Abstract
Adult health behavior is established and formed in childhood, in which, besides the primacy of the family, institutional education plays a significant role. The aim of our systematic review is to analyze health interventions implemented in an institutional environment for children aged 3–6 years. Our research was carried out according to the PRISMA 2020 protocol. The sample of research was determined by using the keywords “health education” or “health promotion” and “preschool” or “kindergarten” in Scopus, ERIC and WOS databases published between 2013 and 2022. Out of a total of 1535 results, 14 proved to be relevant to the eligibility criteria of the study topic. Cochrane Risk of Bias criteria were used for critical appraisal and to limit bias. The majority of the analyzed studies focused on physical activity and nutrition, including the issues of sedentary time, obesity and sustainability. The holistic approach is less typical in the interventions reviewed, with a marginal occurrence of topics related to mental and social health, as well as risk behavior. The interventions proved to be more effective when parents were involved, and the varied, age-appropriate game-based activities also contributed to the formation of health-supporting habits.
1. Introduction
As a result of advancements in medical and health sciences, life expectancy at birth has increased significantly over the last 100 years; this trend, although at a slower pace, continues even today [1,2]. The economic boom following the Second World War contributed to the more favorable living conditions of the population (nutrition, hygienic conditions, recreational opportunities) and to a change in lifestyle and related needs. Parallel to the increase in life expectancy, there is also a growth in the number of years spent in good health; however, due to the risk behaviors present in health behavior, the degree of health loss is still considerable [1]. The rate of chronic diseases associated with dietary risks, smoking, high systolic blood pressure, overweight and obesity is particularly high in the more economically advantaged regions of the world [3].
In addition to risk behaviors in health, human-caused damage, the dangerous levels of pollution of water, air, soil and wildlife; the considerable and undesired disruption of the biosphere’s ecological balance; and the use and exploitation of natural resources also have a negative effect on people’s physical, mental and social health, which was already highlighted at the 1972 UN conference on the human environment [4]. Reducing severe and irreversible damage to the environment and increasing the chances of future generations to meet their own needs have given rise to the idea of sustainable development with a special emphasis on comprehensive health promotion [5]. Nowadays, sustainable health is a major challenge [6]. Growing social expectations, stressful lifestyles and an increasing media use have a negative effect on the lifestyle and health behavior (consumption, time spent in front of a screen) of the adult and child population. This contributes to the exploitation of the body and soul and also leads to a significant increase in mental illnesses, to the extent that psychological disorders represent the most urgent public health issue in Europe; furthermore, globally, one in every eight people is affected by some form of mental disorder [7,8].
1.1. Health Education in Early Childhood
Adult health behavior is established and formed in childhood, in which, besides the primacy of the family, institutional education plays a significant role. During this process, in addition to education surrounding healthy lifestyles, the teacher influences the child’s outlook, value system and behavior by setting an example and conveying values, thus contributing to the child’s development into a healthier adult. This is particularly applicable for preschool education, which has been shown by several studies [9,10,11] to have a greater impact on the development of individuals’ life paths than later stages of public education; furthermore, it is a long-established fact that health-related habits can be formed at a young age before the child realizes their effects on his/her health and quality of life [12,13,14]. Among the values and habits conveyed by early childhood educators, from the point of view of developing a healthy lifestyle, it is extremely important how health as a value and also health-supporting values appear in their behavior and communication.
The institutional education of children aged 3–7 is extremely heterogenous in international comparison. In most countries, only the preschool year is compulsory, while in the preceding years, children’s participation in institutional education depends on the parents’ needs and/or financial means. The names of the institutions dealing with preschool children also display a high degree of diversity (preschool, kindergarten, child care, nursery school, etc.). Furthermore, Royer & Moreau (2015) and Manning et al. (2017) emphasize that the qualifications and titles of professionals working with children are diverse as well (preschool teacher, kindergarten teacher, caregiver, early childhood teacher/educator, day care teacher, child care provider, etc.) [15,16]. These differences can even occur within a single country. Due to the institutional differences, the function of early childhood education also receives a different emphasis: in many cases, the primary function is care, while in others socialization and skills development come to the fore as well. As a result this, institutional health education and related regulations and guidelines vary widely from country to country.
The WHO (2021) standards for early childhood health education focus mainly on nutrition, physical activity, screen time and rest, and place great emphasis on the collaboration between parents and institutions [17]. In several countries, there are no consistent health education regulations; instead, recommendations or guidelines are formulated. In New Zealand, the guidelines developed relate mainly to institutional infrastructure and somatic health [18], while in Australia, besides nutrition, physical activity and hygiene habits, the health education of children living in families with aboriginal and/or disadvantaged socio-cultural backgrounds are given a prominent role [19]. Indian guidelines emphasize a safe institutional environment, in addition to somatic health [20]. In Lithuania, kindergartens develop their health education program based on regulatory documents [21]. In Hungary, the central regulatory document for kindergarten education emphasizes and holistically explains the formation of a healthy lifestyle as the first task of preschool education, on the basis of which every Hungarian kindergarten has to develop a health education program [22]. In Austria and Germany, standards are primarily available for public catering in kindergartens [23,24]. In the United States, national health education standards have been assigned indicators which expand by age, focusing on children’s health and the habits that support it, to which individual member states adapt, developing their own standards in detail [25].
This shows that early childhood health education efforts are a priority even in countries where participation in preschool education is not compulsory. In many countries, health education in early childhood education is implemented in a complex way, immanently embedded in the educational process [21,26]. Complexity means that during health education the teacher does not focus on just one area, but includes both somatic (physical activity, nutrition, personal, community and environmental hygiene, accident prevention, prevention of other risk behaviors) and mental and social health-related content and activities. The immanent nature of health education suggests that health education efforts are not isolated but are present in a comprehensive way in every educational phase of the pedagogical activity. Health promotion in an institutional setting pays special attention to the prevention of health risks, in addition to the formation of health-related habits.
In Western societies, the most significant threats to children’s health are physical inactivity, dietary risks (unbalanced nutrition) and inappropriate sedentary behavior [27], which can lead to obesity, attention deficit disorder, social relationship disorders and motivation problems, among other things. All of these can fundamentally determine the health status and quality of life in adulthood. For this reason, the development of health-promoting habits in preschool children must be given the greatest attention during health education. The most important areas of habit formation are nutrition, physical activity, rest, sedentary behavior [17], as well as personal, community and environmental hygiene. By using habit-formation tools, the desirable good habit element/routine can be incorporated into everyday life in just a few weeks [28], which is why health education interventions can be effective even in the short term. Recognizing this, several preschool health educational intervention programs have been developed in recent decades, of which the collection of the results can help professionals working in this field to develop effective health education programs.
Due to the complexity of health education and the age characteristics of the age group examined, it is difficult to measure the effectiveness of health education interventions in an institutional environment; therefore, many studies are carried out mainly with the involvement of parents and teachers. So, it is not surprising that in the field of early childhood health education, previous systematic reviews focused primarily on parents or teachers [29,30,31,32], possibly on a specific health education area (oral health, obesity) [33,34,35,36,37,38] or on a specific type of disease [39,40]. A comprehensive review of health interventions for the 3–6-year-old age group within an institutional setting has not been carried out so far.
1.2. Aims
Accordingly, the aim of our systematic review is to analyze health intervention programs implemented in institutional settings for children aged 3–6 years.
The following research questions guided this systematic review according to the PICO (2022) format [41]:
- In which areas of health education has intervention been conducted among 3–6-year-old children?
- How holistic is the approach to health education and health promotion in the applied intervention program?
- In what institutional environment are the intervention programs implemented?
- What kind of methods are used during the intervention programs?
- What are the achieved outcomes of applied interventions related to the health education of 3–6-year-old children? To what extent can these programs be considered effective?
- What are the issues that require further exploration?
Answering these questions can contribute to supporting pedagogical interventions in the field of early childhood health education, broadening the methodological repertoire of teachers and shaping their attitudes.
2. Materials and Methods
Our research was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 protocol [42]. The protocol which outlined the aims and range of this systematic review was registered with PROSPERO (ID: CRD42023433707) [43].
To find the answer to the research questions, a systematic literature review was carried out which collected data from research already existing in this topic. To ensure scientific accuracy, the study obeyed the guidelines suggested by the PRISMA statement. The recommendations of the PRISMA statement ensure clarity and transparency on the rationale for the review, on data selection and the obtained findings to make sure that the same procedure is reliable and consistent [42].
2.1. Eligibility Criteria
Studies were included in the selection process if they complied with the following criteria:
- peer-reviewed empirical studies written in English language;
- studies focused on health education or health promotion aimed at 3–6-year-old children in an institutional environment (kindergarten, preschool or other ECEC institution);
- studies based on intervention with outcomes related to children.
- Studies were excluded from the analysis if the following conditions were present:
- the full text was not available;
- types of papers were any of the following: systematic or other reviews, study protocols, pilot studies, secondary analysis, content or document analysis, policy papers, validation of measuring tools without any results;
- studies aimed at parents or professionals working with children (educators, health care professionals, etc.)
- public health programs and measures or programs implemented in the framework of a long-term international project;
- infrastructural development without pedagogical intervention
- studies related to children with acute or chronic diseases or with special educational needs;
- programs supporting healthy development (e.g., development of cognitive or motor skills).
2.2. Information Sources
The research sample was defined in the Scopus, WOS and ERIC databases using the keywords “health education” or “health promotion” and “preschool” or “kindergarten”. The combination of these words was searched in title, abstract and keywords at the same time. As an additional filter, we limited the field of publications to education, psychology, social sciences and multidisciplinary sciences. Furthermore, we determined that the examined studies should be published between 2013 and 2022.
2.3. Selection Process
In the first phase of the search, the SCOPUS database recorded 987 studies, while WOS identified 360 and ERIC found 184 results. We detected four additional records through other sources. The bibliographic data of the results were imported into a Microsoft Excel spreadsheet.
Out of a total of 1535 results, 161 duplicates were removed. After reviewing the titles and abstracts (K.D., E.S., J.P.) of the remaining 1374 records, we excluded from the analysis those studies which did not meet the selection criteria. Based on the reviewed titles and abstracts, we excluded those published as non-journal studies (n = 4) as well as reviews, study protocols and pilot studies (n = 59). In total, 239 studies did not prove to be relevant in terms of content, another 206 papers were not aimed at children aged 3–6, while 276 studies were primarily aimed at parents and/or professionals working with children. In addition, we excluded studies which focused on children with acute or chronic diseases or atypical development (n = 154) or on public health measures (n = 97). In the case of many studies, the intervention was not carried out (n = 86) or took place in a non-institutional setting (n = 72).
We assessed 181 full articles, (M.C., J.F.), from which we excluded a further 18 content-irrelevant studies, 5 theoretical ones, 4 with a public health approach and 22 age-inappropriate papers. In 41 studies there was no intervention, in 34 cases intervention was aimed at parents or teachers, in another 20 cases no results for children were available, while in 13 papers the intervention was carried out in a non-institutional setting.
Twenty-four of the studies proved to be relevant to the eligibility criteria of the study topic. An additional ten articles were excluded due to specific reasons: three interventions focused exclusively on the development of motor skills and two other studies dealt with the presentation of partial results of large-scale international projects. In the case of five studies, the effects of institutional infrastructure development were examined, but no pedagogical intervention was carried out.
Following the inclusion and exclusion criteria, 14 studies were selected for our systematic review (Figure 1) [44,45,46,47,48,49,50,51,52,53,54,55,56,57]. Disagreements arising during the selection process were justified through discussion with members of the research team.
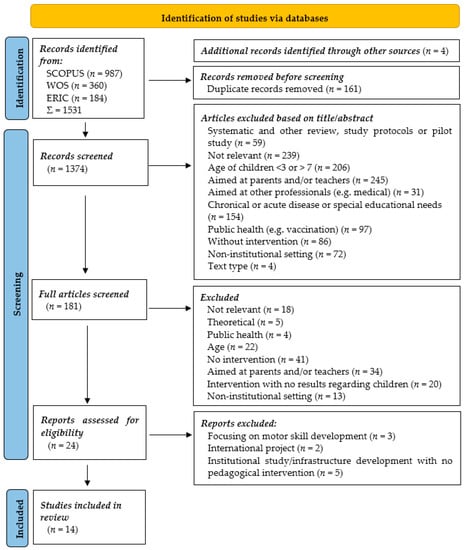
Figure 1.
Flow chart of the searching process according to the PRISMA protocol.
3. Results
3.1. Characteristics of Included Studies
The main characteristics of the selected empirical studies are summarized in Table 1. Ten of the included studies were published in the last five years (2018–2022) [44,45,47,48,49,50,51,53,54,56]. Five of the studies present interventions in Europe [44,46,49,50,52], five in North or South America [45,47,53,55,56], three in Asia [48,51,54] and one in Australia [57]. Between 100 and 500 children took part in half of the studies [44,46,47,50,51,52,54], while in the case of four studies, the number of sample elements was below 100 [45,53,55,57] and three studies had over 500 participants [48,49,56]. With one exception [51], the studies included a heterogenous age group of children in the intervention: four studies focused on children aged 3–4 years [45,49,53,56], three studies on children aged 3–5 years [47,54,57], one study on children aged 3–6 years [44], two studies on children aged 4–5 years [50,52], one study on children aged 4–6 years [46], one study on children aged 5 years [51] and two studies on children aged 5–6 years [48,55].

Table 1.
Selected empirical studies and the health education dimension analyzed.
We have already referred to the international heterogeneity of the institutional environment. Accordingly, four interventions were carried out in preschool [44,48,54,57], two in kindergarten [49,51], two in day care centers [45,56] and six in other ECEC institutional settings [46,47,50,52,53,55].
The duration of the interventions studied also shows a great variety: two interventions were shorter than one month [45,46], three interventions were longer than six months [49,54,56], while nine interventions ranged from 1 to 6 months [44,47,48,50,51,52,53,55,57].
Three interventions focused on nutrition and physical activity [47,56,57] and another three focused exclusively on physical activity [51,52,53] or only nutrition [44,46,55]. In addition to nutrition and physical activity, one study included sustainability [50] and another one on the reduction in screen media use [49]. Three other studies focused on oral health [54], nasal health [45] or the prevention of smoking [48].
3.2. Health Education Fields Examined in the Interventions
Among health education interventions carried out in institutional settings, we did not find any intervention with a complex approach. Some of the interventions aimed at increasing physical activity appeared to be closely connected to nutrition, the prevention of obesity and a reduction in sedentary time.
3.2.1. Physical Activity
Interventions aimed exclusively at an increase in physical activity [51,52,53] mostly increased time spent with vigorous exercise in the short term; however, for shorter-term interventions, the authors [52] highlighted that despite the intensity of the intervention, there was no significant increase in time spent with physical activity and no reduction in sedentary time. Their findings suggest that children who spent more time in preschool proved to be less active, possibly due to a tighter institutional schedule. In their study, Min et al. (2019) proved that physical activity significantly contributes to a psychological need for satisfaction. The intervention they used was introduced in the context of the NASA Mission X program, which is an exercise program consisting of several modules, systematically planned and embedded in a playful frame story, which provided increased internal motivation for kindergarten children during the activities [51].
3.2.2. Nutrition
In the case of three studies [44,46,55], the intervention focused exclusively on demonstrating changes in nutrition-related knowledge and habits, with a main aim of increasing vegetable and/or fruit consumption. The interventions proved to be effective in terms of their results, but, at the same time, the researchers found no spillover effect: the recognition and increased consumption of the fruits and vegetables actually involved in the intervention did not extend to other fruits and vegetables. In the short term, the use of external rewards (through stickers) increased the effectiveness of the intervention [44]. As a result of the interventions, it was also concluded that real results in healthy eating can be achieved through the involvement and commitment of the adults around the children.
3.2.3. Physical Activity and Nutrition
Five studies linked physical activity and healthy eating [47,49,50,56,57]. In their study, as part of the “Get Up and Grow” lifestyle program, Wiseman et al. (2016) implemented the intervention using age-appropriate interactive games (including card-sorting activities, storybooks, craft and coloring activities) during nutrition sessions and organized outdoor games during physical play sessions. After the intervention, there was a significant improvement in the overall knowledge of healthy lifestyle behaviors in the case of the intervention group; however, there was no related change in children’s health behavioral choices [57].
The study by Vaughn et al. (2021) included parents and ECE providers in addition to children aged 3–4 years; however, the results for children showed no significant difference between the experimental and the control group in terms of either nutrition or physical activity [56].
Within the framework of the intervention related to the “Join the Healthy Boat” health promotion program, Kobel et al. (2019) also examined screen media use among 3–4-year-old children, in addition to focusing on physical activity and nutrition. Preschool children in the intervention group spent significantly more days engaging in at least 60 min of MVPA (Moderate to Vigorous Physical Activity) than children in the control group. In addition, the consumption of sweetened beverages decreased to a greater extent in the case of the intervention group. The intervention had no significant effect on media use [49].
As part of the “Color Me Healthy” program, related to Head Start [47], 4–5-year-old children were provided the opportunity to learn about healthy eating and physical activity through an interactive, playful classroom experience. As a result of the intervention, the children recognized fruits and vegetables to a greater extent and were more willing to taste them. Parents reported that the children in the intervention group spent less time in front of the screen and increased their active playtime after the intervention.
Kornilaki et al. (2021) in their study included relevant elements of sustainability in addition to physical activity and nutrition. After the invention, there was a significant increase in children’s knowledge about the links between a healthy lifestyle and sustainability, as well as an increase in fruit and vegetable consumption and physical activity [50].
3.2.4. Nasal Hygiene
In relation to nasal hygiene, Costa et al. (2019) aimed to develop six healthy behaviors among 3–4-year-old children. The intervention implemented within a playful framework contributed to the development of correct health behaviors related to nasal hygiene and to the increase in independence in this regard [45].
3.2.5. Smoking Prevention
In the smoking prevention program carried out in South Korea, age-appropriate activities were used to shape children’s attitudes towards smoking and to expand their knowledge. Thanks to the intervention, the children became able to make the right choices and to protect themselves by developing healthy habits when exposed to smoking because of smokers or a harmful environment around them [48].
3.2.6. Oral Health
During the oral health intervention implemented among children from a low socioeconomic background in India [54], the participants were divided into three groups and provided with different elements of intervention (prohibition of sugary snack consumption in school, teacher supervised daily tooth brushing, oral health education). The results of the intervention show that the prohibition of sugary snack consumption in preschool and daily supervised tooth brushing alone promoted a significant improvement in children’s oral health, regardless of whether they received oral health education or not.
3.3. Methods and Tools of the Interventions Studied
Of the studies included in the analysis, there were seven cluster-randomized studies [44,48,49,50,52,54,56], five quasi-experimental studies [45,47,51,55,57] and two randomized experimental studies [46,53]. All of the studies emphasized that parents were fully informed about the study and gave written consent for their child’s participation. The methodology of the interventions studied is rather diverse and varied (Tables S1 and S2).
Input and output measurements were mainly related to the interventions, including observations (vegetable and fruit consumption, healthy behaviors for nasal hygiene, physical activity), anthropometric measurements, question-and-answer or picture-based interviews with children and parent and teacher questionnaires on the child’s health behavior. Furthermore, dental status examinations were carried out before and after dental hygiene interventions, and in the case of interventions aimed at increasing physical activity, accelerometers were used to measure the child’s activity. In addition, most of the studies also collected data on the sociodemographic characteristics of the participants.
The interventions were based on educational sessions, playful or story-based activities or movement programs, during which the following tools were used: presenting a story, card game with illustrations, other picture-based tests or activities, role plays, videos, power-point presentations, flash card demonstrations, the use of hygienic devices in practice (e.g., toothbrush, toothpaste, handkerchief). In several cases, the children’s activity was encouraged by external rewards (stickers).
3.4. Quality Assessment
For critical appraisal and to limit bias, each included study underwent critical review. Cochrane Risk of Bias criteria [58] were used to explore the risk of bias in the interventional studies. We used the Cochrane risk-of-bias tool for cluster-randomized trials (RoB 2 CRT) [59], the Risk of Bias in quasi-experimental studies tool (ROBINS-I tool) [60] and the Cochrane risk-of-bias tool for randomized trials (RoB 2) [61]. These are not points systems, but rather a judgement of quality, categorized as: high risk (red), unclear risk (yellow) and low risk (green). The results of the quality assessment can be found in Tables S3–S5. As a result of these tools, we can say that most of the studies are good quality studies [47,48,49,50,53,54,56,57]. Only a few of them have some risk, but they also have only a moderate risk of bias [44,45,46,51,52]. One of the quasi-experimental studies [55] has no information about “bias due to missing data”, so the quality check’s result is also “no information”.
4. Discussion
In our systematic review, we aimed to analyze health education programs accompanied by intervention in institutional settings for children aged 3–6. As the focus on healthy lifestyles and the role of early childhood education is growing, there is an increasing research interest in the studied topic.
Despite the large number of publications in the field of early childhood health education, we were able to include few in the review due to the fact that many of them were cross-sectional studies of children’s health knowledge, health status and healthy habits [62,63,64,65,66,67], and also because the majority of recent publications did not focus directly on children, but collected data on children’s health behavior based on the perceptions of adults around them (parents, teachers, health professionals) [68,69,70,71,72,73]. Although some studies described interventions in institutional settings for children aged 3–6, they were not pedagogical in nature, but aimed to influence children’s health behavior only through infrastructural developments (e.g., adding new play equipment to the playground environment) [74,75]. Thirdly, many studies took a health science approach, often focusing on public health measures (e.g., vaccination) [72,76,77] or on a specific group of diseases [78,79,80] or skills development (motor, cognitive skills) [81,82,83]. Finally, in the case of studies relevant to the topic, we have repeatedly found that a large number of publications contained health education recommendations, guidelines, programs or study protocols [62,63,84,85].
We identified a total of 14 studies involving 3–6-year-old children in an institutional setting presenting a health education intervention which also reported the results.
The international heterogeneity of the institutional system of early childhood education is well reflected in the fact that the examined studies report on interventions carried out in different institutional settings (preschool, kindergarten, day care center, Head Start Center, etc.). Participation in early childhood institutional education is not compulsory in all countries; therefore, the tasks and functions of different types of institutions show significant differences, which also affect the content regulation and methodological implementation of health education.
Interventions implemented in an institutional setting were usually short-term ones, lasting from a few weeks to a few months. Some of the programs combine the issue of health education with the perspective of sustainability [49,50,86,87]. There is an increased effort to involve parents [56,88,89] and a special focus on specific target groups (various acute and chronic diseases, conditions related to atypical development, disadvantaged families) [39,40,90,91,92,93].
Based on the systematic analysis of the studies, it can be concluded that physical activity and healthy eating are given increased emphasis during the health education interventions used in early childhood education, with the prevention of obesity and the reduction in screen use as priority goals [44,46,47,49,50,51,52,53,55,56,57]. The dominance of these areas is not surprising as eating habits and an active lifestyle established in early childhood contribute to health maintenance and health promotion in the long term [94].
Several studies emphasize the uniqueness of preschool-organized activities [82,95,96], although it has been a practice in many countries for decades [21,22]. At the same time, WHO guidelines [27] have been drawing the attention to the importance of physical activity for decades and formulating recommendations in this regard. Based on these, they recommend at least 180 min of physical activity per day for preschool children, including 60 min of moderate-to -vigorous intensity physical activity (MVPA) and three days of vigorous intensity aerobic activities per week.
In addition to the above, due to the age of the examined children, the studies prioritize the issue of oral health, but the majority of them mainly include cross-sectional studies or health status assessments [97,98,99].
A holistic approach to health and health education is less common in the context of the reviewed interventions, with a marginal occurrence of topics related to mental and social health, as well as risk behavior.
In all of the analyzed studies, the effort to be child centered appeared, however, based on the intervention descriptions: it seems that the age characteristics of 3–6-year-old children were not always taken into account. This is reflected both in the planned duration of the classroom session and in the requirements set for the children (e.g., selecting only children who could read and write). In addition, in the case of some interventions, a knowledge-based approach was used to achieve health education goals, although several studies confirm that the knowledge of healthy lifestyles and health-promoting habits alone does not lead to a change of behavior [54,57]. This may be due to the fact that some early childhood interventions were initiated and developed by health professionals, who often lack the pedagogical-psychological knowledge and methodological skills related to the education of young children. Moreover, it also occurred that there were no requirements (qualification, knowledge of play pedagogy), other than English language skills, set for the professionals employed by the institutions, who worked with the children and carried out the interventions, so it is questionable to what extent they were able to manage and support the play activities planned by the researchers [56].
The effectiveness of the studied interventions varied. To summarize, based on the studies reviewed, shorter duration and knowledge-focused interventions proved to be less effective; additionally, no spillover effect was experienced. The latter manifested itself in the fact that the effect of the intervention could only be captured in the case of skills closely related to the planned activity. In addition, it is important to emphasize that health-promoting habits for children aged 3–6 years can only be maintained in the long term if the adults around them continuously monitor and confirm correct healthy habits. The effectiveness of interventions can be increased by varied, game-based activities and external reinforcement. During the pre- and post-intervention assessments, the researchers obtained information on the children’s health-related knowledge and the effectiveness of the interventions applied mainly by using pictograms, which can be integrated effectively into kindergarten pedagogical activities.
5. Limitations
Our systematic review was based on three databases: Scopus, WOS and ERIC. Furthermore, only studies published in English language journals and available in their entirety were analyzed. Therefore, it is possible that some relevant publications may have been missed from the analysis.
6. Conclusions
Based on the reviewed studies, the dominance of the content elements related to somatic health (physical activity, nutrition) can be observed and the heterogeneity of the interpretive frameworks in the field of health education content.
Health behavior in early childhood can be captured primarily through health-related habits. Health education interventions in the field of early childhood education proved to be more effective when parents were also involved in the process since health education in the institution is supported and reinforced by similar attitudes and health habits experienced in the family. During all of this, it is important to consider children’s age characteristics and it is advisable to focus on children’s playful activity rather than on the mere transfer of knowledge.
The knowledge, attitude and habits established in the kindergarten environment contribute to children’s health promotion and shape their perspective on sustainability. This can help preschool children to develop their views on health and sustainability and make informed choices about their health behavior.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/educsci13100988/s1, Table S1: Methodology of the included interventions; Table S2: Content of the included interventions; Table S3: Summary of Risk of Bias in cluster-randomized studies; Table S4: Summary of Risk of Bias in quasi-experimental studies; Table S5: Summary of Risk of Bias in randomized experimental studies).
Author Contributions
Two authors M.C. and J.F. screened all studies based on the title and abstract. All papers were screened by three independent authors K.D., E.S. and J.P. A final screening was completed by two authors J.F. and M.C. According to the selection process, J.F. and M.C. prepared the PRISMA flow chart and tables. The specific critical review was conducted by H.B.-C. Writing—review and editing, J.F., J.P., K.D., E.S., H.B.-C. and M.C. All authors have read and agreed to the published version of the manuscript.
Funding
Scientific Foundations of Education Research Program of the Hungarian Academy of Sciences (SZKF-10/2021).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- OECD. Health at a Glance 2021: OECD Indicators; OECD Publishing: Paris, France, 2022. [Google Scholar] [CrossRef]
- WHO. World Health Statistics 2022: Monitoring Health for the SDGs, Sustainable Development Goals; World Health Organization: Paris, France, 2022; Available online: https://cdn.who.int/media/docs/default-source/gho-documents/world-health-statistic-reports/worldhealthstatistics_2022.pdf (accessed on 25 June 2023).
- Fináncz, J.; Podráczky, J.; Nyitrai, Á.; Csima, M. Az egészségműveltség vizsgálatának megalapozása a koragyermekkori nevelésben dolgozók körében [Establishing the foundations for health literacy assessment among early childhood educators.]. Új Pedagógiai Szle. 2021, 71, 19–38. Available online: http://upszonline.hu/index.php?article=711112007 (accessed on 20 April 2023).
- United Nations. Declaration of the United Nations Conference on the Human Environment. 1972. Available online: https://documents-dds-ny.un.org/doc/UNDOC/GEN/NL7/300/05/PDF/NL730005.pdf?OpenElement (accessed on 28 June 2023).
- United Nations. Report of the World Commission on Environment and Development. “Our Common Future” (Brundtland Report). 1987. Available online: https://digitallibrary.un.org/record/139811#record-files-collapse-header (accessed on 18 June 2023).
- Sustainable Development Solutions Network. Health in the Framework of Sustainable Development. Technical Report for the POST-2015 Agenda. 2014. Available online: https://irp-cdn.multiscreensite.com/be6d1d56/files/uploaded/Health-For-All-Report.pdf (accessed on 12 June 2023).
- World Health Organization. Mental Health Atlas 2020; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/publications/i/item/9789240036703 (accessed on 16 June 2023).
- Institute of Health Metrics and Evaluation. Global Health Data Exchange (GHDx). Available online: https://vizhub.healthdata.org/gbd-results/ (accessed on 14 May 2022).
- OECD. Investing in High-Quality Early Childhood Education and Care (ECEC). 2012. Available online: https://www.oecd.org/education/school/48980282.pdf (accessed on 11 April 2023).
- Vandenbroeck, M.; Lenaerts, K.; Beblavý, M. Benefits of Early Childhood Education and Care and the Conditions for Obtaining Them; EENEE Analytical Report No. 32. Prepared for the European Commission; Publications Office of the European Union: Luxembourg, 2018; Available online: https://data.europa.eu/doi/10.2766/20810 (accessed on 22 May 2023).
- Ansari, A.; Pianta, R.C.; Whittaker, J.V.; Vitiello, V.E.; Ruzek, E.A. Starting Early: The Benefits of Attending Early Childhood Education Programs at Age 3. Am. Educ. Res. J. 2019, 56, 1495–1523. [Google Scholar] [CrossRef]
- Hochbaum, G. M: Health Behavior; Wadsworth Publishing Company: Belmont, CA, USA, 1970. [Google Scholar]
- Petosa, R.; Oldfield, D. A Pilot Study of the Impact of Stress Management Techniques on the Classroom Behavior of Elementary School Students. J. Sch. Health 1985, 55, 69–71. [Google Scholar] [CrossRef]
- Sofianopoulo, K.; Bacopoulou, F.; Vlachakis, D.; Kokka, I.; Alexopoulos, E.; Varvogli, L.; Chrousos, G.P.; Darviri, C. Stress Management in Elementary School Students: A Pilot Randomised Controlled Trial. EMBnet J. 2021, 26, e976. [Google Scholar] [CrossRef]
- Royer, N.; Moreau, C. A Survey of Canadian Early Childhood Educators’ Psychological Wellbeing at Work. Early Child. Educ. J. 2016, 44, 135–146. [Google Scholar] [CrossRef]
- Manning, M.; Garvis, S.; Fleming, C.; Wong, G.T. The relationship between teacher qualification and the quality of the early childhood education and care environment. Campbell Syst. Rev. 2017, 13, 1–82. [Google Scholar] [CrossRef]
- World Health Organization. Standards for Healthy Eating, Physical Activity, Sedentary Behaviour and Sleep in Early Childhood Education and Care Settings: A Toolkit; World Health Organization: Geneva, Switzerland, 2021; Available online: https://apps.who.int/iris/rest/bitstreams/1376768/retrieve (accessed on 10 June 2023).
- Midcentral Public Health Service. Health and Safety Guidelines for Early Childhood Education Services. June 2014. Available online: https://www.midcentraldhb.govt.nz/HealthServices/PublicHealth/healthprotection/Documents/MidCentral%20Public%20Health%20Service%20Health%20and%20Safety%20Guidelines%20for%20ECE%20Services.pdf (accessed on 11 June 2023).
- Australian Government, Department of Health. National Action Plan for the Health of Children and Young People 2020–2030; Australian Government: Canberra, Australia, 2019. Available online: https://www.health.gov.au/sites/default/files/documents/2021/04/national-action-plan-for-the-health-of-children-and-young-people-2020-2030-national-action-plan-for-the-health-of-children-and-young-people-2020-2030.pdf (accessed on 11 June 2023).
- National Council of Educational Research and Training. Guidelines for Preschool Education; National Council of Educational Research and Training: New Delhi, India, 2020; Available online: https://ncert.nic.in/dee/pdf/guidelines-for-preschool.pdf (accessed on 14 June 2023).
- Lamanauskas, V.; Malinauskiené, D.; Augiené, D. Health Education in Pre-school Institution: Integration, Effectiveness, Improvement. Eurasia J. Math. Sci. Technol. Educ. 2021, 17, em2046. [Google Scholar] [CrossRef]
- 363/2012. (XII. 17.) Korm. Rendelet az Óvodai Nevelés Országos Alapprogramjáról [Government Decree on the National Core Programme for Kindergarten Education]. Available online: https://net.jogtar.hu/jogszabaly?docid=a1200363.kor (accessed on 11 November 2022).
- Gelbmann, C.; Dieminger-Schnürch, B.; Seper, K.; Simetzberger, S.; Klausmann, L. Qualitätsstandard für die Verpflegung im Kindergarten; Bundesministerium für Soziales, Gesundheit, Pflege und Konsumentenschutz (BMSGPK): Wien, Austria, 2022; Available online: https://www.fitkid-aktion.de/fileadmin/user_upload/medien/DGE-QST/DGE_Qualitaetsstandard_Kita.pdf (accessed on 17 June 2023).
- IN FORM—Deutschlands Initiative für Gesunde Ernährung und mehr Bewegung. DGE-Qualitätsstandard für die Verpflegung in Kitas, 6th ed.; Deutsche Gesellschaft für Ernährung: Bonn, Germany, 2022; Available online: https://www.fitkid-aktion.de/fileadmin/user_upload/medien/DGE-QST/DGE_Qualitaetsstandard_Kita.pdf (accessed on 14 June 2023).
- National Consensus for School Health Education. National Health Education Standards. In Model Guidance for Curriculum and Instruction, 3rd ed.; National Consensus for School Health Education: Atlanta, GA, USA, 2022; Available online: https://www.schoolhealtheducation.org/wp-content/uploads/2022/10/National_Health_Education_Standards_Guide-10.02.2022.pdf (accessed on 12 June 2023).
- Ontario Public Service. The Kindergarten Program; Ontario Public Service: Ontario, Canada, 2016; Available online: https://files.ontario.ca/books/edu_the_kindergarten_program_english_aoda_web_july21.pdf (accessed on 14 June 2023).
- WHO. WHO Guidelines on Physical Activity and Sedentary Behaviour: At a Glance; World Health Organization: Geneva, Switzerland, 2020; Available online: https://apps.who.int/iris/bitstream/handle/10665/337001/9789240014886-eng.pdf (accessed on 11 May 2023).
- Loewenstein, G.; Price, J.; Volpp, K. Habit formation in children: Evidence from incentives for healthy eating. J. Health Econ. 2016, 45, 47–54. [Google Scholar] [CrossRef]
- Borges Rodrigues, S.; Parisod, H.; Barros, L.; Salanterä, S. Examining Empowerment Interventions with Families and Preschool Children: Systematic Review of Randomized Controlled Trials. Health Educ. Behav. 2022, 49, 358–377. [Google Scholar] [CrossRef]
- Chirico, F.; Capitanelli, I.; Bollo, M.; Ferrari, G.; Maran, D.A. Association between workplace violence and burnout syndrome among schoolteachers: A systematic review. J. Health Soc. Sci. 2021, 6, 187–208. [Google Scholar]
- Mytton, J.; Ingram, J.; Manns, S.; Thomas, J. Facilitators and barriers to engagement in parenting programs: A qualitative systematic review. Health Educ. Behav. 2014, 41, 127–137. [Google Scholar] [CrossRef]
- Szpunar, M.; Bruijns, B.; Tucker, P. Measuring Early Childhood Educators’ Physical Activity and Sedentary Behavior-Related Self-Efficacy: A Systematic Review of Tools. Health Educ. Behav. 2021, 48, 455–467. [Google Scholar] [CrossRef]
- Bramantoro, T.; Santoso, C.M.A.; Hariyani, N.; Setyowati, D.; Zulfiana, A.A.; Nor, N.A.M.; Nagy, A.; Pratamawari, D.N.P.; Irmalia, W.R. Effectiveness of the school-based oral health promotion programmes from preschool to high school: A systematic review. PLoS ONE 2021, 16, e0256007. [Google Scholar] [CrossRef]
- dos Santos, A.P.; Nadanovsky, P.; de Oliveira, B.H. A systematic review and meta-analysis of the effects of fluoride toothpastes on the prevention of dental caries in the primary dentition of preschool children. Community Dent. Oral Epidemiol. 2013, 41, 1–12. [Google Scholar] [CrossRef]
- Matvienko-Sikar, K.; Toomey, E.; Delaney, L.; Flannery, C.; McHugh, S.; McSharry, J.; Byrne, M.; Queally, M.; Heary, C.; Kearney, P.M. Behaviour change techniques and theory use in healthcare professional-delivered infant feeding interventions to prevent childhood obesity: A systematic review. Health Psychol. Rev. 2019, 13, 277–294. [Google Scholar] [CrossRef]
- Nekitsing, C.; Blundell-Birtill, P.; Cockroft, J.E.; Hetherington, M.M. Systematic review and meta-analysis of strategies to increase vegetable consumption in preschool children aged 2–5 years. Appetite 2018, 127, 138–154. [Google Scholar] [CrossRef]
- Sanchez-Flack, J.C.; Herman, A.; Buscemi, J.; Kong, A.; Bains, A.; Fitzgibbon, M.L. A systematic review of the implementation of obesity prevention interventions in early childcare and education settings using the RE-AIM framework. Transl. Behav. Med. 2020, 10, 1168–1176. [Google Scholar] [CrossRef]
- Vanderloo, L.M.; Martyniuk, O.J.; Tucker, P. Physical and Sedentary Activity Levels Among Preschoolers in Home-Based Childcare: A Systematic Review. J. Phys. Act. Health 2015, 12, 879–889. [Google Scholar] [CrossRef]
- Alamneh, Y.M.; Adane, F. Magnitude and Predictors of Pneumonia among Under-Five Children in Ethiopia: A Systematic Review and Meta-Analysis. J. Environ. Public Health 2020, 2020, 1606783. [Google Scholar] [CrossRef]
- Szkwarko, D.; Hirsch-Moverman, Y.; Du Plessis, L.; Du Preez, K.; Carr, C.; Mandalakas, A.M. Child contact management in high tuberculosis burden countries: A mixed-methods systematic review. PLoS ONE 2017, 12, e0182185. [Google Scholar] [CrossRef]
- Systematic Review-Research Guide. Available online: https://libguides.murdoch.edu.au/systematic/PICO (accessed on 18 November 2022).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Booth, A.; Clarke, M.; Dooley, G.; Ghersi, D.; Moher, D.; Petticrew, M.; Stewart, L. The nuts and bolts of PROSPERO: An international prospective register of systematic reviews. Syst. Rev. 2012, 9, 2. [Google Scholar] [CrossRef]
- Braga-Pontes, C.; Simões-Dias, S.; Lages, M.; Guarino, M.P.; Graça, P. Nutrition education strategies to promote vegetable consumption in preschool children: The Veggies4myHeart project. Public Health Nutr. 2022, 25, 1061–1070. [Google Scholar] [CrossRef]
- Costa, P.; Ermini, T.; Sigaud, C.H.S. Effects of an educational playful intervention on nasal hygiene behaviors of preschoolers: A quasi-experimental study. Health Promot. Perspect. 2019, 9, 50–54. [Google Scholar] [CrossRef]
- de Droog, S.M.; Buijzen, M.; Valkenburg, P.M. Enhancing children’s vegetable consumption using vegetable-promoting picture books. The impact of interactive shared reading and character-product congruence. Appetite 2014, 73, 73–80. [Google Scholar] [CrossRef]
- Fastring, D.; Keel, K.; Colby, D.; Conner, J.M.; Hilbert, A. Head Start Centers Can Influence Healthy Behaviors: Evaluation of a Nutrition and Physical Activity Educational Intervention. J. Sch. Health 2019, 89, 698–704. [Google Scholar] [CrossRef]
- Kim, S.; Kim, H. Effectiveness of smoking prevention programs for preschool children in South Korea at post intervention. Child. Youth Serv. Rev. 2019, 101, 80–86. [Google Scholar] [CrossRef]
- Kobel, S.; Wirt, T.; Schreiber, A.; Kesztyüs, D.; Kettner, S.; Erkelenz, N.; Wartha, O.; Steinacker, J.M. Intervention Effects of a School-Based Health Promotion Programme on Obesity Related Behavioural Outcomes. J. Obes. 2014, 2014, 476230. [Google Scholar] [CrossRef]
- Kornilaki, E.N.; Skouteris, H.; Morris, H. Developing connections between healthy living and environmental sustainability concepts in Cretan preschool children: A randomized trial. Early Child Dev. Care 2021, 192, 1685–1698. [Google Scholar] [CrossRef]
- Min, J.; Kim, G.; Lim, H.; Carvajal, N.A.; Lloyd, C.W.; Wang, Y. A kindergarten-based child health promotion program: The Adapted National Aeronautics and Space Administration (NASA) Mission X for improving physical fitness in South Korea. Glob. Health Promot. 2019, 26, 52–61. [Google Scholar] [CrossRef]
- O’Dwyer, M.V.; Fairclough, S.J.; Ridgers, N.D.; Knowles, Z.R.; Foweather, L.; Stratton, G. Effect of a school-based active play intervention on sedentary time and physical activity in preschool children. Health Educ. Res. 2013, 28, 931–942. [Google Scholar] [CrossRef] [PubMed]
- Robinson, L.E.; Palmer, K.K.; Webster, E.K.; Logan, S.W.; Chinn, K.M. The Effect of CHAMP on Physical Activity and Lesson Context in Preschoolers: A Feasibility Study. Res. Q. Exerc. Sport. 2018, 89, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Samuel, S.R.; Acharya, S.; Rao, J.C. School Interventions-based Prevention of Early-Childhood Caries among 3-5-year-old children from very low socioeconomic status: Two-year randomized trial. J. Public Health Dent. 2020, 80, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Schindler, J.M.; Corbett, D.; Forestell, C.A. Assessing the effect of food exposure on children’s identification and acceptance of fruit and vegetables. Eat. Behav. 2013, 14, 53–56. [Google Scholar] [CrossRef][Green Version]
- Vaughn, A.E.; Hennink-Kaminski, H.; Moore, R.; Burney, R.; Chittams, J.L.; Parker, P.; Luecking, C.T.; Hales, D.; Ward, D.S. Evaluating a child care-based social marketing approach for improving children’s diet and physical activity: Results from the Healthy Me, Healthy We cluster-randomized controlled trial. Transl. Behav. Med. 2021, 7, 775–784. [Google Scholar] [CrossRef] [PubMed]
- Wiseman, N.; Harris, N.; Lee, P. Lifestyle knowledge and preferences in preschool children: Evaluation of the Get up and Grow healthy lifestyle education programme. Health Educ. J. 2016, 75, 1012–1024. [Google Scholar] [CrossRef]
- A Guide to Evidence Synthesis: 9. Risk of Bias Assessment. Available online: https://guides.library.cornell.edu/evidencesynthesis/bias (accessed on 8 May 2023).
- RoB 2 for Cluster-Randomized Trials. Available online: https://www.riskofbias.info/welcome/rob-2-0-tool/rob-2-for-cluster-randomized-trials (accessed on 14 May 2023).
- ROBINS-I Tool (Risk of Bias in Non-randomized Studies—Of Interventions). Available online: https://www.riskofbias.info/welcome/home (accessed on 14 May 2023).
- Revised Cochrane Risk of Bias Tool for Randomized Trials (RoB 2.0). Available online: https://www.riskofbias.info/welcome/rob-2-0-tool/archive-rob-2-0-2016 (accessed on 14 May 2023).
- Gao, W.; Zhang, Y.; Wu, D.; Dong, Y.; Liu, N.; Wang, H. Compliance with Health-Related Behaviors Guidelines and Its Relationship with Multiple Factors in Preschool Children Aged 3–6 Years: A National Cross-Sectional Survey in China. Int. J. Environ. Res. Public Health 2022, 23, 1262. [Google Scholar] [CrossRef]
- De Craemer, M.; Verbestel, V.; Cardon, G.; Androutsos, O.; Manios, Y.; Chastin, S. Correlates of Meeting the Physical Activity, Sedentary Behavior, and Sleep Guidelines for the Early Years among Belgian Preschool Children: The ToyBox-Study. Int. J. Environ. Res. Public Health 2020, 24, 7006. [Google Scholar] [CrossRef]
- Sterdt, E.; Pape, N.; Kramer, S.; Liersch, S.; Urban, M.; Werning, R.; Walter, U. Do children’s health resources differ according to preschool physical activity programmes and parental behaviour? A mixed methods study. Int. J. Environ. Res. Public Health 2014, 26, 2407–2426. [Google Scholar] [CrossRef]
- Felix, E.; Silva, V.; Caetano, M.; Ribeiro, M.V.V.; Fidalgo, T.M.; Rosa Neto, F.; Sanchez, Z.M.; Surkan, P.J.; Martins, S.S.; Caetano, S.C. Excessive Screen Media Use in Preschoolers Is Associated with Poor Motor Skills. Cyberpsychol. Behav. Soc. Netw. 2020, 23, 418–425. [Google Scholar] [CrossRef]
- Vanderloo, L.M.; Tucker, P. Physical activity and sedentary time among young children in full-day kindergarten: Comparing traditional and balanced day schedules. Health Educ. J. 2017, 76, 29–37. [Google Scholar] [CrossRef]
- Vanderloo, L.M.; Tucker, P.; Johnson, A.M.; van Zandvoort, M.M.; Burke, S.M.; Irwin, J.D. The influence of centre-based childcare on preschoolers’ physical activity levels: A cross-sectional study. Int. J. Environ. Res. Public Health 2014, 5, 1794–1802. [Google Scholar] [CrossRef] [PubMed]
- Myers, G.; Wright, S.; Blane, S.; Pratt, I.S.; Pettigrew, S. A process and outcome evaluation of an in-class vegetable promotion program. Appetite 2018, 125, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Rasmus, K.; Toratti, A.; Karki, S.; Pesonen, P.; Laitala, M.L.; Anttonen, V. Acceptability of a Mobile Application in Children’s Oral Health Promotion-A Pilot Study. Int. J. Environ. Res. Public Health 2021, 22, 3256. [Google Scholar] [CrossRef]
- Roberts-Gray, C.; Sweitzer, S.J.; Ranjit, N.; Potratz, C.; Rood, M.; Romo-Palafox, M.J.; Byrd-Williams, C.E.; Briley, M.E.; Hoelscher, D.M. Structuring Process Evaluation to Forecast Use and Sustainability of an Intervention: Theory and Data From the Efficacy Trial for Lunch Is in the Bag. Health Educ. Behav. 2017, 44, 559–569. [Google Scholar] [CrossRef]
- Wang, Y.; Huang, Z.; Yang, M.; Wang, F.; Xiao, S. Reducing environmental tobacco smoke exposure of preschool children: A randomized controlled trial of class-based health education and smoking cessation counseling for caregivers. Int. J. Environ. Res. Public Health 2015, 12, 692–709. [Google Scholar] [CrossRef]
- Leidner, A.J.; Maughan, E.D.; Bjork, A.; Black, C.; Mazyck, D.; Underwood, J.M. Vaccination-Related Activities at Schools With Kindergartners: Evidence From a School Nurse Survey. J. Sch. Nurs. 2020, 36, 464–471. [Google Scholar] [CrossRef]
- Lee, B.; Kim, Y.E. Factor Structure and Validation of the 12-Item Korean Version of the General Health Questionnaire in a Sample of Early Childhood Teachers. Educ. Sci. 2021, 11, 243. [Google Scholar] [CrossRef]
- Bundy, A.; Engelen, L.; Wyver, S.; Tranter, P.; Ragen, J.; Bauman, A.; Baur, L.; Schiller, W.; Simpson, J.M.; Niehues, A.N.; et al. Sydney Playground Project: A Cluster-Randomized Trial to Increase Physical Activity, Play, and Social Skills. J. Sch. Health 2017, 87, 751–759. [Google Scholar] [CrossRef]
- Sando, O.J.; Mehus, N. Supportive indoor environments for functional play in ECEC institutions: A strategy for promoting well-being and physical activity? Early Child Dev. Care 2021, 191, 921–932. [Google Scholar] [CrossRef]
- Appel, J.M.; Fullerton, K.; Hennessy, E.; Korn, A.R.; Tovar, A.; Allender, S.; Hovmand, P.S.; Kasman, M.; Swinburn, B.A.; Hammond, R.A.; et al. Design and methods of Shape Up Under 5: Integration of systems science and community-engaged research to prevent early childhood obesity. PLoS ONE 2019, 1, e0220169. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.Y.; Leung, K.M.; Tam, W.W.; Lee, A. Varicella vaccine uptake and associated factors in children in Hong Kong. Epidemiol. Infect. 2014, 142, 994–1001. [Google Scholar] [CrossRef] [PubMed]
- Calle-Bustos, A.M.; Juan, M.C.; García-García, I.; Abad, F. An augmented reality game to support therapeutic education for children with diabetes. PLoS ONE 2017, 28, e0184645. [Google Scholar] [CrossRef] [PubMed]
- Noordam, A.C.; Carvajal-Velez, L.; Sharkey, A.B.; Young, M.; Cals, J.W. Care seeking behaviour for children with suspected pneumonia in countries in sub-Saharan Africa with high pneumonia mortality. PLoS ONE 2015, 23, e0117919. [Google Scholar] [CrossRef]
- Milgramm, A.; Corona, L.L.; Janicki-Menzie, C.; Christodulu, K.V. Community-based Parent Education for Caregivers of Children Newly Diagnosed with Autism Spectrum Disorder. J. Autism Dev. Disord. 2022, 52, 1200–1210. [Google Scholar] [CrossRef] [PubMed]
- Sigmundsson, H.; Haga, M. Motor competence is associated with physical fitness in four- to six-year-old preschool children. Eur. Early Child. Educ. Res. J. 2016, 24, 477–488. [Google Scholar] [CrossRef]
- Ruiz-Esteban, C.; Terry Andrés, J.; Méndez, I.; Morales, Á. Analysis of Motor Intervention Program on the Development of Gross Motor Skills in Preschoolers. Int. J. Environ. Res. Public Health 2020, 7, 4891. [Google Scholar] [CrossRef]
- Ngololo Kamara, E.; Kasanda, C.; Van Rooy, G. Provision of Integrated Early Childhood Development in Namibia: Are We on the Right Track? Educ. Sci. 2018, 8, 117. [Google Scholar] [CrossRef]
- Delaney, T.; Jackson, J.K.; Jones, J.; Hall, A.; Dives, A.; Wedesweiler, T.; Campbell, L.; Nathan, N.; Romiti, M.; Trost, S.G.; et al. A Cluster Randomised Controlled Trial of an Intervention to Increase Physical Activity of Preschool-Aged Children Attending Early Childhood Education and Care: Study Protocol for the ‘Everybody Energise’ Trial. Int. J. Environ. Res. Public Health 2019, 4, 4275. [Google Scholar] [CrossRef]
- Mooses, K.; Mäestu, J.; Riso, E.M.; Hannus, A.; Mooses, M.; Kaasik, P.; Kull, M. Different Methods Yielded Two-Fold Difference in Compliance with Physical Activity Guidelines on School Days. PLoS ONE 2016, 25, e0152323. [Google Scholar] [CrossRef]
- Lee, R.E.; Szeszulski, J.; Lorenzo, E.; Arriola, A.; Bruening, M.; Estabrooks, P.A.; Hill, J.L.; O’Connor, T.M.; Shaibi, G.Q.; Soltero, E.G.; et al. Sustainability via Active Garden Education: The Sustainability Action Plan Model and Process. Int. J. Environ. Res. Public Health 2022, 1, 5511. [Google Scholar] [CrossRef] [PubMed]
- Farewell, C.V.; Maiurro, E.; Powers, J.; Puma, J. The Healthy Environment Project: Promoting sustainable change in early childhood education settings. Health Educ. J. 2021, 80, 472–486. [Google Scholar] [CrossRef]
- Latomme, J.; Cardon, G.; De Bourdeaudhuij, I.; Iotova, V.; Koletzko, B.; Socha, P.; Moreno, L.; Androutsos, O.; Manios, Y.; De Craemer, M.; et al. Effect and process evaluation of a kindergarten-based, family-involved intervention with a randomized cluster design on sedentary behaviour in 4- to 6-year old European preschool children: The ToyBox-study. PLoS ONE 2017, 5, e0172730. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Huang, Y.; Zhang, Y.; Liu, F.; Feng, C.X.; Liu, T.; Li, C.; Ling, D.D.; Mu, Y.; Tarver, S.L.; et al. Evaluation of fast food behavior in pre-school children and parents following a one-year intervention with nutrition education. Int. J. Environ. Res. Public Health 2014, 30, 6780–6790. [Google Scholar] [CrossRef] [PubMed]
- Wiggins, L.D.; Nadler, C.; Hepburn, S.; Rosenberg, S.; Reynolds, A.; Zubler, J. Toileting Resistance Among Preschool-Age Children with and Without Autism Spectrum Disorder. J. Dev. Behav. Pediatr. 2022, 1, 216–223. [Google Scholar] [CrossRef]
- Zhou, N.; Wong, H.M.; McGrath, C. Social story-based oral health promotion for preschool children with special healthcare needs: A 24-month randomized controlled trial. Community Dent. Oral Epidemiol. 2020, 48, 415–422. [Google Scholar] [CrossRef]
- Feng, D.; Song, H.; Esperat, M.C.; Black, I. A Multicomponent Intervention Helped Reduce Sugar-Sweetened Beverage Intake in Economically Disadvantaged Hispanic Children. Am. J. Health Promot. 2016, 30, 594–603. [Google Scholar] [CrossRef]
- Rathnayake, N.; De Silva Weliange, S.; Guruge, G.N.D. Effectiveness of a health promotion intervention to address determinants of child neglect in a disadvantaged community in Sri Lanka. J. Health Popul. Nutr. 2021, 8, 48. [Google Scholar] [CrossRef]
- López-Banet, L.; Miguélez Rosique, J.A.; Martínez-Carmona, M.; Ayuso Fernández, G.E. Development of Food Competence in Early Childhood Education. Educ. Sci. 2022, 12, 64. [Google Scholar] [CrossRef]
- Palmer, K.K.; Farquhar, J.M.; Chinn, K.M.; Robinson, L.E. Are Gross Motor Skill Interventions an Equitable Replacement for Outdoor Free Play Regarding Children’s Physical Activity? Am. J. Health Promot. 2022, 36, 643–650. [Google Scholar] [CrossRef]
- Chuang, R.J.; Sharma, S.V.; Perry, C.; Diamond, P. Does the CATCH Early Childhood Program Increase Physical Activity Among Low-Income Preschoolers?—Results From a Pilot Study. Am. J. Health Promot. 2018, 32, 344–348. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, T.; Quissell, D.O.; Henderson, W.G.; Thomas, J.F.; Bryant, L.L.; Braun, P.A.; Albino, J.E. Factors Associated with Oral Health Status in American Indian Children. J. Racial Ethn. Health Disparities 2014, 1, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.; Sokal-Gutierrez, K.; Chung, K.; Lin, W.; Khanh, L.N.; Chung, R.; Hoang, H.T.; Ivey, S.L. Maternal and Child Nutrition and Oral Health in Urban Vietnam. Int. J. Environ. Res. Public Health 2019, 19, 2579. [Google Scholar] [CrossRef] [PubMed]
- George, A.; Grace, R.; Elcombe, E.; Villarosa, A.R.; Mack, H.A.; Kemp, L.; Ajwani, S.; Wright, D.C.; Anderson, C.; Bucknall, N.; et al. The oral health behaviours and fluid consumption practices of young urban Aboriginal preschool children in south-western Sydney, New South Wales, Australia. Health Promot. J. Austr. 2018, 29, 23–30. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).