Addressing Climate Resilience in the African Region: Prioritizing Mental Health and Psychosocial Well-Being in Disaster Preparedness and Response Planning for Mainstream Communities and Migrants
Abstract
1. Introduction
1.1. Context and Background
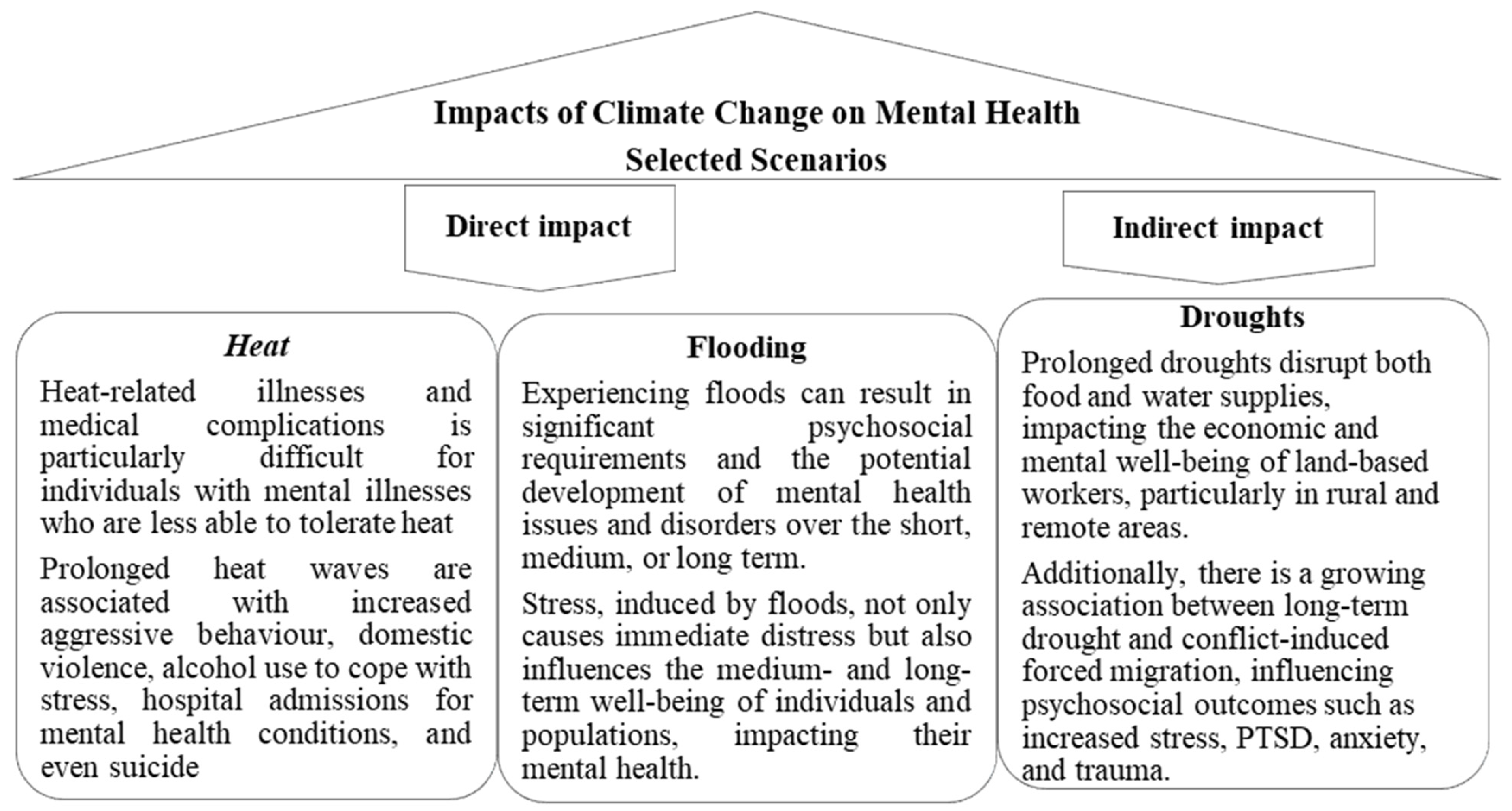
1.1.1. Climate Change and Mental Health Nexus
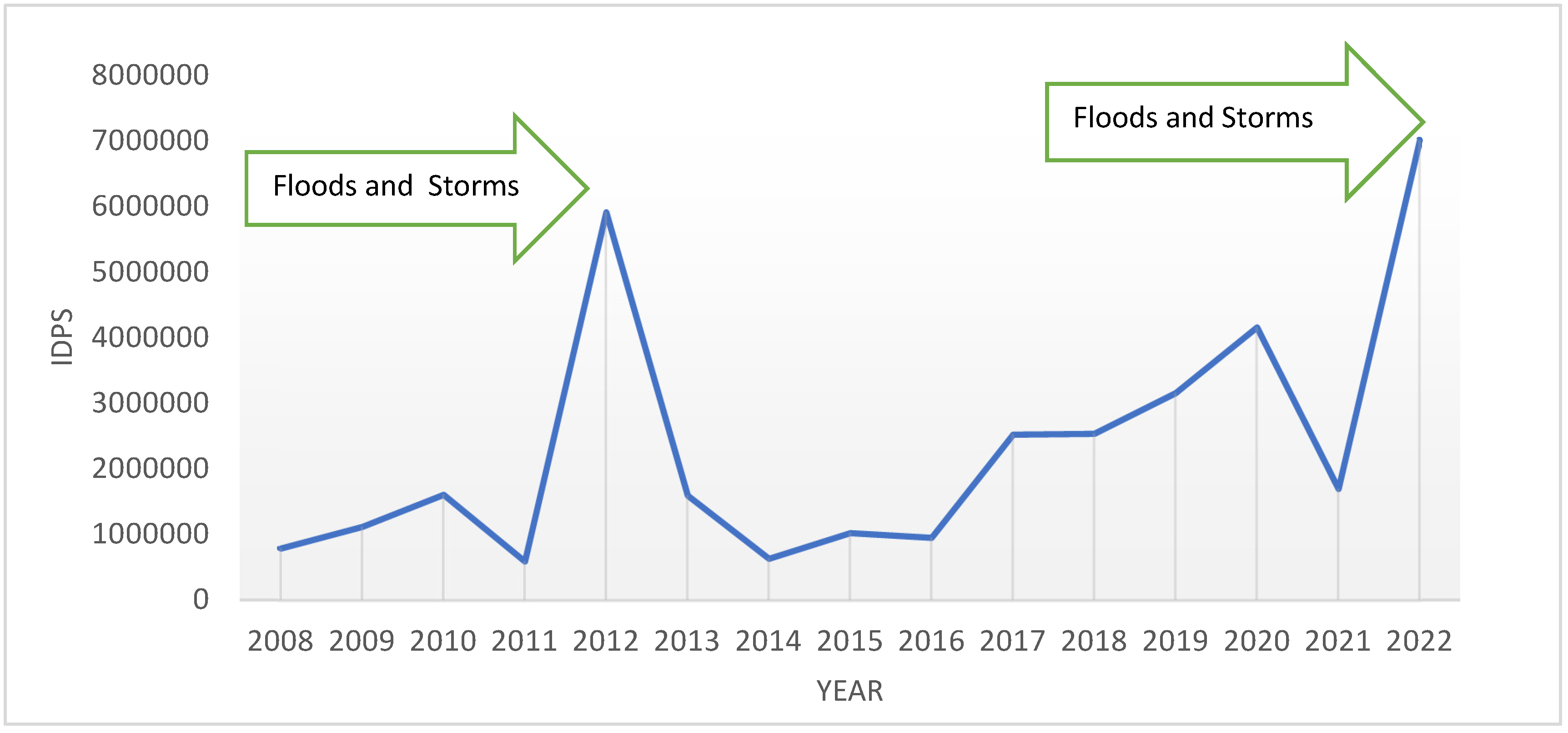
1.1.2. Climate Change–Mental Health–Migration Nexus
Regional Focus: Climate Change–Mental Health–Migration Nexus
Objectives
- Synthesize and summarize the current evidence on how climate change—through extreme weather events, resource insecurity, displacement, and chronic environmental stressors—affects mental health outcomes across diverse African populations, with a focus on vulnerable groups.
- Review and evaluate the extent to which the existing national and regional preparedness and response frameworks in Africa recognize, integrate, and address mental health risks and needs arising from climate change, highlighting the best practices and identifying significant gaps.
- Analyze the effectiveness of the current plans and interventions aimed at supporting mental health and psychosocial well-being during climate-related disasters at both the regional and sub-regional levels. Develop actionable recommendations to enhance these frameworks, ensuring they address the needs of both mainstream and migrant populations, and promote resilience, equity, and accessibility in mental healthcare.
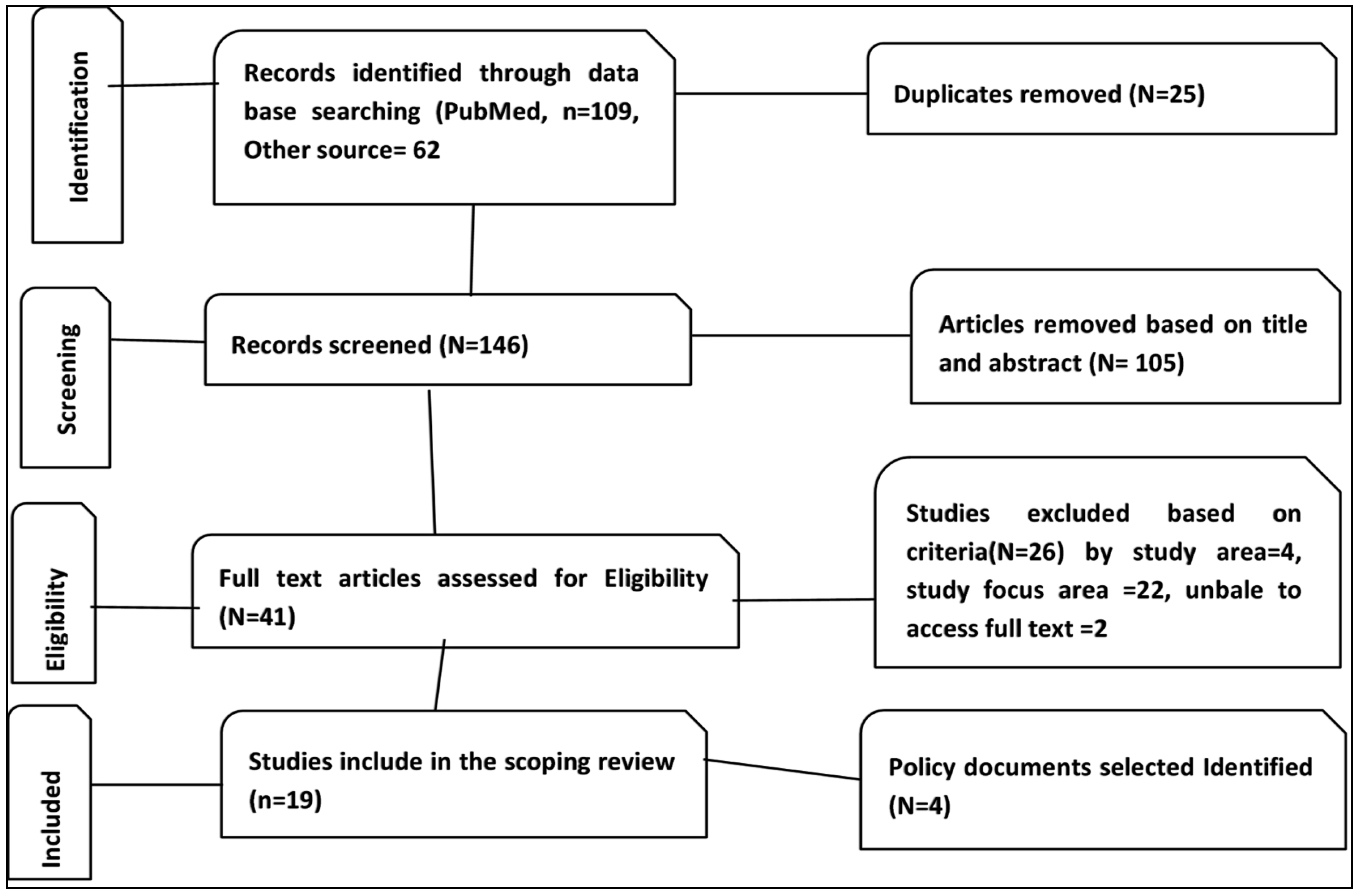
2. Methodology and Framework
2.1. Elements of the Adopted Methodology
2.1.1. Inclusion and Exclusion Criteria
2.1.2. Data Extraction and Analysis
3. Results and Key Observations
3.1. Climate Change and Mental Health Nexus in the African Region and Their Differentiated Impacts
| Study Site | Climate Change and Mental Health | Preparedness/Responseand Adaptation | Gap/Recommendation | The Method Adopted in the Study and Document Type (Formal and Informal Publications) |
|---|---|---|---|---|
| Africa | The climate crisis in Africa is damaging several health determinants, leading to poor health outcomes. Environmental shocks affect mental health directly or indirectly through social impact. | Early warning and adaption | Not mentioned. | Conference paper [59] |
| South Africa | Climate change can worsen existing social stressors, compounding their impacts on mental health. This is due to the amplification of pre-existing vulnerabilities, such as socio-economic conditions, access to healthcare, and other environmental stressors. | Not mentioned | Conducted in-depth analysis of the impact of climate change on mental health, with a particular emphasis on the vulnerable population. | Peer-reviewed paper [56] |
| Africa | The impact of climate change on social connections can lead to emotional disorders. This is because the loss of social capital resulting from climate change can have a negative effect on people’s mental health. | Preserve social capital | Communities highly exposed to climate change require action to preserve their social capital. | Qualitative [42] |
| South Africa | Trauma, loss of property and loved ones, and displacement can lead to anxiety, post-traumatic stress disorder, depression, and even suicide. | Not mentioned | Constant surveillance of climate-related health and associated risks needed. | Peer-reviewed paper [52] |
| Ghana | Can lead to the loss of livestock for farmers, resulting in mental health problems. | Provide veterinary support; treat animal diseases | Mixed method [60] | |
| Africa | Extreme weather results in depression and suicide, especially among farmers. Can also cause chronic distress and solastalgia. | Not mentioned, only explained that adaptation strategies at the sub-national level are often limited. | Adopt a ‘health and climate change in all policies’ approach for better adaptation and mitigation strategies. Sub-national governments often face limitations in implementing adaptation strategies. | Case-based study [54] |
| Tanzania | Leads to anxiety and other poor mental health outcomes. | Not mentioned | Further research is needed to inform policies and interventions that will mitigate the impacts. | Case study [42,61] |
| Tanzania | Climate change can impact the mental health of young people through various channels, resulting in depression. | Not mentioned | Cross-sectional [55] | |
| Kenya | Exposes the community to various stressors, resulting in mental health challenges and a rise in alcohol and substance abuse. | Not mentioned | Report [22] | |
| South Africa | Depression. | Not mentioned | The study did not consider or conduct research considering children. | Survey [53] |
| Zimbabwe and Sudan | Stress disorders and depression are prevalent. | Not mentioned | Literature [23] | |
| Selected African countries | Affect children physically, mentally, and emotionally. | Indigenous knowledge can help individuals cope with climate change by using animal behavior to forecast weather, diversify crops, manage cattle stress, and divide labor during droughts. | More research and surveillance data on mental health effects of climate change in Africa. | [58] |
| Africa | Stress, PTSD, and mental health problems. | Not mentioned | Peer-reviewed paper [62] | |
| S. Africa | Increased aggression, violent behavior, and homicides. | Not mentioned | A call for action to change is made to mitigate these effects at the individual and policy levels. | Narrative report [57] |
| Nigeria | Flooding can trigger psychosocial distress due to socio-economic losses, such as property damage and displacement, experienced by affected individuals. | Provision of daily basic needs | It needs to include mental health policies and funding allocation for its implementation. | [24] |
3.2. Climate Change, Mental Health, and Migration Nexus in the African Region
3.3. Assessment of the Existing Adaption, Preparedness, and Response Plans Using Case Studies
4. Discussion
Limitations
5. Concluding Notes and Way Forward
| Government and Policymakers and Related Stakeholders | Researchers/Academia/Think Tanks | International, Regional Agencies, and Development Financing Institutions |
|---|---|---|
|
|
|
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations/Acronyms
Appendix A. Additional Information Relevant to This Rapid Assessment
- What insights do the existing peer-reviewed assessments and literature offer regarding the impact of climate change on mental health in Africa, particularly considering regional variations?
- What are the existing plans related to mental health and psychosocial well-being in the face of climate change at the regional and sub-regional levels in Africa, and what recommendations can be made to enhance their effectiveness?
| “Mental Health” [MeSH Terms] AND “Climate Change” [Mesh] OR Hurricanes [tw] OR flood OR wildfire* [tw] OR drought [tw] OR “sea level rise” [tw] OR coastal[tw] erosion[tw] OR heatwave*[tw]. “Disaster Planning” [Mesh] OR prevention[tw] OR recovery[tw] OR coping strategies OR Preparedness[tw] OR response[tw] OR plan*[tw] OR intervention[tw]. “Africa”[Mesh] OR Algeria[tw] OR Angola[tw] OR Benin[tw] OR Botswana[tw] OR “Burkina Faso”[tw] OR Burundi[tw] OR “Cabo Verde”[tw] OR Cameroon[tw] OR “Central African Republic”[tw] OR Chad[tw] OR Comoros[tw] OR Congo[tw] OR “Democratic Republic of the Congo”[tw] OR “Cote d’Ivoire”[tw] OR Djibouti[tw] OR Egypt[tw] OR “Equatorial Guinea”[tw] OR Eritrea[tw] OR Eswatini[tw] OR Ethiopia[tw] OR Gabon[tw] OR Gambia[tw] OR Ghana[tw] OR Guinea[tw] OR Guinea-Bissau[tw] OR Kenya[tw] OR Lesotho[tw] OR Liberia[tw] OR Libya[tw] OR Madagascar[tw] OR Malawi[tw] OR Mali[tw] OR Mauritania[tw] OR Mauritius[tw] OR Morocco[tw] OR Mozambique[tw] OR Namibia[tw] OR Niger[tw] OR Nigeria[tw] OR Rwanda[tw] OR “Sao Tome and Principe”[tw] OR Senegal[tw] OR Seychelles[tw] OR “Sierra Leone”[tw] OR Somalia[tw] OR “South Africa”[tw] OR “South Sudan”[tw] OR Sudan[tw] OR Tanzania[tw] OR Togo[tw] OR Tunisia[tw] OR Uganda[tw] OR Zambia[tw] OR Zimbabwe[tw]. Original research papers and gray literature related to our topic using electronic databases, such as Google, Google Scholar, and PubMed, were searched. The search strategy focused on four main areas: Mental Health, Climate Change, Preparedness, and Africa. The search terms included “Mental health,” “Mental health effect,” “climate change adaption,” “climate change,” “hurricanes”, “flood”, “wildfires,” “droughts,” “heatwaves,” “sea-level rise,” “coastal erosion,” “services,” “interventions,” “response,” “preparedness,” “Nigeria,” “Ethiopia,” “Egypt,” “DR Congo,” “Tanzania,” “South Africa,” “Kenya,” “Uganda,” “Sudan,” “Algeria,” OR “Morocco,” “Angola,” “Ghana,” “Mozambique,” “Madagascar,” “Côte d’Ivoire,” “Cameroon,” “Niger,” “Mali,” “Burkina Faso,” “Malawi,” “Zambia,” “Chad,” “Somalia,” “Senegal,” “Zimbabwe,” “Guinea,” “Rwanda,” “Benin,” “Burundi,” “Tunisia,” “South Sudan,” “Togo,” “Sierra Leone,” “Libya,” “Congo,” “Central African Republic,” “Liberia,” “Mauritania,” “Eritrea,” “Gambia,” “Botswana” “Namibia,” “Gabon,” “Lesotho,” “Guinea-Bissau,” “Equatorial Guinea,” “Mauritius,” “Eswatini,” OR “Djibouti,” “Comoros,” “Cabo Verde,” “Sao Tome & Principe,” “Seychelles”, and “Africa. |
Appendix B. Overview of Vulnerable Groups to Climate Change-Induced Mental Health Nexus as Reflected (or Not) in the Existing Studies from the Region
| References | Vulnerability Groups/Factors mentioned or reflected in the study |
| Atwoli, L. et al. 2022 [56,57] | Not mentioned |
| Chersich et al., 2018 [54] | Reflects on women, fishing communities, rural subsistence farmers, and those living in informal settlements |
| Di Giorgi et al., 2020 [58] | Not mentioned |
| Myers, J. et al., 2011 [50] | Not mentioned |
| Nuvey et al., 2020 [59] | Not mentioned |
| Godsmark et al., 2019 [59] | Children and women |
| Heaney et al., 2016 [42] | Not mentioned |
| Prencipe, L. et al., 2023 [53] | Largely focused on Young people |
| Sheriff et al., 2022 [21] | Not mentioned |
| Tomita et al., 2022 [51] | Reflects Women, Black Africans, and individuals with lower educational qualifications or income |
| Trummer et al., 2023 [22] | Children and women |
| Atwoli et al., 2022 [56,57] | Children, migrants |
| Lokotola et al., 2023 [60] | Not mentioned |
| Chetty, I. et al., 2022 [55] | Focuses on existing challenges of poverty, inequality, crime, and political turmoil |
| Oluka EM et al., 2022 [23] | Refelcts on children, older adults, persons with disabilities, and people with mental health conditions |
References
- United Nations. Climate Action. 2023. Available online: https://www.un.org/en/climatechange/what-is-climate-change (accessed on 23 November 2024).
- World Health Organization. Climate Change. 2023. Available online: https://www.who.int/health-topics/climate-change#tab=tab_1 (accessed on 23 November 2024).
- Pan American Health Organization, World Health Orgnization. Climate Change and Health. 2023. Available online: https://www.paho.org/en/topics/climate-change-and-health (accessed on 23 November 2024).
- Padhy, S.K.; Sarkar, S.; Panigrahi, M.; Paul, S. Mental health effects of climate change. Indian J. Occup. Environ. Med. 2015, 19, 3–7. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Mental Health. 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response (accessed on 27 November 2024).
- United Nations Health Agency (World Health Organization). 2019. Available online: https://news.un.org/en/story/2019/10/1048931 (accessed on 27 November 2024).
- European Commission. Tracking Framework for the Implementation of the Commission Communication on a Comprehensive Approach to Mental Health; Directorate-General for Health and Food Safety: Brussels, Belgium, 2024. [Google Scholar]
- European Climate and Public Health Observatory. Climate Change Impacts on Mental Health in Europe an Overview of Evidence March 2022. Available online: https://www.infocop.es/wp-content/uploads/2025/03/European_Climate_Health_Observatory_mental-health_evidence_review_2022.pdf (accessed on 21 January 2025).
- World Health Organization. World Mental Health Report: Transforming Mental Health for All; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Institute for Health Metrics and Evaluation (IHME). GBD Results; IHME, University of Washington: Seattle, WA, USA, 2020; Available online: https://vizhub.healthdata.org/gbd-results/ (accessed on 12 January 2024).
- Hayes, K.; Blashki, G.; Wiseman, J.; Burke, S.; Reifels, L. Climate change and mental health: Risks, impacts and priority actions. Int. J. Ment. Health Syst. 2018, 12, 28. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cianconi, P.; Betrò, S.; Janiri, L. The Impact of Climate Change on Mental Health: A Systematic Descriptive Review. Front. Psychiatry 2020, 11, 74. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sugden, S.G.; Merlo, G. What do Climate Change, Nutrition, and the Environment Have to do With Mental Health? Am. J. Lifestyle Med. 2024. [Google Scholar] [CrossRef]
- American Psychatric Association. Extreme Heat Can Take a Toll on Mental Health. Available online: https://www.psychiatry.org/news-room/apa-blogs/extreme-heat-can-take-a-toll-on-mental-health (accessed on 14 January 2024).
- White, B.P.; Breakey, S.; Brown, M.J.; Smith, J.R.; Tarbet, A.; Nicholas, P.K.; Ros, A.M.V. Mental Health Impacts of Climate Change Among Vulnerable Populations Globally: An Integrative Review. Ann. Glob. Health 2023, 89, 66. [Google Scholar] [CrossRef]
- Clayton, S.; Manning, C.M.; Krygsman, K.; Speiser, M. Mental Health and Our Changing Climate: Impacts, Implications, and Guidance; American Psychological Association, and ecoAmerica: Washington, DC, USA, 2017. [Google Scholar]
- Nagabhatla, N.; Cassidy-Neumiller, M.; Francine, N.N.; Maatta, N. Water, conflicts and migration and the role of regional diplomacy: Lake Chad, Congo Basin, and the Mbororo pastoralist. Environ. Sci. Policy 2021, 122, 35–48. [Google Scholar] [CrossRef]
- Tanarhte, M.; De Vries, A.J.; Zittis, G.; Chfadi, T. Severe droughts in North Africa: A review of drivers, impacts and management. Earth-Sci. Rev. 2024, 250, 104701. [Google Scholar] [CrossRef]
- Jedd, T.; Fragaszy, S.R.; Knutson, C.; Hayes, M.J.; Fraj, M.B.; Wall, N.; Svoboda, M.; McDonnell, R. Drought Management Norms: Is the Middle East and North Africa Region Managing Risks or Crises? J. Environ. Dev. 2021, 30, 3–40. [Google Scholar] [CrossRef]
- Abel, G.J.; Brottrager, M.; Crespo Cuaresma, J.; Muttarak, R. Climate, conflict and forced migration. Glob. Environ. Change 2019, 54, 239–249. [Google Scholar] [CrossRef]
- Sheriff, M.; Mash, R. Climate change and primary health care in Chakama, Kilifi County, Kenya. Afr. J. Prim. Health Care Fam. Med. 2022, 14, e1–e3. [Google Scholar] [CrossRef]
- Trummer, U.; Ali, T.; Mosca, D.; Mukuruva, B.; Mwenyango, H.; Novak-Zezula, S. Climate change aggravating migration and health issues in the African context: The views and direct experiences of a community of interest in the field. J. Migr. Health 2023, 7, 100151. [Google Scholar] [CrossRef] [PubMed]
- Oluka, E.M.; Dossen, S.B.; Ebuenyi, I.D. Flooding in Nigeria, towards prioritizing mental health and psychosocial support. Pan Afr. Med. J. 2022, 43, 199. [Google Scholar] [CrossRef] [PubMed]
- American Psychatric Associaition. How Extreme Weather Events Affect Mental Health. Last Modified May 2023. Available online: https://www.psychiatry.org/patients-families/climate-change-and-mental-health-connections/affects-on-mental-health (accessed on 13 January 2025).
- Hickman, C.; Marks, E.; Pihkala, P.; Clayton, S.; Lewandowski, R.E.; Mayall, E.E.; Wray, B.; Mellor, C.; van Susteren, L. Climate anxiety in children and young people and their beliefs about government responses to climate change: A global survey. Lancet Planet Health 2021, 5, e863–e873. [Google Scholar] [CrossRef] [PubMed]
- Internal Displacements Monitoring Center. Internally Displaced People (IDPs). 2024. Available online: https://www.internal-displacement.org/database/displacement-data/ (accessed on 9 February 2025).
- Mental Helath Foundation. Mental Health and Climate Change-COP26. 2021. Available online: https://www.mentalhealth.org.uk/our-work/policy-and-advocacy/climate-change (accessed on 30 November 2024).
- Ingle, H.E.; Mikulewicz, M. Mental health and climate change: Tackling invisible injustice. Lancet Planet Health 2020, 4, e128–e130. [Google Scholar] [CrossRef]
- Black Dog Institute. The Nexus Between Climate Change and Mental Health Briefing Prepared by Black Dog Institute for COP26. Sydney, Australia 2023. Available online: https://www.blackdoginstitute.org.au/news/the-implications-of-climate-change-on-mental-health/ (accessed on 30 November 2024).
- Adaawen, S.; Rademacher-Schulz, C.; Schraven, B.; Segadlo, N. Chapter 2—Drought, migration, and conflict in sub-Saharan Africa: What are the links and policy options? In Current Directions in Water Scarcity Research; Mapedza, E., Tsegai, D., Bruntrup, M., McLeman, R., Eds.; Elsevier: Amsterdam, The Netherlands, 2019; Volume 2, pp. 15–31. [Google Scholar]
- Alto, M.E.; Nicasio, A.V.; Stewart, R.; Rodríguez-Sanfiorenzo, T.D.; González-Elías, G.; Orengo-Aguayo, R. Provision of mental health services immediately following a natural disaster: Experiences after Hurricane Maria in Puerto Rico. J. Emerg. Manag. 2021, 19, 167–175. [Google Scholar] [CrossRef]
- Yousuf, J.; Mehmood, H.; Aquil, S.; Rija, A.; Syyeda Rahmat, Z.; Malikzai, A. Effects of floods on the mental health of Pakistanis: A commentary. Ann. Med. Surg. 2023, 85, 2253–2255. [Google Scholar] [CrossRef]
- Rodney, R.M.; Swaminathan, A.; Calear, A.L.; Christensen, B.K.; Lal, A.; Lane, J.; Leviston, Z.; Reynolds, J.; Trevenar, S.; Vardoulakis, S.; et al. Physical and Mental Health Effects of Bushfire and Smoke in the Australian Capital Territory 2019–2020. Front. Public Health 2021, 9, 682402. [Google Scholar] [CrossRef]
- World Health Organization. Mental Health of Refugees and Migrants: Risk and Protective Factors and Access to Care; Global Evidence Review on Health and Migration (GEHM) Series; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Torres, J.M.; Casey, J.A. The centrality of social ties to climate migration and mental health. BMC Public Health 2017, 17, 600. [Google Scholar] [CrossRef]
- Okasha, A. Mental health in Africa: The role of the WPA. World Psychiatry 2002, 1, 32–35. [Google Scholar]
- IOM. Migration, Environment and Climate Change: Assessing the Evidence; IOM: Geneva, Switzerland, 2009; 448p, ISBN 978-92-9068-454-1. Available online: http://publications.iom.int/system/files/pdf/migration_and_environment.pdf (accessed on 1 December 2024).
- IOM. IOM Outlook on Migration, Environment and Climate Change; IOM: Geneva, Switzerland, 2014. [Google Scholar]
- Sankoh, O.; Sevalie, S.; Weston, M. Mental health in Africa. Lancet Glob. Health 2018, 6, e954–e955. [Google Scholar] [CrossRef] [PubMed]
- Africa CDC. Mental Health, A Universal Human Right for Africans. 2023. Available online: https://africacdc.org/news-item/mental-health-a-universal-human-right-for-africans/ (accessed on 28 November 2024).
- Camh. Climate Change and Mental Health. 2023. Available online: https://www.camh.ca/en/professionals/professionals--projects/climate-change-and-mental-health (accessed on 28 November 2024).
- Heaney, A.K.; Winter, S.J. Climate-driven migration: An exploratory case study of Maasai health perceptions and help-seeking behaviors. Int. J. Public Health 2016, 61, 641–649. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 1–9. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
- Health Sciences Library. Scoping Reviews: Step 4: Manage Citations. 2023. Available online: https://guides.lib.unc.edu/scoping-reviews/manage-citations (accessed on 5 November 2024).
- UNFCCC. United Nations Framework Convention on Climate Change. 2024. Available online: https://unfccc.int/resource/ccsites/zimbab/conven/text/art01.htm (accessed on 19 June 2024).
- UNDRR. Preparedness|United Nations Office for Disaster Risk Reduction. 2024. Available online: https://www.undrr.org/terminology/disaster (accessed on 19 June 2024).
- Myers, J.; Tucker, T.; Young, T.; Galloway, M.; Manyike, P. A public health approach to the impact of climate change on health in southern Africa-identifying priority modifiable risks. S. Afr. Med. J. 2011, 101, 817–822. [Google Scholar]
- Tomita, A.; Ncama, B.P.; Moodley, Y.; Davids, R.; Burns, J.K.; Mabhaudhi, T.; Modi, A.T.; Slotow, R. Community disaster exposure and first onset of depression: A panel analysis of nationally representative South African data, 2008–2017. PLoS Clim. 2022, 1, 0000024. [Google Scholar] [CrossRef]
- Godsmark, C.N.; Irlam, J.; van der Merwe, F.; New, M.; Rother, H.A. Priority focus areas for a sub-national response to climate change and health: A South African provincial case study. Environ. Int. 2019, 122, 31–51. [Google Scholar] [CrossRef]
- Prencipe, L.; Houweling, T.A.J.; van Lenthe, F.J.; Kajula, L.; Palermo, T. Climate distress, climate-sensitive risk factors, and mental health among Tanzanian youth: A cross-sectional study. Lancet Planet Health 2023, 7, e877–e887. [Google Scholar] [CrossRef]
- Chersich, M.F.; Wright, C.Y.; Venter, F.; Rees, H.; Scorgie, F.; Erasmus, B. Impacts of Climate Change on Health and Wellbeing in South Africa. Int. J. Environ. Res. Public Health 2018, 15, 1884. [Google Scholar] [CrossRef]
- Chetty, I.; Nayager, T.; Morar, T.; Iyaloo, S.; Subramaney, U. Climate Change and Mental Health implications in South Africa. Wits J. Clin. Med. 2022, 4, 151–156. [Google Scholar] [CrossRef]
- Atwoli, L.; Merali, Z.; Muhia, J. Mental health and climate change in Africa. BJPsych Int. 2022, 19, 86–89. [Google Scholar] [CrossRef]
- Atwoli, L.; Erhabor, G.E.; Gbakima, A.A.; Haileamlak, A.; Ntumba, J.K.; Kigera, J.; Laybourn-Langton, L.; Mash, B.; Muhia, J.; Mulaudzi, F.M.; et al. COP27 Climate Change Conference: Urgent action needed for Africa and the world. East Mediterr. Health J. 2022, 28, 785–787. [Google Scholar] [CrossRef] [PubMed]
- Di Giorgi, E.; Michielin, P.; Michielin, D. Perception of climate change, loss of social capital and mental health in two groups of migrants from African countries. Ann. Ist. Super. Sanita 2020, 56, 150–156. [Google Scholar] [CrossRef]
- Nuvey, F.S.; Kreppel, K.; Nortey, P.A.; Addo-Lartey, A.; Sarfo, B.; Fokou, G.; Ameme, D.K.; Kenu, E.; Sackey, S.; Addo, K.K.; et al. Poor mental health of livestock farmers in Africa: A mixed methods case study from Ghana. BMC Public Health 2020, 20, 825. [Google Scholar] [CrossRef]
- Lokotola, C.L.; Mash, R.; Naidoo, K.; Mubangizi, V.; Mofolo, N.; Schwerdtle, P.N. Climate change and primary health care in Africa: A scoping review. J. Clim. Change Health 2023, 11, 100229. [Google Scholar] [CrossRef]
- Serdeczny, O.; Adams, S.; Baarsch, F.; Coumou, D.; Robinson, A.; Hare, W.; Schaeffer, M.; Perrette, M.; Reinhardt, J. Climate change impacts in Sub-Saharan Africa: From physical changes to their social repercussions. Reg. Environ. Change 2017, 17, 1585–1600. [Google Scholar] [CrossRef]
- Bahal’Okwibale, P.M. Mainstreaming Climate-Related Disaster Risk Reduction in Agriculture and Food Sectors in Eastern Africa: Analytical Report; FAO: Addis Ababa, Ethiopia, 2017. [Google Scholar]
- Filho, W.L.; Ternova, L.; Fayyaz, M.M.; Abubakar, I.R.; Kovaleva, M.; Donkor, F.K.; Anuga, S.W.; Matamanda, A.R.; Djekic, I.; Umar, I.A.; et al. An analysis of climate change and health hazards: Results from an international study. Int. J. Clim. Change Strateg. Manag. 2022, 14, 375–398. [Google Scholar] [CrossRef]
- Federal Democratic Republic of Ethiopia. Ethiopia’s Climate Resilient Green Economy-National Adaptation Plan; Federal Democratic Republic of Ethiopia: Addis Ababa, Ethiopia, 2019. [Google Scholar]
- Republic of Kenya. Kenya National Adaptation Plan: 2015–2030; Government of Kenya: Nairobi, Kenya, 2016. [Google Scholar]
- Nwafor, C.; Ogundeji, A.; Nwafor, I.C. Review of agricultural extension and advisory services in sub-Saharan African countries. Progress with private sector involvement. J. Agribus. Rural Dev. 2021, 3, 271–282. [Google Scholar] [CrossRef]
- Republic of South Africa. Republic of South Africa National Climate Change Adaptation Strategy; Republic of South Africa: Pretoria, South Africa, 2020. [Google Scholar]
- Antwi-Agyei, P. Ghana’s National Adaptation Plan Framework. 2018. Available online: https://napglobalnetwork.org/wp-content/uploads/2020/04/napgn-en-2018-ghana-nap-framework.pdf (accessed on 15 October 2024).
- International Organization for Migration. Migration, Climate Change and the Environment; International Organization for Migration: Geneva, Switzerland, 2009. [Google Scholar]
- Africa Union. African Union Climate Change and Resilient Development Strategy and Action Plan (2022–2032). Available online: https://au.int/sites/default/files/documents/41959-doc-CC_Strategy_and_Action_Plan_2022-2032_08_02_23_Single_Print_Ready.pdf (accessed on 15 October 2024).
- World Health Organization. Rabat Declaration Adopted to Improve Refugee and Migrant Health. 2023. Available online: https://www.who.int/news/item/16-06-2023-rabat-declaration-adopted-to-improve-refugee-and-migrant-health (accessed on 27 November 2024).
- Beckline, M.; Sun, Y.; Eric, Z.; John, A.B.; Tahle, M.; Lisette, N.; Bernard, L. Environmental Degradation in Conflict and Post-Conflict Regions. Int. J. Environ. Prot. Policy 2016, 4, 187–195. [Google Scholar] [CrossRef]
- Leal, F.W.; Taddese, H.; Balehegn, M.; Nzengya, D.; Debela, N.; Abayineh, A.; Mworozi, E.; Osei, S.; Ayal, D.Y.; Nagy, G.J.; et al. Introducing experiences from African pastoralist communities to cope with climate change risks, hazards and extremes: Fostering poverty reduction. Int. J. Disaster Risk Reduct. 2020, 50, 101738. [Google Scholar] [CrossRef]



| Country | Extreme Event Risks, Health | Adaptation Options | Potential Impacts on Health | Mental Health | Migration |
|---|---|---|---|---|---|
| Ethiopia | Increase in temperature and drought frequency, and extreme events, including heat waves and storms | Improving human health systems by implementing integrated health and environmental surveillance protocols https://www4.unfccc.int/sites/NAPC/Documents/Parties/Final%20Ethiopia-national-adaptation-plan%20%281%29.pdf (accessed on 14 November 2024) | Increase vector-borne diseases, increase water-borne diseases, severe malnutrition, and increase flood incidence displacement | Not mentioned explicitly | Climate change poses significant risks, including more frequent droughts and floods, which in turn are leading to an increase in the migration of rural residents to urban areas. Term ‘migration’ is mentioned 16 times. |
| Kenya | Not specified for the health sector alone. The word ‘health’ is mentioned about 19 times | Strengthen the integration of climate change adaptation measures in the health sector https://countytoolkit.devolution.go.ke/sites/default/files/resources/Kenya_NAP_Final.pdf (acessed on 14 November 2024) | Impacts on water quality, water resources, changes in habitat, increasing exposure of vulnerable groups, sanitation and drainage, and vector-borne diseases are all areas for concern | Not mentioned explicitly | Strengthen vulnerable groups’ adaptive capacity and promote livelihood diversification for vulnerable groups to reduce rural–urban migration. Term ‘migration’ is mentioned 3 times. |
| South Africa | Changing climate can have a myriad of impacts on the health sector | Ensure that healthcare facilities are equipped and capable of managing the health effects of climate change and diseases sensitive to climate https://unfccc.int/sites/default/files/resource/South-Africa_NAP.pdf (acessed on 14 November 2024) | Quadruple disease burden; poor housing, infrastructure, and service delivery; changes in the distribution of diseases; and catastrophic events may affect the population’s health | Not mentioned explicitly | Migration is addressed only by the term mentioned once. The relationship between climate change and rural–urban migration is a potential area for research. |
| Ghana | Not mentioned | Not mentioned https://faolex.fao.org/docs/pdf/gha189992.pdf (acessed on 14 November 2024) | (Not mentioned) | Not mentioned explicitly | The term ‘migration’ is mentioned 4 times. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shibesh, B.F.; Nagabhatla, N. Addressing Climate Resilience in the African Region: Prioritizing Mental Health and Psychosocial Well-Being in Disaster Preparedness and Response Planning for Mainstream Communities and Migrants. Climate 2025, 13, 139. https://doi.org/10.3390/cli13070139
Shibesh BF, Nagabhatla N. Addressing Climate Resilience in the African Region: Prioritizing Mental Health and Psychosocial Well-Being in Disaster Preparedness and Response Planning for Mainstream Communities and Migrants. Climate. 2025; 13(7):139. https://doi.org/10.3390/cli13070139
Chicago/Turabian StyleShibesh, Belayneh Fentahun, and Nidhi Nagabhatla. 2025. "Addressing Climate Resilience in the African Region: Prioritizing Mental Health and Psychosocial Well-Being in Disaster Preparedness and Response Planning for Mainstream Communities and Migrants" Climate 13, no. 7: 139. https://doi.org/10.3390/cli13070139
APA StyleShibesh, B. F., & Nagabhatla, N. (2025). Addressing Climate Resilience in the African Region: Prioritizing Mental Health and Psychosocial Well-Being in Disaster Preparedness and Response Planning for Mainstream Communities and Migrants. Climate, 13(7), 139. https://doi.org/10.3390/cli13070139







