The Role of Individual and Small-Area Social and Environmental Factors on Heat Vulnerability to Mortality Within and Outside of the Home in Boston, MA
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Case-Only Analysis
3.1.1. Deaths at Home
3.1.2. Deaths Outside of the Home
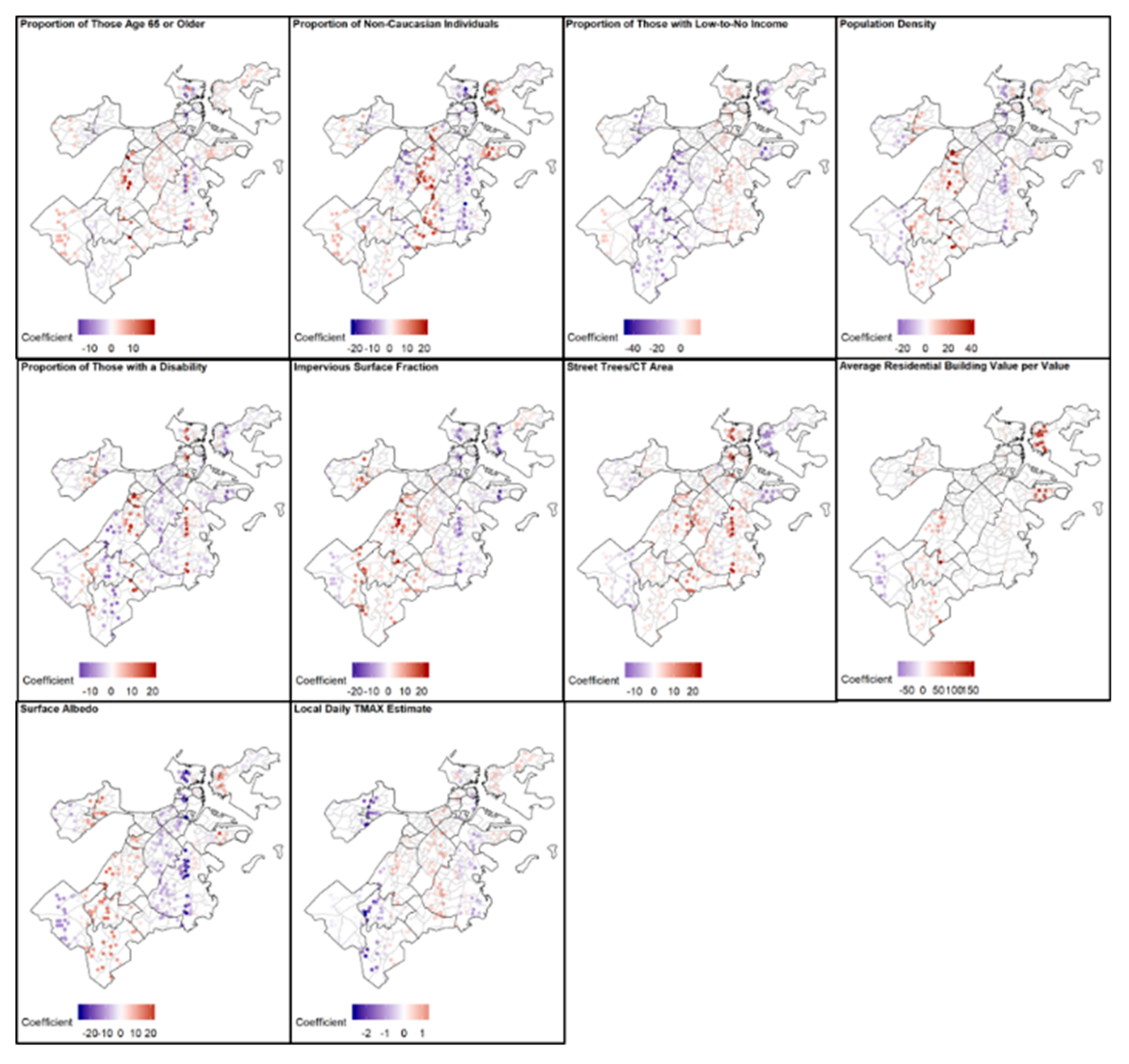
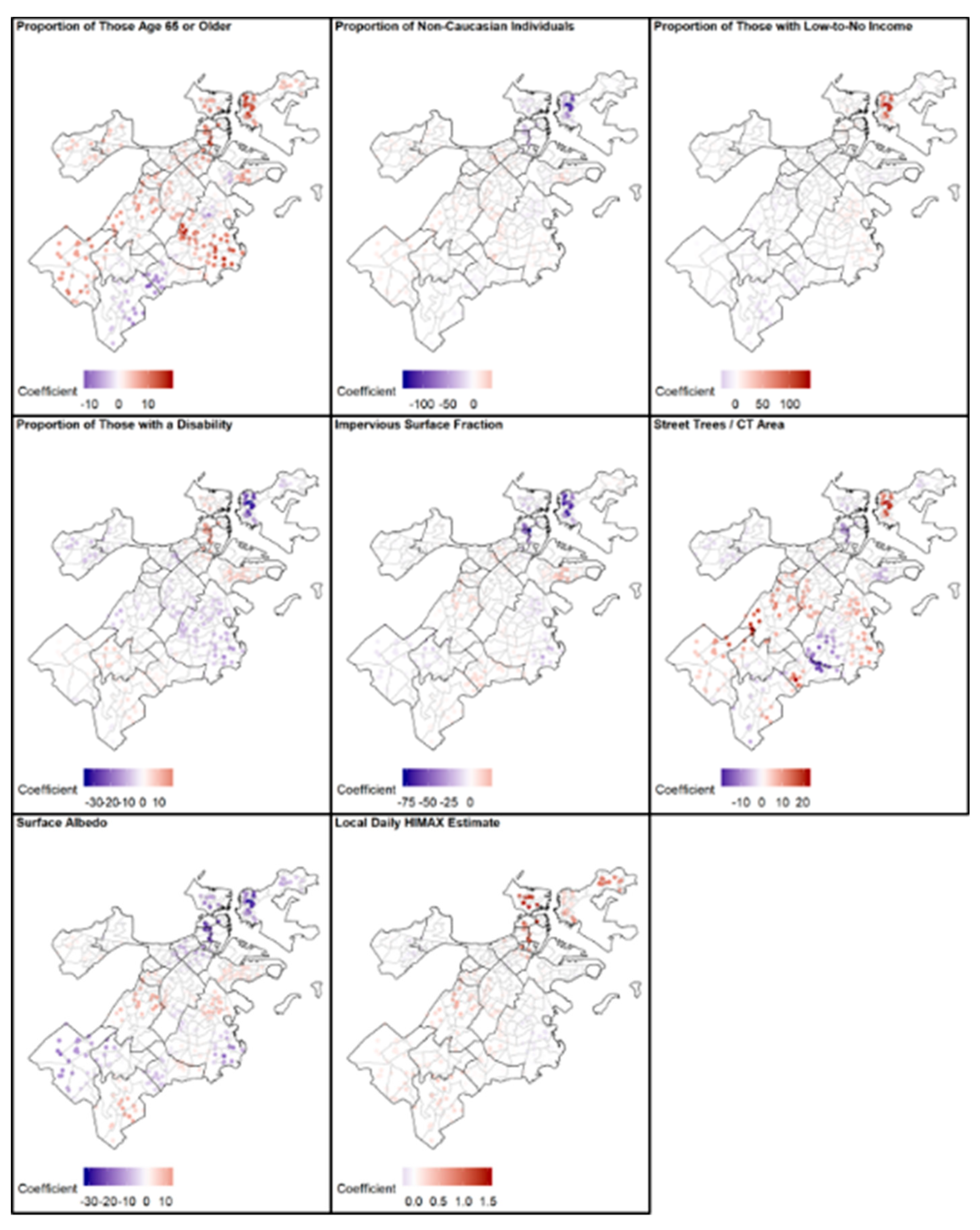
3.2. Geographic Weighted Regression
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- IPCC. 2018: Summary for Policymakers. In Global Warming of 1.5 °C; An IPCC Special Report on the Impacts of Global Warming of 1.5 °C above Pre-Industrial Levels and Related Global Greenhouse Gas Emission Pathways, in the Context of Strengthening the Global Response to the Threat of Climate Change, Sustainable Development, and Efforts to Eradicate Poverty; World Meteorological Organization: Geneva, Switzerland, 2018; pp. 1–32. [Google Scholar]
- Reidmiller, D.R.; Avery, C.W.; Easterling, D.R.; Kunkel, K.E.; Lewis, K.L.M.; Maycock, T.K.; Stewart, B.C. Fourth National Climate Assessment. Volume II: Impacts, Risks, and Adaptation in the United States, Report-in-Brief; U.S. Global Change Research Program: Washington, DC, USA, 2018.
- Zhang, K.; Chen, Y.-H.; Schwartz, J.D.; Rood, R.B.; O’Neill, M.S. Using Forecast and Observed Weather Data to Assess Performance of Forecast Products in Identifying Heat Waves and Estimating Heat Wave Effects on Mortality. Environ. Health Perspect. 2014, 122, 912–918. [Google Scholar] [CrossRef] [PubMed]
- Basu, R. High ambient temperature and mortality: A review of epidemiologic studies from 2001 to 2008. Environ. Health 2009, 8, 13. [Google Scholar] [CrossRef] [PubMed]
- Medina-Ramón, M.; Zanobetti, A.; Cavanagh, D.P.; Schwartz, J. Extreme Temperatures and Mortality: Assessing Effect Modification by Personal Characteristics and Specific Cause of Death in a Multi-City Case-Only Analysis. Environ. Health Perspect. 2006, 114, 1331–1336. [Google Scholar] [CrossRef]
- Son, J.-Y.; Liu, J.C.; Bell, M.L. Temperature-related mortality: A systematic review and investigation of effect modifiers. Environ. Res. Lett. 2019, 14, 073004. [Google Scholar] [CrossRef]
- Zanobetti, A.; Schwartz, J. Temperature and Mortality in Nine US Cities. Epidemiology 2008, 19, 563–570. [Google Scholar] [CrossRef] [PubMed]
- Saha, M.V.; Davis, R.E.; Hondula, D.M. Mortality Displacement as a Function of Heat Event Strength in 7 US Cities. Am. J. Epidemiol. 2014, 179, 467–474. [Google Scholar] [CrossRef]
- Gosling, S.N.; McGregor, G.R.; Páldy, A. Climate change and heat-related mortality in six cities Part 1: Model construction and validation. Int. J. Biometeorol. 2007, 51, 525–540. [Google Scholar] [CrossRef]
- Gosling, S.N.; McGregor, G.R.; Lowe, J.A. Climate change and heat-related mortality in six cities Part 2: Climate model evaluation and projected impacts from changes in the mean and variability of temperature with climate change. Int. J. Biometeorol. 2009, 53, 31–51. [Google Scholar] [CrossRef]
- Curriero, F.C. Temperature and Mortality in 11 Cities of the Eastern United States. Am. J. Epidemiol. 2002, 155, 80–87. [Google Scholar] [CrossRef]
- The City of Boston and the Green Ribbon Commission. Climate Ready Boston; The City of Boston and the Green Ribbon Commission: Boston, MA, USA, 2016; pp. 1–199. [Google Scholar]
- Petkova, E.; Horton, R.; Bader, D.; Kinney, P. Projected Heat-Related Mortality in the U.S. Urban Northeast. Int. J. Environ. Res. Public Health 2013, 10, 6734–6747. [Google Scholar] [CrossRef]
- Reid, C.E.; Mann, J.K.; Alfasso, R.; English, P.B.; King, G.C.; Lincoln, R.A.; Margolis, H.G.; Rubado, D.J.; Sabato, J.E.; West, N.L.; et al. Evaluation of a Heat Vulnerability Index on Abnormally Hot Days: An Environmental Public Health Tracking Study. Environ. Health Perspect. 2012, 120, 715–720. [Google Scholar] [CrossRef] [PubMed]
- Reid, C.E.; O’Neill, M.S.; Gronlund, C.J.; Brines, S.J.; Brown, D.G.; Diez-Roux, A.V.; Schwartz, J. Mapping Community Determinants of Heat Vulnerability. Environ. Health Perspect. 2009, 117, 1730–1736. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.-J.; Kim, H. Effect modification of individual- and regional-scale characteristics on heat wave-related mortality rates between 2009 and 2012 in Seoul, South Korea. Sci. Total Environ. 2017, 595, 141–148. [Google Scholar] [CrossRef]
- Anderson, M.; Carmichael, C.; Murray, V.; Dengel, A.; Swainson, M. Defining indoor heat thresholds for health in the UK. Perspect. Public Health 2013, 133, 158–164. [Google Scholar] [CrossRef]
- Baniassadi, A.; Heusinger, J.; Sailor, D.J. Energy efficiency vs resiliency to extreme heat and power outages: The role of evolving building energy codes. Build. Environ. 2018, 139, 86–94. [Google Scholar] [CrossRef]
- Sailor, D.J.; Baniassadi, A.; O’Lenick, C.R.; Wilhelmi, O.V. The growing threat of heat disasters. Environ. Res. Lett. 2019, 14, 054006. [Google Scholar] [CrossRef]
- Baniassadi, A.; Sailor, D.J.; Krayenhoff, E.S.; Broadbent, A.M.; Georgescu, M. Passive survivability of buildings under changing urban climates across eight US cities. Environ. Res. Lett. 2019, 14, 074028. [Google Scholar] [CrossRef]
- Semenza, J.C.; Rubin, C.H.; Falter, K.H.; Selanikio, J.D.; Flanders, W.D.; Howe, H.L.; Wilhelm, J.L. Heat-Related Deaths during the July 1995 Heat Wave in Chicago. N. Engl. J. Med. 1996, 335, 84–90. [Google Scholar] [CrossRef]
- Smargiassi, A.; Fournier, M.; Griot, C.; Baudouin, Y.; Kosatsky, T. Prediction of the indoor temperatures of an urban area with an in-time regression mapping approach. J. Expo. Sci. Environ. Epidemiol. 2008, 18, 282–288. [Google Scholar] [CrossRef]
- Quinn, A.; Tamerius, J.D.; Perzanowski, M.; Jacobson, J.S.; Goldstein, I.; Acosta, L.; Shaman, J. Predicting indoor heat exposure risk during extreme heat events. Sci. Total Environ. 2014, 490, 686–693. [Google Scholar] [CrossRef]
- Holmes, S.H.; Phillips, T.; Wilson, A. Overheating and passive habitability: Indoor health and heat indices. Build. Res. Inf. 2016, 44, 1–19. [Google Scholar] [CrossRef]
- McDonald, R.I.; Kroeger, T.; Zhang, P.; Hamel, P. The Value of US Urban Tree Cover for Reducing Heat-Related Health Impacts and Electricity Consumption. Ecosystems 2019, 23, 137–150. [Google Scholar] [CrossRef]
- Madrigano, J.; Ito, K.; Johnson, S.; Kinney, P.L.; Matte, T. A Case-Only Study of Vulnerability to Heat Wave–RelatedMortality in New York City (2000–2011). Environ. Health Perspect. 2015, 123, 672–678. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, S. Without AC, Public Housing Residents Swelter Through the Summer. WNYC News, 2016. [Google Scholar]
- Energy Information Administration. Household Energy Use in Massachusetts: A Closer Look at Residential Energy Consumption; Energy Information Administration: Washington, DC, USA, 2009; p. 2. Available online: www.eia.gov/consumption/residential/reports/2009/state_briefs/pdf/ma.pdf (accessed on 6 February 2020).
- Abel, D.; Holloway, T.; Kladar, R.M.; Meier, P.; Ahl, D.; Harkey, M.; Patz, J. Response of Power Plant Emissions to Ambient Temperature in the Eastern United States. Environ. Sci. Technol. 2017, 51, 5838–5846. [Google Scholar] [CrossRef] [PubMed]
- Chuang, W.-C.; Gober, P. Predicting Hospitalization for Heat-Related Illness at the Census-Tract Level: Accuracy of a Generic Heat Vulnerability Index in Phoenix, Arizona (USA). Environ. Health Perspect. 2015, 123, 606–612. [Google Scholar] [CrossRef] [PubMed]
- Coutts, E.; Ito, K.; Nardi, C.; Vuong, T. Planning Urban Heat Island Mitigation in Boston; Trust for Public Land: Boston, MA, USA, 2015; p. 3. Available online: https://www.tpl.org/sites/default/files/UHI_Tufts_Executive%20Summary.pdf (accessed on 6 February 2020).
- Kingsley, S.L.; Eliot, M.N.; Gold, J.; Vanderslice, R.R.; Wellenius, G.A. Current and Projected Heat-Related Morbidity and Mortality in Rhode Island. Environ. Health Perspect. 2016, 124, 460–467. [Google Scholar] [CrossRef]
- National Weather Service. NWS Heat Index. Available online: https://www.weather.gov/safety/heat-index (accessed on 6 February 2020).
- Anderson, G.B.; Bell, M.L. Heat Waves in the United States: Mortality Risk during Heat Waves and Effect Modification by Heat Wave Characteristics in 43 U.S. Communities. Environ. Health Perspect. 2010, 119, 210–218. [Google Scholar] [CrossRef]
- Braga, A.L.F.; Zanobetti, A.; Schwartz, J. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ. Health Perspect. 2002, 110, 859–863. [Google Scholar] [CrossRef]
- Wellenius, G.A.; Eliot, M.N.; Bush, K.F.; Holt, D.; Lincoln, R.A.; Smith, A.E.; Gold, J. Heat-related morbidity and mortality in New England: Evidence for local policy. Environ. Res. 2017, 156, 845–853. [Google Scholar] [CrossRef]
- Iceland, J.; Steinmetz, E. The Effects of Using Census Block Groups Instead of Census Tracts When Examining Residential Housing Patterns; Bureau of the Census: Suitland-Silver Hill, MD, USA, 2003.
- Subramanian, S.V.; Chen, J.T.; Rehkopf, D.H.; Waterman, P.D.; Krieger, N. Comparing Individual- and Area-based Socioeconomic Measures for the Surveillance of Health Disparities: A Multilevel Analysis of Massachusetts Births, 1989–1991. Am. J. Epidemiol. 2006, 164, 823–834. [Google Scholar] [CrossRef]
- United States Census. 2010. Available online: https://www.factfinder.census.gov/faces/nav/jsf/pages/index.xhtml (accessed on 6 February 2020).
- Climate Ready Boston Social Vulnerability. 2017. Available online: https://www.data.boston.gov/dataset/climate-ready-boston-social-vulnerability (accessed on 6 February 2020).
- Trees. 2019. Available online: https://www.bostonopendata-boston.opendata.arcgis.com/datasets/ce863d38db284efe83555caf8a832e2a_1 (accessed on 6 February 2020).
- Impervious Surface Fraction—Census Tracts. 2013. Available online: https://www.worldmap.harvard.edu/data/geonode:impervious_surface_fraction_census_tract_5yd (accessed on 6 February 2020).
- Shields, M.; O’Brien, D.; de Benedictis-Kessner, J. Property Assessment 2018.
- Song, X.; Wang, S.; Hu, Y.; Yue, M.; Zhang, T.; Liu, Y.; Tian, J.; Shang, K. Impact of ambient temperature on morbidity and mortality: An overview of reviews. Sci. Total Environ. 2017, 586, 241–254. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Luo, M.; Walker, R.J.; Liu, X.; Hwang, S.-A.; Chinery, R. Extreme High Temperatures and Hospital Admissions for Respiratory and Cardiovascular Diseases. Epidemiology 2009, 20, 738–746. [Google Scholar] [CrossRef] [PubMed]
- Mastrangelo, G.; Fedeli, U.; Visentin, C.; Milan, G.; Fadda, E.; Spolaore, P. Pattern and determinants of hospitalization during heat waves: An ecologic study. BMC Public Health 2007, 7, 200. [Google Scholar] [CrossRef] [PubMed]
- Gronlund, C.J.; Zanobetti, A.; Schwartz, J.D.; Wellenius, G.A.; O’Neill, M.S. Heat, Heat Waves, and Hospital Admissions among the Elderly in the United States, 1992–2006. Environ. Health Perspect. 2014, 122, 1187–1192. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.-C.; Lin, Y.-K. Association between Temperature and Emergency Room Visits for Cardiorespiratory Diseases, Metabolic Syndrome-Related Diseases, and Accidents in Metropolitan Taipei. PLoS ONE 2014, 9, e99599. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hajat, S.; Haines, A.; Sarran, C.; Sharma, A.; Bates, C.; Fleming, L.E. The effect of ambient temperature on type-2-diabetes: Case-crossover analysis of 4+ million GP consultations across England. Environ. Health 2017, 16, 73. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.; Weinberger, K.R.; Spangler, K.R.; Eliot, M.N.; Braun, J.M.; Wellenius, G.A. Ambient temperature and preterm birth: A retrospective study of 32 million US singleton births. Environ. Int. 2019, 126, 7–13. [Google Scholar] [CrossRef]
- Lin, S.; Sun, M.; Fitzgerald, E.; Hwang, S.-A. Did summer weather factors affect gastrointestinal infection hospitalizations in New York State? Sci. Total Environ. 2016, 550, 38–44. [Google Scholar] [CrossRef]
- Khoury, M.J.; Flanders, W.D. Nontraditional Epidemiologic Approaches in the Analysis of Gene Environment Interaction: Case-Control Studies with No Controls! Am. J. Epidemiol. 1996, 144, 207–213. [Google Scholar] [CrossRef]
- Armstrong, B.G. Fixed Factors that Modify the Effects of Time-Varying Factors: Applying the Case-Only Approach. Epidemiology 2003, 14, 467–472. [Google Scholar] [CrossRef]
- Zanobetti, A.; O’Neill, M.S.; Gronlund, C.J.; Schwartz, J.D. Susceptibility to Mortality in Weather Extremes: Effect Modification by Personal and Small-Area Characteristics. Epidemiology 2013, 24, 809–819. [Google Scholar] [CrossRef]
- Daly, C.; Gibson, W.; Taylor, G.; Johnson, G.; Pasteris, P. A knowledge-based approach to the statistical mapping of climate. Clim. Res. 2002, 22, 99–113. [Google Scholar] [CrossRef]
- PRISM Climate Group, Oregon State University. Parameter-Elevation Regressions on Independent Slopes Model (PRISM); PRISM Climate Group, Oregon State University: Corvallis, OR, USA, 2018. [Google Scholar]
- Daly, C.; Smith, J.W.; Smith, J.I.; McKane, R.B. High-Resolution Spatial Modeling of Daily Weather Elements for a Catchment in the Oregon Cascade Mountains, United States. J. Appl. Meteorol. Climatol. 2007, 46, 1565–1586. [Google Scholar] [CrossRef]
- Spangler, K.R.; Weinberger, K.R.; Wellenius, G.A. Suitability of gridded climate datasets for use in environmental epidemiology. J. Expo. Sci. Environ. Epidemiol. 2019, 29, 777–789. [Google Scholar] [CrossRef] [PubMed]
- Weinberger, K.R.; Spangler, K.R.; Zanobetti, A.; Schwartz, J.D.; Wellenius, G.A. Comparison of temperature-mortality associations estimated with different exposure metrics. Environ. Epidemiol. 2019, 3, e072. [Google Scholar] [CrossRef]
- Triple Decker Trends; Department of Neighborhood Development Research & Development Unit: Boston, MA, USA, 1999; p. 4.
- MacFadden, D.R.; McGough, S.F.; Fisman, D.; Santillana, M.; Brownstein, J.S. Antibiotic resistance increases with local temperature. Nat. Clim. Chang. 2018, 8, 510–514. [Google Scholar] [CrossRef]
- Anderson, C.A. Temperature and Aggression: Ubiquitous Effects of Heat on Occurrence of Human Violence. Psychol. Bull. 1989, 106, 74. [Google Scholar] [CrossRef]
- Butke, P.; Sheridan, S.C. An Analysis of the Relationship between Weather and Aggressive Crime in Cleveland, Ohio. Weather Clim. Soc. 2010, 2, 127–139. [Google Scholar] [CrossRef]
- Anderson, C.A. Heat and Violence. Curr. Dir. Psychol. Sci. 2001, 10, 33–38. [Google Scholar] [CrossRef]
- Michel, S.J.; Wang, H.; Selvarajah, S.; Canner, J.K.; Murrill, M.; Chi, A.; Efron, D.T.; Schneider, E.B. Investigating the relationship between weather and violence in Baltimore, Maryland, USA. Injury 2016, 47, 272–276. [Google Scholar] [CrossRef]
- Williams, A.A.; Allen, J.G.; Catalano, P.J.; Buonocore, J.J.; Spengler, J.D. The influence of heat on emergency services in Boston, MA: Relative risk and time-series analyses of police, medical, and fire dispatches. Am. J. Public Health 2020. In Press. [Google Scholar]
- Obradovich, N.; Tingley, D.; Rahwan, I. Effects of environmental stressors on daily governance. Proc. Natl. Acad. Sci. USA 2018, 115, 8710–8715. [Google Scholar] [CrossRef]
- Page, L.A.; Hajat, S.; Kovats, R.S.; Howard, L.M. Temperature-related deaths in people with psychosis, dementia and substance misuse. Br. J. Psychiatry 2012, 200, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Simning, A.; van Wijngaarden, E.; Conwell, Y. Anxiety, mood, and substance use disorders in United States African-American public housing residents. Soc. Psychiatry Psychiatr. Epidemiol. 2011, 46, 983–992. [Google Scholar] [CrossRef] [PubMed]
- Barbato, J. Areal parameters of the Sea Breeze and its vertical structure in the Boston Basin. BAMS 1978, 59, 1420–1431. [Google Scholar] [CrossRef]
- Lue, S.-H.; Wellenius, G.A.; Wilker, E.H.; Mostofsky, E.; Mittleman, M.A. Residential proximity to major roadways and renal function. J. Epidemiol. Community Health 2008, 67, 629–634. [Google Scholar]
- Tillson, A.-A.; Oreszczyn, T.; Palmer, J. Assessing impacts of summertime overheating: Some adaptation strategies. Build. Res. Inf. 2013, 41, 652–661. [Google Scholar] [CrossRef]
- Krieger, J.; Higgins, D.L. Housing and Health: Time Again for Public Health Action. Am. J. Public Health 2002, 92, 758–768. [Google Scholar] [CrossRef]
- Ho, H.C.; Knudby, A.; Chi, G.; Aminipouri, M.; Lai, D.Y.-F. Spatiotemporal analysis of regional socio-economic vulnerability change associated with heat risks in Canada. Appl. Geogr. 2018, 95, 61–70. [Google Scholar] [CrossRef]
- ParkScore. 2019. Available online: https://www.tpl.org/city/boston-massachusetts (accessed on 6 February 2020).
- Guo, Y.; Gasparrini, A.; Armstrong, B.G.; Tawatsupa, B.; Tobias, A.; Lavigne, E.; Coelho, M.D.S.Z.S.; Pan, X.; Kim, H.; Hashizume, M.; et al. Heat Wave and Mortality: A Multicountry, Multicommunity Study. Environ. Health Perspect. 2017, 125, 087006. [Google Scholar] [CrossRef]
| Characteristic | |
|---|---|
| Warm Season Maximum Temperature [°F] (mean (range)) | 75.7 (46–103) |
| Warm Season Mean Temperature [°F] (mean (range)) | 67.9 (44–92) |
| Warm Season Minimum Temperature [°F] (mean (range)) | 60.1 (37–81) |
| Frequency of TMAX ≥ 90 °F (n) | 201 |
| Frequency of HIMAX ≥ 86 °F (n) | 165 |
| Frequency of TMAX ≥ 85 °F (n) | 502 |
| At-Home Deaths (n) | 6102 |
| Male (n (%)) | 3197 (52.4) |
| Race, Non-Caucasian (n (%)) | 2276 (37.3) |
| ≥65 years old (n (%)) | 3865 (63.3) |
| Outside of the Home Deaths (n) | 34,404 |
| Male (n (%)) | 20,744 (60.3) |
| Race, Non-Caucasian (n (%)) | 4322 (12.6) |
| ≥65 years old (n (%)) | 19,732 (57.4) |
| Assessed value of residential building/area ($)(mean (SD)) | 5910 (28,000) |
| Assessed value of residential land/area ($)(mean (SD)) | 408 (463) |
| Energy efficiency score of residential buildings (mean (SD)) | 6.25 (0.352) |
| Year residential buildings were built/renovated (mean (SD)) | 1970 (15.9) |
| Decade residential buildings were built/renovated (mean (SD)) | 1980 (33.9) |
| Albedo (mean (SD)) | 0.124 (0.0114) |
| Impervious Surface Fraction (mean (SD)) [%] | 0.787 (0.141) |
| Number of street trees/CT area (mean (SD)) | 0.00017 (0.00008) |
| Proportion of population with at least one disability (mean (SD)) [%] | 11.4 (7.4) |
| Proportion of population that is ≤5 years old (mean (SD)) [%] | 16.6 (10.4) |
| Proportion of population with at least 1 medical illness (mean (SD)) [%] | 38.6 (3.19) |
| Proportion of population that is ≥65 years old (mean (SD)) [%] | 10.5 (6.79) |
| Proportion of population that receives low-to-no income (mean (SD)) [%] | 28.0 (17.1) |
| Proportion of population with limited English proficiency (mean (SD)) [%] | 38.5 (17.8) |
| Proportion of population that is not Caucasian (mean (SD)) [%] | 51.6 (30.3) |
| Proportion of population with utilities excluded from rent (mean (SD)) [%] | 82.2 (17.6) |
| Proportion of population that is unemployed | 0.0905 (0.0662) |
| Gross Rent ($/month) | 1180 (471) |
| Ratio of Females-to-Males | 1.06 (0.324) |
| Gini Coefficient | 0.416 (0.0829) |
| Population Density (mean (SD)) [people/mile2] | 23,800 (18,300) |
| Personal | TMAX ≥ 90 °F | HIMAX ≥ 86 °F | TMAX ≥ 85 °F | |||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Female | 1.12 | (0.94, 1.34) | 1.01 | (0.83, 1.22) | 1.05 | (0.93, 1.19) |
| Not Married | 1.14 | (0.94, 1.39) | 1.13 | (0.91, 1.40) | 1.08 | (0.95, 1.24) |
| Race, Non-Caucasian | 0.90 | (0.75, 1.08) | 0.99 | (0.81, 1.21) | 0.99 | (0.87, 1.12) |
| Age < 57 | 1.02 | (0.83, 1.25) | 1.13 | (0.91, 1.41) | 1.03 | (0.89, 1.19) |
| Age > 81 | 0.88 | (0.72, 1.08) | 1.06 | (0.85, 1.32) | 0.94 | (0.82, 1.08) |
| Social | ||||||
| Low Income | 1.30 | (1.06, 1.59) | 0.92 | (0.73, 1.16) | 1.14 | (0.99, 1.32) |
| Unemployment | 1.03 | (0.84, 1.25) | 1.07 | (0.86, 1.32) | 0.98 | (0.85, 1.12) |
| GINI Index | 1.00 | (0.81, 1.22) | 1.01 | (0.81, 1.27) | 0.98 | (0.86, 1.13) |
| Population Density | 1.14 | (0.93, 1.39) | 1.08 | (0.86, 1.35) | 1.10 | (0.95, 1.27) |
| Sex Ratio F:M | 1.02 | (0.84, 1.25) | 0.98 | (0.79, 1.22) | 1.04 | (0.91, 1.19) |
| Utilities not Included | 1.13 | (0.92, 1.39) | 0.89 | (0.71, 1.13) | 1.08 | (0.93, 1.25) |
| Disability | 1.19 | (0.97, 1.46) | 1.09 | (0.87, 1.37) | 1.10 | (0.95, 1.28) |
| Children | 1.17 | (0.95, 1.44) | 1.03 | (0.82, 1.30) | 1.11 | (0.96, 1.28) |
| Elderly | 1.01 | (0.83, 1.24) | 1.01 | (0.81, 1.26) | 0.99 | (0.86, 1.14) |
| Limited English Prof. | 1.29 | (1.05, 1.57) | 0.88 | (0.69, 1.12) | 1.14 | (0.99, 1.32) |
| Race, Non-Caucasian | 1.19 | (0.97, 1.46) | 1.18 | (0.94, 1.48) | 1.14 | (0.98, 1.32) |
| Medical Illness | 0.97 | (0.79, 1.20) | 0.89 | (0.70, 1.12) | 1.01 | (0.87, 1.17) |
| Environmental | ||||||
| Energy Efficiency | 0.96 | (0.78, 1.18) | 0.95 | (0.76, 1.20) | 0.94 | (0.82, 1.09) |
| Assessed Value of Res Land/Total Property Area | 0.91 | (0.74, 1.12) | 0.87 | (0.69, 1.10) | 1.05 | (0.91, 1.20) |
| Assessed Value of Res Building/Gross Floor Area | 1.26 | (1.04, 1.53) | 1.04 | (0.83, 1.29) | 1.10 | (0.96, 1.27) |
| Year Built/Renovated | 1.13 | (0.91, 1.38) | 0.77 | (0.62, 0.95) | 1.12 | (0.97, 1.29) |
| Trees/CT Area | 0.92 | (0.75, 1.13) | 0.76 | (0.60, 0.97) | 0.96 | (0.83, 1.10) |
| Albedo | 0.93 | (0.78, 1.11) | 0.93 | (0.76, 1.13) | 0.93 | (0.82, 1.05) |
| Impervious Surface Fraction | 0.96 | (0.78, 1.17) | 0.96 | (0.77, 1.20) | 1.05 | (0.91, 1.20) |
| Primary Cause of Death | ||||||
| Infection | 1.46 | (0.72, 2.96) | 1.72 | (0.81, 3.65) | 1.69 | (1.02, 2.80) |
| Cancer | 0.84 | (0.69, 1.01) | 0.85 | (0.69, 1.04) | 0.93 | (0.82, 1.06) |
| Inflammatory Disease | 0.87 | (0.35, 2.18) | 1.11 | (0.44, 2.79) | 0.66 | (0.33, 1.30) |
| Endocrine/Nutritional/Metabolic Disease | 1.05 | (0.71, 1.54) | 1.12 | (0.75, 1.69) | 0.94 | (0.72, 1.24) |
| Mental/Behavioral/Neurodevelopmental Disease | 1.26 | (0.86, 1.85) | 0.76 | (0.46, 1.26) | 1.02 | (0.76, 1.36) |
| Nervous System Disease | 1.24 | (0.76, 2.04) | 1.06 | (0.59, 1.88) | 1.07 | (0.74, 1.54) |
| Heart Disease | 1.21 | (1.01, 1.46) | 1.11 | (0.9, 1.37) | 1.11 | (0.97, 1.26) |
| Respiratory Disease | 1.12 | (0.76, 1.67) | 1.12 | (0.73, 1.74) | 1.08 | (0.82, 1.43) |
| Injury/Accident/Event | 0.75 | (0.49, 1.16) | 0.96 | (0.62, 1.49) | 0.97 | (0.74, 1.29) |
| Self-Harm | 0.85 | (0.39, 1.86) | 0.71 | (0.29, 1.78) | 0.72 | (0.41, 1.24) |
| Assault-Related Altercation | 0.79 | (0.4, 1.56) | 1.47 | (0.82, 2.63) | 1.01 | (0.66, 1.54) |
| Personal | TMAX ≥ 90 °F | HIMAX ≥ 86 °F | TMAX ≥ 85 °F | |||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Sex | 1.03 | (0.95, 1.12) | 0.97 | (0.88, 1.05) | 1.03 | (0.98, 1.09) |
| Not Married | 1.04 | (0.96, 1.12) | 1.05 | (0.96, 1.14) | 1.02 | (0.97, 1.07) |
| Race, Non-Caucasian | 0.94 | (0.84, 1.06) | 1.03 | (0.90, 1.17) | 0.92 | (0.85, 1.00) |
| Age > 82 | 0.96 | (0.88, 1.04) | 0.99 | (0.90, 1.09) | 0.93 | (0.87, 0.98) |
| Age < 52 | 1.07 | (0.98, 1.17) | 1.03 | (0.93, 1.14) | 1.09 | (1.02, 1.16) |
| Primary Cause of Death | ||||||
| Infection | 0.81 | (0.55, 1.21) | 1.11 | (0.76, 1.62) | 0.99 | (0.77, 1.28) |
| Cancer | 0.99 | (0.89, 1.10) | 1.01 | (0.90, 1.14) | 1.03 | (0.96, 1.11) |
| Blood/Immune | 1.06 | (0.62, 1.81) | 0.95 | (0.51, 1.75) | 0.87 | (0.59, 1.29) |
| Endocrine/Nutritional/Metabolic | 1.12 | (0.94, 1.34) | 1.09 | (0.90, 1.33) | 1.12 | (0.99, 1.26) |
| Mental/Behavioral/Neurodevelopmental | 0.84 | (0.63, 1.14) | 1.01 | (0.74, 1.37) | 0.9 | (0.73, 1.10) |
| Nervous System Disease | 0.96 | (0.70, 1.33) | 0.83 | (0.57, 1.22) | 0.88 | (0.70, 1.11) |
| Circulatory Disease | 0.99 | (0.91, 1.07) | 0.92 | (0.84, 1.01) | 0.94 | (0.89, 0.99) |
| Respiratory Disease | 0.86 | (0.71, 1.04) | 1.04 | (0.85, 1.28) | 0.92 | (0.80, 1.05) |
| Congenital Disease | 1.54 | (0.70, 3.41) | 0.24 | (0.03, 1.74) | 1.4 | (0.77, 2.53) |
| Injury/Accident/Event | 1.12 | (0.96, 1.31) | 1.02 | (0.86, 1.22) | 1.09 | (0.98, 1.22) |
| Self-Harm | 1.03 | (0.79, 1.34) | 0.87 | (0.63, 1.19) | 1.12 | (0.94, 1.34) |
| Assault-Related Altercation | 1.05 | (0.85, 1.30) | 1.23 | (0.98, 1.53) | 1.09 | (0.94, 1.26) |
| Personal | TMAX ≥ 90 °F | HIMAX ≥ 86 °F | TMAX ≥ 85 °F | |||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Sex | 0.81 | (0.54, 1.21) | 0.74 | (0.47, 1.16) | 0.77 | (0.59, 1.00) |
| Not Married | 1.20 | (0.78, 1.83) | 1.38 | (0.85, 2.24) | 1.12 | (0.85, 1.47) |
| Race, Non-Caucasian | 1.05 | (0.72, 1.54) | 1.2 | (0.78, 1.84) | 1.18 | (0.92, 1.52) |
| Age > 82 | 0.98 | (0.69, 1.39) | 1.07 | (0.73, 1.56) | 0.81 | (0.64, 1.02) |
| Age < 58 | 1.15 | (0.82, 1.60) | 1.53 | (1.07, 2.18) | 1.31 | (1.05, 1.62) |
| Social | ||||||
| Low Income | 0.75 | (0.52, 1.07) | 0.81 | (0.55, 1.19) | 0.99 | (0.79, 1.24) |
| Unemployment | 1.03 | (0.74, 1.45) | 1.16 | (0.81, 1.67) | 1.06 | (0.85, 1.32) |
| GINI Index | 1.34 | (0.96, 1.88) | 0.91 | (0.61, 1.35) | 0.92 | (0.73, 1.16) |
| Population Density | 0.94 | (0.62, 1.43) | 0.9 | (0.56, 1.43) | 0.8 | (0.61, 1.06) |
| Sex Ratio F:M | 0.93 | (0.66, 1.30) | 1.01 | (0.70, 1.46) | 0.85 | (0.68, 1.06) |
| Utilities not Included | 1.07 | (0.76, 1.51) | 0.67 | (0.44, 1.02) | 1.09 | (0.87, 1.36) |
| Children | 0.81 | (0.57, 1.15) | 0.96 | (0.67, 1.39) | 1.07 | (0.87, 1.33) |
| Elderly | 1.49 | (1.07, 2.07) | 0.92 | (0.62, 1.37) | 1.33 | (1.06, 1.66) |
| Limited English Prof. | 0.8 | (0.56, 1.13) | 0.92 | (0.63, 1.35) | 0.99 | (0.79, 1.24) |
| Race, Non-Caucasian | 0.97 | (0.70, 1.36) | 0.91 | (0.62, 1.31) | 1.16 | (0.94, 1.43) |
| Medical Illness | 1.36 | (0.97, 1.91) | 1.24 | (0.85, 1.80) | 1.14 | (0.91, 1.43) |
| Low Income | 0.75 | (0.52, 1.07) | 0.81 | (0.55, 1.19) | 0.99 | (0.79, 1.24) |
| Environmental | ||||||
| Energy Efficiency | 1.44 | (1.03, 2.02) | 1.08 | (0.73, 1.59) | 1.11 | (0.88, 1.40) |
| Assessed Value of Res Land/Total Property Area | 0.86 | (0.56, 1.32) | 0.97 | (0.62, 1.52) | 0.78 | (0.59, 1.03) |
| Assessed Value of Res Building/Gross Floor Area | 0.74 | (0.51, 1.07) | 0.85 | (0.57, 1.27) | 0.98 | (0.78, 1.23) |
| Year Built/Renovated | 0.83 | (0.54, 1.28) | 0.85 | (0.53, 1.38) | 0.81 | (0.61, 1.07) |
| Trees/CT Area | 0.86 | (0.56, 1.34) | 1.12 | (0.72, 1.76) | 0.95 | (0.72, 1.25) |
| Albedo | 1.15 | (0.85, 1.56) | 0.90 | (0.64, 1.25) | 1.1 | (0.90, 1.34) |
| Impervious Surface Fraction | 0.76 | (0.53, 1.10) | 0.90 | (0.61, 1.33) | 0.83 | (0.66, 1.05) |
| Primary Cause of Death | ||||||
| Infection | 0.54 | (0.07, 4.02) | 1.40 | (0.60, 1.14) | 0.77 | (0.62, 0.96) |
| Liver Disease | 0.46 | (0.06, 3.45) | 3.58 | (0.59, 2.39) | 1.14 | (0.70, 1.86) |
| Cancer | 0.88 | (0.59, 1.31) | 0.85 | (0.77, 1.48) | 0.96 | (0.77, 1.21) |
| Diabetes | 1.16 | (0.55, 2.44) | 1.67 | (0.30, 1.93) | 1.26 | (0.75, 2.10) |
| Heart Disease | 0.9 | (0.64, 1.24) | 0.65 | (0.12, 2.10) | 1.26 | (0.68, 2.35) |
| Nervous System Disease | 1.11 | (0.49, 2.50) | 0.78 | (0.46, 3.91) | 0.8 | (0.33, 1.93) |
| Substance Abuse | 2.88 | (1.42, 5.86) | 1.16 | (0.60, 3.98) | 1.75 | (0.90, 3.39) |
| Inflammatory Disease | 0.88 | (0.21, 3.77) | 1.07 | (0.69, 8.62) | 1.6 | (0.56, 4.58) |
| Cerebrovascular Disease | 0.27 | (0.04, 1.95) | 0.33 | (0.06, 3.48) | 1.14 | (0.42, 3.08) |
| Digestive System Related Disease | 0.66 | (0.09, 4.97) | 1.74 | (1.17, 6.73) | 1.75 | (0.89, 3.47) |
| Unknown Causes | 2.38 | (1.13, 5.02) | 1.98 | (0.82, 4.76) | 1.66 | (0.92, 2,99) |
| Assault-Related Altercation | 1.49 | (0.87, 2.54) | 0.92 | (0.39, 38.5) | 1.79 | (1.24, 2.58) |
| Injury/Accident/Event | 0.8 | (0.42, 1.49) | 1.42 | (0.75, 2.68) | 1.11 | (0.77, 1.60) |
| Self-Harm | 1.00 | (0.36, 2.80) | 0.92 | (0.28, 2.98) | 0.99 | (0.50, 1.94) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Williams, A.A.; Allen, J.G.; Catalano, P.J.; Spengler, J.D. The Role of Individual and Small-Area Social and Environmental Factors on Heat Vulnerability to Mortality Within and Outside of the Home in Boston, MA. Climate 2020, 8, 29. https://doi.org/10.3390/cli8020029
Williams AA, Allen JG, Catalano PJ, Spengler JD. The Role of Individual and Small-Area Social and Environmental Factors on Heat Vulnerability to Mortality Within and Outside of the Home in Boston, MA. Climate. 2020; 8(2):29. https://doi.org/10.3390/cli8020029
Chicago/Turabian StyleWilliams, Augusta A., Joseph G. Allen, Paul J. Catalano, and John D. Spengler. 2020. "The Role of Individual and Small-Area Social and Environmental Factors on Heat Vulnerability to Mortality Within and Outside of the Home in Boston, MA" Climate 8, no. 2: 29. https://doi.org/10.3390/cli8020029
APA StyleWilliams, A. A., Allen, J. G., Catalano, P. J., & Spengler, J. D. (2020). The Role of Individual and Small-Area Social and Environmental Factors on Heat Vulnerability to Mortality Within and Outside of the Home in Boston, MA. Climate, 8(2), 29. https://doi.org/10.3390/cli8020029





