Pharmacists’ Knowledge, Attitude and Practice Regarding the Dispensing of Antibiotics without Prescription in Tanzania: An Explorative Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Site
2.2. Study Design and Sampling
2.3. Study Tools
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
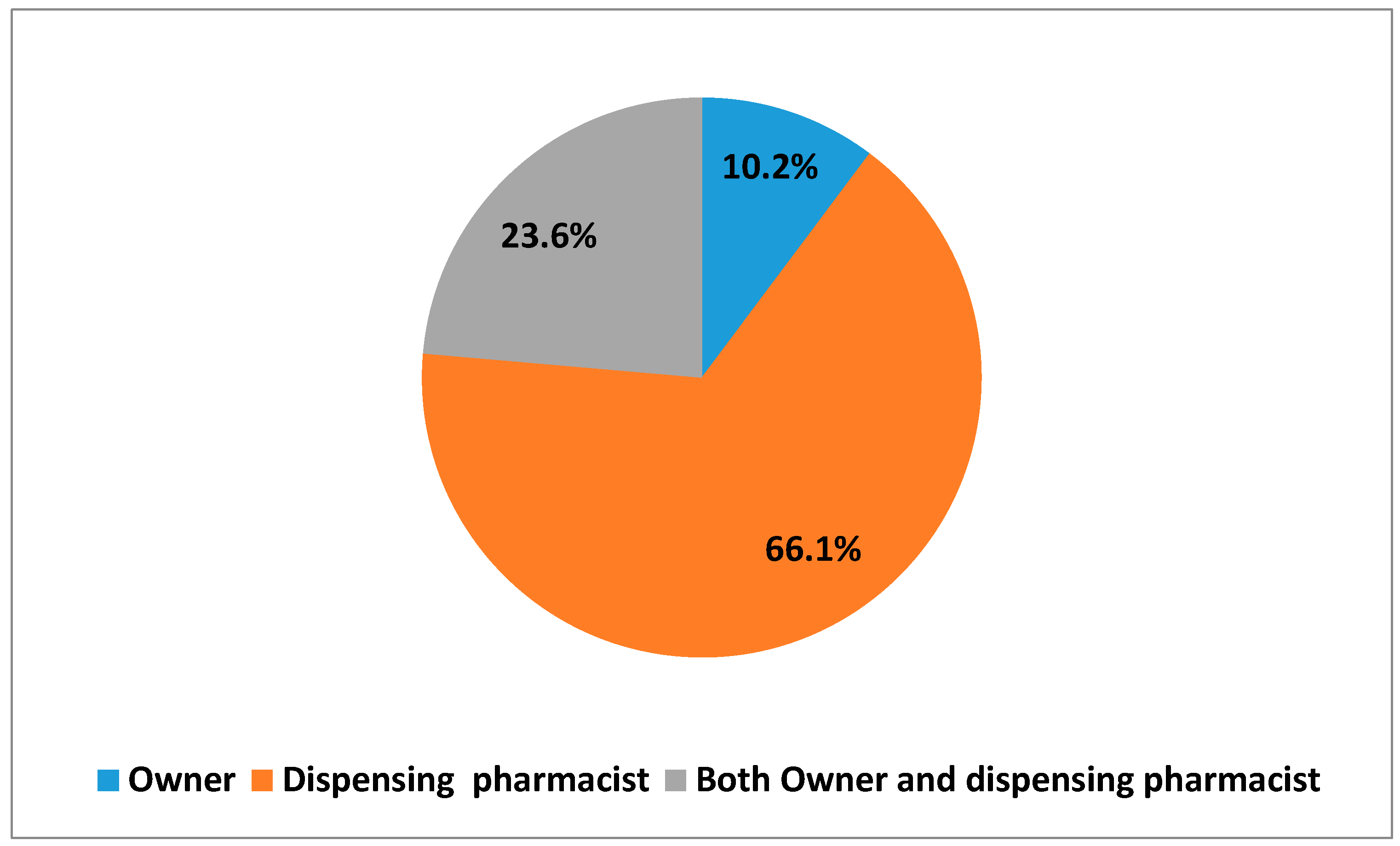
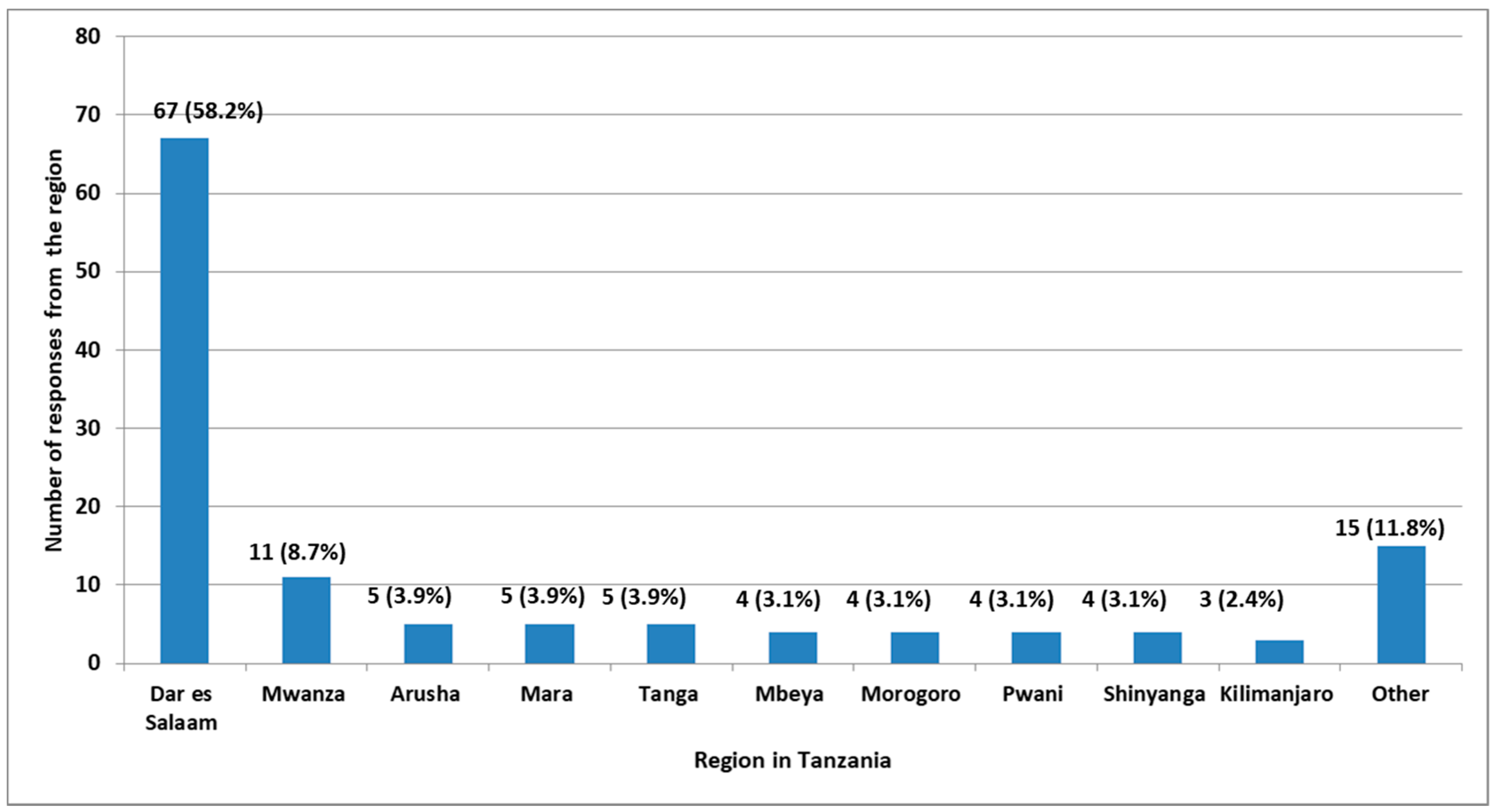
3.1. Socio-Demographic Characteristics
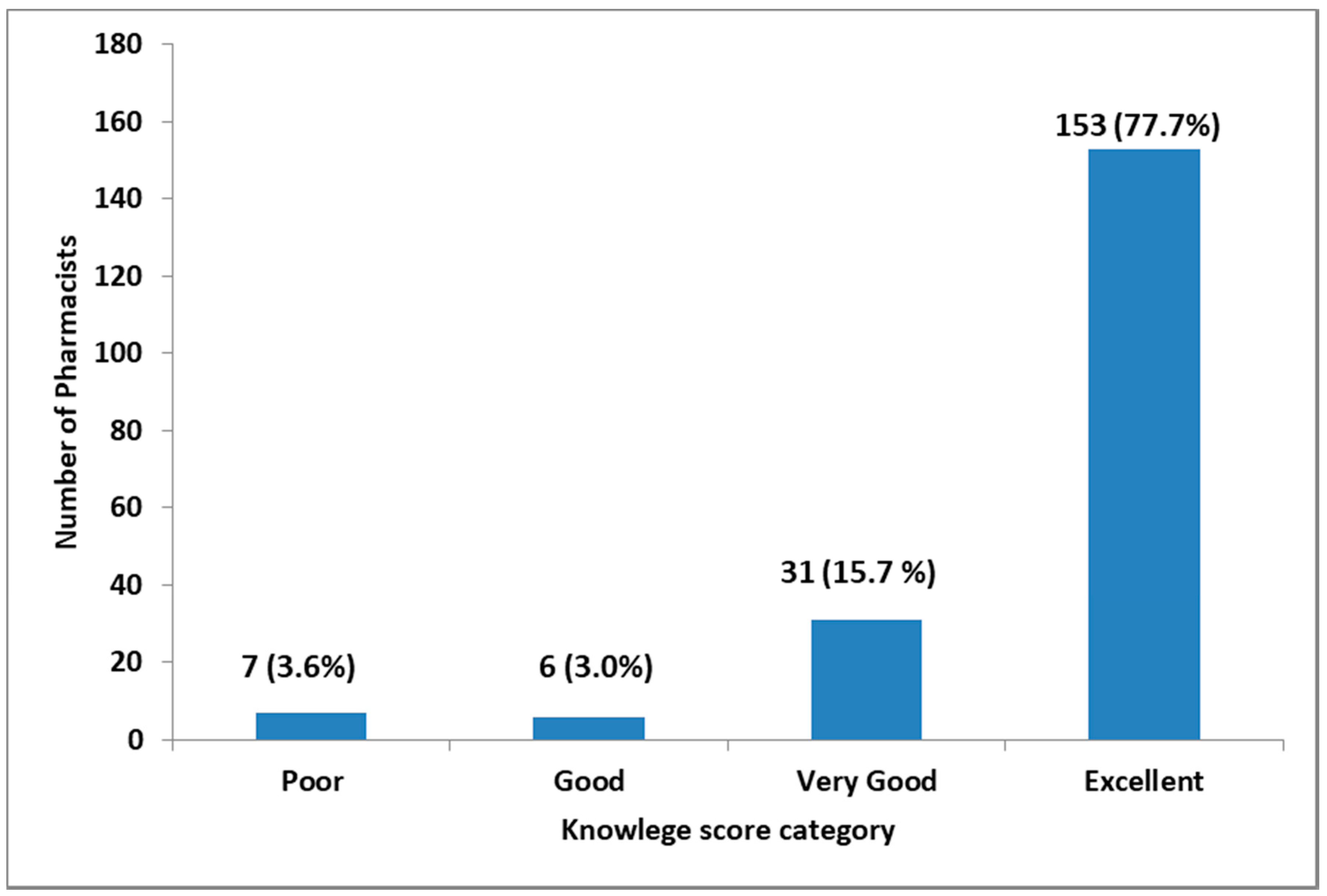
3.2. Pharmacists’ Knowledge
3.3. Pharmacists’ Attitude towards Dispensing of Antibiotics without a Prescription
3.4. Pharmacists’ Practice towards Dispensing of Antibiotics without a Prescription
3.5. Classes of Antibiotics that Were Mostly Dispensed without a Prescription
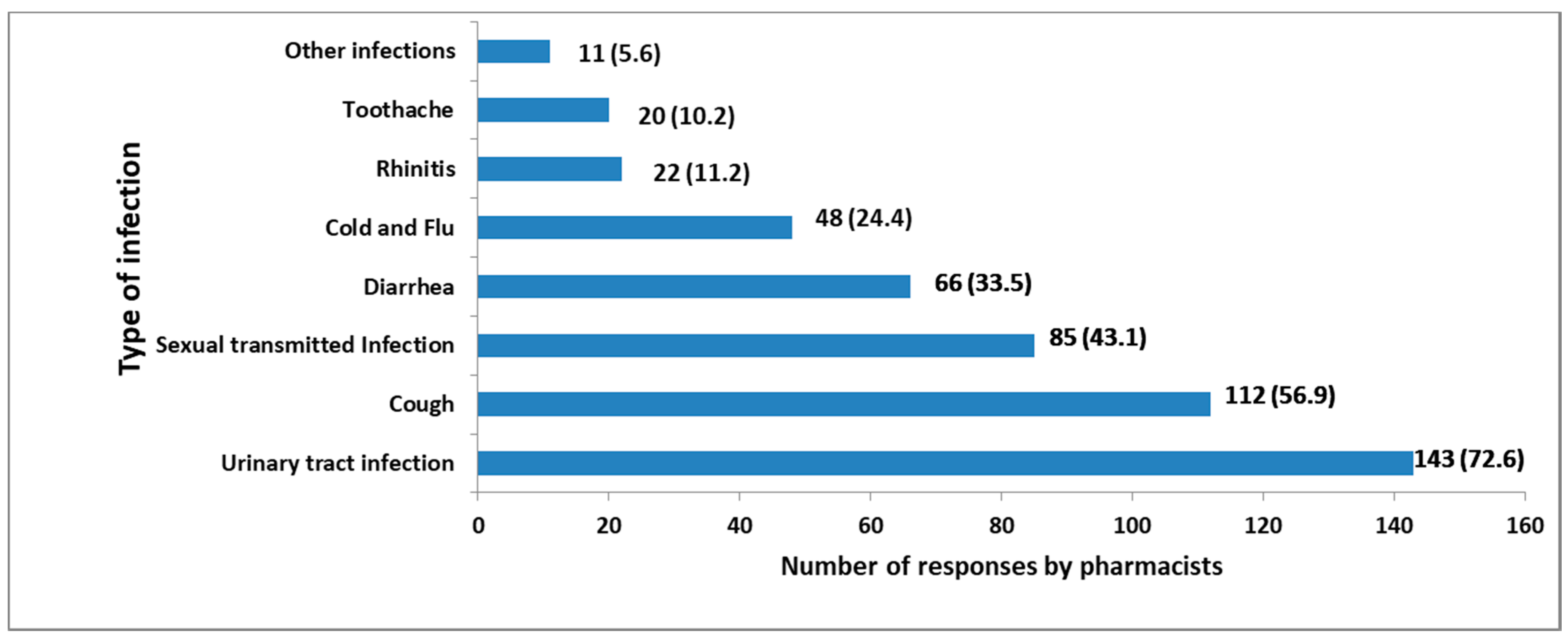
3.6. Medical Conditions and Infections for Which Antibiotics Are Commonly Administered without a Prescription
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Levy, S.B.; Marshall, B. Antibacterial resistance worldwide: Causes, challenges and responses. Nat. Med. 2004, 10, S122–S129. [Google Scholar] [CrossRef] [PubMed]
- Hadi, M.A.; Karami, N.A.; Al-Muwalid, A.S.; Al-Otabi, A.; Al-Subahi, E.; Bamomen, A.; Mohamed, M.M.A.; Elrggal, M.E. Community pharmacists’ knowledge, attitude, and practices towards dispensing antibiotics without prescription (DAwP): A cross-sectional survey in Makkah Province, Saudi Arabia. Int. J. Infect. Dis. 2016, 47, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Nga, D.T.T.; Chuc, N.T.K.; Hoa, N.P.; Hoa, N.Q.; Nguyen, N.T.T.; Loan, H.T.; Toan, T.K.; Phuc, H.D.; Horby, P.; Van Yen, N.; et al. Antibiotic sales in rural and urban pharmacies in northern Vietnam: An observational study. BMC Pharmacol. Toxicol. 2014, 15, 6. [Google Scholar] [CrossRef] [PubMed]
- de Kraker, M.E.A.; Davey, P.G.; Grundmann, H. Mortality and Hospital Stay Associated with Resistant Staphylococcus aureus and Escherichia coli Bacteremia: Estimating the Burden of Antibiotic Resistance in Europe. PLoS Med. 2011, 8, e1001104. [Google Scholar] [CrossRef] [PubMed]
- Stewardson, A.J.; Allignol, A.; Beyersmann, J.; Graves, N.; Schumacher, M.; Meyer, R.; Tacconelli, E.; De Angelis, G.; Farina, C.; Pezzoli, F.; et al. The health and economic burden of bloodstream infections caused by antimicrobial-susceptible and non-susceptible Enterobacteriaceae and Staphylococcus aureus in European hospitals, 2010 and 2011: A multicentre retrospective cohort study. Eurosurveillance 2016, 21, 30319. [Google Scholar] [CrossRef] [PubMed]
- Bahnassi, A. A qualitative analysis of pharmacists’ attitudes and practices regarding the sale of antibiotics without prescription in Syria. J. Taibah Univ. Med. Sci. 2015, 10, 227–233. [Google Scholar] [CrossRef]
- Akpan, M.R.; Isemin, N.U.; Udoh, A.E.; Ashiru-Oredope, D. Implementation of antimicrobial stewardship programmes in African countries: A systematic literature review. J. Glob. Antimicrob. Resist. 2020, 22, 317–324. [Google Scholar] [CrossRef]
- Sangeda, R.Z.; Kibona, J.; Munishi, C.; Arabi, F.; Manyanga, V.P.; Mwambete, K.D.; Horumpende, P.G. Assessment of implementation of Antimicrobial Resistance Surveillance and Antimicrobial Stewardship Programs in Tanzanian health facilities a year after launch of the National Action Plan. Front. Public Health 2020, 8, 454. [Google Scholar] [CrossRef]
- Ayukekbong, J.A.; Ntemgwa, M.; Atabe, A.N. The threat of antimicrobial resistance in developing countries: Causes and control strategies. Antimicrob. Resist. Infect. Control 2017, 6, 47. [Google Scholar] [CrossRef]
- Vazquez-Lago, J.; Gonzalez-Gonzalez, C.; Zapata-Cachafeiro, M.; Lopez-Vazquez, P.; Taracido, M.; López, A.; Figueiras, A. Knowledge, attitudes, perceptions and habits towards antibiotics dispensed without medical prescription: A qualitative study of Spanish pharmacists. BMJ Open 2017, 7. [Google Scholar] [CrossRef]
- Salim, A.M.A.; Elgizoli, B. Exploring the reasons why pharmacists dispense antibiotics without prescriptions in Khartoum state, Sudan. Int. J. Pharm. Pract. 2017, 25, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Haddadin, R.N.; Alsous, M.; Wazaify, M.; Tahaineh, L. Evaluation of antibiotic dispensing practice in community pharmacies in Jordan: A cross sectional study. PLoS ONE 2019, 14, e0216115. [Google Scholar] [CrossRef]
- Farah, R.; Lahoud, N.; Salameh, P.; Saleh, N. Antibiotic dispensation by Lebanese pharmacists: A comparison of higher and lower socio-economic levels. J. Infect. Public Health 2015, 8. [Google Scholar] [CrossRef]
- Leung, E.; Weil, D.E.; Raviglione, M.; Nakatani, H. The WHO policy package to combat antimicrobial resistance. Bull. World Health Organ. 2011, 89, 390–392. [Google Scholar] [CrossRef] [PubMed]
- Embrey, M.; Vialle-Valentin, C.; Dillip, A.; Kihiyo, B.; Mbwasi, R.; Semali, I.A.; Chalker, J.C.; Liana, J.; Lieber, R.; Johnson, K.; et al. Understanding the Role of Accredited Drug Dispensing Outlets in Tanzania’s Health System. PLoS ONE 2016, 11, e0164332. [Google Scholar] [CrossRef]
- Cohen, J.M.; Sabot, O.; Sabot, K.; Gordon, M.; Gross, I.; Bishop, D.; Odhiambo, M.; Ipuge, Y.; Ward, L.; Mwita, A.; et al. A pharmacy too far? Equity and spatial distribution of outcomes in the delivery of subsidized artemisinin-based combination therapies through private drug shops. BMC Health Serv. Res. 2010, 10, S6. [Google Scholar] [CrossRef]
- Horumpende, P.G.; Sonda, T.B.; van Zwetselaar, M.; Antony, M.L.; Tenu, F.F.; Mwanziva, C.E.; Shao, E.R.; Mshana, S.E.; Mmbaga, B.T.; Chilongola, J.O. Prescription and non-prescription antibiotic dispensing practices in part I and part II pharmacies in Moshi Municipality, Kilimanjaro Region in Tanzania: A simulated clients approach. PLoS ONE 2018, 13, e0207465. [Google Scholar] [CrossRef]
- Minzi, O.M.; Manyilizu, V.S. Manyilizu Application of basic pharmacology and dispensing practice of antibiotics in accredited drug-dispensing outlets in Tanzania. Drug Healthc. Patient Saf. 2013, 5, 5. [Google Scholar] [CrossRef] [PubMed]
- Viberg, N.; Kalala, W.; Mujinja, P.; Tomson, G.; Lundborg, C.S. “Practical knowledge” and perceptions of antibiotics and antibiotic resistance among drugsellers in Tanzanian private drugstores. BMC Infect. Dis. 2010, 10, 270. [Google Scholar] [CrossRef] [PubMed]
- National Bureau of Statistics Report of 2012 Population and Housing Census, The United Republic of Tanzania. Available online: https://www.nbs.go.tz/nbs/takwimu/census2012/Basic_Demographic_and_Socio-Economic_Profile_PopularVersion-KeyFindings_2012_PHC_EnglishVersion.pdf (accessed on 6 November 2019).
- The Pharmacy Council of Tanzania Pharmacy Council Tanzania Newsletter. Available online: https://www.pc.go.tz/files/PharmacyCouncilNewsletterApril—June2019.pdf (accessed on 6 November 2019).
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)--A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Erku, D.A.; Aberra, S.Y. Non-prescribed sale of antibiotics for acute childhood diarrhea and upper respiratory tract infection in community pharmacies: A 2 phase mixed-methods study. Antimicrob. Resist. Infect. Control 2018, 7, 92. [Google Scholar] [CrossRef]
- Shet, A.; Sundaresan, S.; Forsberg, B.C. Pharmacy-based dispensing of antimicrobial agents without prescription in India: Appropriateness and cost burden in the private sector. Antimicrob. Resist. Infect. Control 2015, 4, 55. [Google Scholar] [CrossRef] [PubMed]
- Dillip, A.; Embrey, M.; Shekalaghe, E.; Ross-Degnan, D.; Vialle-Valentin, C.; Kimatta, S.; Liana, J.; Rutta, E.; Valimba, R.; Chalker, J. What motivates antibiotic dispensing in accredited drug dispensing outlets in Tanzania? A qualitative study. Antimicrob. Resist. Infect. Control 2015, 4, 30. [Google Scholar] [CrossRef]
- Dekker, A.; Smit, R. Pharmacist Initiated Therapy: Recognition and Treatment of Minor Ailments; Juta and Company Ltd.: Cape Town, South Africa, 1993. [Google Scholar]
- Gebretekle, G.B.; Serbessa, M.K. Exploration of over the counter sales of antibiotics in community pharmacies of Addis Ababa, Ethiopia: Pharmacy professionals’ perspective. Antimicrob. Resist. Infect. Control 2016, 5, 1–7. [Google Scholar] [CrossRef]
- Dooling, K.; Kandeel, A.; Hicks, L.; El-Shoubary, W.; Fawzi, K.; Kandeel, Y.; Etman, A.; Lohiniva, A.; Talaat, M. Understanding Antibiotic Use in Minya District, Egypt: Physician and Pharmacist Prescribing and the Factors Influencing Their Practices. Antibiotics 2014, 3, 233–243. [Google Scholar] [CrossRef]
- Yewale, V.N. Antimicrobial resistance—A ticking bomb! Indian Pediatr. 2014, 51, 171–172. [Google Scholar] [CrossRef] [PubMed]
- Mathews, B.; Thalody, A.A.; Miraj, S.S.; Kunhikatta, V.; Rao, M.; Saravu, K. Adverse Effects of Fluoroquinolones: A Retrospective Cohort Study in a South Indian Tertiary Healthcare Facility. Antibiotics 2019, 8, 104. [Google Scholar] [CrossRef]
- The United Republic of Tanzania Tanzania National Antimicrobial Resistance Action Plan 017-2022. Available online: https://www.flemingfund.org/wp-content/uploads/8b8fc897c422e11504c8c2ba126fac02.pdf (accessed on 2 January 2020).
- Akinyandenu, O.; Akinyandenu, A. Irrational use and non-prescription sale of antibiotics in Nigeria: A need for change. J. Sci. Innov. Res. 2014, 3, 251–257. [Google Scholar]
- Bavestrello, L.; Cabello, A.; Casanova, D. Impact of regulatory measures in the trends of community consumption of antibiotics in Chile. Rev. Med. Chil. 2002, 130, 1265–1272. [Google Scholar] [CrossRef]

| Parameter | Frequency (%) |
|---|---|
| Age, years (n = 197) | |
| 21–30 | 94 (47.7) |
| 31–40 | 70 (35.5) |
| >40 | 33 (16.8) |
| Experience, years (n = 197) | |
| 1–5 | 125 (63.5) |
| >5 | 72 (36.5) |
| Sex (n = 197) | |
| Male | 140 (71.1) |
| Female | 57 (28.9) |
| Education level (n = 197) | |
| Bachelor | 153 (77.7) |
| Masters | 41 (20.8) |
| PhD | 3 (1.5) |
| Country of graduation (n = 197) | |
| Tanzania | 182 (92.4) |
| India | 8 (4.1) |
| Other | 7 (3.5) |
| Dispense antibiotics without a prescription? (n = 197) | |
| Yes | 143 (72.6) |
| No | 54 (27.4) |
| Work in any community Pharmacy? (n = 197) | |
| Yes | 127 (64.5) |
| No | 70 (35.5) |
| Question Responses | Yes | No |
|---|---|---|
| Do you think there is any problem if you dispense antibiotics without a prescription? | 186 (94.4%) | 11 (5.6%) |
| Pharmacist should stop dispensing without a prescription | 156 (79.2%) | 41 (20.8%) |
| I encourage the patient to consult a physician and get a prescription before visiting the pharmacy | 111 (56.3%) | 86 (43.6%) |
| Pharmacists are knowledgeable enough to dispense without a prescription after critical evaluation of patient sickness | 141 (71.6%) | 56 (28.4%) |
| Do you dispense antibiotics without a prescription? | 143 (72.6%) | 54 (27.6%) |
| Work as Community Pharmacist? | No | Yes | Total | p-Value | |
|---|---|---|---|---|---|
| Dispense without a prescription? | Yes | 39 (55.7%) | 104 (81.9%) | 143 (72.6%) | |
| No | 31 (44.3%) | 23 (18.1%) | 54 (27.4%) | ||
| Total | 70 (100%) | 127 (100%) | 197 (100%) | <0.0001 |
| Attitude | Bad | Good | Total | p-Value | |
|---|---|---|---|---|---|
| Dispense without prescription? | Yes | 40 (97.6%) | 103 (66.0%) | 143 (72.6%) | |
| No | 1 (2.4%) | 53 (34.0%) | 54 (27.4%) | ||
| Total | 41 (100%) | 156 (100%) | 197 (100%) | <0.0001 |
| Reasons for Stopping Dispensing Antibiotics without Prescription (n = 83) * | Frequency (%) |
|---|---|
| To prevent the development and spread of AMR | 46 (55.4) |
| To promote rational use of medicines | 13 (15.6) |
| There are stringent regulatory authorities | 11 (13.2) |
| The practice is illegal | 9 (10.8) |
| There will be adequate health facilities in the future | 4 (5.0) |
| Reasons for not stopping the practice in the future (n = 57) * | |
| Pharmacists are knowledgeable enough to dispense without a prescription | 29 (50.9) |
| Profitability nature of pharmacies business | 12 (21.1) |
| Not enough health facilities for patients to obtain a prescription | 9 (15.8) |
| No stringent regulatory authorities | 7 (12.2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poyongo, B.P.; Sangeda, R.Z. Pharmacists’ Knowledge, Attitude and Practice Regarding the Dispensing of Antibiotics without Prescription in Tanzania: An Explorative Cross-Sectional Study. Pharmacy 2020, 8, 238. https://doi.org/10.3390/pharmacy8040238
Poyongo BP, Sangeda RZ. Pharmacists’ Knowledge, Attitude and Practice Regarding the Dispensing of Antibiotics without Prescription in Tanzania: An Explorative Cross-Sectional Study. Pharmacy. 2020; 8(4):238. https://doi.org/10.3390/pharmacy8040238
Chicago/Turabian StylePoyongo, Baraka P., and Raphael Zozimus Sangeda. 2020. "Pharmacists’ Knowledge, Attitude and Practice Regarding the Dispensing of Antibiotics without Prescription in Tanzania: An Explorative Cross-Sectional Study" Pharmacy 8, no. 4: 238. https://doi.org/10.3390/pharmacy8040238
APA StylePoyongo, B. P., & Sangeda, R. Z. (2020). Pharmacists’ Knowledge, Attitude and Practice Regarding the Dispensing of Antibiotics without Prescription in Tanzania: An Explorative Cross-Sectional Study. Pharmacy, 8(4), 238. https://doi.org/10.3390/pharmacy8040238






