Abstract
Climate variability and change are already having a negative impact on the health of tens of millions of Africans through exposure to sub-optimal temperatures and extreme weather conditions as well as increasing the range and transmission of infectious diseases. This study aims to identify climate risks and the vulnerability of health systems as well as individual coping strategies in the city of N’Djaména. To achieve this, we adopted a methodology combining both quantitative and qualitative approaches. Meteorological data on wind, temperature, and rainfall were collected at daily and monthly intervals from the National Meteorological Agency in N’Djaména. Qualitative data were collected via focus group discussions with targets of the city’s health system and quantitative data were collected from the population on the basis of oriented questionnaires. The results show that rising temperatures with heat waves, regular flooding, and strong winds are the major climate risks identified. These have numerous impacts and effects on the city’s health system due to the following vulnerability factors most recognized by city dwellers: insufficient medical equipment in health facilities (IEME), the fragile nature of people’s physiological state in the face of climatic risks (CFEP), and the failure of city sanitation strategies and policies (DSPA). This study proposes a set of recommendations for transformational adaptation of the healthcare sector, which remains vulnerable to climate risks.
1. Introduction
Climate variability and change are already negatively impacting the health of tens of millions of Africans through exposure to sub-optimal temperatures and extreme weather conditions as well as increasing the range and transmission of infectious diseases [1]. Mortality and morbidity will increase as global warming continues, increasing the pressure on healthcare and economic systems [2]. If global warming reaches 2 °C, the distribution and seasonal transmission of vector-borne diseases are likely to intensify, exposing tens of millions more people, mainly in Central, West, East, and Southern Africa. These changes are likely to jeopardize health improvements in future socio-economic development [3]. Taking into account climate change projections, current climate policies, and the resilience of health systems to climate change, future scenarios are even more devastating in terms of morbidity and mortality (World Bank, 2023). For example, the World Meteorological Organization believes that climate-resilient universal health systems are an essential condition for ensuring equitable and effective protection against the health effects of climate change (WMO, 2023). According to ClimaHealth [4], protection against climate change depends on strong health systems and individual adaptation efforts. Furthermore, the best policies for adaptation and resilience strategies involve taking into account local and individual practices [3].
According to the National Adaptation Action Plan (NAPA) and the work of Verisk [5], Chad is considered by the international scientific community as one of the world’s climate change hotspots. Indeed, Chad was classified as the country most at risk, out of 186 countries assessed, in a study on climate vulnerability. In addition, the COVID-19 pandemic has had a major economic impact on the country and has contributed to delaying the implementation of planned adaptation actions. The pandemic has also amplified the vulnerabilities of urban communities to climate change, particularly among those most at risk and marginalized, including women. The NAPA and the various national communications that the country has submitted to the United Nations Framework Convention on Climate Change (UNFCCC) point to the many climate risks weighing on the well-being of rural and urban populations. At the same time, it is glaringly obvious that the studies carried out to date on climate change in Chad have left out the health sector. For example, the work of Abdoulay et al. [6] focused on climate variability, perceptions, and farmers’ adaptation strategies in Chad. As for Bahoutou [7], he based his analysis on rainfall in the Sudanian zone of Chad over the last four decades on the climatic variability in rainfall and mean annual temperature, with sequences of recurrent floods and droughts in and around N’Djaména. Bedoum et al. [8] assessed the impact of rainfall variability and drought on agricultural production in southern Chad. Global warming and migration to the shores of Lake Chad were addressed by Kitoto [9]. The health sector has not merited any attention from the scientific community and professionals involved in implementing climate change adaptation actions.
According to the national and provincial consultations undertaken during the preparation of the National Determined Contribution and studies of the National Climate Change Adaptation Plan, the main climate hazards and impacts in Chad are droughts, temperature rises, floods, and high winds. According to the country’s updated National Determined Contribution [10], the results of consultations with stakeholders have shown that the priority sectors for climate change adaptation are agriculture and livestock, environment and forestry, water and sanitation, renewable energies, gender and social protection, education and communication, risk management, infrastructure and land use planning, fisheries resources, and aquaculture. The health sector and health systems have unfortunately been left in the lurch, despite the international community’s warnings of the severe impact of climate hazards on health. While the Intergovernmental Panel on Climate Change (IPCC) [3], in its latest report, mentions that there are major gaps in the research on understanding and mitigating the vulnerabilities of healthcare systems and the associated impacts of climate change, the report stresses the need to produce scientific information at the local level, enabling one to identify the realities of this vulnerability and the impacts of climate risks on health systems, in order to make way for the design of integrative climate policies. An important step in integrating health adaptation and resilience strategies into urban planning tools and approaches is the production of scientific knowledge on health systems, their vulnerability as perceived by city dwellers, and individual adaptation and resilience strategies (WMO, 2023). Given the lack of scientific knowledge supporting the formulation and implementation of effective health resilience policies, the current study is necessary.
What are the climatic risks and their impact on the population and healthcare systems of the city of N’Djaména? The aim of our study is to fill gaps in the availability of scientific knowledge on the effects of climate risks on healthcare systems and the adaptation strategies used at the individual level in order to activate and catalyze the alignment of climate policies and future planning for the sustainability of the healthcare systems in the city of N’Djaména and its sub-region. Specifically, our study involves the following aims:
- Show the urban climatic risks and their impacts on the health systems of the city of N’Djaména;
- List the vulnerability factors relating to city dwellers and health systems (health infrastructure, health personnel, living environment, and human health) in the city of N’Djaména;
- List adaptation and resilience strategies used at the individual level to facilitate recommendations for a kind of urban planning that takes into account the resilience of health systems.
2. Literature Review
2.1. Vulnerability of Health Systems and Impacts of Climate Risks
The World Health Organization [11] points to five vulnerability factors that exacerbate the impacts of climate risks on health systems. These vulnerability factors include demographic, geographic, biological and health factors, socio-political conditions, and socio-economic factors. According to Dumenu and Obeng [12], national health systems in developing countries are often overwhelmed in the wake of floods as they have few resources to focus on health crises. ClimaHealth [4] points out that health infrastructures are at the mercy of climatic hazards, in that community health centers are often flooded and deprived of electricity during violent storms and floods. As a result, they are unable to provide essential obstetric care and treat the wounded who turn up for help. Climate change is affecting healthcare facilities in many contexts across Africa, from global temperature rises to floods, storms, extreme temperatures, and intense recurrent droughts. All these climatic hazards cause and accentuate the development and distribution of diseases of all kinds.
The work of Peirce et al. [13] and Lala and Hagishima [14] has established a significant link between severe weather events and increased risk of non-communicable respiratory diseases and infectious diseases. Extreme weather events can aggravate pre-existing respiratory conditions and increase the risk of developing climate-sensitive diseases. According to Ashrafuzzaman et al. [15], direct risks include health effects caused by heat waves and extreme weather conditions, including storms, floods, and drought. Climate change will affect the provision of healthcare and other services, as it is currently affecting national economies and infrastructure [16,17]. These risks are unevenly and geographically distributed across countries, cities, and rural areas and affect populations differently, especially poor and marginalized groups, people with disabilities, the elderly, women, and young people, as they are the most vulnerable facets of the population [18].
Mechanisms for indirect impacts on health risks include a complex interplay of ecological and biological systems that influence pathogen growth rates, the range and activity of disease vectors (such as mosquitoes), water flow and quality, and crop yields [19]. Many infectious diseases, including vector-borne diseases, are associated with changes in climatic conditions such as temperature, precipitation, and humidity [20]. Aware of all of the above, Allarané et al. [21] find that the need for populations to adapt to climate change and its socio-health impacts is essential as their survival depends on it. Similarly, Jamali et al. [22] believe that individual strategies should be transformed into curriculum-driven strategies derived from a robust climate framework in order to move towards peoples’ resilience.
2.2. Adaptation and Resilience of Healthcare Systems and Individuals
Health system resilience is “the capacity and ability of health systems to anticipate, prevent, prepare, absorb, adapt and transform when exposed to shocks and stresses, and to provide routine health services without interruption during crisis management” [23]. Climate-resilient health systems are capable of anticipating, responding to, coping with, recovering from, and adapting to climate-related shocks and stress in order to sustainably improve population health, despite an unstable climate [4]. Emergency preparedness and rapid crisis response, including proactive risk management, adequate risk communication, and community empowerment, strengthen resilience [24]. According to Ali et al. [25], a prepared, active, and well-organized community reduces the negative effects of emergencies, thereby reducing morbidity and mortality. Any proactive approach requires the production and valorization of scientific information. Health professionals, especially primary healthcare workers, should educate the community about climate-related health impacts and mitigation strategies [26]. Vulnerable groups such as disabled and dependent people deserve greater attention when extreme weather conditions such as heatwaves or cold snaps occur. They should be contacted by health professionals and relocated to safe areas [27]. Adaptation responses are necessarily context-specific and may focus on providing services to vulnerable and high-risk populations [2,12,20]. Strengthening health systems, including healthcare facilities, is a key element of health adaptation planning and should be included in each country’s national health adaptation plan [4,18,28]. In addition to building climate-resilient health systems, the World Meteorological Organization (WMO, 2023) assumes that building and maintaining public health infrastructure (such as water and sanitation systems, laboratories, access roads, etc.) may be the most important, cost-effective, and urgent strategy for enabling populations and health systems to adapt to climate change. In their research, Ali et al. [25] identified interventions and actions to strengthen resilient health systems capable of coping with the adverse health effects of climate change. A total of 87 actions have been identified to build a climate-resilient healthcare system, classified into six themes. These include good governance and leadership, financing, quality of the healthcare workforce, essential medical products and technology, and health information and service delivery systems. The actions most frequently cited in the development of a national climate change adaptation plan for the health sector are the development of plans for essential services (electricity, heating, cooling, ventilation, and water supply), the assessment of health system vulnerabilities and capacities, and the improvement of surveillance systems targeting climate-sensitive diseases and infectious diseases [2,29].
3. Materials and Methods
3.1. Study Area
N’Djaména, the political capital of the Republic of Chad, is located between 12°00′ and 13°00′ north latitude and 15°00′ and 16°00′ east longitude. It is bordered to the north by the Hadjer-Lamis region, to the east by the Chari-Baguirmi region, to the southeast by the Logone river, and to the west by Cameroon (Figure 1). N’Djaména is 1000 km from the Gulf of Benin, 2000 km from the Mediterranean, 2500 km from the Red Sea, and 100 km south of Lake Chad, at the confluence of the Chari and Logone rivers [30]. The city enjoys a dry tropical Sahelian climate characterized by two distinct seasons: a long dry season of seven to eight months from November to May and a short rainy season of three to five months from May to October. The maximum temperatures range from 33.7 °C to 37.6 °C, while the minimum temperatures range from 20.9 °C to 22.7 °C. Precipitation ranges from 400 to 700 mm/year, in the form of showers of varying severity. It is subdivided into 10 arrondissements with a population of 993,492 in 2009 [31] and an estimated 1,699,208 in 2020 [32].
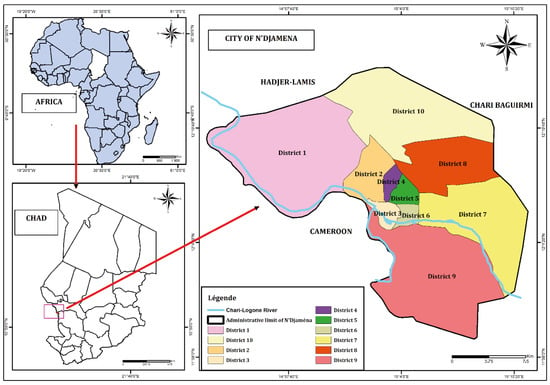
Figure 1.
Geographical location of the city of N’Djaména.
3.2. Sampling and Data Used
This study was carried out using a methodological approach based on documentary research, meteorological data collection, group interviews with managers of public health structures, and individual interviews with the populations of the city’s ten municipal district. The literature search enabled us to browse through similar works carried out in other geographical areas and dealing with the same issue. The meteorological data used were obtained from the National Meteorological Agency. These are rainfall, temperature, and wind data collected in two time sequences. These data have highlighted the constant evolution of meteorological extremes observed in the city of N’Djaména, generating climatic risks that affect the health of the population. The first sequence covers the period from 1960 to 2020, with data at monthly time-steps. It has enabled us to assess the inter-annual variability of rainfall and the inter-annual evolution of wind speed. The second sequence is made up of daily time-step data and covers the period from 1991 to 2020 due to the unavailability of daily data over long periods. This last sequence was used to determine indices of climatic extremes such as the number of days of intense rainfall and heat waves in order to study their evolution over time.
Interviews with health facility managers took place in twenty health centers in the ten districts of N’Djaména, with two health centers per district. The profile of health structure managers is made up of state-qualified doctors, nurses, and midwives. In addition, the interviews with health officials helped us identify existing climatic risks, the various components of health (health facilities, living environment, food, and institutional health governance), and the impacts of climate risks on these health components. Individual surveys were also carried out among sampled households in the city of N’Djaména. The data collection forms used for the population surveys took into account information such as the following:
- −
- Socio-economic characteristics (gender);
- −
- Onset of recurrent diseases and season of onset;
- −
- Vulnerability factors as perceived by city dwellers;
- −
- Coping strategies used by populations in the face of climate-related diseases.
For the household interviews, we surveyed a number of households in each arrondissement, the size of which was proportional to the total number of households. A simple random sampling method was used to select the households to be surveyed. To determine the sample size, we used the inverse of the margin of error formula proposed by Daniel Schwartz. Let n be the sample size for a rounding q, and we have the following:
with Z being the fixed deviation or reduced deviation at a risk of 5% (1,96), corresponding to a confidence interval of 95%, m being the margin of error set at 10%, and P being the proportion of households per district. Table 1 shows the number of respondents by district.

Table 1.
Distribution of respondents by district in N’Djaména.
To administer the household survey questionnaires, we used the KoboCollect software version 2022.4.4., and the data from these surveys were stored on the KoboToolbox platform [15].
3.3. Data Processing and Analysis
The meteorological data collected at daily time-steps were all first subjected to quality control with Rclimdex in order to correct any outliers. These data were then used to identify climatic indices and study the evolution of rainfall, temperature, and wind parameters using the Pettitt and Mann–Kendall statistical tests.
3.3.1. Pettitt Homogeneity Test
The Pettitt test [33] can be used to identify trends and any breaks in stationarity in time series. It was applied with the view of pinpointing the position of an inflection point indicating a possible break. The credibility of these results was verified using Buishand’s U statistical method [34].
KT is the point of change in the series.
3.3.2. Mann–Kendall Trend Test
The Mann–Kendall test is a non-parametric test that measures the significance of trends and breaks in stationarity in time series [35]. Let x1, xT be a sequence of data. Each xi is associated with a number ni counting the elements xj such that i > j and xi > xj. By progressively applying the test described by Sneyers [36], we can determine in detail the periods when groups of above- or below-average values appear.
, the latter, under the null hypothesis of no trend, follows a distribution law of , and ; its formula is then .
The daily data were used to calculate indices characterizing the main risks affecting people’s health. These indices are chosen from the list of indicators linked to climate change variability drawn up by the Expert Team on Climate Change Detection Monotoring and Indices (ETCCDMI) [37]. These indicators are as follows:
- WSDI represents the annual totals of days with at least six consecutive days of maximum temperatures above the 90th percentile. This index is an indicator of heat waves.
- R20 designates the total number of days with precipitation greater than or equal to 20 mm. This index is used to identify intense precipitation events.
- SPI, the standardized precipitation index, is used to assess the interannual variability of time series as well as periods of rainfall deficits and surpluses.

Table 2.
Drought/humidity classification in relation to the SPI value.
The data from field surveys carried out with Kobocollect were analyzed and processed with a computer. Microsoft Excel version 2304 was used to arrange and format the survey data. Next, the R-Studio 4.2.1 software was used with specific packages to apply statistical tests to the time series and produce the graphs. The cartographic illustration of the study town was produced using the ArcGIS 10.4 software and was based on shapefile data retrieved from the N’Djaména town hall Geographic Information System (GIS) department.
4. Results
4.1. Precipitation Risk Analysis
Figure 2 shows the standardized precipitation index (A) and monthly rainfall trends according to the year type (surplus, average, and deficit) (B) over the period from 1960 to 2020. The analysis of this figure shows a high degree of variability in rainfall. The indices ranged from −2.5 to 2.8, indicating three phases in the evolution of rainfall. The first phase was marked by wet periods from 1960 to 1979, with a peak (2.5) in 1961; the second sub-series is characterized by rainfall deficits between 1980 and 2004, with an extremely hot year in 1984. The third phase is characterized by a very stable wet period, with an effect on flooding from 2005 to 2020. This period shows a return of the wet season in N’Djaména (Figure 2A). From this index, the monthly evolution of year types (surplus, average, and deficit) over the period 1960–2020 has been highlighted in Figure 2B. The latter shows that the extremely hot years are characterized by a lack of rainfall, particularly at the heart of rainy periods, whereas the surplus years (very flooded) have surpluses and high rainfall levels during rainy periods and seasons (Figure 2B).
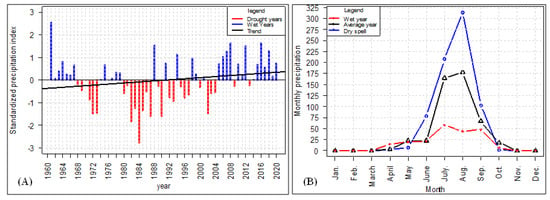
Figure 2.
Standardized precipitation index (A) and monthly rainfall distribution by type of year (B) from 1960 to 2020.
4.2. Analysis of Climatic Extremes
Figure 3 shows interannual trends in the number of days of very intense rainfall (A) and the heatwave index (B) from 1991 to 2020. The analysis of the R20mm index over the last 30 years shows that the city records an average of 10 days of very heavy rainfall per year. The years 1998, 1999, 2000, and 2020 recorded higher numbers of days (14 and 15) of maximum rainfall over the study period. The minimum number of intense rainy days is six, recorded in 1997. Overall, the trend in the number of intense rainy days is upwards (Figure 3A). The analysis of the variation in heat wave days over the period 1991–2020 in the city of Ndjamena shows a significant variation in the number of hot days per year. This number varies from 6 to 24 days, with peaks in 2005 and 2010. Over the thirty-year period, almost 50% of years have seen at least six days of major heat waves. Overall, temperatures in the city of N’Djaména are all on the rise (Figure 3B).
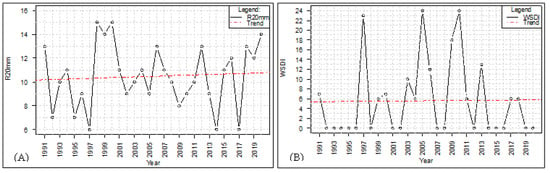
Figure 3.
Interannual trends in days of very intense precipitation (A) and heat waves (B) from 1991 to 2020.
4.3. Wind Speed Dynamics
Figure 4 below shows the inter-annual evolution of wind speed from 1960 to 2020 in the city of N’Djaména. The analysis of this figure shows that the wind speed has varied considerably over time, with higher peaks (3.7 m/s) in 2017 and 2018. The R2 correlation coefficient calculated over this study period is greater than 0.5. This shows that wind speed is strongly correlated with the evolution of years. Pettit’s homogeneity test applied at the 5% threshold to this time series indicates a break in stationarity in 1968. The average rose from 2 m/s between 1960 and 1968 to 3.2 m/s in the second period of the series (1969 to 2020). The Mann–Kendall test shows a p-value well-below 5%, indicating that the upward trend in wind speed over time is highly significant.
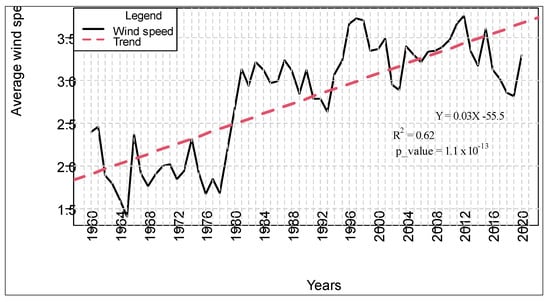
Figure 4.
Interannual variation in wind speed from 1960 to 2020.
4.4. Impacts of Climate Change on Health Components
Table 3 shows the impact of different climatic parameters on the city’s health components. The analysis of this table shows that the health establishments, the living environment, the food sector, and the institutional governance of the health sector are affected in different ways by the meteorological parameters.

Table 3.
Impacts of climate change on health components.
4.4.1. Impacts of Flooding on Health Facilities, Living Environment, and Food Supply
According to those in charge of health facilities and the population of the city of N’Djaména, climatic parameters have a huge impact (Table 3). These impacts include the deterioration and disappearance of healthcare facilities, the discontinuity of healthcare provision in the city, the proliferation of vectors and pathogenic microorganisms, such as the spread of Plasmodium Falciparum, affecting water quality and quantity (drinking water and water used in farming and food processing), the decline in people’s psychic and physiological faculties, etc.
4.4.2. Impacts of Rising Temperatures on Living Conditions and Diet
The people of N’Djaména and those in charge of health facilities have stated that the high temperatures have had a major impact on their living conditions and food supplies. These impacts, mentioned in Table 3, include an increase in certain skin, heart, and respiratory diseases among the population, a reduction in professional productivity, the degradation of food stocks, the putrefaction of food, the acceleration of chemical reactions in the food matrix of certain types of food, the lack of food safety, and the exposure of populations to various illnesses (respiratory diseases, diabetes, cardiovascular accidents, etc.).
4.4.3. Impacts of High Winds on Food and Institutional Health Governance
The high winds in the city of N’Djaména are having a negative impact on the food sector and institutional governance of the health sector, according to statements by health facility managers and the general public (Table 3). These impacts include the contamination of food and drinking water, an increased prevalence of food- and water-borne diseases, increased morbidity among vulnerable people, social stress, the disaggregation of performance and institutional governance efforts in the health sector, and the exacerbation of spending on the health sector by governments and decentralized services, exposing rulers and decision-makers to the hatred and incomprehension of the population.
4.5. Perception of the Seasons in Which the Most Recurrent Diseases Appear
Figure 5 is an alluvial diagram showing the most recurrent diseases according to season and gender. It is mainly used to show associations between categorical variables. In this study, this diagram was used to visualize the population’s perception of the season of onset of the most common diseases as a function of gender. The analysis of this figure clearly shows that cholera and malaria are more frequent in the rainy season. Thermal cramps, on the other hand, are more prevalent in the dry season. Cholera is more likely to occur in women during the rainy season, while malaria is much more likely to occur in men during this period.
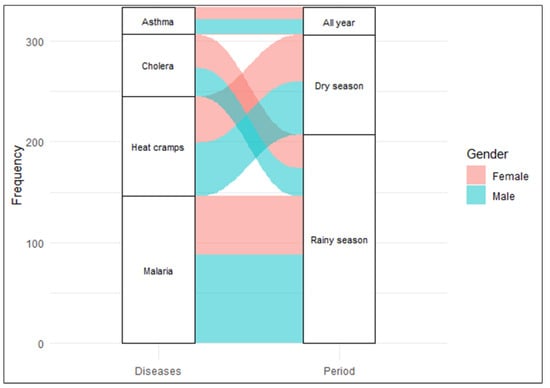
Figure 5.
Perception of the most recurrent illnesses according to season and gender.
4.6. Vulnerability Factors
Figure 6 shows the proportion of vulnerability factors perceived by the city dwellers surveyed in N’Djamena. In all the surveys, twelve vulnerability factors were identified by the citizens. The figure shows that insufficient medical equipment in health facilities (IEME), a fragile physiological state in the face of climatic risks (CFEP), and the failure of city sanitation strategies and policies (DSPA) are the main factors that, according to the women surveyed, make them vulnerable. On the other hand, these factors are rarely cited by men. Only the weakness of insurance mechanisms for populations (FMAP) is cited in equal proportions by both sexes. However, the Khi2 test of independence shows a p-value = 0.2456 with a degree of freedom of 11. As the p-value is above the confidence threshold (5%), the initial hypothesis (H1) that vulnerability factors are linked to gender cannot be validated.
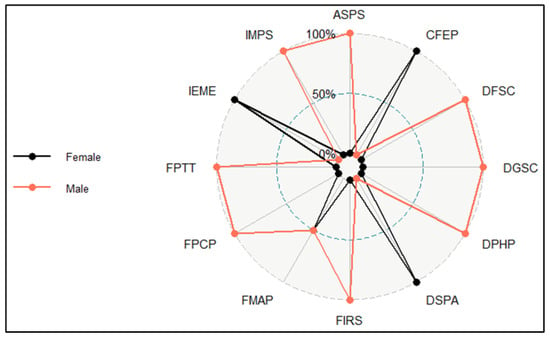
Figure 6.
Perception of vulnerability factors by gender. ASPS: lack of an early warning system in the health sector; CFEP: fragile physiological state in the face of climatic risks; DFSC: failure in the operation of national disaster guarantee funds and services; DGSC: deficiencies in health governance at the community level; DPHP: gradual disappearance of a sense of humanity among the population; DSPA: failure in the city’s sanitation strategies and policies; FIRS: low investment in health-oriented scientific research; FMAP: weaker insurance mechanisms for the population; FPCP: weaknesses in the policy of capacity building for health sector personnel; FPTT: poor performance of water and food treatment technologies; IEME: insufficient medical equipment in health establishments; and IMPS: inadequate healthcare mechanisms.
4.7. Coping Strategies Used by Local Populations
Figure 7 shows the coping strategies used by the population to deal with climate-related illnesses in the city of N’Djaména. The analysis of this figure shows that, during floods, 43.84% of the population surveyed used a combination of coping strategies such as household disinfection with insecticides (DHI) and the use of impregnated mosquito nets (UMI) to protect themselves against malaria. To deal with cholera, the coping strategy used by the population (18.62%) was to disinfect drinking water (DEB). As for adapting to thermal cramps caused by heat waves, the strategies most used by 29.73% of the population were the regular use of tree shade (URA), light/loose clothing during heat waves (HLC), and sleeping outside the house on hot nights (DHM). As for the coping strategies to deal with high winds, 7.81% of the population opted to protect their nasal openings against dust (POP).
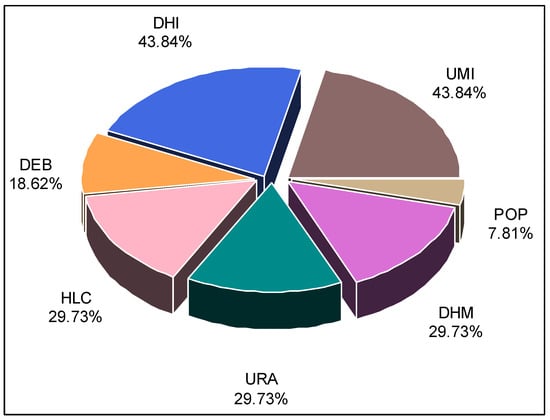
Figure 7.
Proportion of adoption of different adaptation strategies. UMI: use of impregnated mosquito nets; POP: protection of nasal openings against dust; DHM: sleep away from home on hot nights; URA: regular use of shade trees; HLC: light/loose clothing during heat waves; DEB: disinfection of drinking water; and DHI: disinfecting homes with insecticides.
5. Discussion
5.1. Climate Risks, Vulnerability, and Impacts on the Healthcare Sector
Rising temperatures characterizing many very hot years, frequent heavy rains leading to flooding, and very high wind speeds are the results of the oscillation of climatic parameters over many years in the city of N’Djaména. The results revealed the frequency and instability of these climatic parameters and showed that the extreme weather events that result from them are often catastrophic floods, recurrent heat waves, and violent winds. These results confirm those of numerous researchers. According to Allarané et al. [21], extreme weather events such as floods, heat waves, and strong winds have affected not only the living environment but also human health in the city of N’Djaména, sometimes resulting in human deaths. The latest IPCC report [3] also stresses the frequent effects of catastrophic flooding, heat, and high winds in the Sahel region. Bahoutou’s work [7] focuses on the assessment of rainfall and drought in the Sudanian zone of Chad over the last four decades. By analyzing the climatic variability of rainfall and mean annual temperatures, the above-mentioned authors have highlighted sequences of recurrent floods and droughts in southern Chad, a region not far from the city of N’Djaména. Similarly, these results are similar to those of Bedoum et al. [8], who assessed the impact of rainfall variability and drought on agricultural production in southern Chad. The topic of global warming and its link to migration in Lake Chad studied by Kitoto [9] reveals the persistence of extreme weather phenomena.
5.2. Impacts of Climate Risks on Healthcare Systems
In this study, the results visualized the population’s perception of the season of onset of the most common diseases according to gender. These results clearly show that cholera and malaria are more frequent in the rainy season. Thermal cramps, on the other hand, are more common in the dry season. Cholera is more likely to occur in women during the rainy season, while malaria is much more likely to occur in men during this period. Several infectious diseases, including vector-borne diseases, are associated with changes in climatic conditions, such as temperature, precipitation, and humidity [20]. The work of Hlahla and Hill [40] has highlighted the fact that urban communities feel and perceive variations in climatic parameters in different ways in South Africa. According to health facility managers and the people of N’Djaména, climatic risks are having a huge impact on the health sector. Regular flooding has enormous effects on health facilities, the living environment, and food supplies. These impacts include the deterioration and disappearance of health establishments, the discontinuity of health services in the city, the proliferation of vectors and pathogenic microorganisms, the spread of plasmodium falciparum, the impact on water quality and quantity (drinking water and water used in farming and food processing), the reduction in people’s psychological and physiological capacity, etc. For ClimaHealth [4], community health centers are often flooded and deprived of electricity as a result of flooding. Therefore, they are unable to provide essential obstetric care or treat the injured who turn up for help. This is how climate change is affecting healthcare facilities in many contexts across Africa.
The people of N’Djaména and those in charge of health facilities have stated that high temperatures have had a major impact on their living conditions and food supplies. The chain of impacts begins with an increase in the frequency of certain illnesses (skin, heart, and respiratory diseases) among the population, a reduction in professional productivity, the degradation of food stocks, food putrefaction, the acceleration of chemical reactions in the food matrix of certain types of food, food safety insecurity, and the exposure of populations to various illnesses (respiratory diseases, diabetes, cardiovascular accidents, etc.). The work of Peirce et al. [13] and Lala and Hagishima [14] has established a significant link between severe weather events such as heatwave frequency and increased risk for non-communicable respiratory diseases and infectious diseases. According to them, extreme weather events can aggravate pre-existing respiratory conditions and increase the risk of developing climate-sensitive diseases. According to Ashrafuzzaman et al. [15], rising temperatures and heat waves have direct effects on health. Ebi et al. [1] have shown that climate variability and change are already having negative impacts on the health of tens of millions of Africans due to exposure to sub-optimal temperatures and extreme weather conditions as well as increased range and transmission of infectious diseases. In Chad, climate disruption has affected the health sector, making it difficult for people to access basic health services, leading to the emergence of climate-sensitive diseases (malaria, diarrhea, cholera, meningitis, cardiovascular disease, etc.) and a high mortality rate at all ages [41].
The high winds in N’Djaména are having a negative impact on the food sector and on the institutional governance of the health sector, according to statements by health facility managers and the general public. These impacts include the contamination of food and drinking water, the increased prevalence of food- and water-borne diseases, increased morbidity among vulnerable people, social stress, the undermining of performance and institutional governance efforts in the health sector, and the exacerbation of spending on the health sector by governments and decentralized services, etc. These findings reinforce the picture painted by Nhamo and Agyepong [2] when they suggest that mortality and morbidity will increase as global warming continues, putting further pressure on healthcare and economic systems. The mechanisms of the indirect impacts of climate hazards on the occurrence of health risks include a complex interplay of ecological and biological systems that influence pathogen growth rates, the range and activity of disease vectors (such as mosquitoes), water flow and quality, and crop yields [19]. Climate change will affect the provision of healthcare and other services as it affects the national economy and infrastructure [16,17].
5.3. Vulnerability and Sources of Fragility in Healthcare Systems
Of the twelve vulnerability factors identified by citizens, the main ones cited were the following: inadequate medical facilities in health establishments (IEME), the fragile physiological state of certain groups of individuals in the face of climatic risks (CFEP), and the failure of city sanitation strategies and policies (DSPA). The World Health Organization (WHO, 2021) points to five vulnerability factors that exacerbate the impacts of climate risks on health systems. These are demographic factors, geographical factors, biological factors and the health status of citizens, socio-political conditions, and socio-economic factors. The IPCC [3] believes that the best health policies, taking adaptation priorities into account, will enable health systems in vulnerable countries to become more resilient. Many other vulnerability factors were mentioned in the results. These include the absence of an early warning system for the health sector (ASPS), the failure of national calamity guarantee funds and services (DFSC), deficiencies in health governance at community level (DGSC), the gradual disappearance of a sense of humanity and social safety nets among the population (DPHP), the low investment in health-oriented scientific research (FIRS), weak insurance mechanisms for the population (FMAP), weak capacity-building policies for health sector personnel (FPCP), the poor performance of water and food treatment technologies (FPTT), and inadequate health management mechanisms (IMPS). According to Ali et al. [25], the health sector is highly vulnerable to climate change due to the absence and lack of appropriate policies, programs, and measures applicable, particularly in developing countries, to strengthen adaptation and resilience. According to the same authors, unstable and non-resilient healthcare systems exacerbate the negative effects of climate change on people’s health.
5.4. Individual and Institutional Coping Strategies
At the individual level, to adapt during floods, the population surveyed uses both of the following coping strategies to protect against malaria: the disinfection of dwellings with insecticides (DHI) and the use of impregnated mosquito nets (UMI). To cope with cholera, the coping strategy used by the population was disinfecting drinking water (DEB). As for the adaptation to thermal cramps caused by heat waves, the strategies most in demand were the regular use of tree shade (URA), light/loose clothing during heatwaves (HLC), and sleeping outside the house on hot nights (DHM). Atchadé et al. [42] have identified a range of urban ecosystem services that enable city dwellers to adapt to the adverse effects of global warming on urban health. Ashrafuzzaman et al. [15] have also proposed disinfection and water treatment as health resilience strategies. The World Meteorological Organization believes that climate-resilient universal health systems are an essential condition for ensuring equitable and effective protection against the health impacts of climate change (WMO, 2023). According to ClimaHealth [4], protection against climate change depends on strong health systems and individual adaptation efforts. And, the best policies for adaptation and resilience strategies involve taking into account local and individual practices [3]. Emergency preparedness and rapid crisis responses including proactive risk management, adequate risk communication, and community empowerment strengthen resilience [24]. According to the updated National Determined Contribution [10], the warning system, relocation of populations and their habitats, and air-conditioning of offices are the recourse strategies currently being employed. The World Health Organization [11] considers governance and leadership, financing, health workforce, medical products, vaccines and technologies, and information and service delivery to be the six pillars needed to build an effective health system.
6. Conclusions
This study, carried out in the city of N’Djaména, showed the evolution of meteorological parameters and their impact on health systems and populations. The results show that health structures, the living environment, nutrition, and institutional health governance are profoundly affected by climatic risks, namely, floods, heat waves, and violent winds. This situation has repercussions on the health of the city’s population, causing many illnesses. A dozen vulnerability factors were identified by city dwellers, of which three were the most widely recognized. These are the following: insufficient medical equipment in health facilities (IEME), the fragile nature of one’s physiological state in the face of climatic risks (CFEP), and the failure of city sanitation strategies and policies (DSPA). To cope with regular flooding, heat waves, and strong winds, local populations resort to individual coping strategies. Thus, for a transformational adaptation of the already-vulnerable health sector to climate risks, the following recommendations are necessary: strengthen the immune system of vulnerable people (children, pregnant women, and the elderly) by promoting regular vaccination campaigns; improve technologies for treating drinking water and foodstuffs; implement and strengthen policies for managing the living environment, urban development, water management, and sanitation; increase the capacity of social and health infrastructures and medical equipment; and develop nutritional and community governance and strengthen the capacity of healthcare staff through regular training. Our study could have also focused on the correlation between rainfall levels and diseases, with the former favoring the multiplication of malaria pathogens, especially with the current trend of this disease wreaking havoc among vulnerable populations. It would also have been better if the study had truly revealed the interdependence between climatic risks and the evolution of certain diseases and/or infections. That is why the current study is so limited. Future studies could, therefore, explore the real impact of climate risks through the effects of heat on people’s physiological systems. The information generated by the current study can also be used to formulate guidelines and policies for improving healthcare systems in Sahelian cities.
Author Contributions
Conceptualization, N.A.; methodology, N.A.; software, N.A. and V.V.A.A.; validation, F.H.; formal analysis, N.A., V.V.A.A. and A.J.A.; investigation, N.A.; resources, N.A. and F.H.; writing—original draft preparation, N.A.; writing—review and editing, N.A. and A.J.A.; visualization, F.H., A.I.H., R.G.S. and T.-R.N.; supervision, F.H., A.I.H., R.G.S. and T.-R.N.; project administration, F.H.; funding acquisition, N.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Regional Center of Excellence on Sustainable Cities in Africa (CERViDA-DOUNEDON), the Association of African Universities (AUA), and the World Bank. This paper is a part of PhD data collection results whose the amount is 4679.72 USD.
Data Availability Statement
Data will be made available on request.
Acknowledgments
The authors would like to thank the Regional Center of Excellence on Sustainable Cities in Africa (CERViDA-DOUNEDON), the Association of African Universities, and the World Bank Group for the financial support that made this study possible.
Conflicts of Interest
The authors declare no conflicts of interest. Author Adanvo Isaac Houngnigbe was employed by the company CiAAF. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Ebi, K.L.; Barrio, M.O.D. Lessons Learned on Health Adaptation to Climate Variability and Change: Experiences across Low- and Middle-Income Countries. Environ. Health Perspect. 2017, 125, 065001. [Google Scholar] [CrossRef]
- Nhamo, G.; Agyepong, A.O. Climate change adaptation and local government: Institutional complexities surrounding Cape Town’s Day Zero. J. Disaster Risk Stud. 2019, 11, 717. [Google Scholar] [CrossRef]
- IPCC, WGII, Sixth Assessment, Chapter 6. 2022. Available online: https://www.ipcc.ch/report/ar6/wg2/ (accessed on 30 October 2023).
- ClimaHealth. Opinion: Protection from Climate Change Requires Strong Health Systems, Maddie West & Joy Shumake-Guillemot, WMO-WHO Joint Office for Climate and Health. 2023. Available online: https://climahealth.info/opinion-protection-from-climate-change-requires-strong-health-systems/ (accessed on 24 October 2023).
- Verisk Maplecroft 2016. Climate Change Vulnerability 2017. Available online: https://reliefweb.int/report/world/climate-change-vulnerability-index-2017 (accessed on 2 November 2023).
- Abdoulay, M.; Julius, T.N.; Paul, N. Variabilité climatique au Tchad: Perception et stratégie d’adaptation paysanne à Kélo (Tchad). Rev. Electron. Sci. L’environnement VertigO 2022, 22, 1–17. [Google Scholar]
- Baohoutou, L. Les Précipitations en Soudanienne Tchadienne Durant les Quatre Dernières (1960–1999): Variabilités et Impacts. Ph.D. Thesis, Université de Nice, Nice, France, 2007; 245p. [Google Scholar]
- Bedoum, A.; Clobite, B.; Mbanghoguinan, A.; Issak, B.L. Impact de la variabilité pluviométrique et de la sécheresse au sud du Tchad: Effets du changement climatique. Rev. Ivoir. Sci. Technol. 2014, 23, 13–30. [Google Scholar]
- Kitoto, O.A.P. Réchauffement climatique et migration vers les rives du lac Tchad. Migr. Soc. 2016, 163, 149–166. [Google Scholar]
- République du Tchad. Contribution Déterminée au Niveau National Actualisée (CDN Actualisée Tchad); Ministère de l’Environnement, de la Pêche et du Développement Durable: N’Djaména, Chad, 2021; 50p. [Google Scholar]
- WHO. Checklists to Assess Vulnerabilities in Health Care Facilities in the Context of Climate Change; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Dumenu, W.K.; Obeng, E.A. Climate Change and Rural Communities in Ghana: Social Vulnerability, Impacts, Adaptations and Policy Implications. Environ. Sci. Policy 2016, 55, 208–217. [Google Scholar] [CrossRef]
- Peirce, A.M.; Espira, L.M.; Larson, P.S. Climate Change-Related Catastrophic Rainfall Events and Non-Communicable Respiratory Disease: A Systematic Review of the Literature. Climate 2022, 10, 101. [Google Scholar] [CrossRef]
- Lala, B.; Hagishima, A. Impact of Escalating Heat Waves on Students’ Well-Being and Overall Health: A Survey of Primary School Teachers. Climate 2023, 11, 126. [Google Scholar] [CrossRef]
- Ashrafuzzaman, M.; Gomes, C.; Guerra, J. The Changing Climate Is Changing Safe Drinking Water, Impacting Health: A Case in the Southwestern Coastal Region of Bangladesh (SWCRB). Climate 2023, 11, 146. [Google Scholar] [CrossRef]
- Watts, N.; Adger, W.N.; Agnolucci, P.; Blackstock, J.; Byass, P.; Cai, W.; Chaytor, S.; Colbourn, T.; Collins, M.; Cooper, A.; et al. Health and climate change: Policy responses to protect public health. Lancet 2015, 386, 1861–1914. [Google Scholar] [CrossRef]
- Hetcheli, F.; Dandonougbo, I.; Biakouye, A.K. Du village à l’espace périurbain: Mutations socio-économiques du canton d’Adétikopé, un territoire sous influence de Lomé (Togo). In Revue NOTES SCIENTIFIQUES Homme et Société; Numéro Spécial; Université de Lomé: Lomé, Togo, 2017; pp. 311–334. [Google Scholar]
- Chersich, M.F.; Wright, C.Y. Climate change adaptation in South Africa: A case study on the role of the health sector. Glob. Health 2019, 15, 22. [Google Scholar] [CrossRef] [PubMed]
- Bell, J.E.; Brown, C.L.; Conlon, K.; Herring, S.; Kunkel, K.E.; Lawrimore, J.; Luber, G.; Schreck, C.; Smith, A.; Uejio, C. Changes in extreme events and the potential impacts on human health. J. Air Waste Manag. Assoc. 2018, 68, 265–287. [Google Scholar] [CrossRef] [PubMed]
- Herslund, L.B.; Jalayer, F.; Jean-Baptiste, N.; Jorgensen, G.; Kabisch, S.; Kombe, W.; Lindley, S.; Nyed, P.K.; Pauleit, S.; Printz, A.; et al. A multi-dimensional assessment of urban vulnerability to climate change in Sub-Saharan Africa. Nat. Hazards 2015, 82, 149–172. [Google Scholar] [CrossRef]
- Allarané, N.; Azagoun, V.V.A.; Atchadé, A.J.; Hetcheli, F.; Atela, J. Urban Vulnerability and Adaptation Strategies against Recurrent Climate Risks in Central Africa: Evidence from N’Djaména City (Chad). Urban Sci. 2023, 7, 97. [Google Scholar] [CrossRef]
- Jamali, A.; Robati, M.; Nikoomaram, H.; Farsad, F.; Aghamohammadi, H. Urban Resilience and Climate Change: Developing a Multidimensional Index to Adapt against Climate Change in the Iranian Capital City of Tehran. Urban Sci. 2023, 7, 7. [Google Scholar] [CrossRef]
- Ezzati, F.; Mosadeghrad, A.M.; Jaafaripooyan, E. Resiliency of the Iranian healthcare facilities against the COVID-19 pandemic: Challenges and solutions. BMC Health Serv. Res. 2023, 23, 207. [Google Scholar] [CrossRef] [PubMed]
- Xie, E.; Howard, C.; Buchman, S.; Miller, F.A. Acting on climate change for a healthier future: Critical role for primary care in Canada. Can. Fam. Physician 2021, 67, 725–730. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.M.; Isfahani, P.; Eslambolchi, L.; Zahmatkesh, M.; Afshari, M. Strategies to strengthen a climate-resilient health system: A scoping review. Glob. Health 2023, 19, 62. [Google Scholar]
- Green, M.S.; Pri-Or, N.G.; Capeluto, G.; Epstein, Y.; Paz, S. Climate change and health in Israel: Adaptation policies for extreme weather events. Isr. J. Health Policy Res. 2013, 2, 23. [Google Scholar] [CrossRef]
- WHO. WHO Guidance for Climate-Resilient and Environmentally Sustainable Health Care Facilities; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Kjellstrom, T.; Briggs, D.; Freyberg, C.; Lemke, B.; Otto, M.; Hyatt, O. Heat, Human Performance, and Occupational Health: A Key Issue for the Assessment of Global Climate Change Impacts. Annu. Rev. Public Health 2016, 37, 97–112. [Google Scholar] [CrossRef]
- WHO. Operational Framework for Building Climate Resilient Health Systems; World Health Organisation: Geneva, Switzerland, 2015; 56p, Available online: https://apps.who.int/iris/bitstream/handle/10665/189951/9789241565073_eng.pdf (accessed on 4 November 2023).
- Noubayamal, D.E. Vers une Ville-Verte: Proposition du Projet de Développement Urbain de la Commune du 9e Arrondissement de N’Djaména (Tchad). Master’s Thesis, EAMAU, Lomé, Togo, 2018; 195p. [Google Scholar]
- INSEED. Deuxième Recensement Général de la Population et de l’Habitat; Résultats Globaux: N’Djaména, Tchad, 2009; 87p. [Google Scholar]
- Hassane, M.H.; Mahamat, H.A.; Danvidé, T.B. Analyse du processus d’extension de la ville de N’Djamena au Tchad (1900–2018). Geo-Eco-Trop 2021, 45, 507–516. [Google Scholar]
- Pettitt, A. A Non-Parametric Approach to the Change-Point Problem. J. R. Stat. Soc. 1979, 28, 126–135. [Google Scholar] [CrossRef]
- Buishand, T.A. Tests for detecting a shift in the mean of hydrological time series. J. Hydrol. 1984, 73, 51–69. [Google Scholar] [CrossRef]
- Das, S.; Banerjee, S. Investigations of changes in seasonal streamflow and sediment load in the Subarnarekha-Burhabalang basins using Mann-Kendall and Pettitt tests. Arab. J. Geosci. 2021, 14, 946. [Google Scholar] [CrossRef]
- Sneyers, R. Sur l’analyse statistique des séries d’observations. In Note Technique; n°143, OMM-N°415; OMM: Genève, Switzerland, 1975; 192p. [Google Scholar]
- Zhang, X.; Yang, F. RClimDex (1.0) User Manual; Climate Research Branch Environment Canada: Toronto, ON, Canada, 2004; 23p.
- Mckee, T.B.; Doesken, N.J.; Kleist, J. The relationship of drought frequency and duration to time scales. In Proceedings of the Eighth Conference on Applied Climatology, Anaheim, CA, USA, 17–22 January 1993. [Google Scholar]
- OMM. Guide d’Utilisation de l’Indice de Précipitation Normalisé; OMM-N°1090; OMM: Geneva, Switzerland, 2012; 25p. [Google Scholar]
- Hlahla, S.; Hill, T.R. Responses to Climate Variability in Urban Poor Communities in Pietermaritzburg, Kwazulu-Natal, South Africa. Sage Open 2018, 8, 2158244018800914. [Google Scholar] [CrossRef]
- MEPDD. Troisième Communication Nationale (TCN) du Tchad sur les Changements Climatiques; Ministère de l’Environnement, de la Pêche et du Développement Durable: N’Djaména, Chad, 2020; 103p. [Google Scholar]
- Atchadé, A.J.; Kanda, M.; Folega, F.; Atela, J.; Dourma, M.; Wala, K.; Akpagana, K. Urban Ecosystem Services and Determinants of Stakeholders’ Perception for Sustainable Cities Planning in Cotonou (Benin). Sustainability 2023, 15, 9424. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).