf (accessed on 20 April 2022).
- Tong, H.; Papadimitriou, S.; Philip, S.Y.; Faloutsos, C. Proximity Tracking on Dynamic Bipartite Graphs: Problem Definitions and Fast Solutions. In Link Mining: Models, Algorithms, and Applications; Springer: Berlin/Heidelberg, Germany, 2010; pp. 211–236. [Google Scholar]
- Rossi, R.A.; Gallagher, B.; Neville, J.; Henderson, K. Modeling Dynamic Behavior in Large Evolving Graphs. In Proceedings of the Sixth ACM International Conference on Web Search and Data Mining, Rome, Italy, 4–8 February 2013; pp. 667–676. [Google Scholar]
- Yang, Y.; Yu, J.X.; Gao, H.; Pei, J.; Li, J. Mining Most Frequently Changing Component in Evolving Graphs. World Wide Web 2014, 17, 351–376. [Google Scholar] [CrossRef]
- Yang, J.; Leskovec, J. Patterns of Temporal Variation in Online Media. In Proceedings of the Fourth ACM International Conference on Web Search and Data Mining, Hong Kong, China, 9–12 February 2011; pp. 177–186. [Google Scholar]
- Pereira, F.S.F.; de Amo, S.; Gama, J. Evolving Centralities in Temporal Graphs: A Twitter Network Analysis. In Proceedings of the 2016 17th IEEE International Conference on Mobile Data Management (MDM), Porto, Portugal, 13–16 June 2016; Volume 2, pp. 43–48. [Google Scholar]
- Aridhi, S.; Montresor, A.; Velegrakis, Y. BLADYG: A Graph Processing Framework for Large Dynamic Graphs. Big Data Res. 2017, 9, 9–17. [Google Scholar] [CrossRef] [Green Version]
- Koloniari, G.; Pitoura, E. Partial View Selection for Evolving Social Graphs. In Proceedings of the First International Workshop on Graph Data Management Experiences and Systems, New York, NY, USA, 23 June 2013; pp. 1–6. [Google Scholar]
- Jalili, M.; Salehzadeh-Yazdi, A.; Gupta, S.; Wolkenhauer, O.; Yaghmaie, M.; Resendis-Antonio, O.; Alimoghaddam, K. Evolution of Centrality Measurements for the Detection of Essential Proteins in Biological Networks. Front. Physiol. 2016, 7, 375. [Google Scholar] [CrossRef] [Green Version]
- Leventhal, G.E.; Hill, A.L.; Nowak, M.A.; Bonhoeffer, S. Evolution and Emergence of Infectious Diseases in Theoretical and Real-World Networks. Nat. Commun. 2015, 6, 6101. [Google Scholar] [CrossRef] [Green Version]
- Magnien, C.; Tarissan, F. Time Evolution of the Importance of Nodes in Dynamic Networks. In Proceedings of the 2015 IEEE/ACM International Conference on Advances in Social Networks Analysis and Mining (ASONAM), Paris, France, 25–28 August 2015; pp. 1200–1207. [Google Scholar]
- Starnini, M.; Machens, A.; Cattuto, C.; Barrat, A.; Pastor-Satorras, R. Immunization Strategies for Epidemic Processes in Time-Varying Contact Networks. J. Theor. Biol. 2013, 337, 89–100. [Google Scholar] [CrossRef] [Green Version]
- Karimi, F.; Matous, P. Mapping Diversity and Inclusion in Student Societies: A Social Network Perspective. Comput. Human Behav. 2018, 88, 184–194. [Google Scholar] [CrossRef]
- Blondel, V.D.; Guillaume, J.-L.; Lambiotte, R.; Lefebvre, E. Fast Unfolding of Communities in Large Networks. J. Stat. Mech. Theory Exp. 2008, 2008, P10008. [Google Scholar] [CrossRef] [Green Version]
- Yarlagadda, R.; Pinnaka, S.; Etinkaya, E.K.Ç. A Time-Evolving Weighted-Graph Analysis of Global Petroleum Exchange. In Proceedings of the 2015 7th International Workshop on Reliable Networks Design and Modeling (RNDM), Munich, Germany, 5–7 October 2015; pp. 266–273. [Google Scholar]
- Von Landesberger, T.; Brodkorb, F.; Roskosch, P.; Andrienko, N.; Andrienko, G.; Kerren, A. Mobilitygraphs: Visual Analysis of Mass Mobility Dynamics via Spatio-Temporal Graphs and Clustering. IEEE Trans. Vis. Comput. Graph. 2015, 22, 11–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qi, X.; Liu, L.; Cai, G.; Xie, M. A Topology Evolution Model Based on Revised PageRank Algorithm and Node Importance for Wireless Sensor Networks. Math. Probl. Eng. 2015, 2015, 165136. [Google Scholar] [CrossRef] [Green Version]
- Glacet, C.; Fiore, M.; Gramaglia, M. Temporal Connectivity of Vehicular Networks: The Power of Store-Carry-and-Forward. In Proceedings of the 2015 IEEE Vehicular Networking Conference (VNC), Kyoto, Japan, 16–18 December 2015; pp. 52–59. [Google Scholar]
- Küçükkeçeci, C.; Yazici, A. Big Data Model Simulation on a Graph Database for Surveillance in Wireless Multimedia Sensor Networks. Big Data Res. 2018, 11, 33–43. [Google Scholar] [CrossRef] [Green Version]
- Liao, C.-H.; Chen, M.-Y. Building Social Computing System in Big Data: From the Perspective of Social Network Analysis. Comput. Hum. Behav. 2019, 101, 457–465. [Google Scholar] [CrossRef]
- Brunson, J.C.; Laubenbacher, R.C. Applications of Network Analysis to Routinely Collected Health Care Data: A Systematic Review. J. Am. Med. Inform. Assoc. 2018, 25, 210–221. [Google Scholar] [CrossRef]
- McHaney-Lindstrom, M.; Hebert, C.; Flaherty, J.; Mangino, J.E.; Moffatt-Bruce, S.; Root, E.D. Analysis of Intra-Hospital Transfers and Hospital Onset Clostridium Difficile Infection. J. Hosp. Infect. 2019, 102, 168–169. [Google Scholar] [CrossRef]
- Kohler, K.; Ercole, A. Characterising Complex Healthcare Systems Using Network Science: The Small World of Emergency Surgery. arXiv 2019, arXiv:1908.01688. [Google Scholar]
- Kohler, K.; Ercole, A. Can Network Science Reveal Structure in a Complex Healthcare System? A Network Analysis Using Data from Emergency Surgical Services. BMJ Open 2020, 10, e034265. [Google Scholar] [CrossRef] [Green Version]
- McHaney-Lindstrom, M.; Hebert, C.; Miller, H.; Moffatt-Bruce, S.; Root, E. Network Analysis of Intra-Hospital Transfers and Hospital Onset Clostridium Difficile Infection. Health Inf. Libr. J. 2020, 37, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Eken, T.; Jørgensen, S.B.; Thoresen, M.; Søvik, S. Effects of Patient-Level Risk Factors, Departmental Allocation and Seasonality on Intrahospital Patient Transfer Patterns: Network Analysis Applied on a Norwegian Single-Centre Data Set. BMJ Open 2022, 12, e054545. [Google Scholar] [CrossRef] [PubMed]
- Bean, D.M.; Stringer, C.; Beeknoo, N.; Teo, J.; Dobson, R.J.B. Network Analysis of Patient Flow in Two UK Acute Care Hospitals Identifies Key Sub-Networks for A&E Performance. PLoS ONE 2017, 12, e0185912. [Google Scholar]
- Lim, M.E.; Nye, T.; Bowen, J.M.; Hurley, J.; Goeree, R.; Tarride, J.-E. Mathematical Modeling: The Case of Emergency Department Waiting Times. Int. J. Technol. Assess. Health Care 2012, 28, 93–109. [Google Scholar] [CrossRef]
- Wiler, J.L.; Bolandifar, E.; Griffey, R.T.; Poirier, R.F.; Olsen, T. An Emergency Department Patient Flow Model Based on Queueing Theory Principles. Acad. Emerg. Med. 2013, 20, 939–946. [Google Scholar] [CrossRef]
- Maduako, I.; Wachowicz, M.; Hanson, T. STVG: An Evolutionary Graph Framework for Analyzing Fast-Evolving Networks. J. Big Data 2019, 6, 55. [Google Scholar] [CrossRef]
- Li, L.; Wang, P.; Yan, J.; Wang, Y.; Li, S.; Jiang, J.; Sun, Z.; Tang, B.; Chang, T.-H.; Wang, S.; et al. Real-World Data Medical Knowledge Graph: Construction and Applications. Artif. Intell. Med. 2020, 103, 101817. [Google Scholar] [CrossRef]
- Barnett, G.O.; Cimino, J.J.; Hupp, J.A.; Hoffer, E.P. DXplain: An Evolving Diagnostic Decision-Support System. JAMA 1987, 258, 67–74. [Google Scholar] [CrossRef]
- Bisson, L.J.; Komm, J.T.; Bernas, G.A.; Fineberg, M.S.; Marzo, J.M.; Rauh, M.A.; Smolinski, R.J.; Wind, W.M. Accuracy of a Computer-Based Diagnostic Program for Ambulatory Patients with Knee Pain. Am. J. Sports Med. 2014, 42, 2371–2376. [Google Scholar] [CrossRef]
- Miller, R.A. Medical Diagnostic Decision Support Systems—Past, Present, and Future: A Threaded Bibliography and Brief Commentary. J. Am. Med. Inform. Assoc. 1994, 1, 8–27. [Google Scholar] [CrossRef] [Green Version]
- Wang, M.; Liu, M.; Liu, J.; Wang, S.; Long, G.; Qian, B. Safe Medicine Recommendation via Medical Knowledge Graph Embedding. arXiv 2017, arXiv:1710.05980. [Google Scholar]
- Gann, B. Giving Patients Choice and Control: Health Informatics on the Patient Journey. Yearb. Med. Inform. 2012, 21, 70–73. [Google Scholar] [CrossRef] [Green Version]
- Tang, H.; Ng, J.H.K. Googling for a Diagnosis—Use of Google as a Diagnostic Aid: Internet Based Study. BMJ 2006, 333, 1143–1145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robinson, I.; Webber, J.; Eifrem, E. Graph Databases: New Opportunities for Connected Data; O’Reilly Media, Inc.: Newton, MA, USA, 2013. [Google Scholar]
- Kaur, K.; Rani, R. Modeling and Querying Data in NoSQL Databases. In Proceedings of the 2013 IEEE International Conference on Big Data, Silicon Valley, CA, USA, 6–9 October 2013; pp. 1–7. [Google Scholar]
- Maduako, I.; Cavalheri, E.; Wachowicz, M. Exploring the Use of Time-Varying Graphs for Modelling Transit Networks. arXiv 2018, arXiv:1803.07610. [Google Scholar]
- Ajami, S.; Ketabi, S.; Yarmohammadian, M.H.; Bagherian, H. Waiting Time in Emergency Department by Simulation. In Proceedings of the ITCH, Victoria, BC, Canada, 24–27 February 2011; pp. 196–200. [Google Scholar]
- Brysiewicz, P.; Emmamally, W. Focusing on Families in the Emergency Department. Int. Emerg. Nurs. 2017, 100, 1–2. [Google Scholar] [CrossRef]
- Cypress, B.S. The Emergency Department: Experiences of Patients, Families, and Their Nurses. Adv. Emerg. Nurs. J. 2014, 36, 164–176. [Google Scholar] [CrossRef]
- Kash, B.; McKahan, M. The Evolution of Measuring Patient Satisfaction. J. Prim. Health Care Gen. Pract. 2017, 4, 2. [Google Scholar]
- Iwanowski, P.; Budaj, A.; Członkowska, A.; Wasek, W.; Kozłowska-Boszko, B.; Olekedzka, U.; Masełbas, W. Informed Consent for Clinical Trials in Acute Coronary Syndromes and Stroke Following the European Clinical Trials Directive: Investigators’ Experiences and Attitudes. Trials 2008, 9, 45. [Google Scholar] [CrossRef] [Green Version]
- Wilets, I.; O’Rourke, M.; Nassisi, D. How Patients and Visitors to an Urban Emergency Department View Clinical Research. Acad. Emerg. Med. 2003, 10, 1081–1085. [Google Scholar] [CrossRef]
- Flynn, D.; Knoedler, M.A.; Hess, E.P.; Murad, M.H.; Erwin, P.J.; Montori, V.M.; Thomson, R.G. Engaging Patients in Health Care Decisions in the Emergency Department through Shared Decision-Making: A Systematic Review. Acad. Emerg. Med. 2012, 19, 959–967. [Google Scholar] [CrossRef]
- Edwards, B.; Hofmeyr, S.; Stelle, G.; Forrest, S. Internet Topology over Time. arXiv 2012, arXiv:1202.3993. [Google Scholar]
- Borg, A.; Boldt, M. Using VADER Sentiment and SVM for Predicting Customer Response Sentiment. Expert Syst. Appl. 2020, 162, 113746. [Google Scholar] [CrossRef]



| EVENT_TYPE_DESC | Count |
|---|---|
| Administrative Reception | 63,895 |
| Consultation Order | 22,742 |
| Consultation Perform | 22,748 |
| Discharge | 43,429 |
| Doctor Examination End | 62,234 |
| Home Hospitalization | 2 |
| Hospitalization | 18,770 |
| Imaging Test Perform | 17,870 |
| Left Before Completion | 928 |
| Nurse Examination End | 71,034 |
| Nurse Triage End | 63,688 |
| Ordering Imaging Tests | 20,967 |
| Ordering Laboratory Tests | 117,546 |
| Passed Away | 102 |
| Refusal of Admission | 1367 |
| Transfer | 601 |
| Ward Update | 8970 |
| Total | 536,893 |
| Case Number | Event Count | Total Duration | Hour | Day of Week | Path Sequence | |
|---|---|---|---|---|---|---|
| 1 | 11066765 | 5 | 177.4 | 15 | 4 | [Administrative Reception, Nurse Triage End, Nurse Examination End, Doctor Examination End, Discharge] |
| 2 | 11066794 | 6 | 297.0 | 17 | 4 | [Administrative Reception, Nurse Triage End, Doctor Examination End, Nurse Examination End, Hospitalization, Ward Update] |
| 3 | 11066740 | 6 | 83.0 | 17 | 4 | [Doctor Examination End, Consultation Perform, Consultation Order, Consultation Order, Consultation Perform, Discharge] |
| 4 | 11066789 | 8 | 279.0 | 17 | 4 | [Administrative Reception, Nurse Triage End, Nurse Examination End, Doctor Examination End, Hospitalization, Consultation Order, Consultation Perform, Hospitalization] |
| 5 | 11066775 | 4 | 0.05 | 17 | 4 | [Nurse Triage End, Nurse Examination End, Doctor Examination End, Discharge] |
| 6 | 11066791 | 5 | 31.0 | 17 | 4 | [Administrative Reception, Nurse Triage End, Nurse Examination End, Doctor Examination End, Discharge] |
| 7 | 11066733 | 2 | 89.0 | 17 | 4 | [Consultation Perform, Discharge] |
| 8 | 11066773 | 5 | 277.0 | 17 | 4 | [Nurse Triage End, Nurse Examination End, Doctor Examination End, Consultation Order, Discharge] |
| 9 | 11066792 | 7 | 93.0 | 17 | 4 | [Administrative Reception, Nurse Triage End, Nurse Examination End, Consultation Order, Doctor Examination End, Consultation Perform, Discharge] |
| 10 | 11066730 | 2 | 29.0 | 17 | 4 | [Doctor Examination End, Discharge] |
| Path | Freq. | |
|---|---|---|
| 1 | [Administrative Reception, Nurse Triage End, Nurse Examination End, Doctor Examination End, Discharge] | 13,487 |
| 2 | [Administrative Reception, Nurse Triage End, Nurse Examination End, Ordering Laboratory Tests, Ordering Laboratory Tests, Ordering Laboratory Tests, Ordering Laboratory Tests, Doctor Examination End, Discharge] | 960 |
| 3 | [Administrative Reception, Nurse Triage End, Nurse Examination End, Doctor Examination End, Hospitalization] | 939 |
| 4 | [Administrative Reception, Nurse Triage End, Nurse Examination End, Doctor Examination End, Consultation Order, Consultation Perform, Discharge] | 904 |
| 5 | [Administrative Reception, Nurse Triage End, Nurse Examination End, Doctor Examination End, Ordering Imaging Tests, Imaging Test Perform, Discharge] | 870 |
| 6 | [Administrative Reception, Nurse Triage End, Nurse Examination End, Doctor Examination End, Hospitalization, Ward Update] | 858 |
| 7 | [Administrative Reception, Nurse Triage End, Nurse Examination End, Ordering Laboratory Tests, Ordering Laboratory Tests, Ordering Laboratory Tests, Ordering Laboratory Tests, Ordering Laboratory Tests, Doctor Examination End, Discharge] | 822 |
| 8 | [Administrative Reception, Nurse Triage End, Nurse Examination End, Ordering Laboratory Tests, Ordering Laboratory Tests, Ordering Laboratory Tests, Doctor Examination End, Discharge] | 814 |
| 9 | [Administrative Reception, Nurse Triage End, Doctor Examination End, Discharge] | 800 |
| 10 | [Administrative Reception, Nurse Examination End, Nurse Triage End, Doctor Examination End, Discharge] | 648 |
| Three-Consecutive-Event Sequences | Frequency | |
|---|---|---|
| Before Hospitalization | [“Nurse Triage End”, “Nurse Examination End”, “Doctor Examination End”] | 2788 |
| [“Ordering Laboratory Tests”, “Ordering Laboratory Tests”, “Doctor Examination End”] | 1643 | |
| [“Ordering Laboratory Tests”, “Ordering Laboratory Tests”, “Ordering Laboratory Tests”] | 1313 | |
| [“Doctor Examination End”, “Consultation Order”, “Consultation Perform”] | 879 | |
| [“Doctor Examination End”, “Ordering Imaging Tests”, “Imaging Test Perform”] | 619 | |
| After Hospitalization | [“Ordering Laboratory Tests”, “Ordering Laboratory Tests”, “Ordering Laboratory Tests”] | 790 |
| [“Nurse Examination End”, “Ordering Laboratory Tests”, “Ordering Laboratory Tests”] | 104 | |
| [“Ordering Laboratory Tests”, “Ordering Laboratory Tests”, “Ward Update”] | 74 | |
| [“Consultation Order”, “Consultation Perform”, “Ward Update”] | 46 | |
| [“Ordering Laboratory Tests”, “Ward Update”, “Consultation Perform”] | 45 |
| Event before Consultation Order | Frequency |
|---|---|
| “Doctor Examination End” | 8760 |
| “Nurse Examination End” | 3366 |
| “Consultation Order” | 2534 |
| “Ordering Laboratory Tests” | 2232 |
| “Ordering Imaging Tests” | 1428 |
| Event after Consultation Perform | Frequency |
| “Discharge” | 7931 |
| “Hospitalization” | 3455 |
| “Doctor Examination End” | 2382 |
| “Consultation Perform” | 2061 |
| “Consultation Order” | 1325 |
| Top 15 Positive | Top 15 Negative | |||
|---|---|---|---|---|
| Word | Frequency | Word | Frequency | |
| 1 | doctor | 425 | room | 563 |
| 2 | thank | 366 | emergency | 511 |
| 3 | treatment | 309 | doctor | 449 |
| 4 | patient | 285 | time | 293 |
| 5 | nurse | 282 | patient | 277 |
| 6 | staff | 271 | treatment | 240 |
| 7 | everything | 253 | nurse | 209 |
| 8 | service | 245 | waiting | 194 |
| 9 | time | 226 | pain | 182 |
| 10 | emergency room | 206 | long | 152 |
| 11 | excellent | 205 | test | 140 |
| 12 | good | 201 | wait | 119 |
| 13 | attitude | 194 | hospital | 114 |
| 14 | thanks | 181 | arrived | 109 |
| 15 | professional | 181 | without | 107 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reychav, I.; McHaney, R.; Babbar, S.; Weragalaarachchi, K.; Azaizah, N.; Nevet, A. Graph Network Techniques to Model and Analyze Emergency Department Patient Flow. Mathematics 2022, 10, 1526. https://doi.org/10.3390/math10091526
Reychav I, McHaney R, Babbar S, Weragalaarachchi K, Azaizah N, Nevet A. Graph Network Techniques to Model and Analyze Emergency Department Patient Flow. Mathematics. 2022; 10(9):1526. https://doi.org/10.3390/math10091526
Chicago/Turabian StyleReychav, Iris, Roger McHaney, Sunil Babbar, Krishanthi Weragalaarachchi, Nadeem Azaizah, and Alon Nevet. 2022. "Graph Network Techniques to Model and Analyze Emergency Department Patient Flow" Mathematics 10, no. 9: 1526. https://doi.org/10.3390/math10091526
APA StyleReychav, I., McHaney, R., Babbar, S., Weragalaarachchi, K., Azaizah, N., & Nevet, A. (2022). Graph Network Techniques to Model and Analyze Emergency Department Patient Flow. Mathematics, 10(9), 1526. https://doi.org/10.3390/math10091526







