Women’s Beliefs on Early Adherence to Adjuvant Endocrine Therapy for Breast Cancer: A Theory-Based Qualitative Study to Guide the Development of Community Pharmacist Interventions
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Subjects
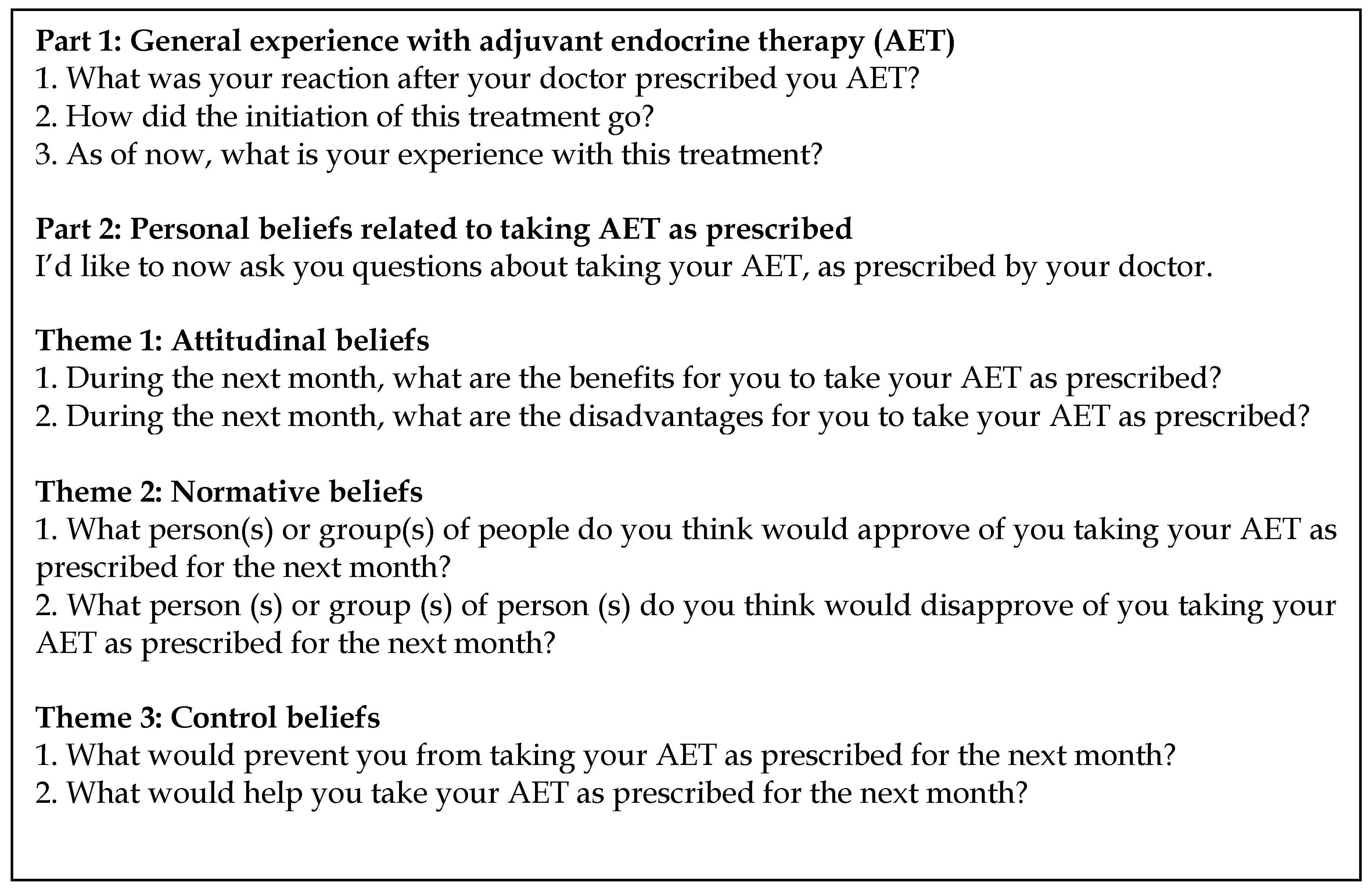
2.3. Data Collection
2.4. Analysis
2.5. Ethical Considerations
3. Results
3.1. Participants
3.2. Medication-Taking Behaviors
3.3. Attitudinal Beliefs
“The advantage they told me, was that it could save me. […] I saw this as prevention against a recurrence.”Individual Interview, Participant E.
“… All the effort made by everyone around us to support us. What’s taking a pill? We owe them that.”Focus Group 1, Participant C.
“If the hot flashes are to help me stay alive, then I’ll just turn down the heating system.”Focus Group 3, Participant Z.
“It’s like a trace of what we’ve experienced, like a passport that you always have on you.”Focus Group 4, Participant M.
3.4. Normative Beliefs
“Yes the doctor prescribed it to you, you trust him. It’s like chemo treatment. It’s preferable to not have it but you are told that you must.”Focus Group 3, Participant J.
“I had tons of questions and I wasn’t able ask them because she [oncologist] was, I felt that she was anxious, busy, it seemed as though I had to go quickly. So I was left with my questions.”Individual Interview, Participant K.
“I don’t talk because I’m not able to talk about it.”Individual Interview, Participant C.
“We were twelve and twice a day, morning group and evening [discussion] group, I received all the information from them because they had gone through it before me.”Focus Group 5, Participant S.
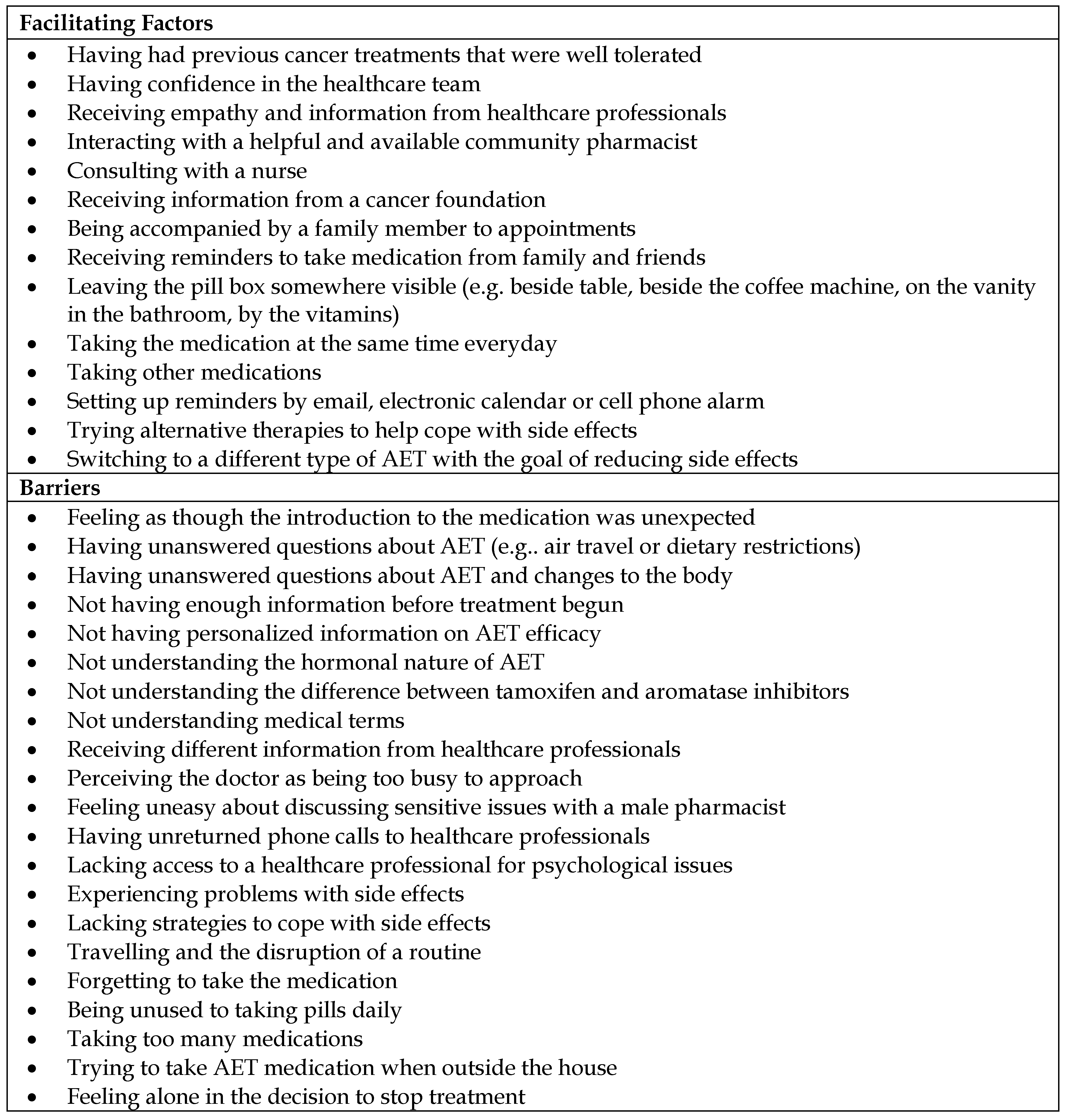
3.5. Control Beliefs
“I asked myself what do I do everyday of my life? At breakfast, my jar of peanut butter… Every morning, it is there.”Focus Group 3, Participant F.
“She [nurse navigator] said “well, we will try another molecule. Maybe that one will serve you better than the other.” […] For me, it was like a door had opened and there could be something else that is more comfortable for five years.”Individual Interview, Participant J.
“… the hot flashes. I would wake up during the night and be drenched. I skipped one month [of AET].”Focus Group 3, Participant F.
3.6. Additional Constructs
3.6.1. Perceived Risk
“It [AET] was strongly recommended because I was in a risky age group. I had just turned 40. And then, because my cancer was hormone sensitive and very reactive…”Individual Interview, Participant B.
3.6.2. Anticipated Regret
“If I don’t take it I feel a bit guilty. I mean to say that if my cancer comes back, I’ll say well there, you didn’t follow it.”Individual Interview, Participant H.
3.6.3. Moral Standards
“It is THE treatment, that’s it. I did not have anything else. I didn’t have any treatment besides this. So it was awful, but I was obligated.”Individual Interview, Participant C.
3.6.4. Self-Identity
“I have to say that I was never a person who is very pro-medication. I was very annoyed that I had to take it.”Individual Interview, Participant B.
4. Discussion
5. Conclusions
Reference
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Jatoi, I.; Chen, B.E.; Anderson, W.F.; Rosenberg, P.S. Breast cancer mortality trends in the united states according to estrogen receptor status and age at diagnosis. J. Clin. Oncol. 2007, 25, 1683–1690. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.J.; Neven, P.; Drijkoningen, M.; Paridaens, R.; Wildiers, H.; Van Limbergen, E.; Berteloot, P.; Amant, F.; Vergote, I.; Christiaens, M.R. Association between tumour characteristics and her-2/neu by immunohistochemistry in 1362 women with primary operable breast cancer. J. Clin. Pathol. 2005, 58, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Burstein, H.J.; Prestrud, A.A.; Seidenfeld, J.; Anderson, H.; Buchholz, T.A.; Davidson, N.E.; Gelmon, K.E.; Giordano, S.H.; Hudis, C.A.; Malin, J.; et al. American society of clinical oncology clinical practice guideline: Update on adjuvant endocrine therapy for women with hormone receptor-positive breast cancer. J. Clin. Oncol. 2010, 28, 3784–3796. [Google Scholar] [CrossRef] [PubMed]
- Burstein, H.J.; Temin, S.; Anderson, H.; Buchholz, T.A.; Davidson, N.E.; Gelmon, K.E.; Giordano, S.H.; Hudis, C.A.; Rowden, D.; Solky, A.J.; et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: American society of clinical oncology clinical practice guideline focused update. J. Clin. Oncol. 2014, 32, 2255–2269. [Google Scholar] [CrossRef] [PubMed]
- Gotay, C.; Dunn, J. Adherence to long-term adjuvant hormonal therapy for breast cancer. Expert Rev. Pharmacoecon. Outcomes Res. 2011, 11, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Chlebowski, R.T.; Geller, M.L. Adherence to endocrine therapy for breast cancer. Oncology 2006, 71, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Huiart, L.; Ferdynus, C.; Giorgi, R. A meta-regression analysis of the available data on adherence to adjuvant hormonal therapy in breast cancer: Summarizing the data for clinicians. Breast Cancer Res. Treat. 2013, 138, 325–328. [Google Scholar] [CrossRef] [PubMed]
- Murphy, C.C.; Bartholomew, L.K.; Carpentier, M.Y.; Bluethmann, S.M.; Vernon, S.W. Adherence to adjuvant hormonal therapy among breast cancer survivors in clinical practice: A systematic review. Breast Cancer Res. Treat. 2012, 134, 459–478. [Google Scholar] [CrossRef] [PubMed]
- Dunn, J.; Gotay, C. Adherence rates and correlates in long-term hormonal therapy. Vitam. Horm. 2013, 93, 353–375. [Google Scholar] [PubMed]
- Makubate, B.; Donnan, P.T.; Dewar, J.A.; Thompson, A.M.; McCowan, C. Cohort study of adherence to adjuvant endocrine therapy, breast cancer recurrence and mortality. Br. J. Cancer 2013, 108, 1515–1524. [Google Scholar] [CrossRef] [PubMed]
- Winn, A.N.; Dusetzina, S.B. The association between trajectories of endocrine therapy adherence and mortality among women with breast cancer. Pharmacoepidemiol. Drug Saf. 2016, 25, 953–959. [Google Scholar] [CrossRef] [PubMed]
- Yu, K.D.; Zhou, Y.; Liu, G.Y.; Li, B.; He, P.Q.; Zhang, H.W.; Lou, L.H.; Wang, X.J.; Wang, S.; Tang, J.H.; et al. A prospective, multicenter, controlled, observational study to evaluate the efficacy of a patient support program in improving patients’ persistence to adjuvant aromatase inhibitor medication for postmenopausal, early stage breast cancer. Breast Cancer Res. Treat. 2012, 134, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Ziller, V.; Kyvernitakis, I.; Knoll, D.; Storch, A.; Hars, O.; Hadji, P. Influence of a patient information program on adherence and persistence with an aromatase inhibitor in breast cancer treatment—the compas study. BMC Cancer 2013, 13, 407. [Google Scholar] [CrossRef] [PubMed]
- Neven, P.; Markopoulos, C.; Tanner, M.; Marty, M.; Kreienberg, R.; Atkins, L.; Franquet, A.; Gnant, M.; Neciosup, S.; Tesarova, P.; et al. The impact of educational materials on compliance and persistence rates with adjuvant aromatase inhibitor treatment: First-year results from the compliance of aromatase inhibitors assessment in daily practice through educational approach (cariatide) study. Breast 2014, 23, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Hadji, P.; Blettner, M.; Harbeck, N.; Jackisch, C.; Luck, H.J.; Windemuth-Kieselbach, C.; Zaun, S.; Kreienberg, R. The patient’s anastrozole compliance to therapy (pact) program: A randomized, in-practice study on the impact of a standardized information program on persistence and compliance to adjuvant endocrine therapy in postmenopausal women with early breast cancer. Ann. Oncol. 2013, 24, 1505–1512. [Google Scholar] [CrossRef] [PubMed]
- Markopoulos, C.; Neven, P.; Tanner, M.; Marty, M.; Kreienberg, R.; Atkins, L.; Franquet, A.; Gnant, M.; Neciosup, S.; Tesarova, P.; et al. Does patient education work in breast cancer? Final results from the global cariatide study. Future Oncol. 2015, 11, 205–217. [Google Scholar] [CrossRef] [PubMed]
- Wagner, V.L.; Jing, W.; Boscoe, F.P.; Schymura, M.J.; Roohan, P.J.; Gesten, F.C. Improving adjuvant hormone therapy use in medicaid managed care-insured women, new york state, 2012–2014. Prev. Chronic Dis. 2016, 13, E120. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Abraham, C. Interventions to change health behaviours: Evidence-based or evidence-inspired? Psychol. Health 2004, 19, 29–49. [Google Scholar] [CrossRef]
- Ekinci, E.; Nathoo, S.; Korattyil, T.; Vadhariya, A.; Zaghloul, H.A.; Niravath, P.A.; Abughosh, S.M.; Trivedi, M.V. Interventions to improve endocrine therapy adherence in breast cancer survivors: What is the evidence? J. Cancer Surviv. 2018, 12, 348–356. [Google Scholar] [CrossRef] [PubMed]
- Pellegrini, I.; Sarradon-Eck, A.; Soussan, P.B.; Lacour, A.C.; Largillier, R.; Tallet, A.; Tarpin, C.; Julian-Reynier, C. Women’s perceptions and experience of adjuvant tamoxifen therapy account for their adherence: Breast cancer patients’ point of view. Psycho Oncol. 2010, 19, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Harrow, A.; Dryden, R.; McCowan, C.; Radley, A.; Parsons, M.; Thompson, A.M.; Wells, M. A hard pill to swallow: A qualitative study of women’s experiences of adjuvant endocrine therapy for breast cancer. BMJ Open 2014, 4. [Google Scholar] [CrossRef] [PubMed]
- Verbrugghe, M.; Verhaeghe, S.; Decoene, E.; De Baere, S.; Vandendorpe, B.; Van Hecke, A. Factors influencing the process of medication (non-)adherence and (non-)persistence in breast cancer patients with adjuvant antihormonal therapy: A qualitative study. Eur. J. Cancer Care 2017, 26, e12339. [Google Scholar] [CrossRef] [PubMed]
- Wells, K.J.; Pan, T.M.; Vazquez-Otero, C.; Ung, D.; Ustjanauskas, A.E.; Munoz, D.; Laronga, C.; Roetzheim, R.G.; Goldenstein, M.; Carrizosa, C.; et al. Barriers and facilitators to endocrine therapy adherence among underserved hormone-receptor-positive breast cancer survivors: A qualitative study. Support. Care Cancer 2016, 24, 4123–4130. [Google Scholar] [CrossRef] [PubMed]
- Van Londen, G.J.; Donovan, H.S.; Beckjord, E.B.; Cardy, A.L.; Bovbjerg, D.H.; Davidson, N.E.; Morse, J.Q.; Switzer, G.E.; Verdonck-de Leeuw, I.M.; Dew, M.A. Perspectives of postmenopausal breast cancer survivors on adjuvant endocrine therapy-related symptoms. Oncol. Nurs. Forum 2014, 41, 660–668. [Google Scholar] [CrossRef] [PubMed]
- Iacorossi, L.; Gambalunga, F.; Fabi, A.; Giannarelli, D.; Marchetti, A.; Piredda, M.; De Marinis, M.G. Adherence to oral administration of endocrine treatment in patients with breast cancer: A qualitative study. Cancer Nurs. 2018, 41, E57–E63. [Google Scholar] [CrossRef] [PubMed]
- Wickersham, K.; Happ, M.B.; Bender, C.M. Keeping the boogie man away: Medication self-management among women receiving anastrozole therapy. Nurs. Res. Pract. 2012, 2012, 9. [Google Scholar] [CrossRef] [PubMed]
- Wouters, H.; van Geffen, E.C.G.; Baas-Thijssen, M.C.; Krol-Warmerdam, E.M.; Stiggelbout, A.M.; Belitser, S.; Bouvy, M.L.; van Dijk, L. Disentangling breast cancer patients’ perceptions and experiences with regard to endocrine therapy: Nature and relevance for non-adherence. Breast 2013, 22, 661–666. [Google Scholar] [CrossRef] [PubMed]
- Cahir, C.; Dombrowski, S.U.; Kelly, C.M.; Kennedy, M.J.; Bennett, K.; Sharp, L. Women’s experiences of hormonal therapy for breast cancer: Exploring influences on medication-taking behaviour. Support. Care Cancer 2015, 23, 3115–3130. [Google Scholar] [CrossRef] [PubMed]
- Brauer, E.R.; Ganz, P.A.; Pieters, H.C. “Winging it“: How older breast cancer survivors persist with aromatase inhibitor treatment. J. Oncol. Pract. 2016, 12, e991–e1000. [Google Scholar] [CrossRef] [PubMed]
- Lambert, L.K.; Balneaves, L.G.; Howard, A.F.; Gotay, C.C. Patient-reported factors associated with adherence to adjuvant endocrine therapy after breast cancer: An integrative review. Breast Cancer Res. Treat. 2018, 167, 615–633. [Google Scholar] [CrossRef] [PubMed]
- Van der Laan, D.M.; Elders, P.J.M.; Boons, C.; Beckeringh, J.J.; Nijpels, G.; Hugtenburg, J.G. Factors associated with antihypertensive medication non-adherence: A systematic review. J. Hum. Hypertens. 2017, 31, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Capoccia, K.; Odegard, P.S.; Letassy, N. Medication adherence with diabetes medication: A systematic review of the literature. Diabetes Educ. 2016, 42, 34–71. [Google Scholar] [CrossRef] [PubMed]
- Cane, J.; O’Connor, D.; Michie, S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement. Sci. 2012, 7. [Google Scholar] [CrossRef] [PubMed]
- Eldredge, L.K.B.; Markham, C.M.; Ruiter, R.A.C.; Kok, G.; Parcel, G.S. Planning Health Promotion Programs: An Intervention Mapping Approach; Wiley: Hoboken, NJ, USA, 2016. [Google Scholar]
- Michie, S.; Atkins, L.; West, R. The Behaviour Change Wheel: A Guide to Designing Interventions; Silverback: Stuttgart, Germany, 2014. [Google Scholar]
- Godin, G.; Kok, G. The theory of planned behavior: A review of its applications to health-related behaviors. AJHP 1996, 11, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Armitage, C.J.; Conner, M. Efficacy of the theory of planned behaviour: A meta-analytic review. Br. J. Soc. Psychol. 2001, 40, 471–499. [Google Scholar] [CrossRef] [PubMed]
- Rich, A.; Brandes, K.; Mullan, B.; Hagger, M.S. Theory of planned behavior and adherence in chronic illness: A meta-analysis. J. Behav. Med. 2015, 38, 673–688. [Google Scholar] [CrossRef] [PubMed]
- Zoellner, J.; Krzeski, E.; Harden, S.; Cook, E.; Allen, K.; Estabrooks, P.A. Qualitative application of the theory of planned behavior to understand beverage behaviors among adults. J. Acad. Nutr. Diet. 2012, 112, 1774–1784. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Krueger, R.A.; Casey, M.A. Focus Groups: A Practical Guide for Applied Research; SAGE Publications: Thousand Oaks, CA, USA, 2014. [Google Scholar]
- Green, J.; Thorogood, N. Qualitative Methods for Health Research; SAGE Publications: Thousand Oaks, CA, USA, 2013. [Google Scholar]
- Miles, M.B.; Huberman, A.M.; Saldana, J. Qualitative Data Analysis; SAGE Publications: Thousand Oaks, CA, USA, 2013. [Google Scholar]
- Saldana, J. The Coding Manual for Qualitative Researchers; SAGE Publications: Thousand Oaks, CA, USA, 2012. [Google Scholar]
- Paillé, P.; Mucchielli, A. L’analyse Qualitative en Sciences Humaines et Sociales; Armand Colin: Paris, French, 2012; p. 424. [Google Scholar]
- Rosenstock, I.M.; Strecher, V.J.; Becker, M.H. Social learning theory and the health belief model. Health Educ. Quart. 1988, 15, 175–183. [Google Scholar] [CrossRef]
- Sheeran, P.; Orbell, S. Augmenting the theory of planned behavior: Roles for anticipated regret and descriptive norms. J. Appl. Soc. Psychol. 1999, 29, 2107–2142. [Google Scholar] [CrossRef]
- Godin, G. Les Comportements Dans le Domaine de la Santé; Presses de l’Université de Montréal: Montréal, QC, Canada, 2013. [Google Scholar]
- Conner, M.; Armitage, C.J. Extending the theory of planned behavior: A review and avenues for further research. J. Appl. Soc. Psychol. 1998, 28, 1429–1464. [Google Scholar] [CrossRef]
- Chlebowski, R.T.; Kim, J.; Haque, R. Adherence to endocrine therapy in breast cancer adjuvant and prevention settings. Cancer Prev. Res. 2014, 7, 378–387. [Google Scholar] [CrossRef] [PubMed]
- Van Liew, J.R.; Christensen, A.J.; de Moor, J.S. Psychosocial factors in adjuvant hormone therapy for breast cancer: An emerging context for adherence research. J. Cancer Surviv. 2014, 8, 521–531. [Google Scholar] [CrossRef] [PubMed]
- Heisig, S.R.; Shedden-Mora, M.C.; von Blanckenburg, P.; Schuricht, F.; Rief, W.; Albert, U.S.; Nestoriuc, Y. Informing women with breast cancer about endocrine therapy: Effects on knowledge and adherence. Psycho Oncol. 2015, 24, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Horne rR Concordance, Adherence and Compliance in Medicine Taking. In National Co-Ordinating Centre for NHS Service Delivery and Organisation r, 2005. Available online: http://www.netscc.ac.uk/hsdr/files/project/SDO_FR_08-1412-076_V01.pdf (accessed on 6 June 2018).
- Abbott, R.; Edwards, S.; Whelan, M.; Edwards, J.; Dranitsaris, G. Are community pharmacists equipped to ensure the safe use of oral anticancer therapy in the community setting? Results of a cross-country survey of community pharmacists in canada. J. Oncol. Pharm. Pract. 2014, 20, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Kennelty, K.A.; Chewning, B.; Wise, M.; Kind, A.; Roberts, T.; Kreling, D. Barriers and facilitators of medication reconciliation processes for recently discharged patients from community pharmacists’ perspectives. RSAP 2015, 11, 517–530. [Google Scholar] [CrossRef] [PubMed]
- Laliberte, M.C.; Perreault, S.; Damestoy, N.; Lalonde, L. Ideal and actual involvement of community pharmacists in health promotion and prevention: A cross-sectional study in Quebec, Canada. BMC Public Health 2012, 12, 192. [Google Scholar] [CrossRef] [PubMed]
- Lea, V.M.; Corlett, S.A.; Rodgers, R.M. Workload and its impact on community pharmacists’ job satisfaction and stress: A review of the literature. Int. J. Pharm. Pract. 2012, 20, 259–271. [Google Scholar] [CrossRef] [PubMed]
- Bharadia, R.; Lorenz, K.; Cor, K.; Simpson, S.H. Financial remuneration is positively correlated with the number of clinical activities: An example from diabetes management in alberta community pharmacies. Int. J. Pharm. Pract. 2018, 26, 77–80. [Google Scholar] [CrossRef] [PubMed]
- Guillaumie, L.; Moisan, J.; Grégoire, J.P.; Villeneuve, D.; Beaucage, C.; Bujold, M.; Lauzier, S. Perspective of community pharmacists on their practice with patients who have an antidepressant drug treatment: Findings from a focus group study. Res. Social. Adm. Pharm. 2015, 11, e43–e56. [Google Scholar] [CrossRef] [PubMed]
| Focus Groups | Individual Interviews | Total | |
|---|---|---|---|
| (n = 34) | (n = 9) | (n = 43) | |
| Age (years) | |||
| ≤49 | 5 | 1 | 6 |
| 50–59 | 13 | 4 | 17 |
| 60–69 | 8 | 2 | 10 |
| ≥70 | 8 | 2 | 10 |
| Level of education | |||
| Primary school | 1 | 1 | 2 |
| Secondary school | 7 | 1 | 8 |
| College | 11 | 3 | 14 |
| University | 15 | 4 | 19 |
| Time since breast cancer diagnosis (months) 1 | |||
| mean (range) | 16.5 (5–30) | 20.3 (6–32) | 17.3 (5–32) |
| Breast surgery | |||
| Yes | 34 | 9 | 43 |
| No | 0 | 0 | 0 |
| Other breast cancer treatments received | |||
| Chemotherapy | 14 | 4 | 18 |
| Radiotherapy | 32 | 6 | 38 |
| Trastuzumab | 5 | 1 | 6 |
| Number of adjuvant treatments received in addition to AET 1 | |||
| 0 | 2 | 3 | 5 |
| 1 | 18 | 2 | 20 |
| 2 | 10 | 2 | 12 |
| 3 | 4 | 1 | 5 |
| Adjuvant endocrine treatment prescribed at time of the study | |||
| Tamoxifen | 14 | 5 | 19 |
| Letrozole | 2 | 1 | 3 |
| Anastrozole | 18 | 3 | 21 |
| Exemestane | 0 | 0 | 0 |
| Time since first AET prescription (months) | |||
| mean (range) | 10.9 (2–21) | 12.6 (2–24) | 11.2 (2–24) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Humphries, B.; Collins, S.; Guillaumie, L.; Lemieux, J.; Dionne, A.; Provencher, L.; Moisan, J.; Lauzier, S. Women’s Beliefs on Early Adherence to Adjuvant Endocrine Therapy for Breast Cancer: A Theory-Based Qualitative Study to Guide the Development of Community Pharmacist Interventions. Pharmacy 2018, 6, 53. https://doi.org/10.3390/pharmacy6020053
Humphries B, Collins S, Guillaumie L, Lemieux J, Dionne A, Provencher L, Moisan J, Lauzier S. Women’s Beliefs on Early Adherence to Adjuvant Endocrine Therapy for Breast Cancer: A Theory-Based Qualitative Study to Guide the Development of Community Pharmacist Interventions. Pharmacy. 2018; 6(2):53. https://doi.org/10.3390/pharmacy6020053
Chicago/Turabian StyleHumphries, Brittany, Stéphanie Collins, Laurence Guillaumie, Julie Lemieux, Anne Dionne, Louise Provencher, Jocelyne Moisan, and Sophie Lauzier. 2018. "Women’s Beliefs on Early Adherence to Adjuvant Endocrine Therapy for Breast Cancer: A Theory-Based Qualitative Study to Guide the Development of Community Pharmacist Interventions" Pharmacy 6, no. 2: 53. https://doi.org/10.3390/pharmacy6020053
APA StyleHumphries, B., Collins, S., Guillaumie, L., Lemieux, J., Dionne, A., Provencher, L., Moisan, J., & Lauzier, S. (2018). Women’s Beliefs on Early Adherence to Adjuvant Endocrine Therapy for Breast Cancer: A Theory-Based Qualitative Study to Guide the Development of Community Pharmacist Interventions. Pharmacy, 6(2), 53. https://doi.org/10.3390/pharmacy6020053





